Abstract
Purpose
Phytosterols reduce intestinal cholesterol absorption and help to lower LDL-cholesterol. Many Chinese adults are lactose-intolerant and cannot tolerate bovine milk enriched with phytosterol. Soya-milk is a common beverage in Asia and it has beneficial effects on general health. We therefore conducted a randomized double-blind controlled trial to assess the effectiveness of a phytosterols-enriched soya drink in lowering serum LDL-cholesterol level (primary outcome) and other cardiovascular parameters (secondary outcomes).
Methods
One hundred and fifty-nine normocholesterolaemic participants (85 men and 74 women; aged 19–79) were randomized to daily intake of one serving of phytosterols-enriched soya drink (N = 82), equivalent to 2 g of phytosterol per day, or a matched soya drink without phytosterols (N = 77) for 3 weeks. Adverse events, withdrawal and compliance were documented.
Results
Among the treatment group (N = 82), phytosterols-enriched soya drink significantly decreased LDL-cholesterol by 5.96% (SE 1.48, 95% CI − 8.91%, − 3.00%) with a median of 6.74% compared with baseline, resulting in a significant reduction of 4.70% (95% CI − 8.89%, − 0.51%; p = 0.028) with a median of 5.20% compared with placebo (N = 77). In contrast, there were no significant changes in other lipid parameters, blood glucose, blood pressure, body weight or waist circumference. Remarkably, 95% of the participants randomized to the fortified drink reported no adverse events at all.
Conclusions
Daily consumption of a phytosterols-enriched soya drink may be a simple and cost-neutral means of lowering LDL-cholesterol in individuals in China, with massive population and rising incidence of coronary heart disease (ClinicalTrials.gov identifier: NCT02881658; date of registration: 14 Aug 2016).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Elevated serum low-density lipoprotein cholesterol (LDL-C) level is the major modifiable risk factor of cardiovascular diseases [1]. It is well-documented that reducing LDL-C with pharmacological agents, such as statins, prevents cardiovascular events [2]. Although statins are widely used for treating hypercholesterolemia, concerns about their safety and adverse effects have led to discontinuation and non-compliance of the drug [3]. Thus, there is a need to develop non-pharmacological ways of reducing LDL-C.
Phytosterols, or plant sterols, are found naturally in plants and plant-based foods such as soybean, nuts and seeds. They are structurally similar to cholesterol but cannot be absorbed in the human gut; they thus compete with cholesterol for intestinal absorption and enhance cholesterol excretion. Phytosterols may also affect whole-body cholesterol metabolism, and thereby lower blood cholesterol level [4]. The role of phytosterols in reducing serum levels of LDL-C is recognized by regulatory authorities in EU, US, Canada, and Australia/New Zealand [5]. The FDA Health Claims state that “Foods containing at least 0.65 g per serving of vegetable oil plant sterol esters, eaten twice a day with meals for a daily total intake of at least 1.3 g, as part of a diet low in saturated fat and cholesterol, may reduce the risk of heart disease” [6]. Currently, various food products have been fortified with phytosterols. The food matrix and fat content affect the effectiveness of LDL-C reduction. When the same amount of phytosterols is consumed in low-fat milk, greater reduction of LDL-C was observed compared with that consumed in bread or cereal [7]. Whereas, another study showed a similar effect on lipid reduction in low- and medium-fat soymilk fortified with phytosterols [8].
Adding phytosterols to dairy products is the most common approach in commercial products and their effectiveness in lowering LDL-C has been shown in clinical trials [9]. Our previous randomized controlled trial (RCT) showed that drinking phytosterols-enriched milk twice a day lowered LDL-C in Hong Kong Chinese [10]. However, it is well documented that lactose intolerance is prevalent in Asians [11]. Thus, soya milk, a popular beverage in Asia [12], may serve as a better food matrix for phytosterols. Soya milk is a protein-rich drink and regular intake is considered as part of a healthy diet. It has potential benefits in relieving hot flushes [13] and improving lipid profiles [14]. Long-term intake of isoflavones from soya milk has bone-sparing effects [12]. However, whether phytosterols-enriched soya milk is useful in lowering LDL-C is largely unknown. In particular, the effects of 2 g-phytosterol formulation taken once daily in people with normocholesterolemia has not been previously tested. We therefore conducted a double-blind RCT to evaluate whether taking phytosterols-enriched soya drink once daily would reduce LDL-C in normocholesterolemic Chinese.
Methods
The study design was a randomized, double-blind, single-center, two-arm, placebo-controlled trial. The trial was conducted in a University setting, and in accordance with the Good Clinical Practice (GCP) Guideline issued by The International Council for Harmonisation (ICH) [15]. The study protocol was approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (HKU/HA HKW IRB). All participants gave written informed consent. The trial was registered at clinicaltrials.gov on 14 Aug 2016 and was assigned the number NCT02881658.
Participants were healthy Chinese male or female aged 18 or above recruited from the community, with appropriate literacy to understand and ability to comply with the study requirements. After receiving all demographic information, medical and medication history of the participants at their baseline visit, those who met any of the following criteria were excluded: high blood cholesterol, LDL-C and familial hypercholesterolemia; on regular medications of known interference with lipid profiles (e.g. hormone replacement treatment, diuretics, beta-blockers, statins or other lipid-lowering drug treatment) or over-the-counter supplements that claim to reduce blood cholesterol or gastrointestinal (GI) related medications (e.g. antacid); smoking > 1 pack/day; heavy alcohol intake (> 40 g/day for men; > 30 g/day for women); intolerance or dislike of soya products; known soy allergy; history of sitosterolaemia; history of other major chronic diseases such as diabetes (type I or type II), thyroid, renal or liver disease or any GI malabsorption syndrome; refusal to stop consuming phytosterols-enriched products other than the product under investigation, if any, during the study; receiving systemic treatment or topical treatment likely to interfere with the evaluation of the study parameters; pregnancy or lactation during the study period.
Each participant was randomly assigned to either placebo or treatment group, given packs of soya drink containing phytosterols at a daily dose of either 0 g or 2 g, respectively, for a period of 3 weeks in a double-blind manner. The randomization was handled by the Data Management and Medical Statistics Unit of the Clinical Trials Centre, The University of Hong Kong. Prior to the start of the study, the randomized specifications were defined and the randomization codes were generated online using a web-based randomization system, namely a randomization module within Research Electronic Data Capture (REDCap), which is a secure web application developed by Vanderbilt University, for building and managing online surveys and databases. Block randomization was used to balance the study groups in terms of participant numbers, sex and age group (18–40 years and > 40 years). Block randomization of sizes 2, 4 or 6 with equal probability were used to maintain approximately 1:1 allocation of treatment within the four stratum: (1) male aged 18–40 years; (2) male aged > 40 years; (3) female aged 18–40 years and (4) female aged > 40 years. Both investigators and participants were completely blinded to treatment allocation throughout the study.
Demographic information, medical and medication history
During the baseline visit, the participant’s demographic information, medical and medication history were obtained. Medical history included past and current illnesses, alcohol and tobacco use, dietary and exercise habits, and pregnancy status if applicable. Information on prescription, over-the-counter and herbal medications as well as health supplements within 3 months were recorded.
Study product and intervention
The product used was based on a commercially-available soya drink (Vitasoy Calci-Plus Hi-calcium Plant Sterol Soya Milk provided by Vitasoy International Holdings Ltd.). Participants in the treatment and placebo group were given packs of 250 mL soya drinks with identical appearances. The 250 mL soya drinks for the treatment group contained 2 g phytosterols while that for the placebo group were not fortified. The nutrient profiles of two drinks were the same except higher total fat in phytosterols-enriched soya drink (2.8 g/100 mL) compared with the placebo (1.2 g/100 mL) (Supplementary Table 1). In preliminary blind tasting, the drink for the placebo group was found to be well-matched and indistinguishable from that for the treatment group. According to EU commission regulation, “a daily intake of 1.5–2.4 g/s plant sterols or stanols reduces LDL-C by 7–10% in 2–3 weeks” [16]. Thus, the current study was designed to evaluate the effectiveness of lipid–lowering effect by a phytosterols-enriched soya drink for 3 weeks. Participants were asked to consume one pack of 250 mL soya drink daily during their main meal for three consecutive weeks. Both groups were advised to maintain their usual dietary and exercise habits during the study period.
Study compliance
The study product was given to the subject during their baseline visit. At the end of the study, participants were requested to return unused packs and a card that recorded product consumption so that compliance could be assessed.
Physical and laboratory assessments
At the start date and end date of the study, the height, weight, waist and hip circumference, body temperature and blood pressure of study participants were measured. Blood pressure was measured using a GE CARESCAPE V100 (Fairfield, CT) automated blood pressure monitor. Waist and hip circumference were measured at the midpoint between the lowest rib and the iliac crest, and at the widest part of the hip, respectively, in a horizontal plane. Fasting blood samples at the two visits were taken to measure serum LDL-C, HDL-C, total cholesterol, triglycerides, creatinine, and blood glucose by the Ortho-Vitros Fusion 5.1 automated analyzer.
Statistical analysis
PASS 12 was used to calculate the sample size of this study. ANCOVA was used to estimate the sample size with baseline serum LDL-C level as the independent covariate, assuming a power of 0.8 according to a previous study [17], an attrition rate of 25% and a maximum tolerable false-positive rate of 5%.
Results were expressed as mean and standard deviation for continuous variables, and as number and percentage for categorical variables. The primary objective of the current study was to compare the changes in serum LDL-C level at the end of week 3 between the groups. ANCOVA was used to evaluate the least square (LS) mean differences and % changes with age, sex, baseline BMI and baseline LDL-C value as covariates. Efficacy analysis was performed on both intention-to-treat (ITT) and the per-protocol (PP) population. ITT consisted of all cases that had been randomized. PP included all eligible participants who had 80% compliance with the study product, efficacy data collected within the pre-specified allowable visit window, and no significant violation against the protocol.
The secondary objective of this study was to compare the changes in other cardiometabolic risk factors (including blood pressure, BMI, waist and hip circumferences, serum HDL-C, total cholesterol, triglycerides, and fasting glucose) between the treatment and placebo groups. The secondary efficacy analysis was performed on the ITT population. Subgroup analyses were performed to compare LS mean difference in primary and secondary endpoints between groups in the PP population; and changes in serum lipid profile of subjects in ITT population stratified by baseline LDL-C level between groups. All data management and statistical analysis were performed with SAS®.
Results
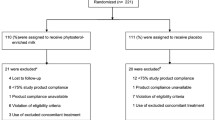
A total of 201 subjects were recruited (100 in the treatment group and 101 in the placebo group) in July 2016 and all final visits were completed in January 2017 (Fig. 1). Seven participants did not return for the final visit, one withdrew from the study and six were lost to follow-up. Sixteen and 19 participants from treatment and placebo groups respectively were removed from further analysis because they met the exclusion criteria or had an undetermined baseline LDL-C level (Supplementary Table 3). The baseline characteristics of participants are shown in Table 1.
Finally, 159 participants (82 treatment; 77 placebo) were included in the ITT analysis. The mean compliance rate was 97.9% (range 76.2–100%) in the treatment group and 97.7% (range 76.2–100%) in the placebo group. The treatment group had a reduction in serum LDL-C by LS mean 0.12 mmol/L (SE 0.058) (Table 2) when compared with the placebo group after adjusted for baseline LDL-C. Among the treatment group, LDL-C decreased from 2.80 mmol/L (SE 0.08) to 2.62 mmol/L (SE, 0.08) over the 3-week study period, representing a significant decrease by 5.96% (SE 1.48) with a median of 6.74%. Meanwhile, the placebo group had a reduction in LDL-C from 2.69 mmol/L (SE 0.08) to 2.64 mmol/L (SE 0.09) across the study period, representing an insignificant decrease by 1.25% (SE 1.51) with a median of 1.54%. There was a difference of 4.70% (SE 2.12) with a median of 5.20% between treatment and placebo groups. Similar results were found in the PP population (Supplementary Table 4). As there was no significant interaction with sex (p = 0.76), the analysis was not stratified by sex. No significant differences were found between groups with respect to changes in blood pressure, weight, BMI, waist circumference, hip circumference, serum creatinine, HDL-C, triglycerides, or fasting glucose levels (Table 2).
Adverse events are shown in Table 3. Only 5 (3.1%) out of all 159 study participants reported adverse events. The adverse events were nearly all gastrointestinal discomfort without any serious adverse events and did not result in withdrawal.
Discussion
In this randomized, double-blind controlled trial, a phytosterols-enriched soya drink, with 2 g of phytosterols per day, was shown conclusively to lower LDL-C level, with only 3.1% participants reporting adverse events related to GI discomfort.
This cholesterol-lowering effect of the phytosterols-enriched soya drink is consistent with previous studies, many of which involved Caucasians consuming dairy-type products, with a reported LDL-lowering effects ranging from 6 to 12% [18]. Our previous RCT using phytosterols-enriched milk powder showed similar LDL-C lowering effect among Chinese adults, but more participants (around 30%) experienced adverse events such as diarrhea and flatulence when consuming milk products [10]. In contrast, there is a long tradition of taking soya drinks in Asian countries, such as China, Japan, Korea, Thailand, Malaysia and Singapore, because soya milk is well-tolerated. As shown in the current study, the compliance rate was close to 100%. The number of adverse events was strikingly low.
Components other than phytosterols in soya milk may offer additional benefits. The LDL-C was also lowered in the placebo group, although the reduction did not reach statistical significant (mean change − 0.05 mmol/L, 95% CI − 0.13, 0.03). Such beneficial effect may be contributed by other nutrients such as soy protein [19] and isoflavones [20]. In addition, soy product has been reported to exert multiple beneficial effects, such as alleviating hot flushes, reducing risk of coronary heart disease, breast and prostate cancer [21]. Notably, the total LDL-C reduction in the treatment group was 5.96% (median 6.74%), with the mean reduction as compared with the placebo group at 4.70% (median 5.20%). This demonstrated that consuming phytosterols-enriched soya drink lowered LDL-C by a greater extent than the standard soya drink. Although a greater reduction of LDL-C was shown among people with higher serum cholesterol at baseline in a previous study [21], there were no significant differences in LDL-C, HDL-C, total cholesterol, and triglycerides level in our subgroup analysis stratified by baseline LDL-C level (Supplementary Table 5). Phytosterols are fortified in food with stanol esters, sterol esters, or free (unesterified) plant sterols and stanols. Their particle size and the fatty acid used for esterification affect the cholesterol-lowering property due to the bioavailability and efficacy in competing with intestinal cholesterol absorption [9]. Therefore, the formulation of phytosterols has an important bearing on the effectiveness of cholesterol lowering effect. The phytosterols included in the fortified soya drink are mainly sterol esters (> 90%), therefore these components are likely to account for the treatment effect. Meanwhile, the free sterols included are mainly β-sitosterol, campesterol, and stigmasterol (Supplementary Table 2). Our study might lack the specificity to determine which phytosterols are responsible for the reduction of LDL-C, but evidence demonstrates no conclusive difference in lipid-lowering effect between free and esterified plant sterols [4]. Nevertheless, there are factors affecting lipid profile other than phytosterol and soy intake, such as diet and lifestyle. Participants were therefore advised not to change their diet and lifestyle during the study period. In an intervention period lasting only a few weeks, these factors are unlikely to change significantly.
Lowering LDL-C may have additional benefits beyond simply reducing cardiovascular risk. There are substantial studies showing that high serum cholesterol and LDL-C levels are correlated with reduced bone mineral density (BMD) and consequent increased risk of osteoporotic fracture [22]. Similarly, it has also been reported that high serum cholesterol is associated with tumour development and progression, including cancers of breast, prostate and colon [23]. Thus, lowering LDL-C may have a great impact on general health. Although statins are the first-line drugs to lower LDL-C level, there are disadvantages in using these pharmacological interventions. Statins are known to cause myositis and liver enzyme elevations, and increase the risk of developing diabetes [24]. Evolocumab, an antibody that binds specifically to proprotein convertase subtilisin kexin 9 (PCSK9), blocks PCSK9-mediated degradation of low-density lipoprotein receptors in the liver and effectively increases the clearance of LDL-C. However, the drug is expensive, exceeds generally accepted cost-effectiveness thresholds, and has potential risk of causing injection site reaction, allergic reaction and muscle-related events [25, 26]. In contrast, non-pharmaceutical management such as phytosterols are well-tolerated and serious adverse effects are almost absent [27]. Phytosterols are therefore suitable for those at low cardiovascular risk and have no or only mild elevation in LDL-C. In patients already taking statins, phytosterols still have an additive role in lowering LDL-C [28]. From the public health perspective, fortified food with potential health benefits, such as phytosterols-enriched drinks, are generally more acceptable to the public and hence has greater public health impact.
This study has several strengths and clinical implications. It is worth noting that we studied normocholesterolaemic adults of both sexes, with a wide age range (from 19 to 79 years). This is the first study to investigate if phytosterol is useful in reducing LDL-C among Chinese individuals with normocholesterolaemia, while previous studies mainly examined the effects of phytosterols in individuals with hyperlipidemia. In reality, people with hypercholesterolemia may be prescribed pharmacological intervention like statins, which is more efficacious in lowering LDL-C level. The importance of phytosterols-enriched food lies in preventing the rise in cholesterol and retarding the development of atherosclerosis in an early stage in asymptomatic individuals. Moreover, our participants are typical of the general population and differ from the high-risk older patients in most lipid lowering trials, thus our findings are generalizable to the whole population. The high tolerability, low toxicity and low antigenicity of phytosterols make them ideal for primary prevention in the general population, except for people with sitosterolaemia. In addition, the parallel design adopted in this study is more advantageous than the cross-over design commonly employed in pharmacokinetic and pharmacodynamics studies. Unlike the cross-over design, participants in the present study do not require a wash-out period between receiving treatment and placebo, resulting in shorter completion time and lowering the chance of dropout. Carry-over effect of phytosterols between treatment and placebo can be avoided using the parallel design. Based on FDA’s suggestion, the formulation of consuming one serving a day is more convenient than consuming twice daily [6]. The use of soya milk as a phytosterols-enriched beverage provides an alternative to people with lactose intolerance, which is not only prevalent in Asia, but also present in other regions. Soya milk per se may offer additional health benefits.
Nevertheless, there are limitations. Firstly, study participants are usually more motivated and have better compliance with regular consumption of the product than the general population. Moreover, compliance may decrease with time in reality. Secondly, as the trial was not conducted in an inpatient setting, the diet of the participants during the trial period could not be strictly controlled, especially when phytosterols are naturally present in many foods. However, the amount of phytosterol in typical food items is extremely low. Thirdly, we did not measure plasma phytosterols or lathosterol levels to document their changes during the trial. Phytosterols work mainly at a local level in the gut and so plasma levels may not directly reflect their efficacy. Moreover, it is not a standard practice to measure participants’ plasma levels in clinical trials of efficacy of investigational products.
In conclusion, daily intake of phytosterols-enriched soya drink with 2 g phytosterols is an effective way to reduce LDL-C and is well-tolerated in Chinese. If this highly accepted and inexpensive way of lowering LDL-C level is implemented on a nationwide scale, a consequent slight decrease in LDL-C at the population level would be expected to have a highly positive impact on cardiovascular disease and general health.
References
Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L (2004) Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case–control study. Lancet 364(9438):937–952. https://doi.org/10.1016/S0140-6736(04)17018-9
Cholesterol Treatment Trialists Collaborators (2012) The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet 380(9841):581–590. https://doi.org/10.1016/S0140-6736(12)60367-5
Davies JT, Delfino SF, Feinberg CE, Johnson MF, Nappi VL, Olinger JT, Schwab AP, Swanson HI (2016) Current and emerging uses of statins in clinical therapeutics: a review. Lipid Insights 9:13–29. https://doi.org/10.4137/LPI.S37450
Jones PJH, Shamloo M, MacKay DS, Rideout TC, Myrie SB, Plat J, Roullet JB, Baer DJ, Calkins KL, Davis HR, Barton Duell P, Ginsberg H, Gylling H, Jenkins D, Lutjohann D, Moghadasian M, Moreau RA, Mymin D, Ostlund RE Jr, Ras RT, Ochoa Reparaz J, Trautwein EA, Turley S, Vanmierlo T, Weingartner O (2018) Progress and perspectives in plant sterol and plant stanol research. Nutr Rev 76(10):725–746. https://doi.org/10.1093/nutrit/nuy032
Jew S, Antoine J, Bourlioux P, Milner J, Tapsell LC, Yang Y, Jones PJH (2015) Nutrient essentiality revisited. J Funct Foods 14:203–209. https://doi.org/10.1016/j.jff.2015.01.024
United States FDA (2018) Health claims: plant sterol/stanol esters and risk of coronary heart disease (CHD), 21 C.F.R. §101.83. https://www.ecfr.gov/cgi-bin/ECFR?SID=9597fbb69b17673c3588a74ae48fd0e2. Accessed 13 July 2018
Clifton PM, Noakes M, Sullivan D, Erichsen N, Ross D, Annison G, Fassoulakis A, Cehun M, Nestel P (2004) Cholesterol-lowering effects of plant sterol esters differ in milk, yoghurt, bread and cereal. Eur J Clin Nutr 58(3):503–509. https://doi.org/10.1038/sj.ejcn.1601837
Rideout TC, Chan YM, Harding SV, Jones PJ (2009) Low and moderate-fat plant sterol fortified soymilk in modulation of plasma lipids and cholesterol kinetics in subjects with normal to high cholesterol concentrations: report on two randomized crossover studies. Lipids Health Dis 8:45. https://doi.org/10.1186/1476-511X-8-45
Abumweis SS, Barake R, Jones PJ (2008) Plant sterols/stanols as cholesterol lowering agents: a meta-analysis of randomized controlled trials. Food Nutr Res. https://doi.org/10.3402/fnr.v52i0.1811
Cheung CL, Ho DK, Sing CW, Tsoi MF, Cheng VK, Lee GK, Ho YN, Cheung BM (2017) Randomized controlled trial of the effect of phytosterols-enriched low-fat milk on lipid profile in Chinese. Sci Rep 7:41084. https://doi.org/10.1038/srep41084
Solomons NW (2002) Fermentation, fermented foods and lactose intolerance. Eur J Clin Nutr 56(Suppl 4):S50–S55. https://doi.org/10.1038/sj.ejcn.1601663
Rizzo G, Baroni L (2018) Soy, soy foods and their role in vegetarian diets. Nutrients. https://doi.org/10.3390/nu10010043
Taku K, Melby MK, Kronenberg F, Kurzer MS, Messina M (2012) Extracted or synthesized soybean isoflavones reduce menopausal hot flash frequency and severity: systematic review and meta-analysis of randomized controlled trials. Menopause 19(7):776–790. https://doi.org/10.1097/gme.0b013e3182410159
Clarkson TB (2002) Soy, soy phytoestrogens and cardiovascular disease. J Nutr 132(3):566S–569S. https://doi.org/10.1093/jn/132.3.566S
ICH (2016) Integrated addendum to ICH E6(R1): guideline for good clinical practice E6(E2). https://www.ich.org/products/guidelines/efficacy/efficacy-single/article/integrated-addendum-good-clinical-practice.html. Accessed 01 May 2019
Amending Regulations (EC) No 983/2009 and (EU) No 384/2010 as regards the conditions of use of certain health claims related to the lowering effect of plant sterols and plant stanols on blood LDL-cholesterol Text with EEA relevance (2014). https://eur-lex.europa.eu/eli/reg/2014/686/oj. Accessed 01 May 2019
Thomsen AB, Hansen HB, Christiansen C, Green H, Berger A (2004) Effect of free plant sterols in low-fat milk on serum lipid profile in hypercholesterolemic subjects. Eur J Clin Nutr 58(6):860–870. https://doi.org/10.1038/sj.ejcn.1601887
Ras RT, Geleijnse JM, Trautwein EA (2014) LDL-cholesterol-lowering effect of plant sterols and stanols across different dose ranges: a meta-analysis of randomised controlled studies. Br J Nutr 112(2):214–219. https://doi.org/10.1017/S0007114514000750
Ramdath DD, Padhi EM, Sarfaraz S, Renwick S, Duncan AM (2017) Beyond the cholesterol-lowering effect of soy protein: a review of the effects of dietary soy and its constituents on risk factors for cardiovascular disease. Nutrients. https://doi.org/10.3390/nu9040324
Taku K, Umegaki K, Sato Y, Taki Y, Endoh K, Watanabe S (2007) Soy isoflavones lower serum total and LDL cholesterol in humans: a meta-analysis of 11 randomized controlled trials. Am J Clin Nutr 85(4):1148–1156. https://doi.org/10.1093/ajcn/85.4.1148
Messina M (2016) Soy and health update: evaluation of the clinical and epidemiologic literature. Nutrients. https://doi.org/10.3390/nu8120754
Mandal CC (2015) High cholesterol deteriorates bone health: new insights into molecular mechanisms. Front Endocrinol 6:165. https://doi.org/10.3389/fendo.2015.00165
Murai T (2015) Cholesterol lowering: role in cancer prevention and treatment. Biol Chem 396(1):1–11. https://doi.org/10.1515/hsz-2014-0194
Sattar N, Preiss D, Murray HM, Welsh P, Buckley BM, de Craen AJ, Seshasai SR, McMurray JJ, Freeman DJ, Jukema JW, Macfarlane PW, Packard CJ, Stott DJ, Westendorp RG, Shepherd J, Davis BR, Pressel SL, Marchioli R, Marfisi RM, Maggioni AP, Tavazzi L, Tognoni G, Kjekshus J, Pedersen TR, Cook TJ, Gotto AM, Clearfield MB, Downs JR, Nakamura H, Ohashi Y, Mizuno K, Ray KK, Ford I (2010) Statins and risk of incident diabetes: a collaborative meta-analysis of randomised statin trials. Lancet 375(9716):735–742. https://doi.org/10.1016/S0140-6736(09)61965-6
Sabatine MS, Giugliano RP, Keech AC, Honarpour N, Wiviott SD, Murphy SA, Kuder JF, Wang H, Liu T, Wasserman SM, Sever PS, Pedersen TR (2017) Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med 376(18):1713–1722. https://doi.org/10.1056/NEJMoa1615664
Fonarow GC, Keech AC, Pedersen TR, Giugliano RP, Sever PS, Lindgren P, van Hout B, Villa G, Qian Y, Somaratne R, Sabatine MS (2017) Cost-effectiveness of evolocumab therapy for reducing cardiovascular events in patients with atherosclerotic cardiovascular disease. JAMA Cardiol 2(10):1069–1078. https://doi.org/10.1001/jamacardio.2017.2762
QuIlez J, GarcIa-Lorda P, Salas-Salvado J (2003) Potential uses and benefits of phytosterols in diet: present situation and future directions. Clin Nutr 22(4):343–351. https://doi.org/10.1016/S0261-5614(03)00060-8
Han S, Jiao J, Xu J, Zimmermann D, Actis-Goretta L, Guan L, Zhao Y, Qin L (2016) Effects of plant stanol or sterol-enriched diets on lipid profiles in patients treated with statins: systematic review and meta-analysis. Sci Rep 6:31337. https://doi.org/10.1038/srep31337
Author information
Authors and Affiliations
Contributions
BMYC and CLC designed the study, interpreted the data and wrote the first draft. YPC, YCC, CWS, MFT, VKFC, GKYL were involved in subject enrollment, subject interview and performing physical assessments, BMYC and CLC supervised the whole RCT. All authors have read and approved the final version of the manuscript and its conclusions. The corresponding authors had full access to the data and had final responsibility for the decision to submit for publication.
Corresponding authors
Ethics declarations
Conflict of interest
Yes, there is potential competing interest. All authors declare: grants from The University of Hong Kong, sponsorship from Vitasoy International Holdings Ltd. for the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chau, YP., Cheng, YC., Sing, CW. et al. The lipid-lowering effect of once-daily soya drink fortified with phytosterols in normocholesterolaemic Chinese: a double-blind randomized controlled trial. Eur J Nutr 59, 2739–2746 (2020). https://doi.org/10.1007/s00394-019-02119-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-019-02119-w