Abstract
Purpose
The aim of this study was (1) to assess AT through 13 different mathematical approaches and to compare their results; and (2) to understand if AT occurs after moderate WL.
Methods
Ninety-four participants [mean (SD); BMI, 31.1 (4.3) kg/m2; age, 43.0 (9.4) years; 34% females] underwent a 1-year lifestyle intervention (clinicaltrials.gov ID: NCT03031951) and were randomized to intervention (IG, n = 49) or control groups (CG, n = 45), and all measurements were made at baseline and after 4 months. Fat mass (FM) and fat-free mass (FFM) were measured by dual-energy X-ray absorptiometry and REE by indirect calorimetry. AT was assessed through 13 different approaches, varying in how REE was predicted and/or how AT was assessed.
Results
IG underwent a mean negative energy balance (EB) of 270 (289) kcal/day, p < 0.001), resulting in a WL of − 4.8 (4.9)% and an FM loss of − 11.3 (10.8)%. Regardless of approach, AT occurred in the IG, ranging from ~ − 65 to ~ − 230 kcal/day and three approaches showed significant AT in the CG.
Conclusions
Regardless of approach, AT occurred after moderate WL in the IG. AT assessment should be standardized and comparisons among studies with different methodologies to assess AT must be avoided.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of obesity is increasing worldwide and is considered a major global health problem. Since obesity is caused by an alteration in energy balance (EB), as a result of a prolonged excess energy intake (EI) that surpasses energy expenditure (EE), a strategy to achieve weight loss needs to affect one or both sides of the EB equation by increasing EE and/or decreasing EI. Although it seems simple, EB represents a complex and dynamic system in which its components vary over time [1] and change in response to perturbations in either side of the equation [2, 3].
Interventions aimed at losing weight are abundant in the current literature [4, 5]. However, difficulties in losing weight and maintaining it are common. The lack of adherence to dietary and physical activity (PA) recommendations has been pointed out as one of the major problems, especially if they are not adopted at a long-term basis [6]. Additionally, the existence of metabolic, behavioral, and psychological compensations that may occur during negative EB, including compensatory changes in EE [7], spontaneous PA [8], and increases in EI [9] have been studied.
Originally called “luxuskonsumption”, evidence regarding the existence of adaptive thermogenesis (AT) was reported at the beginning of the last century [10, 11]. However, this “phenomenon” only became a matter of debate in the second half of the century, mainly due to the possible role of the brown adipose tissue as the main effector on AT [12, 13]. In 1995, Leibel et al. [14] brought an innovated perspective by showing that the measured decrease in metabolic rate induced by weight loss (WL) was greater than the change predicted by baseline values of fat mass (FM) and fat-free mass (FFM). Therefore, AT has been defined as the decrease in the EE components [resting energy expenditure (REE) and physical activity energy expenditure (PAEE)] beyond what could be predicted from the changes in FM and FFM in response to a negative EB [15, 16].
AT has been studied as a possible barrier to WL, as its existence has been reported not only after a period of WL but also in an early stage of a caloric restriction. In fact, Heinitz et al. [17] showed that the magnitude of AT in the early stage of caloric deficit predicts long-term changes in body composition. Therefore, similarly to the assessments used to categorize spendthrift versus thrifty phenotypes, the inclusion of AT as a predictor of WL may lead to a better understanding the reasons for a higher susceptibility to weight change and therefore difficulties in maintaining a reduced weight state [17]. However, AT’s existence has been recently questioned, especially in the long-term weight management [18,19,20,21,22,23,24], whereas some authors showed that AT may difficult WL and promote weight regain in studies inducing massive WL [22, 25,26,27], others argued that the suppositions regarding AT are exaggerated [28, 29].
The lack of consistency among studies may be due to the lack of standardization of the methodologies to assess AT in REE. As a consequence, different methodologies have been used in the literature, varying on how REE and body composition were assessed [30]. To our knowledge, only Byrne et al. [31] assessed AT using more than one approach to calculate changes in REE, using three different equations to predict REE. As their goal was to compare two different approaches of caloric restriction (intermittent versus continuous), comparisons among methodologies were not addressed in detail. Therefore, the aim of this study was (1) to assess AT through 13 different mathematical approaches (differing in how AT is assessed and/or how REE is predicted) and (2) to understand if AT occurs after a lifestyle intervention.
Methodology
Participants and study design
This study is a part of a major randomized clinical trial performed among healthy former top-level athletes with overweight and obesity (clinicaltrials.gov ID: NCT03031951) [32]. A schematic description of the study phases is presented in Fig. 1.
A total of 94 healthy participants of both sexes were selected and randomly assigned to one of the two groups: intervention or control group. All of the participants were overweight/obese (BMI \(\ge \) 24.9 kg/m2), inactive (< 20 min/day of vigorous physical activity intensity for at least 3 days per week or < 30 min/day of moderate intensity physical activity for at least 5 days per week [33]), aged 18–65 years, and ready to modify their diet to achieve a lower body weight. For a more detailed description of inclusion and exclusion criteria, see the study protocol [32]. In this study, we used measurements made at baseline (0 months) and after the intervention (4 months).
Lifestyle intervention
Nutritional appointments were given by a registered dietitian to each participant. This meeting was intended to provide a well-balanced personalized diet plan, calculated to create a moderate energy restriction from ~ 300 to 500 kcal/day according to each participant’s energy requirements and preferences. Additional appointments were also realized to adjust caloric intake throughout the intervention. In addition, participants attended 12 educational sessions aimed to promote a healthy lifestyle, including educational content and practical application in the areas of PA and exercise, diet and eating behavior, as well as behavior modification.
Participants from the control group were placed on a waiting list to be offered the lifestyle intervention. Upon the completion of the study’s assessments, they had the opportunity to receive the proper nutritional monitoring and the content taught during the educational sessions.
Anthropometry
Subjects had their weight and height measured wearing a bathing suit and without shoes to the nearest 0.01 kg and 0.1 cm, respectively, with a scale and stadiometer (Seca, Hamburg, Germany). Body mass index was calculated using the formula [weight (kg)/height2 (m2)].
Dual-energy X-ray absorptiometry (DXA)
To estimate total and regional FM and FFM, dual-energy X-ray absorptiometry (DXA) (Hologic Explorer-W, Waltham, USA) was used. A whole-body scan was performed, and the attenuation of X-rays pulsed between 70 and 140 kV synchronously with the line frequency for each pixel of the scanned image will be measured. Total abdominal fat, which includes intra-abdominal fat plus subcutaneous fat, was distinguished using DXA by identifying a specific region of interest (ROI) within the analysis programme. Specific DXA ROI for abdominal regional fat was defined as follows: from the upper edge of the second lumbar vertebra (approximately 10 cm above the L4–L5) to above the iliac crest and laterally encompassing the entire breadth of the abdomen, and thus determining total abdominal FM. The calibration procedures were performed according to the manufacturer’s instructions [34]. All the assessments (before and after the intervention) were performed by the same investigator.
Measured resting energy expenditure (REE)
Measured REE (mREE) was obtained in the morning when fasted (7.00–10.00 a.m.). All measurements were performed in the same room at an environmental temperature and humidity of approximately 22 ºC and 40–50%, respectively. The MedGraphics CPX Ultima indirect calorimeter (MedGraphics Corporation, Breezeex Software, Italy) was used to measure breath-by-breath oxygen consumption (\(\dot{V}\)O2) and carbon dioxide production (\(\dot{V}\)CO2) using a facial mask. The oxygen and carbon dioxide analyzers were calibrated in the morning before testing using known gas concentration. The flow and volume were measured using a pneumotachograph calibrated with a 3L-syringe (Hans Rudolph, Inc.TM). Before testing, participants were instructed about all the procedures and asked to relax, breathe normally, and not to sleep or talk during the evaluation.
Before the test, participants rested in supine position for 15 min covered with a blanket, and the calorimeter device was then attached to the mask and breath by breath. \(\dot{V}\)O2 and \(\dot{V}\)CO2 were measured for 30 min, performing a total test duration of 45 min. The first and the last 5 min of data collection were discarded. Steady-state intervals were defined as 5-min periods with ≤ 10% CV for \(\dot{V}\)O2 and \(\dot{V}\)CO2 and Respiratory Exchange Ratio between 0.7 and 1.0 [35]. The mean \(\dot{V}\)O2 and \(\dot{V}\)CO2 of 5 min steady states was used in Weir equation [36] and the period with the lowest REE was considered for data analysis.
Adaptive thermogenesis (AT)
To detect differences in REE beyond what we would expect from body composition alterations, AT was assessed through different approaches, varying in how predicted REE (pREE) was calculated and/or how AT was assessed (Table 1).
To identify the four used approaches regarding the pREE, numbers 1–4 were attributed, where pREE was assessed:
-
1.
By creating a predictive equation using baseline FFM (kg) as an independent predictor;
-
2.
By creating a predictive equation using baseline FM (kg) and FFM (kg) as independent predictors;
-
3.
By creating a predictive equation using baseline FM (kg), FFM (kg), sex, and age as independent predictors;
-
4.
According to the Hayes’ model, i.e., through the sum of the energy production of tissue-organ components (brain, skeletal muscle, adipose tissue, bone, and residual mass) derived from DXA [37].
Regarding the assessment of AT, four approaches were used, identified from A to D, in which:
-
(A)
mREE was adjusted for FM and FFM by linear regression and AT was assessed as the difference between an adjusted REE at baseline and after 4 months (for this approach, pREE was not used) [31];
-
(B)
AT was assessed simply by subtracting pREE (assessed through one of the four aforementioned equations) from mREE (indirect calorimetry), at the end of the intervention (4 months) [24, 31, 38];
-
(C)
AT was calculated as: (a) subtracting pREE from mREE at 4 months; (b) subtracting pREE from mREE at baseline and therefore subtracting the result of (b) from the result of (a) [19, 39];
-
(D)
%AT was calculated as 100 \(\times \) [(mREE/pREE) – 1) after 4 months, and therefore, AT is assessed as (%AT/100) \(\times \) mREE at baseline [40, 41].
To assess AT, approaches 1–4 (pREE) and A–D (AT) were combined, creating 13 methodologies (pREE is not required for approach A).
For all situations, negative values indicate a lower-than-expected decrease in REE considering the changes in body composition, i.e., the measured REE is lower-than-predicted REE, whereas positive values represent a change in REE equal to or greater than the predicted REE (measured REE higher than predicted REE) [7].
Calculation of energy balance (EB)
The EB equation is denoted as follows:
When the EE surpasses the EI, EB is negative. On the other hand, EB is positive when EI is larger than EE. EB represents the average rate of energy deficit or surplus expressed in kilocalories per day and can be calculated from the changed body energy stores from the beginning to the end of the WL intervention. Hence, using the established energy densities for FM and FFM, the follow equation will be applied to quantify the average rate of changed body energy store or lost in kilocalories per day
where \(\Delta\)FM and \(\Delta\)FFM represent the change in grams of FM and FFM from the beginning to end of the intervention and \(\Delta \)t is the time length of the intervention in days.
Statistical analysis
Statistical analysis was performed using IBM SPSS statistics version 25.0 (IBM, Chicago, Illinois, USA). To test the normality of the variables, the Kolmogorov–Smirnov test was performed. Baseline differences between intervention and control group, and between the groups arbitrarily divide into those who lost at least 3% of body weight (which is likely to result in clinically meaningful health benefits [42]) vs those who did not (lost < 3% of body weight) were assessed by independent two sample t test.
Changes in body composition and were assessed by performing Linear Mixed Models, adjusted for randomized group and time as fixed effects and for sex and the baseline values as covariates, assessing the impact of treatment, time (baseline—0 months, post-intervention—4 months) and treatment-by-time interaction. The covariance matrix for repeated measures within subjects over time was modeled as compound symmetry. The one-sample t test was performed to test the significance for AT.
Statistical significance was set at a two-sided p < 0.05.
Results
A total of 94 participants [BMI = 31.1 (4.3) kg/m2, age = 43.0 (9.4) years, 34% females] were included. Changes in body composition and resting energy expenditure are presented in Table 2. A detailed description of the main results of the Champ4life project is presented elsewhere [43].
A time*group interaction was observed for weight and FM (p < 0.05). Weight, FM, and FFM decreased over time for intervention group (within group differences, p < 0.05).
Energy balance calculation
A mean negative EB of 270 (289) kcal/d was observed for the intervention group (different from zero, (p < 0.001), which resulted in a WL of − 4.8 (4.9)% and an FM loss of − 11.3 (10.8)%. The control group presented an EB of 14 (129) kcal/day (not different from zero, p = 0.489), as no significant WL or changes in body composition stores were observed.
Adaptive thermogenesis’ assessment: comparison among approaches
The results for AT are presented in Table 3.
The intervention group showed a significant AT for all four approaches, while the control group presented it for approach A, B.4, and D.4. Differences between groups were found for approach A and C.1 (p < 0.05).
A large variability was found for every approach for both intervention and control group. Approach A was the only with smaller variability (− 179 to 176 and − 205 to 103 for control and intervention group, respectively). When comparing the remaining approaches, approaches C.1.–C.4. were the ones that showed a lower variability.
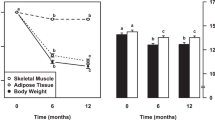
Relation between the variability in AT and the magnitude of WL
The variability in AT (in relative values, %) according to the amount of WL (in relative values, %) for approaches that differed between groups (p < 0.05) is illustrated in Fig. 2 for the IG and CG. The variability in AT according to the amount of WL for all the approaches is presented as a supplementary file (Supplementary file 1).
Implications of adaptive thermogenesis’ calculations according to a specific weight-loss cut-off
A sub-analysis comparing AT values arbitrarily dividing the sample in those who lost at least 3% of their initial weight (WL \(\ge \) 3%) with those who did not (WL \(<\) 3%) is presented in Table 4. From the intervention group, 27 participants (66%) lost at least 3% of their initial weight, being included in the WL group. The WL group was composed of 30 participants [37% female, age: 44.6 (6.0) year] with a mean weight of 90.8 (14.4) kg and 33.6 (8.3)% of FM.
Fifty-two participants were included in the other group (WL < 3%) [33% females, age: 43.4 (10.5) year], with 91.4 (17.9) g and 32.8 (7.7)% for FM. No differences were found between groups for the baseline values.
A mean EB of − 324 (276) and of 132 (84) kcal/day was found for the WL \(\ge \) 3% and the WL < 3% group, respectively (both different from zero, p < 0.001). AT values ranged from ~ − 70 to ~ − 220 kcal for those who lost weight and all the approaches were statistically significant (p < 0.05), except for D.2. For the WL \(\ge \) 3% group, AT was not found in any approach (p > 0.05). Differences between groups were found for approach A, C.1, C.2, C.3, and C.4 (p < 0.05).
Discussion
The major finding of this paper is the clear discrepancy among the methodologies used to assess AT, with values ranging from ~ − 70 to − 220 kcal/day for the intervention group.
An effect of the intervention on AT was observed only for approach A and C.1, while no significant differences between the IG and the CG were found for the remaining methodologies used to assess AT. The IG presented a lower-than-predicted REE when using all the approaches, whereas the CG showed a lower-than-expected decrease on REE using approaches A, B.4, and D.4, though no significant changes in energy stores were observed. In the current literature, AT can be calculated through several mathematical approaches, varying in how REE is predicted and/or how AT is assessed. The most common approach is to assess AT as the difference between measured and predicted REE (calculated through a predictive equation using population’s baseline outcomes) [18, 23, 38]. Other studies performed a similar approach but considering the baseline residuals (measured minus predicted REE at baseline) [19, 39]. Other methodologies were performed, such as the difference between an adjusted measured REE (for FM and/or FFM) before and after a weight-loss intervention (without predicting REE) [31] or as described in Thomas et al. [7, 40]. Therefore, the discrepant findings regarding AT among studies can be in part due to differences in their methodologies.
The mechanisms underlying AT are not well understood, but it has been speculated to involve decreases in circulating leptin, thyroid hormones [15, 44], and blunted activity of the sympathetic nervous system [15]. A leptin reduction is usually associated with an increase in hunger and consequently increased EI [45, 46], leading to a neutral or even positive EB, jeopardizing WL. Moreover, Tremblay et al. [47], showed that changes in circulating organic pollutants (organochlorines), known for their anti-thermogenic properties, were the main predictors of AT, explaining about 50% of its variance. More specifically, increases in organochlorines after WL may exert influence on metabolism, as these compounds play a role on mitochondrial activity [48] and they seem to be an independent predictor of the REE [49]. In our study, AT seems to be subtle, highly variable between individuals, and possibly affected by the high variability seen in body weight responses to the intervention [2]. Also, when comparing people who lost at least 3% of their initial weight with those who did not, only approach A and C (C.1–C.4) showed differences between groups (p < 0.05). Nevertheless, all approaches showed significant values for AT for those who had a WL \(\ge \) 3%. Also, AT seems to be irrelevant for the other group, as only three approaches significant AT values.
As a consequence of the high variability among AT approaches, some important methodological questions emerge, specifically: (i) should studies regarding AT be compared independently of their methodology to assess AT? (ii) which approach to assess AT should be used as a standard approach?
Since there are several plausible mathematical approaches to determine AT, it is possible that each study may present the approach that better reflects the existence of AT, which can explain the inconsistent findings that have been questioned for long-term weight management [18,19,20,21,22, 50,51,52]. Also, the EB status of the participants when measurements are taken were not always considered, as most studies did not assure a neutral EB when assessing AT. Therefore, the variability in the degree of energy conservation among studies may be partially explained by the EB status at the time of the measurements. Therefore, studies with different methodologies to assess AT should not be compared. Also, the discrepancy among methodologies underscores the importance of standardizing the mathematical approach to assess AT. Predicting REE from organ/tissue masses tied to their specific metabolic rates seems to be the most accurate method [53]. However, only a few studies used this method due to the considerable time and cost associated [54,55,56]. Hayes et al. [37] suggested an alternative approach that extends the DXA method to a tissue-organ level, predicting REE through the sum of the energy production of tissue-organ components derived from DXA. However, so far, no paper regarding AT used this approach to predict REE. In our study, using this solution to predict REE led to higher REE values when compared with the other approaches (predictive equations based on our sample’s characteristics). Consequently, approaches that predicted REE through the DXA-REE solution revealed the highest AT values. Therefore, it seems that this methodology may not be suitable as an alternative to determine AT, as it may exacerbate the degree of energy conservation.
Alternatively, predicting REE through a predictive equation using the baseline outcomes from the studied population is widely used due to its simplicity [18, 23, 38, 50, 57]. Nevertheless, there are also several ways to compare measured and predicted REE (using equations) among studies (such as approaches B, C and D). However, it should be noted that approach C (AT (kcal/day) = [(\({}_{{\quad {\text{m}}}}^{{{\text{4mo}}}} {\text{REE}} - {}_{\quad p}^{{{\text{4mo}}}} {\text{REE}}\)) – (\({}_{\quad \quad m}^{{{\text{Baseline}}}} {\text{REE}} - {}_{\quad \quad p}^{{{\text{baseline}}}} {\text{REE)}}\)]) reduces the large discrepancy between data treatment regarding pREE (approaches 1–4). Thus, it seems that it can be considered the strongest approach regarding methodologies to assess AT. Also, it is known that the FFM’s impact on the REE differs after WL [58, 59]. It is recognized that after WL, anatomical and molecular changes on FFM occur. Recently, Müller et al. [60] studied the impact of these changes in FFM composition on AT. As a result, adjusting changes in REE for these anatomical and molecular changes in FFM lead to a decrease on the magnitude of AT [60]. Therefore, along with mathematical issues, AT should also be accounted for functional body components when assessing energy conservation.
Considering mathematical approaches, some recommendations to standardize AT assessment models have been recently addressed [61]. First, the created predictive equation should provide a good fit for the observations and use the baseline participants’ characteristics to derive the models. The use of equations developed for other populations should be avoided. Also, variables such as sex and age should be included when creating the equation as they have been shown to influence REE [62]. More important, residuals (i.e., differences between measured and predicted REE) should be calculated not only after WL but also at baseline and should be considered when assessing AT (approach C). If residuals are statistically different from zero at baseline, it means that participants have already a predicted REE different from the measured value that should be accounted when assessing AT.
Despite the limitations of each methodology, the magnitude of AT in our study was smaller than that observed from studies who reported higher WL (by diet-only or combined diet and exercise intervention) [63, 64]. Though, people who lost more weight were not necessarily those who had a larger degree of AT. In fact, changes in REE as a response to a caloric restriction are widely variable between-subjects [65], as some individuals lost weight and did not show a significant decrease in REE (spendthrift phenotype), while others showed greater decreases in REE (thrifty phenotype) [66]. Thus, the existence of these two different phenotypes may be the reason why some people were able to lose weight without any considerable decreases in any of the EE components. However, more studies should be conducted to understand why some people lose moderate weight and do not show a lower-than-expected decrease in REE.
Our AT values are consistent with those presented in other similar studies with smaller energy deficit [23, 39, 50, 54, 56, 67]. Thus, it is possible that AT appears not only after an aggressive energy restriction but also under a moderate energy deficit. Although AT values were statistically significant, its clinical significance needs to be taken into consideration. It is known that behavioral and metabolic compensations are interconnected, and AT may affect our eating behavior, and hence WL [53].
Although the current study reveals clear discrepancies between methods to assess AT some limitations should be addressed. First, it should be noted that there is no clear definition nor a criterion method for AT. Therefore, we cannot assure that a certain methodology is accurate as we do not have a “reference value” of AT to use when comparing methods of assessing AT. Also, we cannot assure that both at baseline and post-programme assessments of our participants occurred under an equal EB. As they were measured right after the intervention, they could still be attempting to lose weight and, consequently, be under a negative EB. Some studies that conducted a follow-up period after WL (where participants were weight stable) reported that AT disappeared over time [23, 50]. Thus, a weight maintenance period to maintain a stable weight would have strengthened the results. It is known that studies that follow up massive WL (“Biggest Loser” contestants) [68] showed that AT not only remains significant but also increased regardless of a substantial weight regain over time. However, in addition to methodological limitations, such as changes in instruments over the study timeline and the lack of control in diet and exercise prior to the final REE measurement [29], it is important to underscore that this type of intervention (intensive diet and exercise intervention to promote a massive WL) does not reflect the impact of moderate WL on AT. Therefore, their findings should not be extrapolated to other WL studies that assessed AT.
In conclusion, after a moderate WL, AT was present and differed between groups only for 2 out of the 13 used approaches. Therefore, the lack of standardization among methodologies leads to an uncertainty regarding AT’s existence. Moreover, the magnitude of AT differed significantly among methodologies to predict REE and to assess AT. Therefore, there is a need to standardize the AT assessment and comparison among studies with different methods should be carefully interpreted.
Availability of data and materials
Non applicable.
Code availability
Non applicable.
References
Edholm OG, Adam JM, Healy MJ, Wolff HS, Goldsmith R, Best TW (1970) Food intake and energy expenditure of army recruits. Br J Nutr 24(4):1091–1107. https://doi.org/10.1079/bjn19700112
Casanova N, Beaulieu K, Finlayson G, Hopkins M (2019) Metabolic adaptations during negative energy balance and their potential impact on appetite and food intake. Proc Nutr Soc 78(3):279–289. https://doi.org/10.1017/s0029665118002811
Melby CL, Paris HL, Foright RM, Peth J (2017) Attenuating the biologic drive for weight regain following weight loss: must what goes down always go back up? Nutrients. https://doi.org/10.3390/nu9050468
Ma C, Avenell A, Bolland M, Hudson J, Stewart F, Robertson C, Sharma P, Fraser C, MacLennan G (2017) Effects of weight loss interventions for adults who are obese on mortality, cardiovascular disease, and cancer: systematic review and meta-analysis. BMJ. https://doi.org/10.1136/bmj.j4849
Felix HC, West DS (2013) Effectiveness of weight loss interventions for obese older adults. Am J Health Promot AJHP 27(3):191–199. https://doi.org/10.4278/ajhp.110617-LIT-259
Gurevich-Panigrahi T, Panigrahi S, Wiechec E, Los M (2009) Obesity: pathophysiology and clinical management. Curr Med Chem 16(4):506–521. https://doi.org/10.2174/092986709787315568
Thomas DM, Bouchard C, Church T, Slentz C, Kraus WE, Redman LM, Martin CK, Silva AM, Vossen M, Westerterp K, Heymsfield SB (2012) Why do individuals not lose more weight from an exercise intervention at a defined dose? An energy balance analysis. Obes Rev 13(10):835–847. https://doi.org/10.1111/j.1467-789X.2012.01012.x
Levine JA, Eberhardt NL, Jensen MD (1999) Role of nonexercise activity thermogenesis in resistance to fat gain in humans. Science 283(5399):212–214
Hollstein T, Basolo A, Ando T, Krakoff J, Piaggi P (2021) Reduced adaptive thermogenesis during acute protein-imbalanced overfeeding is a metabolic hallmark of the human thrifty phenotype. Am J Clin Nutr. https://doi.org/10.1093/ajcn/nqab209
Gulick A (1995) A study of weight regulation in the adult human body during over-nutrition. Obes Res 3(5):501–512. https://doi.org/10.1002/j.1550-8528.1995.tb00182.x
Neumann RO (1902) Experimentelle beiträge zur lehre von dem täglichen nahrungsbedarf des menschen unter besonderer berück-sichtigung der notwendigen eiweissmenge
Rothwell NJ, Stock MJ (1983) Luxuskonsumption, diet-induced thermogenesis and brown fat: the case in favour. Clin Sci (Lond) 64(1):19–23. https://doi.org/10.1042/cs0640019
Hervey GR, Tobin G (1983) Luxuskonsumption, diet-induced thermogenesis and brown fat: a critical review. Clin Sci (Lond) 64(1):7–18. https://doi.org/10.1042/cs0640007
Leibel RL, Rosenbaum M, Hirsch J (1995) Changes in energy expenditure resulting from altered body weight. N Engl J Med 332(10):621–628. https://doi.org/10.1056/nejm199503093321001
Major GC, Doucet E, Trayhurn P, Astrup A, Tremblay A (2007) Clinical significance of adaptive thermogenesis. Int J Obes (Lond) 31(2):204–212. https://doi.org/10.1038/sj.ijo.0803523
Dulloo AG, Jacquet J, Montani JP, Schutz Y (2012) Adaptive thermogenesis in human body weight regulation: more of a concept than a measurable entity? Obes Rev 13(Suppl 2):105–121. https://doi.org/10.1111/j.1467-789X.2012.01041.x
Heinitz S, Hollstein T, Ando T, Walter M, Basolo A, Krakoff J, Votruba SB, Piaggi P (2020) Early adaptive thermogenesis is a determinant of weight loss after six weeks of caloric restriction in overweight subjects. Metabolism 110:154303. https://doi.org/10.1016/j.metabol.2020.154303
Gomez-Arbelaez D, Crujeiras AB, Castro AI, Martinez-Olmos MA, Canton A, Ordoñez-Mayan L, Sajoux I, Galban C, Bellido D, Casanueva FF (2018) Resting metabolic rate of obese patients under very low calorie ketogenic diet. Nutr Metab (Lond) 15:18. https://doi.org/10.1186/s12986-018-0249-z
Browning MG, Rabl C, Campos GM (2017) Blunting of adaptive thermogenesis as a potential additional mechanism to promote weight loss after gastric bypass. Surg Obes Relat Dis 13(4):669–673. https://doi.org/10.1016/j.soard.2016.11.016
Marlatt KL, Redman LM, Burton JH, Martin CK, Ravussin E (2017) Persistence of weight loss and acquired behaviors 2 year after stopping a 2-year calorie restriction intervention. Am J Clin Nutr 105(4):928–935. https://doi.org/10.3945/ajcn.116.146837
Novaes Ravelli M, Schoeller DA, Crisp AH, Shriver T, Ferriolli E, Ducatti C, Marques de Oliveira MR (2019) Influence of energy balance on the rate of weight loss throughout one year of Roux-en-Y gastric bypass: a doubly labeled water study. Obes Surg 29(10):3299–3308. https://doi.org/10.1007/s11695-019-03989-z
Wolfe BM, Schoeller DA, McCrady-Spitzer SK, Thomas DM, Sorenson CE, Levine JA (2018) Resting metabolic rate, total daily energy expenditure, and metabolic adaptation 6 months and 24 months after bariatric surgery. Obesity (Silver Spring) 26(5):862–868. https://doi.org/10.1002/oby.22138
Martins C, Gower BA, Hill JO, Hunter GR (2020) Metabolic adaptation is not a major barrier to weight-loss maintenance. Am J Clin Nutr. https://doi.org/10.1093/ajcn/nqaa086
Martins C, Roekenes J, Salamati S, Gower BA, Hunter GR (2020) Metabolic adaptation is an illusion, only present when participants are in negative energy balance. Am J Clin Nutr 112(5):1212–1218. https://doi.org/10.1093/ajcn/nqaa220
Bettini S, Bordigato E, Fabris R, Serra R, Dal Pra C, Belligoli A, Sanna M, Compagnin C, Foletto M, Prevedello L, Fioretto P, Vettor R, Busetto L (2018) Modifications of resting energy expenditure after sleeve gastrectomy. Obes Surg 28(8):2481–2486. https://doi.org/10.1007/s11695-018-3190-3
Tam CS, Rigas G, Heilbronn LK, Matisan T, Probst Y, Talbot M (2016) Energy adaptations persist 2 years after sleeve gastrectomy and gastric bypass. Obes Surg 26(2):459–463. https://doi.org/10.1007/s11695-015-1972-4
Carrasco F, Papapietro K, Csendes A, Salazar G, Echenique C, Lisboa C, Diaz E, Rojas J (2007) Changes in resting energy expenditure and body composition after weight loss following Roux-en-Y gastric bypass. Obes Surg 17(5):608–616. https://doi.org/10.1007/s11695-007-9117-z
Flatt JP (2007) Exaggerated claim about adaptive thermogenesis. Int J Obes (Lond) 31(10):1626. https://doi.org/10.1038/sj.ijo.0803641 (author reply 1627–1628)
Kuchnia A, Huizenga R, Frankenfield D, Matthie JR, Earthman CP (2016) Overstated metabolic adaptation after “the biggest loser” intervention. Obesity 24(10):2025–2025. https://doi.org/10.1002/oby.21638
Muller MJ, Bosy-Westphal A (2013) Adaptive thermogenesis with weight loss in humans. Obesity (Silver Spring) 21(2):218–228. https://doi.org/10.1002/oby.20027
Byrne NM, Sainsbury A, King NA, Hills AP, Wood RE (2018) Intermittent energy restriction improves weight loss efficiency in obese men: the MATADOR study. Int J Obes (Lond) 42(2):129–138. https://doi.org/10.1038/ijo.2017.206
Silva AM, Nunes CL, Matias CN, Jesus F, Francisco R, Cardoso M, Santos I, Carraça EV, Silva MN, Sardinha LB, Martins P, Minderico CS (2020) Champ4life study protocol: a one-year randomized controlled trial of a lifestyle intervention for inactive former elite athletes with overweight/obesity. Nutrients. https://doi.org/10.3390/nu12020286
American College of Sports M, Riebe D, Ehrman JK, Liguori G, Magal M (2018) ACSM's guidelines for exercise testing and prescription
Lewiecki EM, Binkley N, Morgan SL, Shuhart CR, Camargos BM, Carey JJ, Gordon CM, Jankowski LG, Lee JK, Leslie WD (2016) Best practices for dual-energy X-ray absorptiometry measurement and reporting: International Society for Clinical Densitometry Guidance. J Clin Densitom 19(2):127–140. https://doi.org/10.1016/j.jocd.2016.03.003
Compher C, Frankenfield D, Keim N, Roth-Yousey L (2006) Best practice methods to apply to measurement of resting metabolic rate in adults: a systematic review. J Am Diet Assoc 106(6):881–903. https://doi.org/10.1016/j.jada.2006.02.009
Weir JB (1949) New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol 109(1–2):1–9
Hayes M, Chustek M, Wang Z, Gallagher D, Heshka S, Spungen A, Bauman W, Heymsfield SB (2002) DXA: potential for creating a metabolic map of organ-tissue resting energy expenditure components. Obes Res 10(10):969–977. https://doi.org/10.1038/oby.2002.132
Thom G, Dombrowski SU, Brosnahan N, Algindan YY, Rosario Lopez-Gonzalez M, Roditi G, Lean MEJ, Malkova D (2020) The role of appetite-related hormones, adaptive thermogenesis, perceived hunger and stress in long-term weight-loss maintenance: a mixed-methods study. Eur J Clin Nutr 74(4):622–632. https://doi.org/10.1038/s41430-020-0568-9
Ten Haaf T, Verreijen AM, Memelink RG, Tieland M, Weijs PJM (2018) Reduction in energy expenditure during weight loss is higher than predicted based on fat free mass and fat mass in older adults. Clin Nutr 37(1):250–253. https://doi.org/10.1016/j.clnu.2016.12.014
Borges JH, Hunter GR, Silva AM, Cirolini VX, Langer RD, Páscoa MA, Guerra-Júnior G, Gonçalves EM (2019) Adaptive thermogenesis and changes in body composition and physical fitness in army cadets. J Sports Med Phys Fit 59(1):94–101. https://doi.org/10.23736/s0022-4707.17.08066-5
Silva AM, Matias CN, Santos DA, Thomas D, Bosy-Westphal A, MüLler MJ, Heymsfield SB, Sardinha LB (2017) Compensatory changes in energy balance regulation over one athletic season. Med Sci Sports Exerc 49(6):1229–1235. https://doi.org/10.1249/mss.0000000000001216
Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, Hu FB, Hubbard VS, Jakicic JM, Kushner RF, Loria CM, Millen BE, Nonas CA, Pi-Sunyer FX, Stevens J, Stevens VJ, Wadden TA, Wolfe BM, Yanovski SZ, Jordan HS, Kendall KA, Lux LJ, Mentor-Marcel R, Morgan LC, Trisolini MG, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC Jr, Tomaselli GF (2014) 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation 129(25 Suppl 2):S102-138. https://doi.org/10.1161/01.cir.0000437739.71477.ee
Silva AM, Nunes CL, Jesus F, Francisco R, Matias CN, Cardoso M, Santos I, Carraça EV, Finlayson G, Silva MN, Dickinson S, Allison D, Minderico CS, Martins P, Sardinha LB (2021) Effectiveness of a lifestyle weight-loss intervention targeting inactive former elite athletes: the Champ4Life randomised controlled trial. Br J Sports Med. https://doi.org/10.1136/bjsports-2021-104212
Maclean PS, Bergouignan A, Cornier MA, Jackman MR (2011) Biology’s response to dieting: the impetus for weight regain. Am J Physiol Regul Integr Comp Physiol 301(3):R581-600. https://doi.org/10.1152/ajpregu.00755.2010
Mars M, de Graaf C, de Groot LC, Kok FJ (2005) Decreases in fasting leptin and insulin concentrations after acute energy restriction and subsequent compensation in food intake. Am J Clin Nutr 81(3):570–577. https://doi.org/10.1093/ajcn/81.3.570
Mars M, de Graaf C, de Groot CP, van Rossum CT, Kok FJ (2006) Fasting leptin and appetite responses induced by a 4-day 65%-energy-restricted diet. Int J Obes (Lond) 30(1):122–128. https://doi.org/10.1038/sj.ijo.0803070
Tremblay A, Pelletier C, Doucet E, Imbeault P (2004) Thermogenesis and weight loss in obese individuals: a primary association with organochlorine pollution. Int J Obes Relat Metab Disord 28(7):936–939. https://doi.org/10.1038/sj.ijo.0802527
Pardini RS (1971) Polychlorinated biphenyls (PCB): effect on mitochondrial enzyme systems. Bull Environ Contam Toxicol 6(6):539–545. https://doi.org/10.1007/bf01796863
Pelletier C, Doucet E, Imbeault P, Tremblay A (2002) Associations between weight loss-induced changes in plasma organochlorine concentrations, serum T(3) concentration, and resting metabolic rate. Toxicol Sci 67(1):46–51. https://doi.org/10.1093/toxsci/67.1.46
Karl JP, Roberts SB, Schaefer EJ, Gleason JA, Fuss P, Rasmussen H, Saltzman E, Das SK (2015) Effects of carbohydrate quantity and glycemic index on resting metabolic rate and body composition during weight loss. Obesity (Silver Spring) 23(11):2190–2198. https://doi.org/10.1002/oby.21268
Pourhassan M, Bosy-Westphal A, Schautz B, Braun W, Glüer CC, Müller MJ (2014) Impact of body composition during weight change on resting energy expenditure and homeostasis model assessment index in overweight nonsmoking adults. Am J Clin Nutr 99(4):779–791. https://doi.org/10.3945/ajcn.113.071829
de Jonge L, Bray GA, Smith SR, Ryan DH, de Souza RJ, Loria CM, Champagne CM, Williamson DA, Sacks FM (2012) Effect of diet composition and weight loss on resting energy expenditure in the POUNDS LOST study. Obesity (Silver Spring) 20(12):2384–2389. https://doi.org/10.1038/oby.2012.127
Muller MJ, Enderle J, Bosy-Westphal A (2016) Changes in energy expenditure with weight gain and weight loss in humans. Curr Obes Rep 5(4):413–423. https://doi.org/10.1007/s13679-016-0237-4
Bosy-Westphal A, Kossel E, Goele K, Later W, Hitze B, Settler U, Heller M, Gluer CC, Heymsfield SB, Muller MJ (2009) Contribution of individual organ mass loss to weight loss-associated decline in resting energy expenditure. Am J Clin Nutr 90(4):993–1001. https://doi.org/10.3945/ajcn.2008.27402
Bosy-Westphal A, Schautz B, Lagerpusch M, Pourhassan M, Braun W, Goele K, Heller M, Glüer CC, Müller MJ (2013) Effect of weight loss and regain on adipose tissue distribution, composition of lean mass and resting energy expenditure in young overweight and obese adults. Int J Obes (Lond) 37(10):1371–1377. https://doi.org/10.1038/ijo.2013.1
Müller MJ, Enderle J, Pourhassan M, Braun W, Eggeling B, Lagerpusch M, Glüer CC, Kehayias JJ, Kiosz D, Bosy-Westphal A (2015) Metabolic adaptation to caloric restriction and subsequent refeeding: the Minnesota Starvation Experiment revisited. Am J Clin Nutr 102(4):807–819. https://doi.org/10.3945/ajcn.115.109173
Nymo S, Coutinho SR, Torgersen LH, Bomo OJ, Haugvaldstad I, Truby H, Kulseng B, Martins C (2018) Timeline of changes in adaptive physiological responses, at the level of energy expenditure, with progressive weight loss. Br J Nutr 120(2):141–149. https://doi.org/10.1017/s0007114518000922
Bosy-Westphal A, Müller MJ, Boschmann M, Klaus S, Kreymann G, Lührmann PM, Neuhäuser-Berthold M, Noack R, Pirke KM, Platte P, Selberg O, Steiniger J (2009) Grade of adiposity affects the impact of fat mass on resting energy expenditure in women. Br J Nutr 101(4):474–477. https://doi.org/10.1017/s0007114508020357
Bosy-Westphal A, Braun W, Schautz B, Müller MJ (2013) Issues in characterizing resting energy expenditure in obesity and after weight loss. Front Physiol 4:47. https://doi.org/10.3389/fphys.2013.00047
Müller MJ, Heymsfield SB, Bosy-Westphal A (2021) Are metabolic adaptations to weight changes an artefact? Am J Clin Nutr. https://doi.org/10.1093/ajcn/nqab184
Nunes CL, Casanova N, Francisco R, Bosy-Westphal A, Hopkins M, Sardinha LB, Silva AM (2021) Does Adaptive Thermogenesis occur after weight loss in adults? A systematic review. Br J Nutr. https://doi.org/10.1017/S0007114521001094
Johnstone AM, Murison SD, Duncan JS, Rance KA, Speakman JR (2005) Factors influencing variation in basal metabolic rate include fat-free mass, fat mass, age, and circulating thyroxine but not sex, circulating leptin, or triiodothyronine. Am J Clin Nutr 82(5):941–948. https://doi.org/10.1093/ajcn/82.5.941
Rosenbaum M, Leibel RL (2016) Models of energy homeostasis in response to maintenance of reduced body weight. Obesity (Silver Spring) 24(8):1620–1629. https://doi.org/10.1002/oby.21559
Johannsen DL, Knuth ND, Huizenga R, Rood JC, Ravussin E, Hall KD (2012) Metabolic slowing with massive weight loss despite preservation of fat-free mass. J Clin Endocrinol Metab 97(7):2489–2496. https://doi.org/10.1210/jc.2012-1444
Müller MJ (2019) About “spendthrift” and “thrifty” phenotypes: resistance and susceptibility to overeating revisited. Am J Clin Nutr 110(3):542–543. https://doi.org/10.1093/ajcn/nqz090
Piaggi P, Vinales KL, Basolo A, Santini F, Krakoff J (2018) Energy expenditure in the etiology of human obesity: spendthrift and thrifty metabolic phenotypes and energy-sensing mechanisms. J Endocrinol Invest 41(1):83–89. https://doi.org/10.1007/s40618-017-0732-9
McNeil J, Schwartz A, Rabasa-Lhoret R, Lavoie JM, Brochu M, Doucet É (2015) Changes in leptin and peptide YY do not explain the greater-than-predicted decreases in resting energy expenditure after weight loss. J Clin Endocrinol Metab 100(3):E443-452. https://doi.org/10.1210/jc.2014-2210
Fothergill E, Guo J, Howard L, Kerns JC, Knuth ND, Brychta R, Chen KY, Skarulis MC, Walter M, Walter PJ, Hall KD (2016) Persistent metabolic adaptation 6 years after “The Biggest Loser” competition. Obesity (Silver Spring) 24(8):1612–1619. https://doi.org/10.1002/oby.21538
Funding
Financial support was provided by the Portuguese Institute of Sports and Youth and by the International Olympic Committee, under the Olympic Solidarity Promotion of the Olympic Values Unit (Sports Medicine and Protection of Clean Athletes Programme). The current work was also supported by national funding from the Portuguese Foundation for Science and Technology within the R&D units UIDB/00447/2020. C.L.N. and R.F. were supported with a Ph.D. scholarship from the Portuguese Foundation for Science and Technology (SFRH/BD/143725/2019 and 2020.05397.BD, respectively).
Author information
Authors and Affiliations
Contributions
CLN: conceptualization, methodology, data curation, data analysis, and writing the original draft. CNM, FJ, and RF: data curation, reviewing, and editing. MH: data analysis, reviewing, and editing. SBH, AB-W, LBS, PM, and CSM: reviewing and editing. AMS: conceptualization, methodology, supervision, reviewing, and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors reported no conflicts of interest.
Ethics approval
The Ethics Committee of the Faculty of Human Kinetics, University of Lisbon (Lisbon, Portugal), approved the study (CEFMH Approval Number: 16/2016).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
The authors affirm that human research participants provided informed consent for publication.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nunes, C.L., Jesus, F., Francisco, R. et al. Adaptive thermogenesis after moderate weight loss: magnitude and methodological issues. Eur J Nutr 61, 1405–1416 (2022). https://doi.org/10.1007/s00394-021-02742-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-021-02742-6