Abstract
The success of therapies targeting myocardial reperfusion injury is limited, while the cardioprotective impact of mitigating ischemia-related damage remains less explored. We have recently shown in a pig model that the intravenous administration of a modified atorvastatin preparation during ischemia attenuates the rise of cardiac ischemia injury biomarkers. In the following study, we sought to investigate the mechanisms behind these ischemia-related cardioprotective effects. Ischemia was induced by 90 min total coronary balloon occlusion in pigs fed a normocholesterolemic regime. Fifteen minutes after the onset of ischemia, animals were randomized to receive intravenous atorvastatin preparation (IV-atorva) or vehicle. After ischemia animals were euthanized to assess the effect of IV-atorva treatment on gene and protein levels/activation of senescence-, apoptosis-, and cardioprotective/metabolic-related markers. Proof-of-concept studies were carried out in mice and rats in which treatments or vehicle were administered 15 min after initiation of ischemia induced by permanent coronary ligation. Western-blot analyses revealed that in the ischemic myocardium of IV-atorva-treated pigs, RhoA was inactivated, phosphorylation of p53 and caspase-3 was reduced and AMPK was activated with the consequent regulation of the mTOR/raptor-signaling pathway. IV-atorva-treated rats showed, as compared to vehicle, a significant reduction (60%) in scar size assessed at 1 month by histological staining, and mice studies demonstrated the causal involvement of AMPK activation in IV-atorva mediated cardioprotective effects. We demonstrate in pigs and rodents that prompt intravenous treatment with atorvastatin during ischemia limits cardiac cell death and reduces infarct size through AMPK signaling.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite advances in the treatment of acute coronary syndrome (ACS), subsequent mortality remains high [22] and the development of incident heart failure has increased [36]. While prompt reperfusion is required to salvage the jeopardized myocardium and limit infarct size, the reperfusion process induces the activation of deleterious signaling cascades that deepen cellular damage, ultimately amplifying cardiomyocyte death and myocardial infarction (MI) size enlargement, the so-called ischemia/reperfusion (I/R) injury [6, 52]. The final size of infarction, therefore, depends on reperfusion-related damage on top of ischemic injury which, in turn, is directly related to the duration of the ischemic period.
Interventions inhibiting ischemic damage to limit myocardial injury remain insufficiently explored as a therapeutic alternative. Indeed, a strategy and/or drug capable of mitigating infarct size in the setting of ischemic heart disease remains to be discovered. Thus far, novel therapeutic strategies directed at limiting cardiac damage acting upon reperfusion have had modest results [21]. Ischemic conditioning, a treatment consisting on the application of brief episodes of I/R, either locally or distally, in the setting of reperfusion, has provided promising results in multiple experimental animal models [19, 27, 49] by mitigating reperfusion injury upon the activation of intrinsic pro-survival signaling cascades and reducing infarct size. Unfortunately, the results of Phase-II/Phase-III clinical trials testing the application of these mechanical conditioning approaches have not consistently shown cardioprotection [11, 44].
At a pharmacological level, the only Phase-III clinical trial designed to asses inhibition of I/R injury through the administration of Cyclosporine A in patients with ST-elevation MI (STEMI) was neutral [10]. It is worth noting that we showed that HMG-CoA-reductase (HMG-CoA-R) inhibition by administration of simvastatin just prior to reperfusion, significantly reduced reperfusion injury in swine [48]. This effect was not associated with its lipid-lowering activity, but rather to its inhibitory effect on isoprenoid synthesis. Cardiac healing was further enhanced thereafter by prolonged post-MI oral simvastatin treatment [48]. Moreover, pre-procedural statin therapy has been associated with a reduction in the incidence of larger sized, stenting-related myocardial infarctions in patients undergoing coronary intervention [18]. Therefore, all together, these results have led us to hypothesize that an early appropriate pharmacological intervention during ischemia could limit myocardial damage progression.
So far, remote ischemic conditioning, metoprolol, and intravenous atorvastatin have shown promising effects protecting the heart from ongoing ischemic injury [15, 16, 26, 31]. Indeed, our group has recently shown that the intravenous administration of an atorvastatin preparation (IV-atorva) during ischemia significantly attenuates the rise of cardiac ischemia injury biomarkers [ischemia modified albumin (IMA), cardiac fatty-acid-binding protein (CFABP), and myoglobin], proposing rapid intravenous treatment of acute STEMI patients on first medical contact to reduce the progression of cardiac damage [31]. However, the potential mechanisms behind IV-atorva protective effects remain to be elucidated. In the present study, we provide molecular and cellular insights to understand the effects derived from IV-atorva administration during coronary occlusion in detaining the advancement of ischemic injury and mitigating the progression of MI damage before reperfusion.
Methods
Ethics
Experimental procedures were reviewed and approved by the Institutional Animal Care and Use Committees (CEEA-IR) and authorized by the Animal Experimental Committee of the local government (#5601) in accordance with the Spanish law (RD 53/2013) and European Directive 2010/63/EU. In addition, the investigation conforms to the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH Publication No. 85-23, revised 1985), follows the ARRIVE guidelines, adheres to the Practical guidelines for rigor and reproducibility in preclinical and clinical studies on cardioprotection [5, 29], and is committed to the 3Rs of laboratory animal research and consequently used the minimal number of animals to reach statistical significance [24]. All animals were allowed to acclimatize 7 days before any intervention and housed in individual cages under light-controlled conditions and room temperature.
Experimental design
The experimental design followed in the translational porcine study is detailed in our recent paper by Mendieta et al. [31]. To this end, animals were sedated, and anesthesia was maintained with isoflurane during the whole experimental procedure. Cardiac rhythm, arterial oximetry, and arterial pressure were continuously monitored. Just prior to the procedure, prophylactic antiarrhythmic amiodarone and lidocaine perfusions were initiated to prevent malignant left ventricular arrhythmias. All animals were subjected to the same antiarrhythmic pharmacological approach to allow a direct comparison between the groups. By percutaneous approach and fluoroscopy guidance, ischemia was induced by complete coronary balloon occlusion of the mid-left anterior descending (LAD) coronary artery for 90 min [49, 50]. After 15 min of ischemia, animals were allocated to randomly and blindly receive an intravenous infusion of a modified atorvastatin preparation (IV-atorva, 0.5 mg/kg; n = 7) or vehicle (n = 7). The atorvastatin preparation refers to a soluble atorvastatin calcium salt formulation for intravenous administration (Patent PCT/EP2018/058158). After the ischemic period, animals were directly sacrificed (without reperfusion) with propofol overdose and potassium chloride (2 mol/L). Hearts were rapidly excised to obtain myocardial tissue for molecular studies. Blood samples were collected in EDTA at baseline and after 90 min of ischemia from the femoral artery for peripheral blood mononuclear cell (PBMC) isolation by the Ficoll method.
The mice MI model was performed by LAD coronary artery ligation as previously reported [9]. To this end, male CH3 mice (8–10 weeks, weighing 25–30 g) were intubated and anesthetized with a mixture of O2/isoflurane and mechanically ventilated (rate 90 breaths/min, tidal volume 0.1 mL). Rectal temperature was continuously monitored throughout the surgery and maintained within 37–38 °C using a heating pad and heat lamp. An anterior thoracotomy was performed; the heart was exposed, and the LAD coronary artery was occluded with an intramural stitch (7-0 silk suture, consistent ligation of the left coronary artery, as it emerges from under the left atrium) for 45 min. Successful and complete coronary ligation was verified by electrocardiographic visualization of STEMI pattern that was monitored by high-frequency ultrasounds with Vevo2100 from Visualsonics, and by the visualization of a pale, hypokinetic ventricular myocardium distal to the site of the occlusion. Fifteen minutes after coronary ligation (i.e., 15 min after the onset of ischemia), a single dose of atorvastatin (6 mg/kg; equivalent to 40 mg human; n = 6), β-OH-simvastatin (6 mg/kg; n = 6), or PBS volume for vehicle/controls (n = 6) were administered intraperitoneally. The simvastatin preparation is a solubilized β-hydroxy acid form prepared by conventional hydrolysis (see Patent PCT/EP2018/058158). Ischemia was continued for another 30 min after administration of the single dose (i.e., altogether 45 min of ischemia), and then, mice were directly sacrificed and the heart was carefully excised for infarct size measurement. For morphometric analysis of infarct size, the mouse heart was immersed in a fixative solution (4% paraformaldehyde), embedded in optimal cutting compound (OCT) and cross-sectioned from apex to base (10 µm-thick sections 200 µm distanced). Sections were stained with haematoxylin and eosin and morphometric infarct size analysis was determined using image analysis software (ImageJ, NIH). Taking into consideration that reperfusion is required to obtain a valid infarct size evaluation by TTC staining [42], we chose histopathology to assess cardiac damage, because it is considered to be the gold standard for infarct size analysis, although, as a drawback, it does not allow calculating the ischemic area and, therefore, expressing the size. However, as additional information, infarct size was also assessed by TTC staining (1%). The size of infarction was calculated by the sum of infarcted areas in each section.
Effect of IV-atorva on myocardial RhoA inhibition
We examined whether intravenous administration of IV-atorva affected RhoA activation in the ischemic myocardium of pigs. To this end, tissue samples obtained from the ischemic myocardium of all animals were pulverized and homogenized in lysis buffer for protein isolation and total RhoA assessment. The separation of the membrane and cytosolic fractions was performed by a modification of the lysis buffer protocol [46]. Briefly, tissue powder was homogenized in buffer solution (1 mol/L NaCl, 20 mmol/L Tris pH 7.4, 1 mmol/L DTT and protease inhibitors) and centrifuged. The supernatant was collected (referred to as the cytosolic fraction) and pellets were resuspended, and the membrane proteins were extracted by incubation in 500 mmol/L Tris–HCl pH 7.4, 20% sodium dodecyl sulfate, 100 mmol/L sodium orthovanadate, and protease inhibitors. The extract was centrifuged and the supernatant was collected as the membrane fraction. Protein concentration (in total myocardial tissue, in the cytoplasm fraction and in the membrane fraction) was quantified by the Pierce method. RhoA (Santa Cruz) was determined in total, cytosolic and membrane fractions of the ischemic cardiac tissue of all animals by Western-blot analysis. The intensity of the Western-blot bands was detected with Chemi-Doc (Bio-Rad) and they were quantified with the Quantity one Software (Bio-Rad). Intensities are expressed in arbitrary units (AU).
Effect on myocardial transcript levels and protein expression/activation of markers related to myocardial apoptosis and cardioprotection
We assessed in both the ischemic and non-ischemic myocardium of infarcted pigs, the effect of IV-atorva treatment on gene and protein levels/activation of senescence-, apoptosis-, and cardioprotective- related markers. Accordingly, tissue samples were pulverized and homogenized in Tripure (Roche) for RNA isolation or homogenized in lysis buffer for protein extraction. We performed transcriptomic and Western-blot analyses of (1) p53; (2) caspase-3; (3) AMPK; and (4) eNOS. At a protein level, we assessed: (1) phosphorylated p53 (Ser15) and total p53; (2) cleaved caspase-3 and total caspase-3; (3) AMPK and AMPK phosphorylated at Thr172 (P-AMPK) or activated AMPK; (4) mTOR and mTOR phosphorylated at Ser-7292; (5) raptor and raptor phosphorylated at Ser-792; and (6) eNOS, and eNOS phosphorylated at Ser1177 (P-eNOS) or activated eNOS. The degree of p53, caspase-3, AMPK, mTOR, raptor, and eNOS activation was evaluated by assessing the corresponding ratios (phosphorylated form/total expression). mRNA levels were normalized to the housekeeping gene 18SrRNA, and the intensity of the bands was calculated by densitometry and expressed as arbitrary units (AU).
IV-atorva effect on the inflammatory response
Local myocardial inflammatory response
The effect of atorvastatin on the myocardial expression of monocyte chemoattractant protein-1 (MCP-1/CCL2) was evaluated at mRNA and protein levels in the infarcted pigs. The threshold cycle (Ct) values were determined and normalized to the housekeeping gene 18SrRNA to adjust for equal amounts of RNA, whereas β-actin was used as the protein-loading control. In addition, we also assessed neutrophil infiltration in the ischemic tissue. For this purpose, myocardial samples were embedded in OCT, frozen, and 5 μm sections were obtained from each sample and mounted on gelatinized slides for neutrophil staining (anti-neutrophil elastase antibody, Abcam). Images were captured with an Olympus Vanox AHBT3 microscope, digitalized by a Sony 3 charged-couple device and infiltrated neutrophils counted by a single-blinded observer from an average of 10-fields/animal.
Systemic inflammatory response
We assessed gene levels of toll-like receptor 4 (TLR4) and MCP-1, and protein expression of MCP-1 in circulating PBMCs from pigs. The Ct values were determined and normalized to the housekeeping gene 18SrRNA, whereas Ponceau Red was used for protein-loading control.
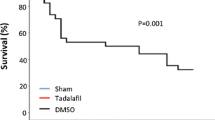
The contribution of AMPK on atorvastatin-mediated cardioprotection
We assessed the causal contribution of AMPK activation on the cardioprotective effects afforded by IV-atorva in the mouse model of coronary ligation. In this case, an AMPK inhibitor (compound C; 30 mg/kg; dissolved in DMSO) was given intraperitoneally 15 min before atorvastatin administration (6 mg/kg; equivalent to 40 mg in human) to block any potential effect of the statin on AMPK activation. IV-atorva was administered at 15 min of ischemia and after 30 min (total ischemic period 45 min) mice were sacrificed and hearts were processed for myocardial infarct size and 8-OH-dG (Abcam ab48508) staining, a measurement indicative of oxidative stress-induced DNA damage.
Cardioprotective effect of different statins: impact on oxidative damage
We explored in the mouse model of coronary ligation whether other statins (i.e., β-OH-simvastatin; 6 mg/kg; administered intraperitoneally in n = 6) also protected against ischemia damage and further investigated the impact of statin treatment on myocardial oxidative damage. To this end, ischemic myocardial tissue was cut into 5 μm-thick slices for 8-OH-dG staining. Staining was calculated by a single-blinded observer from an average of 5-fields/animal as percentage of the stained area. Images were captured by Nikon Eclipse 80i microscope and digitized by Retiga 1300i Fast camera.
IV-atorva effects on scar size
Finally, we addressed whether a single intravenous dose of IV-atorva early after ischemia reduces myocardial scar formation assessed 30 days after induction of ischemia. This method was performed in male Sprague–Dawley rats (n = 16; 8–10 weeks old, weighing 250–300 g; Janvier Laboratory). The animals were anesthetized through intraperitoneal injection of a cocktail containing alfaxalone (10 mg/kg) + midazolam (0.6 mg/kg) + buprenorphine (0.1 mg/kg), intubated by means of a cannula and connected to ventilator for rodents. A left thoracotomy was performed at the level of the fourth intercostal space and MI was induced by permanent LAD coronary artery ligation surrounding it with a 6-0 suture. After 15 min of ischemia rats were randomly given an intravenous injection of 2.75 mg/kg of IV-atorva (equivalent to 40 mg human; n = 8) or equal PBS volume for vehicle/controls (n = 8). Thirty minutes after IV-atorva administration the thoracic cavity was closed with a 4-0 silk suture and animals were allowed to recover and kept for the following 30 days and then sacrificed. Afterwards, hearts were carefully excised for morphometric assessment of infarct size.
Biochemical parameters
Blood was drawn at sacrifice in all pigs for biochemical analyses.
Statistical analysis
The Shapiro–Wilk test was applied to verify the normal distribution of the data. Continuous variables are expressed as mean ± standard deviation. The variation among group means was evaluated using the parametric ANOVA test, followed by the post hoc Scheffé’s comparison method. T test was used for two group mean comparison. A value of P < 0.05 was considered significant. All statistical analyses were performed with the statistical software package Statview.
Results
IV-atorva administered during ischemia inhibits myocardial RhoA activation
The total amount of RhoA protein in the ischemic myocardium remained similar in IV-atorva-treated animals and control pigs (Fig. 1). However, RhoA activation was significantly inhibited in the IV-atorva-treated animals. As such, non-treated control animals showed a lower RhoA cytoplasm/membrane ratio indicative of higher RhoA translocation to the membrane (active form), whereas in IV-atorva-treated animals RhoA was mainly localized in the cytoplasm (inactive).
IV-atorva administration during ischemia inhibits Rho-A activation. RhoA inhibition expressed as ratio between RhoA detected in the cytoplasm (cyt; inactive form) vs. Rho A detected in the membrane (mb; active form). Tissue sampling and Western-blot analyses were performed at the end of the ischemia period (90 min).*P < 0.05 vs. control
IV-atorva administered during ischemia reduces cellular senescence and limits apoptosis execution
The treatment with IV-atorva did not affect p53 mRNA levels or total protein content during the study period of 90 min (Fig. 2a). While total protein content remained unchanged, IV-atorva-treated animals showed reduced p53 activation in the ischemic myocardium and no effects were observed on p53 activation in the non-ischemic heart. Indeed, the p-p53/p53 ratio (a cell senescence marker) was significantly reduced in the ischemic myocardium of treated pigs.
IV-atorva administration during ischemia reduces myocardial cell death in pigs. Intravenous administration of IV-atorva diminished cellular senescence (a) and apoptosis execution (b) in the ischemic myocardium. Tissue sampling and western blot analyses were performed at the end of the ischemia period (90 min).*P < 0.05 vs. control -Isch group; n = 7 animals/group; Isch ischemic myocardium, Non-Isch non-ischemic myocardium
Similarly, IV-atorva did not affect either gene expression or total caspase-3 protein content in ischemic and non-ischemic myocardium as compared to controls. Yet, IV-atorva reduced the levels of cleaved (active) caspase-3 within the ischemic myocardium (Fig. 2b) and consequently reduced the cleaved caspase-3/total caspase-3 ratio (an index of apoptosis execution).
No differences were observed in eNOS transcript levels in the different cardiac regions (Supplemental Fig. 1a), and IV-atorva did not affect ischemia-induced eNOS activation (Supplemental Fig. 1b) during the 90 min of the study.
IV-atorva administered during ischemia limits MI-induced inflammatory response
Myocardial inflammatory recruitment
As shown in Fig. 3a, IV-atorva treatment significantly prevented both MCP-1 mRNA and protein upregulation in the ischemic myocardium as compared to control pigs (P < 0.05). No changes were detected on MCP-1 expression in the non-ischemic myocardial tissue. In addition, the amount of infiltrating neutrophils was reduced by around 50% in the ischemic myocardium of IV-atorva-treated pigs as compared to control animals (Fig. 3b).
IV-atorva administration during ischemia limits myocardial inflammatory response. a Myocardial expression of MCP-1. b Neutrophil cardiac infiltration expressed as % of reduction. Tissue sampling and Western-blot analyses were performed at the end of the ischemia period (90 min).*P < 0.05 vs. control
Systemic inflammatory response in pigs
IV-atorva treatment also markedly attenuated the ischemia-triggered increase in MCP-1 expression in circulating PBMCs both at gene and protein levels (Fig. 4a). No changes were detected in TLR4 expression levels in PBMCs neither prior- (time 0 min) nor post- (time 90 min) ischemia induction (Fig. 4b).
Lipid levels and liver and kidney parameters
No changes were detected as per lipid levels nor liver or kidney function parameters among all animals (Supp. Table 1).
IV-atorva cardioprotective effects during ischemia involve AMPK/mTOR/raptor signaling
IV-atorva did not affect myocardial AMPK mRNA levels or total protein content in the pig hearts (Fig. 5a). While total protein levels remained unchanged, p-AMPK levels were significantly reduced in the ischemic myocardium of control animals but not in the IV-atorva-treated animals (Fig. 5a). No changes were observed in p-AMPK in the non-ischemic cardiac tissue. Accordingly, the ratio p-AMPK/AMPK was significantly increased in IV-atorva-treated pigs.
Involvement of AMPK on IV-statin-related cardioprotection. a Effect of IV-atorva on myocardial AMPK expression and activation in pigs. b Administration of an AMPK inhibitor (i.e., C compound) prior IV-atorva administration abolishes atorvastatin-related cardioprotective effects in mice. c Effects on oxidative damage in mice. Tissue sampling and Western-blot analyses were performed at the end of the ischemia period (90 min) *P < 0.05 vs. non-isch; †P < 0.05 vs. control; **P < 0.05 vs. control and AMPK inh + atorvastatin; IS infarct size, atorva atorvastatin, Isch ischemic myocardium, Non-Isch non-ischemic myocardium
In the MI mice model, we tested whether blockade of AMPK activation by Compound C was able to inhibit the effects of IV-atorva. Indeed, TTC staining revealed that blockade of AMPK activation by Compound C abolished the infarct size-reducing properties achieved by IV-atorva administered shortly after ischemia induction (Fig. 5b). Moreover, AMPK activation also protected against oxidative damage since the administration of Compound C abolished these protective effects (Fig. 5c).
We further assessed AMPK downstream effectors mTOR and raptor involved in autophagy and protein synthesis. As shown in Fig. 6, IV-atorva-administered animals displayed lower activation levels of mTOR (Fig. 6a) in the ischemic cardiac region, whereas, conversely, showed a significant enhancement on P-raptor (Fig. 6b).
Analysis of AMPK downstream effectors mTOR and raptor. Effect of IV-atorva on myocardial mTOR (a) and raptor (b) expression and activation in pigs. Tissue sampling and Western-blot analyses were performed at the end of the ischemia period (90 min).*P < 0.05 vs. control; atorva atorvastatin, Isch ischemic myocardium, Non-Isch non-ischemic myocardium
Simvastatin and atorvastatin exert comparable cardiac protective effects during ischemia
In comparison with vehicle-administered animals, both IV-atorva and β-OH-simvastatin administration reduced the size of infarction by around 50% in the mice model of MI (Fig. 7a). These cardioprotective effects were associated with a significant reduction in myocardial oxidative damage (70% reduction; P < 0.05) in the ischemic myocardium as compared to controls (Fig. 7b).
Cardioprotective effects of statins administered intravenously in a mice model of MI. Size of infarction (a) and intracellular oxidative damage (b). Tissue sampling was performed at the end of the ischemia period (45 min). *P < 0.05 vs. control. IV-β-OH-simva intravenous administration of a beta-hydroxi acid form of simvastatin
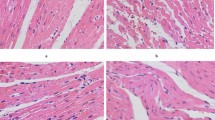
IV-atorva administration during the ischemic insult reduces scar size in a model of chronic ischemia is rats
A single dose of IV-atorva 15 min after the onset of ischemia resulted in a significant 60% reduction in scar size assessed 30 days after induction of ischemia, as compared to control non-treated rats (P < 0.05; Fig. 8a). This effect was consistent among all treated animals (Fig. 8b).
Single administration of IV-atorva during ischemia reduces infarct size assessed 30 days after ischemia induction in a rat model of persistent coronary artery ligation. a Reduction in infarct size expressd. b Individual data. Tissue sampling was performed at the end of the ischemia period (30 days). *P < 0.05 vs. control. N = 6 animals/group
Discussion
In our previous study using a well-characterized MI swine model, where intravenous IV-atorva was administered early upon the onset of ischemia, we observed a significant and sustained reduction of ischemic injury in treated animals detected by an attenuation in the rise of cardiac ischemia biomarkers, that remained at significantly lower levels than in vehicle-administered pigs even after 90 min of ischemia onset. Our results in pigs euthanized before reperfusion clearly indicated that IV-atorva reduced ischemic injury [31]. Moreover, our observations were reported in a preclinical animal model of MI that, in contrast to rodents, comes closest to human STEMI in its temporal and spatial infarct development [20, 29]. In the present work, we evidence the mechanisms behind IV-atorva’s cardioprotective effects. As such, IV-atorva administration in pigs during ischemia: (1) reduces oxidative damage and apoptosis execution in the ischemic myocardium likely preventing cardiac cell death; (2) limits the inflammatory response both locally and systemically; and (3) improves cardiac metabolism through the AMPK/mTORC1 signaling pathway. Moreover, we also demonstrate, in proof-of-principle studies using different rodent models, that IV-atorva reduces infarct size in mice and scar formation in rats at 30 days post-ischemia induction (central figure).

Through the inhibition of HMG-CoA-R, statins reduce LDL-cholesterol levels and decrease cardiovascular morbidity and mortality [2]. Moreover, intensive statin therapy has demonstrated clinical benefit in NSTEMI patients, an effect also observed in patients subjected to elective coronary intervention procedures [8, 13]. Beyond their lipid-lowering effects, which occur after prolonged inhibition of liver HMG-CoA-R, statins have direct cardio- and vasculo- protective properties that explain their beneficial effects in the acute phase of MI. Indeed, several clinical trials (MIRACLE, PROVE-IT-TIMI 22, A–Z, JUPITER) have evidenced the pleiotropic effects of statins [12, 25, 37, 45]. Thus far, experimental studies have shown that statin treatment exerts protective effects that result from the downstream inhibition of small G-protein isoprenylation including the prevention in oxidative stress, a rapid upregulation of endothelial nitric oxide production, red blood cell eNOS activation, and a reduction in infarct size [1, 28, 30]. In this later context, our group demonstrated that the administration of oral rosuvastatin early after reperfusion reduced infarct size in a closed-chest pig model of MI. This effect was due to a reduction in apoptotic cell death and inflammatory cell infiltration leading to improved cardiac function. Moreover, we demonstrated that the effects of rosuvastatin were not related to changes in LDL-cholesterol levels but rather to the inhibition of RhoA translocation in cardiac cell membranes, and activation of cardioprotective kinases (RISK kinases: PI3K/Akt, PKC, Erk). Indeed, the addition of geranylgeranyl pyrophosphate reversed the effect of rosuvastatin by activating the RhoA pathway and, therefore, its translocation to the membranes [7, 47]. In addition, many experimental studies in isolated perfused mouse hearts and rats have shown that statins exert cardioprotection in the setting of I/R, either when administered prior to MI induction (chronic and/or early delivery) or after MI [3, 41]. Interestingly, in 2018, the SECURE-PCI Trial, which investigated the effect of a loading dose of atorvastatin prior to planned PCI on major adverse cardiovascular events in ACS patients, had neutral results. However, significant beneficial effects were observed in the STEMI subgroup of patients, all of which received the treatment close to the moment of intervention [4]. We have recently demonstrated that IV-atorva administration during ischemia significantly attenuates ischemic injury [31]. Here, we evidence that such cardioprotective effects are mediated through RhoA inhibition, reduced oxidative damage, reduced senescence, reduced apoptosis execution, and enhanced AMPK activation within the 90 min of the study. While mRNA expression levels and protein levels were not modified within these 90 min of the study in pigs and 45 min in rodents (actual IV-statin treatment times were 75 min in pigs and 30 min in rodents), post-transductional processes, and protein signaling were interfered by IV-statin. Indeed, proteins related to apoptosis execution (cleaved caspase 3) [14] and cellular senescence (p53-phosphorylation) [39], that are activated during the ischemic process, were significantly reduced in statin-treated animals likely preventing myocyte cell loss. Similarly, eNOS protein levels were unaffected by IV-atorva due to this narrow window from treatment to euthanasia (75 min). In the mice model, we also demonstrate that the reduction in infarct size observed upon IV-atorva administration is comparable to that observed upon treatment with another modified statin, simvastatin, and was associated with a significant blockade of DNA oxidative damage induced by ischemia. Whether other more hydrophylic statins show similar acute effects remains to be determined. We also demonstrate a causal contribution of AMPK to the effects of IV-atorva administration, since the pre-treatment of mice with an AMPK inhibitor significantly reduced the effects of IV-atorva on infarct size and on the inhibition of DNA oxidative damage. It has long been known that statins activate vascular cell AMPK activity in vitro [43], and fairly recent studies have demonstrated that Rho-kinase inhibition operates through AMPK activation [23]. Indeed, we have observed that the disruption of RhoA induces AMPK activation in our statin-treated animals [34]. Of note, previous studies in mouse isolated perfused hearts had shown an enhancement of myocardial AMPK activation during the global ischemic insult [40]. Yet, our in vivo pig model of 90 min total LAD coronary occlusion does not reflect changes in AMPK between the ischemic and remote cardiac tissue. Whether the differences rely on the different level of ischemia of the experimental approach (total heart vs. one coronary bed) or the animal model, deserves to be investigated. Interestingly, we also observe that AMPK activation is associated with mTOR inhibition and raptor activation [35]. Raptor and mTOR are key components of the mTORC1 pathway, along with the mammalian lethalSEC13 protein 8 (mLST8). Inhibition of mTOR limits mTORC1 activity, whereas raptor acts as an AMPK substrate and upon phosphorylation directly inhibits the mTORC1 signaling [17]. Overall, our data suggest that early administration of IV-atorva during ischemia enhances AMPK activation, thereby promoting autophagy and the degradation of cell components to maintain essential activity and viability, and inhibiting RNA translation and protein synthesis to limit energy consumption that can then be utilized for more vital cellular functions (e.g., cell survival). In concurrence with our findings, the role of enhancing autophagy as a cardioprotective strategy in the setting of MI has been recently supported [33].
The lack of continuous assessment of myocardial changes at different timepoints throughout the ischemic period after treatment with the statin can be considered a limitation in our study. No doubt this monitoring would have strengthened our results. Indeed we only have protein analysis at the end of the 90 min of ischemia. However, considering the strong association between ischemic damage and reperfusion injury [38], and our further ongoing results, we can postulate that intravenous statin administration during ischemia impacts the overall phenomenon of I/R injury.
Finally, the rat model of permanent artery ligation demonstrates that intravenous administration of a bolus injection of IV-atorva at the beginning of ischemia translates into lower myocardial scarring at 30 days post-MI, further supporting infarct size reduction and a long-term benefit of this pharmacological approach on left ventricular remodeling.
We had previously published that 90 min of myocardial ischemia promoted an inflammatory phenotype by inducing cardiac local recruitment of macrophages and systemic activation of mononuclear cells [51]. Here, we evidence that IV-atorva early after ischemia induction not only reduces the cardiac expression of a chemokine critically involved in monocyte recruitment, but also limits neutrophil infiltration in the ischemic myocardium. Moreover, we have also evidenced that IV-atorva early after ischemia induction exerts anti-inflammatory effects that extend beyond the cardiac ischemic tissue to the systemic circulation by preventing ischemia-related MCP-1induction in circulating PBMCs. Whether these anti-inflammatory effects translate into diminished microvascular obstruction and further cardioprotection deserves to be investigated [32].
Conclusions
Intravenous administration of statin in the early phase of ischemia induces fast-acting and long-standing cardioprotective effects, which are mediated by isoprenoid synthesis inhibition in the damaged cardiac cells. Accordingly, RhoA activation pathways are interrupted, apoptosis, cell damage, and cell senescence are halted and AMPK-mediated pathways promoted, ultimately reducing infarct size. Our findings, obtained using three different animal models help to explain the prompt, robust and reproducible cardioprotective effects observed upon IV-atorva treatment administration.
References
Antoniades C, Demosthenous M, Reilly S, Margaritis M, Zhang MH, Antonopoulos A, Marinou K, Nahar K, Jayaram R, Tousoulis D, Bakogiannis C, Sayeed R, Triantafyllou C, Koumallos N, Psarros C, Miliou A, Stefanadis C, Channon KM, Casadei B (2012) Myocardial redox state predicts in-hospital clinical outcome after cardiac surgery effects of short-term pre-operative statin treatment. J Am Coll Cardiol 59:60–70. https://doi.org/10.1016/j.jacc.2011.08.062
Baigent C, Blackwell L, Emberson J, Holland LE, Reith C, Bhala N, Peto R, Barnes EH, Keech A, Simes J, Collins R (2010) Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet 376:1670–1681. https://doi.org/10.1016/S0140-6736(10)61350-5
Bell RM, Yellon DM (2003) Atorvastatin, administered at the onset of reperfusion, and independent of lipid lowering, protects the myocardium by up-regulating a pro-survival pathway. J Am Coll Cardiol 41:508–515. https://doi.org/10.1016/s0735-1097(02)02816-4
Berwanger O, Santucci EV, de Barros ESPGM, Jesuino IA, Damiani LP, Barbosa LM, Santos RHN, Laranjeira LN, Egydio FM, Borges de Oliveira JA, Dall Orto FTC, Beraldo de Andrade P, Bienert IRC, Bosso CE, Mangione JA, Polanczyk CA, Sousa A, Kalil RAK, Santos LM, Sposito AC, Rech RL, Sousa ACS, Baldissera F, Nascimento BR, Giraldez R, Cavalcanti AB, Pereira SB, Mattos LA, Armaganijan LV, Guimaraes HP, Sousa J, Alexander JH, Granger CB, Lopes RD, Investigators S-P (2018) Effect of loading dose of atorvastatin prior to planned percutaneous coronary intervention on major adverse cardiovascular events in acute coronary syndrome: the SECURE-PCI randomized clinical trial. JAMA 319:1331–1340. https://doi.org/10.1001/jama.2018.2444
Botker HE, Hausenloy D, Andreadou I, Antonucci S, Boengler K, Davidson SM, Deshwal S, Devaux Y, Di Lisa F, Di Sante M, Efentakis P, Femmino S, Garcia-Dorado D, Giricz Z, Ibanez B, Iliodromitis E, Kaludercic N, Kleinbongard P, Neuhauser M, Ovize M, Pagliaro P, Rahbek-Schmidt M, Ruiz-Meana M, Schluter KD, Schulz R, Skyschally A, Wilder C, Yellon DM, Ferdinandy P, Heusch G (2018) Practical guidelines for rigor and reproducibility in preclinical and clinical studies on cardioprotection. Basic Res Cardiol 113:39. https://doi.org/10.1007/s00395-018-0696-8
Braunwald E, Kloner RA (1985) Myocardial reperfusion: a double-edged sword? J Clin Investig 76:1713–1719. https://doi.org/10.1172/JCI112160
Bulhak A, Roy J, Hedin U, Sjoquist PO, Pernow J (2007) Cardioprotective effect of rosuvastatin in vivo is dependent on inhibition of geranylgeranyl pyrophosphate and altered RhoA membrane translocation. Am J Physiol-Heart Circ Physiol 292:H3158–H3163. https://doi.org/10.1152/ajpheart.01354.2006
Cannon CP, Braunwald E, McCabe CH, Rader DJ, Rouleau JL, Belder R, Joyal SV, Hill KA, Pfeffer MA, Skene AM, Pravastatin or Atorvastatin E, Infection Therapy-Thrombolysis in Myocardial Infarction I (2004) Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med 350:1495–1504. https://doi.org/10.1056/NEJMoa040583
Cubedo J, Vilahur G, Casani L, Mendieta G, Gomez-Jabalera E, Juan-Babot O, Padro T, Badimon L (2016) Targeting the molecular mechanisms of ischemic damage: protective effects of alpha-crystallin-B. Int J Cardiol 215:406–416. https://doi.org/10.1016/j.ijcard.2016.04.072
Cung TT, Morel O, Cayla G, Rioufol G, Garcia-Dorado D, Angoulvant D, Bonnefoy-Cudraz E, Guerin P, Elbaz M, Delarche N, Coste P, Vanzetto G, Metge M, Aupetit JF, Jouve B, Motreff P, Tron C, Labeque JN, Steg PG, Cottin Y, Range G, Clerc J, Claeys MJ, Coussement P, Prunier F, Moulin F, Roth O, Belle L, Dubois P, Barragan P, Gilard M, Piot C, Colin P, De Poli F, Morice MC, Ider O, Dubois-Rande JL, Unterseeh T, Le Breton H, Beard T, Blanchard D, Grollier G, Malquarti V, Staat P, Sudre A, Elmer E, Hansson MJ, Bergerot C, Boussaha I, Jossan C, Derumeaux G, Mewton N, Ovize M (2015) Cyclosporine before PCI in patients with acute myocardial infarction. N Engl J Med 373:1021–1031. https://doi.org/10.1056/NEJMoa1505489
Davidson SM, Ferdinandy P, Andreadou I, Botker HE, Heusch G, Ibanez B, Ovize M, Schulz R, Yellon DM, Hausenloy DJ, Garcia-Dorado D, Action CC (2019) Multitarget strategies to reduce myocardial ischemia/reperfusion injury: JACC review topic of the week. J Am Coll Cardiol 73:89–99. https://doi.org/10.1016/j.jacc.2018.09.086
de Lemos JA, Blazing MA, Wiviott SD, Lewis EF, Fox KA, White HD, Rouleau JL, Pedersen TR, Gardner LH, Mukherjee R, Ramsey KE, Palmisano J, Bilheimer DW, Pfeffer MA, Califf RM, Braunwald E, Investigators (2004) Early intensive vs a delayed conservative simvastatin strategy in patients with acute coronary syndromes: phase Z of the A to Z trial. JAMA 292:1307–1316. https://doi.org/10.1001/jama.292.11.1307
Di Sciascio G, Patti G, Pasceri V, Gaspardone A, Colonna G, Montinaro A (2009) Efficacy of atorvastatin reload in patients on chronic statin therapy undergoing percutaneous coronary intervention: results of the ARMYDA-RECAPTURE (atorvastatin for reduction of myocardial damage during angioplasty) randomized trial. J Am Coll Cardiol 54:558–565. https://doi.org/10.1016/j.jacc.2009.05.028
Duran X, Vilahur G, Badimon L (2009) Exogenous in vivo NO-donor treatment preserves p53 levels and protects vascular cells from apoptosis. Atherosclerosis 205:101–106. https://doi.org/10.1016/j.atherosclerosis.2008.11.016
Garcia-Ruiz JM, Fernandez-Jimenez R, Garcia-Alvarez A, Pizarro G, Galan-Arriola C, Fernandez-Friera L, Mateos A, Nuno-Ayala M, Aguero J, Sanchez-Gonzalez J, Garcia-Prieto J, Lopez-Melgar B, Martinez-Tenorio P, Lopez-Martin GJ, Macias A, Perez-Asenjo B, Cabrera JA, Fernandez-Ortiz A, Fuster V, Ibanez B (2016) Impact of the timing of metoprolol administration during STEMI on infarct size and ventricular function. J Am Coll Cardiol 67:2093–2104. https://doi.org/10.1016/j.jacc.2016.02.050
Gaspar A, Lourenco AP, Pereira MA, Azevedo P, Roncon-Albuquerque R Jr, Marques J, Leite-Moreira AF (2018) Randomized controlled trial of remote ischaemic conditioning in ST-elevation myocardial infarction as adjuvant to primary angioplasty (RIC-STEMI). Basic Res Cardiol 113:14. https://doi.org/10.1007/s00395-018-0672-3
Gwinn DM, Shackelford DB, Egan DF, Mihaylova MM, Mery A, Vasquez DS, Turk BE, Shaw RJ (2008) AMPK phosphorylation of raptor mediates a metabolic checkpoint. Mol Cell 30:214–226. https://doi.org/10.1016/j.molcel.2008.03.003
Herrmann J, Lerman A, Baumgart D, Volbracht L, Schulz R, von Birgelen C, Haude M, Heusch G, Erbel R (2002) Preprocedural statin medication reduces the extent of periprocedural non-Q-wave myocardial infarction. Circulation 106:2180–2183. https://doi.org/10.1161/01.cir.0000037520.89770.5e
Heusch G (2015) Molecular basis of cardioprotection: signal transduction in ischemic pre-, post-, and remote conditioning. Circ Res 116:674–699. https://doi.org/10.1161/circresaha.116.305348
Heusch G, Skyschally A, Kleinbongard P (2018) Translation, translation, translation. Circ Res 123:931–933. https://doi.org/10.1161/circresaha.118.313947
Ibanez B, Heusch G, Ovize M, Van de Werf F (2015) Evolving therapies for myocardial ischemia/reperfusion injury. J Am Coll Cardiol 65:1454–1471. https://doi.org/10.1016/j.jacc.2015.02.032
Johansson S, Rosengren A, Young K, Jennings E (2017) Mortality and morbidity trends after the first year in survivors of acute myocardial infarction: a systematic review. BMC Cardiovasc Disord 17:53. https://doi.org/10.1186/s12872-017-0482-9
Kamel WA, Sugihara E, Nobusue H, Yamaguchi-Iwai S, Onishi N, Maki K, Fukuchi Y, Matsuo K, Muto A, Saya H, Shimizu T (2017) Simvastatin-induced apoptosis in osteosarcoma cells: a key role of RhoA-AMPK/p38 MAPK signaling in antitumor activity. Mol Cancer Ther 16:182–192. https://doi.org/10.1158/1535-7163.MCT-16-0499
Kilkenny C, Browne WJ, Cuthill IC, Emerson M, Altman DG (2010) Improving bioscience research reporting: the ARRIVE guidelines for reporting animal research. PLoS Biol 8:e1000412. https://doi.org/10.1371/journal.pbio.1000412
Kinlay S, Schwartz GG, Olsson AG, Rifai N, Sasiela WJ, Szarek M, Ganz P, Libby P, Myocardial Ischemia Reduction with Aggressive Cholesterol Lowering Study I (2004) Effect of atorvastatin on risk of recurrent cardiovascular events after an acute coronary syndrome associated with high soluble CD40 ligand in the myocardial ischemia reduction with aggressive cholesterol lowering (MIRACL) study. Circulation 110:386–391. https://doi.org/10.1161/01.cir.0000136588.62638.5e
Kleinbongard P, Amanakis G, Skyschally A, Heusch G (2018) Reflection of cardioprotection by remote ischemic perconditioning in attenuated ST-segment elevation during ongoing coronary occlusion in pigs: evidence for cardioprotection from ischemic injury. Circ Res 122:1102–1108. https://doi.org/10.1161/CIRCRESAHA.118.312784
Lacerda L, Somers S, Opie LH, Lecour S (2009) Ischaemic postconditioning protects against reperfusion injury via the SAFE pathway. Cardiovasc Res 84:201–208. https://doi.org/10.1093/cvr/cvp274
Laufs U, Adam O (2012) Acute effects of statins. J Am Coll Cardiol 59:71–73. https://doi.org/10.1016/j.jacc.2011.08.063
Lindsey ML, Bolli R, Canty JM Jr, Du XJ, Frangogiannis NG, Frantz S, Gourdie RG, Holmes JW, Jones SP, Kloner RA, Lefer DJ, Liao R, Murphy E, Ping P, Przyklenk K, Recchia FA, Schwartz Longacre L, Ripplinger CM, Van Eyk JE, Heusch G (2018) Guidelines for experimental models of myocardial ischemia and infarction. Am J Physiol Heart Circ Physiol 314:H812–H838. https://doi.org/10.1152/ajpheart.00335.2017
Ludolph B, Bloch W, Kelm M, Schulz R, Kleinbongard P (2007) Short-term effect of the HMG-CoA reductase inhibitor rosuvastatin on erythrocyte nitric oxide synthase activity. Vasc Health Risk Manag 3:1069–1073
Mendieta G, Ben-Aicha S, Casani L, Badimon L, Sabate M, Vilahur G (2019) Intravenous statin administration during ischemia exerts cardioprotective effects. J Am Coll Cardiol 74:475–477. https://doi.org/10.1016/j.jacc.2019.05.020
Niccoli G, Montone RA, Ibanez B, Thiele H, Crea F, Heusch G, Bulluck H, Hausenloy DJ, Berry C, Stiermaier T, Camici PG, Eitel I (2019) Optimized treatment of ST-elevation myocardial infarction. Circ Res 125:245–258. https://doi.org/10.1161/CIRCRESAHA.119.315344
Nikolaou PE, Boengler K, Efentakis P, Vouvogiannopoulou K, Zoga A, Gaboriaud-Kolar N, Myrianthopoulos V, Alexakos P, Kostomitsopoulos N, Rerras I, Tsantili-Kakoulidou A, Skaltsounis AL, Papapetropoulos A, Iliodromitis EK, Schulz R, Andreadou I (2019) Investigating and re-evaluating the role of glycogen synthase kinase 3 beta kinase as a molecular target for cardioprotection by using novel pharmacological inhibitors. Cardiovasc Res 115:1228–1243. https://doi.org/10.1093/cvr/cvz061
Noda K, Nakajima S, Godo S, Saito H, Ikeda S, Shimizu T, Enkhjargal B, Fukumoto Y, Tsukita S, Yamada T, Katagiri H, Shimokawa H (2014) Rho-kinase inhibition ameliorates metabolic disorders through activation of AMPK pathway in mice. PLoS One 9:e110446. https://doi.org/10.1371/journal.pone.0110446
Oakhill JS, Scott JW, Kemp BE (2012) AMPK functions as an adenylate charge-regulated protein kinase. Trends Endocrinol Metab TEM 23:125–132. https://doi.org/10.1016/j.tem.2011.12.006
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, Gonzalez-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P, Group ESCSD (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur heart J 37:2129–2200. https://doi.org/10.1093/eurheartj/ehw128
Ridker PM, Cannon CP, Morrow D, Rifai N, Rose LM, McCabe CH, Pfeffer MA, Braunwald E, Pravastatin or Atorvastatin E, Infection Therapy-Thrombolysis in Myocardial Infarction I (2005) C-reactive protein levels and outcomes after statin therapy. N Engl J Med 352:20–28. https://doi.org/10.1056/NEJMoa042378
Rossello X, Ibanez B (2018) Infarct size reduction by targeting ischemic injury: back to square one. Circ Res 122:1041–1043. https://doi.org/10.1161/circresaha.118.312939
Rufini A, Tucci P, Celardo I, Melino G (2013) Senescence and aging: the critical roles of p53. Oncogene 32:5129–5143. https://doi.org/10.1038/onc.2012.640
Russell RR 3rd, Li J, Coven DL, Pypaert M, Zechner C, Palmeri M, Giordano FJ, Mu J, Birnbaum MJ, Young LH (2004) AMP-activated protein kinase mediates ischemic glucose uptake and prevents postischemic cardiac dysfunction, apoptosis, and injury. J Clin Investig 114:495–503. https://doi.org/10.1172/JCI19297
Scalia R, Gooszen ME, Jones SP, Hoffmeyer M, Rimmer DM 3rd, Trocha SD, Huang PL, Smith MB, Lefer AM, Lefer DJ (2001) Simvastatin exerts both anti-inflammatory and cardioprotective effects in apolipoprotein E-deficient mice. Circulation 103:2598–2603. https://doi.org/10.1161/01.cir.103.21.2598
Skyschally A, van Caster P, Iliodromitis EK, Schulz R, Kremastinos DT, Heusch G (2009) Ischemic postconditioning: experimental models and protocol algorithms. Basic Res Cardiol 104:469–483. https://doi.org/10.1007/s00395-009-0040-4
Sun W, Lee TS, Zhu M, Gu C, Wang Y, Zhu Y, Shyy JY (2006) Statins activate AMP-activated protein kinase in vitro and in vivo. Circulation 114:2655–2662. https://doi.org/10.1161/circulationaha.106.630194
Touboul C, Angoulvant D, Mewton N, Ivanes F, Muntean D, Prunier F, Ovize M, Bejan-Angoulvant T (2015) Ischaemic postconditioning reduces infarct size: systematic review and meta-analysis of randomized controlled trials. Arch Cardiovasc Dis 108:39–49. https://doi.org/10.1016/j.acvd.2014.08.004
Tsimikas S, Witztum JL, Miller ER, Sasiela WJ, Szarek M, Olsson AG, Schwartz GG, Myocardial Ischemia Reduction with Aggressive Cholesterol Lowering Study I (2004) High-dose atorvastatin reduces total plasma levels of oxidized phospholipids and immune complexes present on apolipoprotein B-100 in patients with acute coronary syndromes in the MIRACL trial. Circulation 110:1406–1412. https://doi.org/10.1161/01.cir.0000141728.23033.b5
Vilahur G, Casani L, Juan-Babot O, Guerra JM, Badimon L (2012) Infiltrated cardiac lipids impair myofibroblast-induced healing of the myocardial scar post-myocardial infarction. Atherosclerosis 224:368–376. https://doi.org/10.1016/j.atherosclerosis.2012.07.003
Vilahur G, Casani L, Pena E, Duran X, Juan-Babot O, Badimon L (2009) Induction of RISK by HMG-CoA reductase inhibition affords cardioprotection after myocardial infarction. Atherosclerosis 206:95–101. https://doi.org/10.1016/j.atherosclerosis.2009.02.009
Vilahur G, Casani L, Pena E, Juan-Babot O, Mendieta G, Crespo J, Badimon L (2014) HMG-CoA reductase inhibition prior reperfusion improves reparative fibrosis post-myocardial infarction in a preclinical experimental model. Int J Cardiol 175:528–538. https://doi.org/10.1016/j.ijcard.2014.06.040
Vilahur G, Cubedo J, Casani L, Padro T, Sabate-Tenas M, Badimon JJ, Badimon L (2013) Reperfusion-triggered stress protein response in the myocardium is blocked by post-conditioning. Systems biology pathway analysis highlights the key role of the canonical aryl-hydrocarbon receptor pathway. Eur Heart J 34:2082–2093. https://doi.org/10.1093/eurheartj/ehs211
Vilahur G, Gutierrez M, Casani L, Cubedo J, Capdevila A, Pons-Llado G, Carreras F, Hidalgo A, Badimon L (2015) Hypercholesterolemia abolishes high-density lipoprotein-related cardioprotective effects in the setting of myocardial infarction. J Am Coll Cardiol 66:2469–2470. https://doi.org/10.1016/j.jacc.2015.08.901
Vilahur G, Hernandez-Vera R, Molins B, Casani L, Duran X, Padro T, Badimon L (2009) Short-term myocardial ischemia induces cardiac modified C-reactive protein expression and proinflammatory gene (cyclo-oxygenase-2, monocyte chemoattractant protein-1, and tissue factor) upregulation in peripheral blood mononuclear cells. J Thromb Haemost JTH 7:485–493. https://doi.org/10.1111/j.1538-7836.2008.03244.x
Vilahur G, Juan-Babot O, Pena E, Onate B, Casani L, Badimon L (2011) Molecular and cellular mechanisms involved in cardiac remodeling after acute myocardial infarction. J Mol Cell Cardiol 50:522–533. https://doi.org/10.1016/j.yjmcc.2010.12.021
Acknowledgements
We gratefully acknowledge the valuable help and support of M.A. Canovas, P. Catalina, and J. Moreno with animal handling and for the proper conduct of all the experimental and molecular work. This article is part of the PhD studies of G.Mendieta at the Medical School of the University of Barcelona and at the Cardiovascular Program ICCC.
Funding
This work was supported by the Fundació Investigació Marato TV3 #20154310 (to GV), Plan Nacional de Salud (PNS) [PGC2018-094025-B-I00 to GV and SAF2016-76819-R to LB] from the Spanish Ministry of Science and Innovation and funds FEDER “Una Manera de Hacer Europa”; and CIBERCV (to LB). We thank the support of the Generalitat of Catalunya (Secretaria d’Universitats i Recerca del Departament d’Economia i Coneixement de la Generalitat, 2017 SGR 1480) and the Fundación Investigación Cardiovascular-Fundación Jesus Serra for their continuous support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
LB and GV are the authors of the patent (PCT/EP2018/058158) that includes the use of statins for intravenous administration. The remaining authors have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mendieta, G., Ben-Aicha, S., Casani, L. et al. Molecular pathways involved in the cardioprotective effects of intravenous statin administration during ischemia. Basic Res Cardiol 115, 2 (2020). https://doi.org/10.1007/s00395-019-0760-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00395-019-0760-z