Abstract
Purpose
The present study aimed to investigate the molecular mechanisms underlying the anticancer properties of ginger extract (GE) in mice bearing solid Ehrlich carcinoma (SEC) and to evaluate the use of GE in combination with doxorubicin (DOX) as a complementary therapy against SEC.
Methods
SEC was induced in 60 female mice. Mice were divided into four equal groups: SEC, GE, DOX and GE + DOX. GE (100 mg/kg orally day after day) and DOX (4 mg/kg i.p. for 4 cycles every 5 days) were given to mice starting on day 12 of inoculation. On the 28th day, blood samples were collected, mice were scarified, tumor volume was measured, and tumor tissues were excised.
Results
The anti-cancer effect of GE was mediated by activation of adenosine monophosphate protein kinase (AMPK) and down-regulation of cyclin D1 gene expression. GE also showed pro-apoptotic properties as evidenced by elevation of the P53 and suppression of nuclear factor-kappa B (NF-κB) content in tumor tissue. Co-administration of GE alongside DOX markedly increased survival rate, decreased tumor volume, and increased the level of phosphorylated AMPK (PAMPK) and improved related pathways compared to DOX group. In addition, the histopathological results demonstrated enhanced apoptosis and absence of multinucleated cells in tumor tissue of GE + DOX group.
Conclusion
AMPK pathway and cyclin D1 gene expression could be a molecular therapeutic target for the anticancer effect of GE in mice bearing SEC. Combining GE and DOX revealed a greater efficacy as anticancer therapeutic regimen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is one of the most prevalent cancers with a high mortality rate all over the world [1]. Severe cardiotoxicity is a major drawback in doxorubicin (DOX) treatment for breast cancer due to its oxidative stress action. Therefore, it is preferred to combine DOX with other compounds as a complementary therapy to antagonize or neutralize its prominent side effects [2].
The use of complementary and alternative medicine has been growing alongside conventional medical treatments. Complementary therapy is widely used as an aid for management of several diseases such as depression [3], arthritis [4], asthma [5] and cancer [6]. Natural products and herbal medicine have been used for treatment of various diseases and have exhibited anticancer activities [7].
Ginger (Zingiber officinale), belonging to family Zingiberaceae, has been cultivated for thousands of years as a spice and for medicinal purposes [8]. The biologically active constituents of ginger are gingerols, shogaols, paradols and zingerone [8]. Ginger possesses antioxidant [9], anti-inflammatory [10], antidiabetic [11] and anticancer activities [1]. Ginger has anti-tumorigenic effect both in vivo and in vitro in different cancer types [12, 13]. Ginger exhibits anti-cancer effect through the expression of activating transcription factor 3 in human colorectal cancer cells [14]. In addition, the crude ethanolic extract of ginger indicates promising anticancer activity against cholangiocarcinoma [15]. The anticancer effect of ginger and its components is mediated by modulation of a wide range of signaling molecules. Ginger extract (GE) increases antioxidant enzymes including superoxide dismutase and glutathione peroxidase [16]. In different cancers, GE inhibits transcription of nuclear factor-kappa B (NF-κB) and the inflammatory cytokine tumor necrosis factor-α (TNF-α). GE could also modulate P53, P21, and vascular endothelial growth factor expression [17].
Mitogenic signals can induce cyclin D1 expression and binding to cdk4/ or cdk6 in G1 phase of the cell cycle to induce proteins involved in DNA replication [18]. Previous studies reported that adenosine monophosphate protein kinase (AMPK) activation has a critical role in cellular physiology such as inhibition of cell proliferation and growth, and activation of autophagy [19]. In the present study, we evaluated the anticancer effect of GE in mice with solid Ehrlich carcinoma (SEC) with emphasis on AMPK pathway and cyclin D1 gene expression as molecular targets. An attempt was being made in this work to augment DOX cytotoxicity using GE as a complementary therapy.
Materials and methods
Drugs
Doxorubicin hydrochloride (Adriblastina(R) vials, Pharmacia Italia S.P.A., Italy) was dissolved in 0.9% sterile sodium chloride solution. Ethanolic ginger extract (MEPACO Pharmaceutical Co., Sharqia, Egypt) was dissolved in propylene glycol. The ethanolic ginger extract contains [6]-gingerol 0.74%, [8]-gingerol 0.13%, [10]-gingerol 0.15%, [6]-shogaol 0.14%, [8]-shogaol 0.011%, [10]-shogaol 0.047, [6]-paradol 0.004%, [1]-dehydrogingerdione 0.019%.
Animals and experimental design
Ehrlich carcinoma is a transplantable model for breast cancer. The guidelines for the care and use of laboratory animals approved by Research Ethics Committee (Faculty of Pharmacy, Tanta University, Egypt) (FPTU-REC, 129/2013/930) were followed. In this study, 60 female Swiss albino mice aged 6–8 weeks old and weighed 18–22 g were obtained from National Research Center (Cairo, Egypt). Mice were provided with standard pellet diet and water ad libitum. The standard pellet diet is composed of 5% lipids, 21% protein, 4% crude fiber, 1% calcium, 8% ash, 0.6% phosphorus, 2% vitamin, 3.4% glucose, and 55% carbohydrates. 1 × 106 of the Ehrlich ascites carcinoma (EAC) cells was obtained from the Pharmacology and Experimental Oncology Unit of the National Cancer Institute (Cairo University, Egypt). The cell viability was found to be more than 99% by trypan blue dye exclusion method [20]. EAC cells were implanted subcutaneously into the right thigh of the lower limb of mice. A palpable solid tumor mass (about 100 mm3) was developed within 12 days. Then, animals were divided into 4 equal groups as follows: SEC group—mice were given the vehicles, GE group—mice were given 100 mg/kg GE by oral gavage, day after day starting on the 12th day of inoculation until day 26 [21], DOX group—mice were injected i.p. with 4 mg/kg DOX for 4 cycles every 5 days (on the 12th, 17th, 22nd, and 27th day) according to [22], GE + DOX group—mice were given both drugs at the specified doses and regimens.
The survival rate was calculated for each experimental group according to [23], using the following formula: Survival rate = (number of live animals in a group on the 28th day/number of animals in the same group at the start of experiment) × 100. On the 12th day and then day after day till the end of experiment, the dimensions of the tumor were measured with a Vernier caliper (Tricle Brand, Shanghai, China). Tumor volume was calculated according to [24], using the following formula: Tumor volume (mm3) = 0.52 AB2, where: A is the length of minor axis and B is the length of major axis. Tumor inhibition rate (TIR) was calculated as follows: TIR = (mean tumor volume of control tumor group − mean tumor volume of treated group) × 100/mean tumor volume of control tumor group [25].
On the 28th day, mice were anaesthetized by ether, blood samples were withdrawn via cardiac puncture and then mice were killed by cervical dislocation. Using cooling centrifuge (Laborzentrifugen 3-3OK, Sigma, Germany), serum samples were obtained at 3000 rpm for 20 min and stored at −80 °C for determination of P53 level. Tumor tissue was carefully excised and divided into portions. One portion was fixed in 10% formalin for histopathological examination and the other portions were kept frozen at −80 °C.
ELISA assay for PAMPK, NF-κB and P53
Enzyme-linked immunosorbent assay (ELISA) kits were obtained from Glory Science Co. (USA) and utilized to determine the level of phosphorylated AMPK (PAMPK)-pT172 and (NF-κB)-p65 in tumor tissue and to assess the level of the tumor suppressor gene P53 in serum, according to the manufacturer’s protocol.
DNA content of tumor tissue
Using G-spin™ total DNA extraction kit (iNtRON Biotechnology Co., Korea), DNA was extracted from tumor tissue and its concentration was measured at 260 nm according to [26] using spectrophotometer (Unicam, England).
Real time-polymerase chain reaction (RT-PCR) for cyclin D1
Total RNA was isolated from tumor tissue using RNA-spin™ total RNA extraction kit (iNtRON Biotechnology Co., Korea) under liquid nitrogen according to the manufacturer’s protocol. Primers (Biosearch technologies Co., USA) used in RT-PCR are presented in Table 1 and were prepared according to [27]. Total RNA was reverse transcribed to cDNA using SYBR Green I PCR (iNtRON Biotechnology Co., Korea). Real-time PCR was performed at the following conditions: 95 °C, 30 s (Pre-denaturation), then 40 cycles (95 °C for 5 s for denaturation and 55 °C for 10 s for annealing/extension). Each sample was analyzed and normalized to the level of housekeeping gene (β-actin) and expressed as relative copy number (RCN). Ct (threshold cycle) values of the sample were calculated, and transcript levels were analysed by the 2−ΔCt method.
Histopathological examination
Sections of tumor tissue were prepared (3–5 µm thick) and stained with hematoxylin and eosin (H&E). Tumor tissues were examined for the histopathological features as well as the count of apoptotic cells and images were recorded using Olympus microscope (Japan) equipped with spot digital camera, and computer program MATLAB software.
Statistical analysis
Analysis of data was performed with statistical package for social science (SPSS) software version 16. Data are presented as mean ± SD. Comparison between groups was performed with one-way analysis of variance (ANOVA) using Fisher’s least-significant differences (LSD) option. Statistical significance was obtained at P > 0.05 [28].
Results
Effect on survival rate and tumor volume
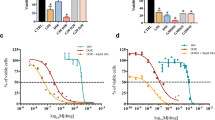
The survival rate was 67% in SEC group and increased to 80% in DOX group, and to 100% in GE group and GE + DOX group (Fig. 1a). The tumor volume in SEC group on day 12 was 120.2 ± 5.12 mm3 and increased gradually till it reached 1585.5 ± 168.6 mm3 on day 28. Treatment of SEC-bearing mice with GE, DOX, or both drugs exhibited a significant decrease (P < 0.05) in tumor volume on day 28 to 1280.6 ± 140.4, 1120.9 ± 113.1, and 960.5 ± 100 mm3, respectively, compared to SEC group (Fig. 1b). Regarding tumor inhibition rate, co-treatment with GE and DOX exerted TIR of 38.9% versus 22.9% in GE group and 33.9% in DOX group (Fig. 1c).
Effect of co-treatment with GE and DOX on mice bearing SEC. a Survival rate. b Tumor volume. c Tumor inhibition rate. Data are presented as mean ± SD. Significant difference between groups was calculated on day 28. a Significant versus SEC group. b Significant versus GE group. c Significant versus DOX group
Effect on PAMPK, NF-κB and P53 levels
Figure 2a shows that treatment of SEC mice with DOX significantly (P < 0.01) reduced the level of PAMPK in tumor tissue (0.1857 ± 0.022 ng/g tissue) compared to SEC group (0.305 ± 0.038 ng/g tissue). On the other hand, GE alone or co-treatment with GE and DOX caused a significant increase (P < 0.001) in the level of PAMPK to reach 1.55 ± 0.065 and 1.39 ± 0.058 ng/g tissue, respectively, compared to SEC group. In addition, the level of PAMPK was significantly increased in GE group (P < 0.01) and co-treatment group (P < 0.001) compared to DOX group.
GE alone or in combination with DOX significantly (P < 0.001) lowered NF-κB content in tumor tissue to 8.7 ± 0.9 and 1.85 ± 0.37 ng/g tissue, respectively, compared to SEC group (10.3 ± 1.06 ng/g tissue) (Fig. 2b). On the other hand, treatment of SEC mice with DOX resulted in a significant increase (P < 0.01) in NF-κB content (11.2 ± 1.24 ng/g tissue) compared to SEC group. However, the combined treatment with GE and DOX significantly (P < 0.001) lowered NF-κB content compared to each treatment alone.
Treatment of SEC-bearing mice with GE, DOX, or both drugs resulted in a significant increase (P < 0.001) in serum P53 level to 480.08 ± 35.1, 863.08 ± 49.1, and 1445.2 ± 73.8 pg/mL, respectively, compared to SEC group (109.46 ± 11.6 pg/mL) (Fig. 2c). In addition, co-treatment with GE and DOX raised serum P53 level significantly (P < 0.01) compared to either GE or DOX group.
Effect on tumor DNA content
Treatment of SEC-bearing mice with GE, DOX, or both drugs resulted in a significant decrease (P < 0.001) in DNA content (72 ± 10, 41 ± 9, and 20 ± 4 pg/g tissue, respectively) compared to SEC group (132 ± 15 pg/g tissue) (Fig. 3 ). Co-treatment with GE and DOX significantly lowered tumor DNA content versus GE monotreated group (P < 0.001) and versus DOX group (P < 0.01).
Effect on cyclin D1 gene expression
Figure 4 shows that treatment of SEC mice with DOX significantly (P < 0.05) increased cyclin D1 gene expression in tumor tissue (0.119 ± 0.023 RCN) compared to SEC group (0.0975 ± 0.0095 RCN). On the other hand, GE alone or in combination with DOX caused a significant decrease (P < 0.01) in cyclin D1 gene expression to reach 0.04 ± 0.0063 and 0.013 ± 0.0062 RCN, respectively, compared to SEC group. Cyclin D1 gene expression was significantly decreased in GE group compared to DOX group (↓66.3%, P < 0.01). Combined treatment with GE and DOX significantly decreased (P < 0.001) cyclin D1 gene expression by 67.5% versus GE group and 89% versus DOX group (Fig. 4 ).
Histopathological results
Tumor sections from SEC group showed numerous multinucleated cells, dilated blood vessels and few apoptotic residual bodies (Fig. 6a). On the other hand, tumor sections from mice treated with GE showed a significant increase (P < 0.001) in apoptotic cell count to reach (40 ± 4.1 cells) compared to SEC group (16 ± 0.8 cells) (Figs. 5, 6b). Treatment of SEC mice with DOX resulted in a significant increase (P < 0.001) in apoptotic cell count (20 ± 0.82 cells) compared to SEC group (Figs. 5, 6c). Co-treatment group showed absence of multinucleated cells in tumor tissue with a significant increase (P < 0.001) in apoptotic cell count (50 ± 5 cells) compared to SEC group (Figs. 5, 6d). However, the apoptotic cell count in co-treatment group showed a significant increase (P < 0.01) versus DOX mono-treatment group (Fig. 5).
Haematoxylin and eosin (H&E) photomicrographs ×40 of tumor sections from SEC-bearing mice. a SEC group showing a large fibrotic sheet (half moon symbol), groups of multinucleated cells (closed down arrows), dilated blood vessels (four-pointed star), few apoptotic residual bodies (open “L” symbol) and increased apoptosis (open triangles) (H&E ×40). b GE group showing increased apoptosis (open triangles) (H&E ×40). c DOX group showing increased apoptosis (open triangles) (H&E ×40). d GE + DOX group showing absence of multinucleated cells, and an area of necrosis (open oval) with increased apoptosis (open triangles) (H&E ×40)
Discussion
The major problem in breast cancer chemotherapy is the toxicity of the established drugs [29]. However, plants and plant-derived products have proved effective and safe in the treatment and management of cancer. Many natural products and their analogues have been identified as potent anti-cancer agents including ginger and its constituents [30]. In the current study, we hypothesized that the anticancer effects of ginger extract might potentiate the effectiveness of DOX in treatment of breast cancer mice.
Inoculation of EAC cells into the right thigh of the lower limb of mice induced tumor development and neoplastic changes as shown by the histopathological results. SEC group showed numerous multinucleated cells and dilated blood vessels. The histopathological changes observed in SEC group, herein, were partially corrected by ginger extract treatment. Ginger extract group showed a significant increase in apoptotic cell count compared to SEC group. In addition, co-treatment of SEC mice with ginger extract and DOX showed absence of multinucleated cells in tumor tissue and significantly increased apoptosis compared to each of SEC and DOX groups. The phenolic substances present in ginger, generally, possess strong anti-oxidative and anti-inflammatory properties and exert substantial anti-mutagenic and anti-carcinogenic activities [12].
Our histopathological findings were parallel with the regression of tumor volume and also with the increase of serum level of P53 by each of ginger extract, DOX and both. P53 is a key tumor suppressor that plays a critical role in preventing cancer progression by inhibiting proliferation and inducing apoptosis of tumor cells [31]. Ginger induced apoptosis in endometrial cancer cells by increasing the expression of P53 and Bax and simultaneously decreasing the expression of Bcl-2 [13]. In addition, [32] reported that DOX induced apoptosis in mammary gland carcinoma.
Treatment of SEC mice with DOX significantly decreased PAMPK level. It was reported that DOX induced inhibition of AMPK and resulted in genotoxic stress and P53 activation in both carcinoma and non-carcinoma cells [33]. These effects may be accounted for inability of DOX to affect signaling upstream of AMPK including liver kinase B1 (LKB1) [34] and this is the mechanism behind its cardiotoxicity.
However, in the current study, ginger extract treatment induced a significant increase in the level of active phosphorylated form of AMPK. It was reported that ginger extract induced AMPK activation through a Ca+2 calmodulin-dependent protein kinase kinase (CaMKK) pathway [35]. Several upstream kinases, including LKB1 and CaMKK pathways, activate AMPK by phosphorylation of a threonine residue (Thr172) [36]. The anticancer effect of AMPK is linked to inhibition of anabolic pathways that promote cell growth, such as synthesis of phospholipids, fatty acids, ribosomal RNA, and proteins [37]. Herein, the combination of ginger extract with DOX caused a significant increase in the level of PAMPK to 7.5 folds compared to DOX group. Activation of AMPK could mediate the anticancer effect of ginger extract by which ginger extract potentiated the cytotoxic effect of DOX and compensated for the deleterious inhibitory effect of DOX on AMPK in the co-treatment group.
NF-κB signaling is activated by extracellular stimuli, which are recognized by receptors and transmitted into the cell [38]. These signaling cascades can activate IκB kinase (IKK), which phosphorylates the inhibitory IκB subunit of the NF-κB-IκB complex in the cytoplasm [39]. This phosphorylation leads to IκB degradation by the proteasome and releasing NF-κB from the inhibitory complex. The freed NF-κB proteins are then transported into the nucleus where they bind to their target genes for transcription [39]. Our results revealed that ginger extract treatment significantly decreased NF-κB content in tumor tissue. These results were in agreement with [35], who reported that ginger extract induced suppression of NF-κB activity through inhibition of IKK and stabilization of inhibitory IκBα.
On the other hand, DOX mono-treatment, herein, significantly increased NF-κB content in tumor tissue. The atypical NF-κB activation was induced by DOX through inhibition of c-Abl tyrosine kinase in breast cancer cells and therefore, sensitivity of the cancer cells to DOX was diminished [40]. In the present study, a greater reduction of NF-κB content (↓83.5%) in tumor tissue was achieved by co-treatment with ginger extract and DOX, thereby correcting the effect of DOX on NF-κB level.
Cyclin D1 is a biomarker of cancer progression. During G1 phase, cyclin D1 is synthesized rapidly, then degraded when the cell enters the S phase. Activation of cyclin-dependent kinases (CDKs), CDK4 and CDK6, by cyclin D1 is responsible for cancer progression [41]. Our data indicated that the anticancer effect of ginger extract was associated with a significant reduction in cyclin D1 gene expression. These results were in agreement with [42], who reported that ginger extract induced G0/G1 cells’ arrest in HT 29 and HCT 116 colon cancer cell lines. It was reported that ginger extract down-regulated cyclin D1 gene expression via mTOR and Wnt/β-catenin pathways in colon cancer cells [43]. In addition, 6-Shogaol, a constituent of ginger, decreased the level of several signal transducer and activator of transcription 3(STAT3) and NF-κB-regulated target genes including cyclin D1 [44]. However, treatment of SEC mice with DOX in the current work resulted in a significant increase in cyclin D1 gene expression. DOX induced overexpression of cyclin D1 in human breast cancer T47D cells at the G2/M phase [45]. It was reported that DOX induced resistance in HL-60 cells which is related to increase in S-phase cells and increased telomerase activity [46]. These effects may be explained by the inhibition of AMPK activity by DOX. On the other hand, the increased AMPK activity leads to SIRT1 activation and decreasing inflammation [47]. It was found that inhibition of SIRT1 is associated with increased telomerase activity [48, 49]. Fortunately, combined treatment with ginger extract and DOX induced a greater down-regulation of cyclin D1 gene expression compared to mono-treatment groups that indicated the synergistic effect of ginger extract on DOX treatment.
Aggressiveness of various neoplasms is increased with uncontrolled proliferation and a parallel increase in cellular DNA content. Cyclin D1 depletion increased caspase-3 activities, apoptosis and induced DNA damage [50]. Activation of AMPK and down-regulation of cyclin D1, as observed in this work, resulted in reduction of DNA content in ginger extract mono-treatment group and co-treatment group. These results were in agreement with [51], who reported that ginger inhibited prostate cancer cell proliferation. Despite DOX diminished AMPK activity and induced cyclin D1 up-regulation, it significantly decreased DNA content in DOX mono-treatment group because its anticancer effect is related to free radicals’ generation that causes damage to cellular membranes, DNA and proteins [52]. Moreover, DOX can intercalate itself into DNA molecules and causing inhibition of DNA polymerase activity and ultimately ceasing DNA replication [53]. DOX was reported to reduce DNA content in mammary gland carcinoma [32].
Conclusion
The antineoplastic properties of ginger extract were proved in the present work, the molecular mechanisms mediating the anti-proliferative activity of ginger extract in SEC mice involved activation of AMPK pathway and down-regulation of cyclin D1 and consequently induction of apoptosis and reduction of DNA and NF-κB contents in tumor tissue. Co-treatment of SEC mice with both ginger extract and DOX showed a greater anticancer efficacy than mono-treatment with either drug. The use of ginger extract as a complementary therapy with DOX could augment its cytotoxic effects through different molecular mechanisms.
References
Tan BS, Kang O, Mai CW, Tiong KH, Khoo AS, Pichika MR et al (2013) 6-Shogaol inhibits breast and colon cancer cell proliferation through activation of peroxisomal proliferator activated receptor γ (PPAR γ). Cancer Lett 336(1):127–139
Elbialy NS, Mady MM (2015) Ehrlich tumor inhibition using doxorubicin containing liposomes. Saudi Pharma J 23(2):182–187
de Manincor M, Bensoussan A, Smith CA, Barr K, Schweickle M, Donoghoe LL et al (2016) Individualized yoga for reducing depression and anxiety, and improving well-being: a randomized controlled trial. Depress Anxiety. doi:10.1002/da.22502
Mielenz TJ, Xiao C, Callahan LF (2016) Self-management of arthritis symptoms by complementary and alternative medicine movement therapies. J Altern Complement Med 22(5):404–407
Xie Y, Wan W, Zhao Y, Xie J, Wu Q (2016) Impacts on asthma at persistent stage and immune function in the patients treated with acupuncture for warming yang and benefiting qi. Zhongguo Zhen Jiu 35(11):1089–1093
Dişsiz G, Yilmaz M (2016) Complementary and alternative therapies and health literacy in cancer patients. Complement Ther Clin Pract 23:34–39
Rajesh E, Sankari LS, Malathi L, Krupaa JR (2015) Naturally occurring products in cancer therapy. J Pharm Bioallied Sci. doi:10.4103/0975-7406.155895
Prasad S, Tyagi AK (2015) Ginger and its constituents: role in prevention and treatment of gastrointestinal cancer. Gastroenterol Res Pract. doi:10.1155/2015/142979
Höferl M, Stoilova I, Wanner J, Schmidt E, Jirovetz L, Trifonova D et al (2015) Composition and comprehensive antioxidant activity of ginger (Zingiber officinale) essential oil from Ecuador. Nat Prod Commun 10(6):1085–1090
Mangprayool T, Kupittayanant S, Chudapongse N (2013) Participation of citral in the bronchodilatory effect of ginger oil and possible mechanism of action. Fitoterapia 89:68–73
Anfenan ML (2014) Evaluation of nutritional and anti-diabetic activity of different forms of ginger in rats. Middle East J Sci Res 21(1):56–62.
Hessien M, Doniaa T, El-Gendy S, Abou Sikkenaa M (2013) Unfractionated green tea and ginger polyphenols induce apoptotic, cytotoxic and antioxidant effects in hepatoma cells. J Herbal Med 3:87–98
Liu Y, Whelan RJ, Pattnaik BR, Ludwig K, Subudhi E, Rowland H, et al (2012) Terpenoids from Zingiber officinale (Ginger) induce apoptosis in endometrial cancer cells through the activation of p53. Plos One. doi:10.1371/journal.pone.0053178
Park GH, Park JH, Song HM, Eo HJ, Kim MK, Lee JW et al (2014) Anti-cancer activity of ginger (Zingiber officinale) leaf through the expression of activating transcription factor 3 in human colorectal cancer cells. BMC Complement Altern Med 14(1):408
Plengsuriyakarn T, Viyanant V, Eursitthichai V, Tesana S, Chaijaroenkul W, Itharat A et al (2012) Cytotoxicity, toxicity, and anticancer activity of Zingiber officinale Roscoe against cholangiocarcinoma. Asia Pac J Cancer Prev 9:4597–4606
Jeena K, Liju VB, Kuttan R (2013) Antioxidant, anti-inflammatory and anti-nociceptive activities of essential oil from ginger. Indian J Physiol Pharmacol 57(1):51–62
Tsuboi K, Matsuo Y, Shamoto T et al (2014) Zerumbone inhibits tumor angiogenesis via NF-κB in gastric cancer. Oncol Rep 31(1):57–64
Musgrove EA, Caldon CE, Barraclough J, Stone A, Sutherland RL (2011) Cyclin D as a therapeutic target in cancer. Nat Rev Cancer 11(8):558–572
Hardie DG, Ross FA, Hawley SA (2012) AMPK: a nutrient and energy sensor that maintains energy homeostasis. Nat Rev Mol Cell Biol 13(4):251–262
Shahabuddin MS, Nambiar M, Moorthy BT, Naik PL, Choudhary B (2011) A novel structural derivative of natural alkaloid ellipticine, MDPSQ, induces necrosis in leukemic cells. Invest New Drugs 29:523–533
Habib SH, Makpol S, Abdul Hamid NA, Das S, Ngah WZ, Yusof YA (2008) Ginger extract (Zingiber officinale) has anti-cancer and anti-inflammatory effects on ethionine-induced hepatoma rats. Clinics 63(6):807–813
Iliopoulos D, Hirsch HA, Struhl K (2011) Metformin decreases the dose of chemotherapy for prolonging tumor remission in mouse xenografts involving multiple cancer cell types. Cancer Res 71(9): 3196–201.
Cosetti M, Yu GP, Schantz SP (2008) Five-year survival rates and time trends of laryngeal cancer in the US population. Arch Otolaryngol Head Neck Surg 134(4):370–379
Osman Ael-M, Ahmed MM, Khayyal MT, el-Merzabani MM (1993) Hyperthermic potentiation of ciplatin cytotoxicity on solid Ehrlich carcinoma. Tumori 79(4):268–272
Salem ML, Shoukry NM, Teleb WK, Abdel-Daim MM, Abdel-Rahman MA (2016) In vitro and in vivo antitumor effects of the Egyptian scorpion Androctonus amoreuxi venom in an Ehrlich ascites tumor model. SpringerPlus. doi:10.1186/s40064-016-2269-3
Glasel J (1995) Validity of nucleic acid purities monitored by 260 nm/280 nm absorbance ratios. Biotechniques 18(1):62–63
Gu Y, Zhang S, Wu Q, Xu S, Cui Y, Yang Z et al (2010) Differential expression of decorin, EGFR and cyclin D1 during mammary gland carcinogenesis. JECCR. doi:10.1186/1756-9966-29-6
Field A (2009) Discovering statistics using SPSS. Sage, London
Anampa J, Makower D, Sparano JA (2015) Progress in adjuvant chemotherapy for breast cancer: an overview. BMC Med. doi:10.1186/s12916-015-0439-8
Bukhari SN, Jantan I, Seyed MA (2015) Effects of plants and isolates of Celastraceae family on cancer pathways. Anticancer Agents Med Chem 15(6):681–693
Muller PA, Vousden KH (2014) Mutant p53 in cancer: new functions and therapeutic opportunities. Cancer Cell 25(3):304–317
Khedr NF, Khalil RM (2015) Effect of hesperidin on mice bearing Ehrlich solid carcinoma maintained on doxorubicin. Tumour Biol 36(12):9267–9275
Wang S, Song P, Zou M (2012) Inhibition of AMP-activated protein kinase α (AMPK α) by doxorubicin accentuates genotoxic stress and cell death in mouse embryonic fibroblasts and cardiomyocytes. J Biol Chem 287(11):8001–8012
Gratia S, Kay L, Potenza L, Seffouh A, Novel-Chate V, Schnebelen C et al (2012) Inhibition of AMPK signalling by doxorubicin: at the crossroads of the cardiac responses to energetic, oxidative, and genotoxic stress. Cardiovasc Res 95(3):290–299
Roufogalis BD (2014) Zingiber officinale (ginger): a future outlook on its potentiain prevention and treatment of diabetes and prediabetic state. New J Sci. doi:10.1155/2014/674684.
Carling D, Mayer FV, Sanders MJ, Gamblin SJ (2011) AMP activated protein kinase: nature’s energy sensor. Nat Chem Biol 7:512–518
Lengyel E, Litchfield LM, Mitra AK, Nieman KM, Mukherjee A, Zhang Y et al (2015) Metformin inhibits ovarian cancer growth and increases sensitivity to paclitaxel in mouse models. Am J Obstet Gynecol 212(4):479.e1-479.e10
Wu D, Wu P, Zhao L, Huang L, Zhang Z, Zhao S et al (2015) NF-κB expression and outcomes in solid tumors: a systematic review and meta-analysis. Medicine (Baltimore). doi:10.1097/MD.0000000000001687
Napetschnig J, Wu H (2013) Molecular basis of NF-κB signaling. Annu Rev Biophys 42:19.1–19.26
Esparza Lopez J, Medina-Franco H, Escobar-Arriaga E, Leon-Rodrı´guez E, Zentella-Dehesa A, Ibarra-Sa´nchez MJ (2013) Doxorubicin induces atypical NF-jB activation through c-Abl kinase activity in breast cancer cells. J Cancer Res Clin Oncol 139:1625–1635
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144(5):646–674
Abdullah S, Zainal Abidin SA, Murad NA, Makpol S, Wan Ngah WZ, Yusof YA (2010) Ginger extract (Zingiber officinale) triggers apoptosis and G0/G1 cells arrest in HCT 116 and HT 29 colon cancer cell lines. Afr J Biochem Res 4(4):134–42
Wee LH, Morad NA, Aan GJ, Makpol S, Ngah WZ, Yusof YA (2015) Mechanism of chemoprevention against colon cancer cells using combined Gelam honey and Ginger extract via mTOR and Wnt/β-catenin pathways. Asia Pac J Cancer Prev 16(15): 6549–56
Saha A, Blando J, Silver E, Beltran L (2014) 6-Shogaol from dried ginger inhibits growth of prostate cancer cells both in vitro and in vivo through inhibition of STAT3 and NF-kB signaling. Cancer Prev Res 7:627–638
Rezaei PF, Fouladdel S, Ghaffari SM, Amin G, Azizi E (2012) Induction of G1 cell cycle arrest and cyclin D1 down-regulation in response to pericarp extract of Baneh in human breast cancer T47D cells. J Pharm Sci. doi:10.1186/2008-2231-20-101
Huang KZ, Nie DN, Yin SM, Li YQ, Xie SF, Ma LP et al (2011) Cyclin D1, hTERT expression and telomerase activity in HL-60 and HL-60A cell lines and their significance. J Exp Hematol 19(4):911–915
Żuryń A, Litwiniec A, Klimaszewska-Wiśniewska A, Nowak JM, Gackowska L, Myśliwiec BJ, Pawlik A, Grzanka A (2014) Expression of cyclin D1 after treatment with doxorubicin in the HL-60 cell line. Cell Biol Int 38(7):857–867
Ruderman NB, Xu XJ, Nelson L, Cacicedo JM, Saha AK, Lan F, Ido Y (2010) AMPK and SIRT1: a long-standing partnership? Am J Physiol Endoc M 298(4):E751–E760
Narala SR, Allsopp RC, Wells TB, Zhang G, Prasad P, Coussens MJ, Rossi DJ, Weissman IL, Vaziri H (2008) SIRT1 acts as a nutrient-sensitive growth suppressor and its loss is associated with increased AMPK and telomerase activity. Mol Biol Cell 19(3):1210–9
Mohanty S, Mohanty A, Sandoval N, Tran T, Bedell V, Wu J et al (2016) Cyclin D1 depletion induces DNA damage in mantle cell lymphoma lines. Leukemia Lymphoma 23:1–3
Brahmbhatt M, Gundala SR, Asif G, Shamsi SA, Aneja R (2013) Ginger phytochemicals exhibit synergy to inhibit prostate cancer cell proliferation. Nutr Cancer 65(2):263–272
Thorna CF, Oshiroa C, Marshe S, Hernandez-Boussardb T, McLeodd H, Teri Kleina TE et al (2011) Doxorubicin pathways: pharmacodynamics and adverse effects. Pharmacogenet Genom 21(7):440–446
Tacar O, Sriamornsak P, Dass CR (2013) Doxorubicin: an update on anticancer molecular action, toxicity and novel drug delivery systems. J Pharm Pharmacol 65(2):157–170
Acknowledgements
Authors gratefully acknowledge Dr. Mona A. Yehia, Professor of Histochemistry and Cell Biology, Medical Research Institute, Alexandria, for conducting and interpreting the histopathological examination.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
El-Ashmawy, N.E., Khedr, N.F., El-Bahrawy, H.A. et al. Ginger extract adjuvant to doxorubicin in mammary carcinoma: study of some molecular mechanisms. Eur J Nutr 57, 981–989 (2018). https://doi.org/10.1007/s00394-017-1382-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-017-1382-6