Abstract
Purpose
Diabetes and obesity are characterized by glucose intolerance, fat deposition, inflammation, and dyslipidemia. Recent reports postulated that distinct gut microbiota alterations were observed in obese/diabetic subjects and modulating gut microbiota beneficially through specific probiotics could be a potential therapeutic option for type 2 diabetes/obesity. Therefore, we attempted to study the efficacy of probiotics of Indian gut origin (Lactobacillus plantarum MTCC5690 and Lactobacillus fermentum MTCC5689) along with a positive control, Lactobacillus rhamnosus (LGG) on glucose/lipid homeostasis in high-fat-diet-induced diabetic animal model.
Methods
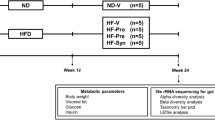
C57BL/6J male mice were divided into seven groups (n = 6 per group) comprising feeding on: (1) Normal Pellet Diet (NPD), (2) High-Fat Diet (HFD), (3) HFD with LGG, (4) HFD with MTCC5690, (5) HFD with MTCC5689, (6) HFD with metformin, and 7) HFD with vildagliptin for a period of 6 months. Biochemical markers, glucose tolerance, insulin resistance, and GLP-1 and LPS levels were assessed by standard protocols. Gut integrity was measured by intestinal permeability test. Transcriptional levels of tight junction proteins (TJPs) were probed in small intestinal tissues while inflammatory signals and other pathway specific genes were profiled in liver, visceral adipose tissue, and skeletal muscle.
Results
Mice fed with HFD became insulin resistant, glucose intolerant, hyperglycemic, and dyslipidemic. Diabetic mice were characterized to exhibit decreased levels of GLP-1, increased gut permeability, increased circulatory levels of LPS, decrease in the gene expression patterns of intestinal tight junction markers (occludin and ZO-1), and increased proinflammatory gene markers (TNFα and IL6) in visceral fat along with decreased mRNA expression of FIAF and adiponectin. Diabetic mice also exhibited increased mRNA expression of ER stress markers in skeletal muscle. In addition, liver from HFD-fed diabetic mice showed increased gene expressions of proinflammation, lipogenesis, and gluconeogenesis. Probiotic interventions (most prominently the MTCC5689) resisted insulin resistance and development of diabetes in mice under HFD feeding and beneficially modulated all the biochemical and molecular alterations in a mechanistic way in several tissues. The metabolic benefits offered by the probiotics were also more or less similar to that of standard drugs such as metformin and vildagliptin.
Conclusion
Native probiotic strains MTCC 5690 and MTCC 5689 appear to have potential against insulin resistance and type 2 diabetes with mechanistic, multiple tissue-specific mode of actions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The 7th edition of the International Diabetes Federation Atlas projects, approximately 515 million people with diabetes worldwide and India alone harbors more than 70 million diabetics. A study conducted to determine the prevalence of diabetes in India (ICMR-INDIAB Study) has shown that the prevalence of prediabetes and diabetes is alarmingly higher in both urban and rural areas and that the number is expected get higher and higher in the coming years [1]. Along with diabetes, overweight and obesity are also emerging as health burden worldwide and in developing countries like India. Due to new economic policy, India and other developing countries are undergoing rapid urbanization. Urbanization has led to rapid changes in lifestyle, decreased physical activity, and easy accessibility to food which contains high fat, sugar, and calorie. This might be one of the important factors for metabolic disorders including type 2 diabetes (T2DM). Epidemiological studies demonstrated that not only genetic factors, but environmental risk factors also influence the prevalence of diabetes and obesity in India [2]. While several omics studies are underway to dissect out the molecular pathogenesis of diabetes and obesity related disorders, gut microbiota has been proposed as an environmental factor, accountable for the development of diabetes and obesity.
Gut microbiota control intestinal permeability, which determines the threshold at which metabolic endotoxemia could induce the metabolic disorders [3]. Energy homeostasis and proinflammatory signals are key factors for the pathogenesis of diabetes, obesity, and associated metabolic disorders. The gut microbiota also plays major role in the regulation of energy homeostasis and inflammatory signatures. While modulating the gut microbiota could be a potential therapeutic target for the treatment of diabetes and obesity, the best way for modulating the gut flora balance in intestine can be achieved by probiotic treatment. Probiotics are live microorganisms which, when administered in adequate amounts confer a health benefit on the host [4]. Species of Lactobacillus and Bifidobacterium are most commonly used microbes as a probiotics. Among these probiotics, lactobacillus species have been claimed to confer health benefits on the management of diabetes and obesity [5, 6]. Recent clinical trial also demonstrated the efficacy of Lactobacillus gasseri treatment in improving the glucose homeostasis and decreasing the abdominal adiposity and body weight [7]. Selective increase in lactic acid bacteria/bifidobacteria supplement has been shown to improve the enteroendocrine L cell proliferation, thereby modulating the gut peptide production (glucagon-like peptide-1, peptide YY and ghrelin) [8, 9]. Type 2 diabetes patients treated with specific lactobacillus strains exhibited appropriate insulin secretion through augmented incretin release implying that oral ingestion of one specific strain may serve as a novel therapeutic approach to improve glucose-dependent insulin release [10].
While the scientific evidence of probiotics has been well studied worldwide, such studies are lacking in India. India being a country with potential microbial diversity, most of the probiotics benefits are claimed as either anectodal or with scarce scientific evidence. Recently, two probiotic strains viz., Lactobacillus plantarum MTCC5690 and L. fermentum MTCC5689 of Indian gut origin were isolated from the fecal samples by the National Dairy Research Institute, Karnal, India and characterized for their identity by 16S rRNA, PCR, RAPD, and whole-genome sequencing [11, 12] and deposited at the International repository under Budapest treaty at MTCC, IMTECH, Chandigarh, India. The efficacy of these two probiotic strains with medicinal properties was also reported previously [13–18]. Therefore, we evaluated the efficacy of these two potential probiotic strains against HFD-induced insulin-resistant diabetic mice model with a focus on disease biology and molecular investigations.
Materials and methods
Animal experiments
Adult (age 8–10 week) male C57BL/6J mice were housed in polypropylene cages in an animal room maintained with a 12-h light/dark cycle at 24 ± 2 °C and 55 ± 5 % humidity. Animals were allowed free access to water and respective diet throughout the study. The animals used in the present study were cared according to the principles and guidance of the Committee for the Purpose of Control and Supervision of Experiments on Animals (CPCSEA). All the protocols and procedures were approved by the Institutional Animal Ethics Committee (IAEC). Normal pellet diet (NPD) and high-fat diet (HFD-57 % kcal energy from fat source) were procured from the National Institute for Nutrition, Hyderabad. Fecal and urine sample were collected on every month with body weight and feed intake recorded periodically.
C57BL/6J mice were divided into seven groups with similar body weight. All lactobacillus probiotic cultures viz. LGG, MTCC 5690, and MTCC 5689 were obtained from ICAR-National Dairy Research Institute (NDRI), Karnal, India. The reference Lactobacillus strain, L. rhamnosus GG was used as the positive control for probiotic treatment. Our experimental study design included standard anti-diabetic drugs such as metformin and vildagliptin which were obtained as a gift sample from Orchid Research Laboratories, Chennai. The study groups therefore, comprised of the following: (1) Normal Pellet Diet (NPD), (2) High-Fat Diet (HFD), (3) HFD with LGG treatment (HFD-LGG), (4) HFD with MTCC 5690 treatment (HFD-MTCC 5690), (5) HFD with MTCC 5689 treatment (HFD-MTCC 5689), (6) HFD with metformin treatment (HFD-Met), and (7) HFD with vildagliptin treatment (HFD-Vilda). Each group comprised of six animals. All the dietary regimen and respective probiotic or drug treatment schedules were continued for 6 months. Dose of viable probiotic bacterial strains (LGG, MTCC 5690 and MTCC 5689) was approximately 1.5 × 109 colonies/mouse/day, p.o. Dose of the metformin and viladgliptin was 300 mg/kg and 1 mg/kg; p.o, respectively. PBS (10 mL/kg; p.o) vehicle treatment was given to NPD and HFD groups (which did not receive any probiotic/drug treatment). Detailed study plan and treatment schedule were presented in Table 1.
Biochemical estimation
At the end of the study, all animals were fasted for 12 h. Blood was collected by retro-orbital plexus puncture and approximately 0.4 ml of blood collected in 10 % EDTA tubes. Plasma was separated upon centrifugation @ 3000 RPM for 15 min at 4 °C and stored at −80 °C until the assays performed. Biochemical analyses were carried out on a PerkinElmer auto-biochemical analyzer. Fasting plasma glucose (GOD-POD method), serum cholesterol (CHOD-PAP method), serum triglycerides (GPO-PAP method), and HDL cholesterol (direct method, polyethylene glycol-pretreated enzymes) were measured. Low-density lipoprotein (LDL) cholesterol was calculated using the Friedewald formula [19]. The HOMA-IR index (homeostasis model assessment) was calculated as follows: HOMA index = fasting glucose (mmol/L) × fasting insulin (mU/L)/22.5 [20]. Plasma insulin was estimated by ELISA (Mercodia kit, Sweden). Glycated hemoglobin (HbA1c) was estimated by high-pressure liquid chromatography using the Variant machine (Bio-Rad, Hercules, California, USA). LPS levels were determined using LAL (Limulus Amebocyte Lysate) assay reagent (Lonza, Walkersville, MD, USA) and expressed as EU/ml.
Insulin tolerance test (ITT)
While hyperglycemia is the hallmark of type 2 diabetes, it originates from insulin resistance. Insulin tolerance test (ITT) is the standard protocol that has routinely been used in preclinical studies to report either improvement or deterioration of insulin sensitivity. Therefore, we assessed the dynamic characteristics of blood glucose after short insulin injection by ITT. All animals were fasted for 5 h. Ultra-short action insulin was administered on abdominal cavity (Actarapid Nova Nordisk, Bangalore; Dose: 0.5 IU/kg; ip). Blood was collected by tail cut, and glucose levels measured by glucometer at 0, 15, 30, 60 and 120 min after insulin injection. Area under curve was calculated by Graph pad software. Glucose disposal rate (% KITT) was calculated by standard preclinical method [21].
Oral glucose tolerance test (OGTT)
At the end of 4-month treatment schedule, OGTT was performed in overnight-fasted (12–14 h) animals as per protocols described previously [22]. Glucose load (2 g/kg/10 mL, p.o) was given to all the animals. Blood was collected by tail cut method. Blood glucose was measured by one-touch glucometer (Accu-check glucometer, Life scan, Johnson & Johnson Ltd) at 0, 30, 60, 90, and 120 min after glucose challenge. Area under curve was calculated by Graph pad software.
In vivo Intestinal permeability assay
Gut permeability was assessed during the 5th month (i.e., around day 150 of the trial period). This measurement is based on the intestinal permeability of 4000 Da fluorescent dextran–FITC (DX-4000–FITC) in systemic circulation (DX-4000–FITC; FD4000; Sigma-Aldrich, St. Louis, Missouri, USA) [23]. Briefly, mice that had fasted for 6 h were administrated DX-4000–FITC through oral gavages (500 mg/kg body weight; 125 mg/ml). After 4 h of DX-4000–FITC administration, 100 µl of blood was collected from the tip of the tail vein and plasma was separated upon centrifugation. DX-4000-FITC concentration (which is a surrogate marker of intestinal permeability) was estimated in plasma by using fluorescence reader (Modulus Micro plate reader, Turner Biosystems, Sunneyvale, CA, USA) set at excitation 485 nm and emission 535 nm.
mRNA quantification by real-time PCR
Total RNA from gastrointestinal tract (GIT) or visceral fat tissue/skeletal muscle/liver of the study animals was isolated by using Illustra™ RNA spin Mini isolation Kit (GE Life sciences Ltd, USA). cDNA was synthesized as described previously [24]. Quantitative real-time PCR was performed for specific genes (β actin, occludin, Zonula occludens-1, TNFα, IL6, Adiponectin, FIAF, GRP78, PERK, IRE1-α, XBP1, CHOP, SREBP-1c, GLUT4, MCP-1, GCK, PEPCK, G6Pc, and FOXO1) using SYBR green master mix (Applied Biosystems). PCR amplification was carried out using ABI-7000 (Applied Biosystems) with cycle conditions (initial cycle: 50 °C for 2 min, initial denaturation 95 °C for 15 s, 40 cycles of denaturation 95 °C for 15 s, and annealing/extension of 60 °C for 1 min). Expression levels of genes were determined using \(2^{{ - \Delta \Delta c_{t} }}\) method; data normalized using β-actin (\(2^{{ - \Delta c_{t} }}\)) and a control condition (\(2^{{ - \Delta \Delta c_{t} }}\)). The primer sequences of specific genes probed in this study are listed in Table 2.
Glucagon-like peptide-1 (GLP-1) estimation
Animals were fasted for overnight. 400 µL of blood was collected in fasting stage to estimate fasting plasma glucose and insulin estimation. 2gm/kg oral glucose challenge was given at 0 min to all the animals. After 30 min, animals were bled and 500 µL of blood was collected into the tube containing 10 % EDTA and 30 µM dipeptidyl peptidase-4 (DPP4) inhibitors (obtained as gift sample from Glenmark Research center, Mumbai, India).This DPP-4 inhibitor prevents the GLP-1 degradation. Plasma was separated upon centrifugation @ 3000 RPM for 15 min at 4 °C and stored at −80 °C until the assays performed. Glucose-induced GLP-1 levels were estimated by using ELISA as per the manufacture instruction (USCN life sciences Inc. USA). Plasma glucose and insulin were also estimated after glucose challenge.
Statistical analysis
Experimental values are expressed as Mean ± SD or Mean ± SEM. Data were analyzed either by using Student’s t test or by using one-way ANOVA followed by Tukey’s multiple post hoc test. Differences were considered significant at p < 0.05. All analyses were done using GraphPad Prism and Windows-based SPSS statistical package (version 10.0, Chicago, IL).
Results
Preclinical characterization and Biochemical markers
Table 3 depicts the biochemical status of the study groups. Significant (p < 0.05) elevation of plasma glucose, total cholesterol, and triglyceride levels were observed in mice fed with high-fat diet (HFD) compared to normal pellet diet (NPD) group. All the glycemic and lipid parameters were significantly reduced in mice with probiotic treatments with the potential effects seen much more with MTCC 5689. The standard drugs metformin and vildagliptin as expected showed glucose and lipid profile lowering actions. While the mice fed with HFD exhibited hyperinsulinemic state as evident from the increased insulin levels, all the treatment arms significantly reduced hyperinsulinemia. The HbA1c test is one of the best methods to determine the previous glycemic episodes of the patients. In this study HFD feeding increases the HbA1c levels, compared to NPD (3.3 ± 0.2 vs 2.7 ± 0.1; p < 0.05). However, metformin and vildagliptin treatment as well as all probiotic treatments (LGG, MTCC 5690 and MTCC 5689) alleviated the HFD-induced elevation of HbA1c levels. Homeostatic model assessment (HOMA-IR) is a method used to quantify insulin resistance, which was significantly increased in HFD group compared with NPD group (4.6 ± 0.2 vs 28 ± 5). All probiotic strains and drug treatments were significantly reduced the elevated HOMA-IR implying amelioration of insulin resistance. Moreover, it was noted that MTCC 5689 pronounced more efficacious effects than other two probiotic strains. Six months of HFD feeding caused significant increase in body weight in mice compared to NPD-fed animals (46.2 ± 3.2 vs 35 ± 3.2; p < 0.05). MTCC 5689 (38.1 ± 1.5; p < 0.05) and metformin (36.2 ± 2.2; p < 0.05) significantly reduced the body weight and restored to normal. Other treatment regimen also showed nonsignificant body weight reductions in the mice. It is important to note that all probiotic/drug treatments reduced bodyweight along with improvements in glucose homeostasis without any significant changes in feed intake. It is interesting to note that, mice treated with the probiotic strains, viz., MTCC5690 and MTCC5689, had improved glycemic and lipid control along with reduction of hyperinsulinemia and HOMA-IR indices that is comparable to anti-diabetic drugs such as metformin and vildagliptin.
Assessment of insulin tolerance test (ITT)
In order to assess the insulin-resistant versus insulin sensitivity status of the study animals, we measured the dynamic characteristics of blood glucose after insulin injection by short insulin tolerance test (ITT). Figure 1a depicts the glucose levels at time points 0, 15, 30, 60, and 120 min after insulin injection in all the study groups. From this glucose disposal curves, the area under curve were plotted to calculate the percentage of glucose disposal rate (% KITT). Interestingly, the % K ITT (percentage of glucose disposal rate) value decreased markedly in HFD group compared to animals fed with NPD diet (0.34 ± 0.06 vs 0.68 ± 0.14; p < 0.05) (Fig. 1b) implying that HFD-fed mice were insensitive to exogenous insulin, i.e., insulin resistance was established in peripheral tissues. All the probiotic and drug treatments significantly increased the % K ITT values implying a significant (p < 0.05) improvement in insulin sensitivity.
a Blood glucose values during insulin tolerance test (ITT) under the experimental conditions at different time points (all values are Mean ± SEM). b Percentage KITT (glucose disposal rate) values during insulin tolerance test (ITT) under the experimental conditions (all values are Mean ± SEM; # p < 0.05 compared to NPD; *p < 0.05 compared to HFD)
Assessment of glucose intolerance
Oral glucose tolerance test (OGTT) was employed to determine the glycemic responses to exogenously administered glucose in all the groups at 4 months of drug or probiotic treatment. Figure 2a depicts the glucose levels at time points 0, 30, 60, 90, and 120 min during OGTT, and from this, the incremental AUCs (area under the curves) of plasma glucose were calculated for all the study groups and are presented in Fig. 2b. Mice fed with HFD exhibited significantly (p < 0.05) increased AUC of plasma glucose compared to NPD-fed animals (Fig. 2b), demonstrating that HFD-fed mice become glucose-intolerant and diabetic. HFD-fed animals treated with LGG, MTCC 5689, metformin, or vildagliptin showed significantly (p < 0.05) decreased AUC levels plasma glucose implying that mice fed with probiotics/drugs become more glucose-tolerant and resisted the genesis of diabetic state.
a Glucose excursion pattern measured during oral glucose tolerance test (OGTT) under the experimental condition at different time points (all values are Mean ± SEM). b Area under curve (AUC) calculated from blood glucose values measured at different time point (0–120 min) during OGTT under the experimental conditions. All values are Mean ± SEM; # p < 0.05 compared to NPD; *p < 0.05 compared to HFD
Circulating GLP-1 level estimation
GLP-1 is one of the key incretin hormones, and it plays a major role in nutrient-induced insulin secretion from the β cells. Apart from this, GLP-1 also reduces gastric emptying thereby inducing satiety. In our study, glucose-induced GLP-1 levels were significantly decreased in animals fed with HFD compared to NPD-fed mice (0.6 ± 0.2 vs 3.2 ± 1 pg/mL, p < 0.05) (Fig. 3). All the probiotic treatments increased and normalized the levels of GLP-1 equal to the conditions seen in control animals. Interestingly HFD mice treated with either metformin or vildagliptin showed several fold increase in the glucose-induced GLP-1 levels.
Effect of probiotic treatment on Intestinal permeability in vivo
Gut integrity level was examined by permeability of fluorescent-tagged dye (DX-4000–FITC) toward systemic circulation from gastrointestinal tract. If gut integrity was damaged, movement of fluorescent-tagged dye concentration will be more in the systemic circulation indicating the increase in gut permeability. HFD-fed mice exhibited elevated plasma DX-4000–FITC concentration (0.16 ± 0.01 vs 0.27 ± 0.05; p < 0.05) as compared to NPD-fed group (Fig. 4) implying that HFD feeding is associated with loss of gut integrity and increase in gut permeability. LGG, MTCC 5690, and MTCC 5689 probiotic treatment groups showed significant decrease in plasma DX-4000–FITC levels indicating an association of gut integrity maintenance under these conditions. Standard drugs like metformin and vildagliptin treatment also showed marked decrease in gut permeability.
Alterations in intestinal tight junction markers
Since HFD-fed mice showed increased gut permeability state, we next determined the extent of transcriptional levels of intestinal tight junction markers in the study groups. Besides exhibiting increased gut permeability, HFD-fed animals also showed significantly (p < 0.05) reduced mRNA expression of epithelial tight junction markers such as occludin and ZO-1 (Fig. 5a, b). All the probiotic treated mice showed a significantly (p < 0.05) increased gene expression profile of the intestinal tight junction markers, occludin and ZO-1. Standard drugs like metformin and vildagliptin also improved the transcriptional levels of intestinal tight junction markers.
Reduction of endotoxemia under treatment with probiotics/drugs
Compared to mice fed with NPD, HFD-fed mice showed significantly (p < 0.05) elevated serum levels of LPS (Fig. 6). All the treatments significantly (p < 0.05) decreased the LPS levels and the best reduction of endotoxemia was observed with MTCC5689 and LGG. This clearly implies that reduction of endotoxemia and restoration of intestinal barrier integrity by the probiotics treatment are tightly linked to the improvement in intestinal permeability.
Effect of probiotic treatment on gene expression profiles in visceral fat
Since HFD consumption is linked to glucose/lipid dyshomeostasis and proinflammation and there exists gut-adipose axis regulatory networks, we next evaluated certain gene expression markers from the visceral adipose tissue from the study groups. There was a several fold increase (p < 0.05) in IL6 and TNFα gene expression in the visceral fat of HFD-fed mice compared to control animals (Fig. 7a, b). However, animals treated with probiotics or drugs significantly (p < 0.05) reduced the HFD-induced increase in proinflammatory gene expression profiles. While FIAF gene expression was significantly (p < 0.05) downregulated in visceral fat of animals fed with HFD diet compared to NPD diet (Fig. 7c), this was significantly (p < 0.05) improved in the presence of probiotics/drugs. We have also examined the adiponectin gene expression level in the visceral adipose tissue from all the study groups. It was found that adiponectin gene expression was significantly (p < 0.05) downregulated in visceral fat of animals fed with HFD compared to NPD (Fig. 7d). Except for LGG, mice treated with other probiotics/drugs showed significantly (p < 0.05) increased transcriptional levels of adiponectin in visceral fat tissue.
Effect of probiotic treatment on gene expression profiles of ER stress markers in skeletal muscle
Since endoplasmic reticulum (ER) stress pathway is emerging as a drug target for type 2 diabetes, we have checked the gene expression patterns of ER stress markers in skeletal muscle from the mice. Compared to control animals, skeletal muscle from mice fed with HFD showed significantly (p < 0.05) elevated transcriptional levels of ER stress markers viz., GRP78 (Fig. 8a), PERK (Fig. 8b), IRE1α (Fig. 8c), XBP1 (Fig. 8d), and CHOP (Fig. 8e). Interestingly, all probiotic/drug treatments considerably restored the ER stress markers to near normal levels. Additional experiments (data not shown) also revealed an increasing trend of lipogenic marker viz., SREBP-1c and decreasing trend of GLUT-4 mRNA levels in skeletal muscle from mice fed with HFD compared to control animals. Again, probiotic/drug treatments restored the SREBP-1c and GLUT4 transcriptional levels albeit with statistical insignificance.
Transcriptional levels of ER stress markers in skeletal muscle tissue from the study groups. a mRNA expression of GRP78, b mRNA expression of PERK, c mRNA expression of IRE1-α, d mRNA expression of XBP1, e mRNA expression of CHOP. All values are Mean ± SEM; # p < 0.05 compared to NPD; *p < 0.05 compared to HFD
Effect of probiotic treatment on gene expression profiles of proinflammation, lipogenesis, and gluconeogenesis in liver
Compared to control animals, liver from the HFD-fed diabetic mice showed significantly (p < 0.05) increased expression of proinflammatory genes such as TNFα (Fig. 9a), IL-6 (Fig. 9b) and MCP-1 (Fig. 9c), as well as increased mRNA expression of GCK (Fig. 9d) and SREBP1c (Fig. 9e). More importantly, liver from the HFD-fed diabetic mice showed significantly (p < 0.05) increased expression of key gluconeogenic genes such as phosphoenol pyruvate carboxykinase (PEPCK) (Fig. 9f) and glucose 6 phosphatase catalytic subunit (G6Pc) (Fig. 9g), along with increased expression of FOXO1 (Fig. 9h), the predominant transcription factor connected with hepatic gluconeogenesis. Interestingly, transcription of all these genes were significantly (p < 0.05) reduced and normalized under the treatment of probiotics as well as anti-diabetic agents.
Discussion
Although there is hope and hype in the usage of probiotics as nutritional supplements and therapeutic modality for many disease states including type 2 diabetes, there is lack of studies that looked into the scientific basis of probiotics with a focus on disease biology and mode of action benefits. Therefore, our study is significant in reporting the following findings: (a) HFD-fed diabetic mice were characterized to exhibit decreased levels of GLP-1, increased gut permeability and circulatory LPS levels and decreased gene expression patterns of intestinal tight junction markers (viz., occludin and ZO-1). (b) Diabetic mice showed increased proinflammatory gene markers (TNFα and IL6) in visceral fat accompanied by decreased mRNA expression of FIAF and adiponectin and increased transcriptional levels of ER stress makers in the skeletal muscle as well as increased gene expression profiles of gluconeogensis in liver. (c) Indigenous probiotic interventions (most prominently the native MTCC 5689 strain) resisted insulin resistance and development of diabetes in mice under HFD feeding and beneficially modulated all the biochemical and molecular alterations both at the systemic and tissue levels. (d) Interestingly all the metabolic benefits seen with the probiotics strains are more or less comparable to that of standard anti-diabetic drugs such as metformin and vildagliptin.
Intestinal flora has been recently proposed as an environmental factor involved in the control of lipids, glucose, body weight, and energy homeostasis. Food and Agriculture Organization/World Health Organization (FAO/WHO) suggested that use of probiotics/prebiotics (functional food) can result in metabolic benefits through modulation of gut microbiota specifically lactobacilli and bifidobacteria [4]. In our study, indigenous probiotic strains (MTCC 5690 and MTCC 5689) improved glucose tolerance and resisted insulin resistance and type 2 diabetes in mice fed with high-fat diet. Preclinical biochemical investigations revealed that these probiotics were able to reduce glucose and lipid levels along with reduction in body weight gain. Our observations and findings correlated well with previous studies [3, 8, 25, 26].
It appears that the beneficial effect of MTCC 5690 and MTCC 5689 in our study could be mediated by mechanism(s) that could improve the gut integrity, decrease systemic levels of LPS (and thereby proinflammation), increase GLP-1, decrease ER stress, and subsequently improve peripheral insulin sensitivity. Supplementation of certain probiotic strains have been shown to beneficially modulate glucose and lipid homeostasis [27]. Previous studies demonstrated that, LPS triggers immune system and proinflammatory cytokines. Prolonged HFD feeding favors the gut environment toward gram-negative bacteria abundance and elevated LPS levels [28, 29]. Normally LPS (endotoxin) leakage was controlled by gut integrity, and gut integrity was maintained by tight junction proteins (TJPs such as occludin and zonula occludens-1). TJPs prevent the translocation of LPS into the systemic circulation. Studies by Cani et al. [8, 30] reported that HFD feeding decreased the TJP expression and resulted in intestinal permeability (leaky gut) as well as elevated LPS in systemic circulation. Four weeks of subcutaneous infusion of LPS resulted in fasting hyperglycemia, hyperinsulinemia, and body weight gain in rodent model, and these metabolic abnormalities resembled those in HFD-fed mice [3, 30]. Since endotoxemia (increased circulatory levels of lipopolysaccharide) has been identified as a triggering factor of insulin resistance in mice, the suppression of endotoxemia by probiotic supplementation is considered as a protective mechanism [31]. In one of our pioneering clinical studies, we have already shown association of increased circulatory LPS levels in patients with type 2 diabetes [32]. Significant reduction of circulatory LPS levels in our present study accompanied by maintenance of gut permeability along with increased expression of intestinal tight junction proteins (occludin and ZO-1) under the probiotic treatment implies that the anti-inflammatory benefits and improvement in peripheral insulin sensitivity might have originated from reduction of endotoxemia and associated signaling cascade. An oral administration of Lactobacillus casei Shirota was able to enhance the expression of plasma lipopolysaccharide-binding protein (LBP) and consequently reduced endotoxemia in murine models of obesity and T2DM [33]. In another study, the consumption of the probiotic strain, Bifidobacteriumanimalis subsp. Lactis 420, suppressed the bacterial translocation process from intestine to tissues, which might lead to metabolic bacteremia in the early onset of T2DM [34]. Together, these finding emphasize that gut microbiota plays a major role in regulating gut integrity, reducing the circulatory levels of LPS and curtailing proinflammation at several sites. While our study demonstrated the mechanistic action of indigenous probiotic strains, further metagenomics work is needed to document the beneficial gut microbiota alterations in such preclinical and clinical studies.
One of the important findings in our study is that all the probiotic/drug treatments increased the nutrient-induced circulatory levels of GLP-1. While vildagliptin regulation of GLP-1 is a direct mechanism [35] and metformin has been shown to increase GLP-1 levels [36], similar effects by the probiotics in our study imply that regulation of GLP-1 by probiotics could be one of the mechanisms of glucose homeostasis regulation. While L cell is responsible for the secretion of GLP-1 [37] and related gut hormones, it has been earlier claimed that probiotics or prebiotics might increase the L cells abundance in the gastrointestinal tract [8]. In a recent study, combining probiotics and/or prebiotics with anti-diabetic drugs (such as metformin and sitagliptin) has been shown to improve glycemic control and insulin sensitivity in mice via beneficial incretin modulation [38]. Based on the literature, we speculate that L cell activation could be linked to beneficial alterations in short-chain fatty acids (SCFAs). Probiotic treatments have been shown to alter a diverse range of pathways outcomes, including alterations SCFAs. While SCFAs (acetate, propionate, and butyrate) are the fermented products of fibers by intestinal microbiota, experimental evidence exists in that GLP-1 level was improved by SCFA-mediated L cell activation [39]. SCFAs upregulate the intestinal proglucagon (a precursor for GLP-1) mRNA expression and peptide-Y (PYY) and act as a ligand for many G-protein-coupled receptors (GPR43). SCFA has been shown to stimulate GPR43 and thereby improves the proliferation and activation of enteroendocrine L cells [40]. While investigating the effect of L. fermentum on representative microbial populations and overall metabolic activity of the human intestinal microbiota using a three-stage continuous culture system, Pereira et al. [41] have demonstrated increased levels of butyrate. Recent metagenomics studies on type 2 diabetes revealed that patients with type 2 diabetes exhibited altered gut microbiota diversity with loss of butyrate-producing bacteria [42, 43]. Connecting all the above, it appears that future studies are warranted to delineate whether the indigenous probiotic strains used in our study could beneficially alter gut microbiota as well as the levels of SCFAs including butyrate.
Proteins secreted from adipose tissue are increasingly recognized to play an important role in the regulation of glucose and lipid metabolism. Suppression of fasting-induced adipocyte factor (FIAF) gene expression in adipose tissue from the HFD-fed mice and upregulation of FIAF by probiotics/drugs in our study is an important observation. Using transgenic mice that mildly over express FIAF in peripheral tissues, Mandard et al. [44] showed that FIAF is an extremely powerful regulator of lipid metabolism and adiposity. In our study, systemic triglyceride levels were significantly decreased under the treatment of probiotics/drugs in association with upregulation of FIAF in visceral fat tissue. In this context, it is important to note that FIAF has been shown to antagonize the activity of lipoprotein lipase (LPL), thereby preventing the storage of triglycerides as fat [45]. Moreover, Bäckhed et al. [46] have demonstrated a mice model in which the gut microbiota suppresses FIAF expression in response host sensitivity to over nutrition, thereby increasing LPL activity and ultimately fat deposition in adipocytes. In another study [47], mice supplemented with Lactobacillus paracasei ssp. paracasei F19 showed reduction of fat storage and higher levels of circulating FIAF even under a high-fat diet. The same alterations in FIAF expression, but to a lesser extent, were observed in co-culture of colonic cell lines with Bifidobacteriumanimalis subsp. lactis Bb12 [47]. In our study, visceral fat from mice fed with HFD showed reduced mRNA expression of adiponectin, and this was restored to normal levels by the potential probiotics. Kim et al. [48] have also reported probiotics-mediated improvement in insulin sensitivity and reduction of adiposity in high-fat diet-fed mice through enhancement of adiponectin production. Therefore, future studies are warranted to delineate the mechanism(s) by which gut microbiota alterations and/or probiotic interventions could beneficially modulate FIAF and adiponectin signals and thereby regulate lipid and glucose homeostasis.
It is now well known that ER stress plays an important role in the progression of insulin resistance in a tissue-specific manner [49]. In one of our recent clinical studies, we have also demonstrated association of increased ER stress markers and proinflammation in patients with type 2 diabetes [50]. Therefore, increased ER stress markers in the skeletal muscle of mice fed with HFD and the amelioration of ER stress by probiotics in our study is an important observation. Previously, Park et al. [51] have reported that Lactobacillus rhamnosus GG improved glucose tolerance through alleviating ER stress in skeletal muscle and suppressed macrophage activation in db/db mice. Further studies are warranted to clarify whether probiotics could function as ‘chaperones’ and offer insulin-sensitizing effects. Recent studies imply a dynamic crosstalk between intestinal microbiota and multiple organs dysfunction in the genesis of obesity and diabetes [52]. Consistent with this, our study also reports increased gene expression of proinflammation, lipogenesis, and gluconeogenesis in liver from the HFD-fed diabetic mice and all of these transcriptional alterations were significantly reduced under the probiotics treatment. A study by Yoo et al. [53] also revealed that certain strain-specific probiotics could beneficially act against metabolic disorders. While our study exposed the several of the tissue-specific beneficial alterations of indigenous probiotic strains, it is suggested that advancements in such studies would unravel novel opportunities for next-generation probiotics targeting type 2 diabetes and other associated metabolic disorders.
To conclude, HFD-fed mice in our study were demonstrated to be insulin resistant, glucose intolerant, dyslipedimic, and obese, and are characterized to exhibit decreased levels of GLP-1, increased circulatory LPS levels and gut permeability, decrease in the gene expression patterns of intestinal tight junction markers (occludin and ZO-1), increased proinflammatory gene markers (TNFα and IL6) in visceral fat accompanied by decreased mRNA expression of FIAF and adiponectin and increased transcriptional levels of ER stress makers in the skeletal muscle as well as increased gene expression profiles of gluconeogensis in liver. Probiotic interventions (most prominently the indigenous MTCC 5689 strain) resisted insulin resistance and development of diabetes in mice under HFD feeding and beneficially modulated all the biochemical and molecular alterations in a mechanistic way both at systemic and tissue levels. Further metagenomics and metabolomics studies would unravel and extend the therapeutic benefits of probiotics. Since several recent studies on probiotics also reported improved glucose and glycemic factors in healthy volunteers and patients with diabetes [54–58], it appears that the probiotic strain MTCC 5689 on further investigations could be a promising candidate to enter into human clinical trials.
Abbreviations
- MTCC 5690:
-
Lactobacillus plantarum Lp91
- MTCC 5689:
-
Lactobacillus fermentum Lf1
- LGG:
-
Lactobacillus rhamnosus GG
- FIAF:
-
Fasting-induced adipocyte factor
- ZO-1:
-
Zonula occludens-1
- NPD:
-
Normal pellet diet
- HFD:
-
High-fat diet
- IL6:
-
Interleukin 6
- TNFα:
-
Tumor necrosis factor alpha
- LPS:
-
Lipopolysaccharide
- GRP78:
-
Glucose-regulated protein 78
- PERK:
-
Protein kinase R (PKR)-like endoplasmic reticulum kinase
- IRE1-α:
-
Inositol-requiring enzyme 1 alpha
- XBP1:
-
X-box-binding protein 1
- CHOP:
-
CCAAT-enhancer-binding protein homologous protein
- SREBP-1c:
-
Sterol regulatory element-binding protein 1 (SREBP-1)
- GLUT4:
-
Glucose transporter, member 4
- MCP1:
-
Monocyte chemoattractant protein-1
- GCK:
-
Glucokinase
- PEPCK:
-
Phosphoenolpyruvate carboxykinase
- G6Pc:
-
Glucose-6-phosphatase catalytic subunit
- FOXO1:
-
Forkhead box protein O1
References
Anjana RM, Pradeepa R, Deepa M, Datta M, Sudha V, Unnikrishnan R, Bhansali A, Joshi SR, Joshi PP, Yajnik CS, Dhandhania VK, Nath LM, Das AK, Rao PV, Madhu SV, Shukla DK, Kaur T, Priya M, Nirmal E, Parvathi SJ, Subhashini S, Subashini R, Ali MK, Mohan V, Group II (2011) Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: phase I results of the Indian Council of Medical Research- INdiaDIABetes (ICMR-INDIAB) study. Diabetologia 54:3022–3027. doi:10.1007/s00125-011-2291-5
Mohan V, Sudha V, Radhika G, Radha V, Rema M, Deepa R (2007) Gene-environment interactions and the diabetes epidemic in India. Forum Nutr 60:118–126. doi:10.1159/0000107088
Cani PD, Bibiloni R, Knauf C, Waget A, Neyrinck AM, Delzenne NM, Burcelin R (2008) Changes in gut microbiota control metabolic endotoxemia-induced inflammation in high-fat diet-induced obesity and diabetes in mice. Diabetes 57:1470–1481. doi:10.2337/db07-1403
FAO/WHO (2002) Working Group Report on Drafting Guidelines for the Evaluation of Probiotics in Food London, Ontario, Canada
Yadav H, Jain S, Sinha PR (2007) Antidiabetic effect of probiotic dahi containing Lactobacillus acidophilus and Lactobacillus casei in high fructose fed rats. Nutrition (Burbank, Los Angeles County, Calif.) 23:62–68. doi:10.1016/j.nut.2006.09.002
Matsuzaki T, Nagata Y, Kado S, Uchida K, Kato I, Hashimoto S, Yokokura T (1997) Prevention of onset in an insulin-dependent diabetes mellitus model, NOD mice, by oral feeding of Lactobacillus casei. Actapathol Microbiol Immunol Scand 105:643–649
Kadooka Y, Sato M, Imaizumi K, Ogawa A, Ikuyama K, Akai Y, Okano M, Kagoshima M, Tsuchida T (2010) Regulation of abdominal adiposity by probiotics (Lactobacillus gasseri SBT2055) in adults with obese tendencies in a randomized controlled trial. Euro J Clin Nutr 64:636–643. doi:10.1038/ejcn.2010.19
Cani PD, Lecourt E, Dewulf EM, Sohet FM, Pachikian BD, Naslain D, De Backer F, Neyrinck AM, Delzenne NM (2009) Gut microbiota fermentation of prebiotics increases satietogenic and incretin gut peptide production with consequences for appetite sensation and glucose response after a meal. Am J Clin Nutr 90:1236–1243. doi:10.3945/ajcn.2009.28095
Kaji I, Karaki S-I, Tanaka R, Kuwahara A (2011) Density distribution of free fatty acid receptor 2 (FFA2)-expressing and GLP-1-producing enteroendocrine L cells in human and rat lower intestine, and increased cell numbers after ingestion of fructo-oligosaccharide. J Mol Histol 42:27–38. doi:10.1007/s10735-010-9304-4
Simon M-CC, Strassburger K, Nowotny B, Kolb H, Nowotny P, Burkart V, Zivehe F, Hwang J-HH, Stehle P, Pacini G, Hartmann B, Holst JJ, MacKenzie C, Bindels LB, Martinez I, Walter J, Henrich B, Schloot NC, Roden M (2015) Intake of Lactobacillus reuteri improves incretin and insulin secretion in glucose-tolerant humans: a proof of concept. Diabetes Care 38:1827–1834. doi:10.2337/dc14-2690
Grover S, Sharma VK, Mallapa RH, Batish VK (2013) Draft Genome Sequence of Lactobacillus fermentum Lf1, an Indian isolate of human gut origin. Genome Announc 14(1(6)): pii: e00883–13. doi: 10.1128/genomeA.00883-13
Grover S, Sharma VK, Mallapa RH, Batish VK (2013) Draft genome sequence of lactobacillus plantarum strain Lp91, a promising Indian probiotic isolate of human gut origin. Genome Announc 21;1(6): pii:e00976–13. doi:10.1128/genomeA.00976-13
Kumar R, Grover S, Batish VK (2011) Hypocholesterolaemic effect of dietary inclusion of two putative probiotic bile salt hydrolase-producing Lactobacillus plantarum strains in Sprague-Dawley rats. Br J Nutr 105:561–573. doi:10.1017/S0007114510003740
Duary RK, Rajput YS, Batish VK, Grover S (2011) Assessing the adhesion of putative indigenous probiotic lactobacilli to human colonic epithelial cells. Indian J Med Res 134:664–671. doi:10.4103/0971-5916.90992
Duary RK, Bhausaheb MA, Batish VK, Grover S (2012) Anti-inflammatory and immunomodulatory efficacy of indigenous probiotic Lactobacillus plantarum Lp91 in colitis mouse model. Mol Biol Rep 39:4765–4775
Chandran A, Duary RK, Grover S, Batish VK (2013) Relative expression of bacterial and host specific genes associated with probiotic survival and viability in the mice gut fed with Lactobacillus plantarum Lp91. Microbiol Res 168:555–562
AparnaSudhakaran V, Panwar H, Chauhan R, Duary RK, Rathore RK, Batish VK, Grover S (2013) Modulation of anti-inflammatory response in lipopolysaccharide stimulated human THP-1 cell line and mouse model at gene expression level with indigenous putative probiotic lactobacilli. Genes Nutr 8:637–648
Chauhan R, Vasanthakumari AS, Panwar H, Mallapa RH, Duary RK, Batish VK, Grover SC (2014) Amelioration of colitis in mouse model by exploring antioxidative potentials of an indigenous probiotic strain of Lactobacillus fermentum Lf1. BioMed Res Int 2014:206732
Whiting MJ, Shephard MD, Tallis GA (1997) Measurement of plasma LDL cholesterol in patients with diabetes. Diabetes Care 20:12–14
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Zhang JQ, Gao CR, Huang QL (1997) Determination of insulin sensitivity by short insulin tolerance test using capillary blood glucose. Chin J Endocrinol Metab 13:77–80
Srinivasan K, Patole PS, Kaul CL, Ramarao P (2004) Reversal of glucose intolerance by pioglitazone in high fat diet-fed rats. Methods Find Exp Clin Pharmacol 26:327–333
Wang Q, Fang CH, Hasselgren PO (2001) Intestinal permeability is reduced and IL-10 levels are increased in septic IL-6 knockout mice. Am J Physiol Regul Integr Comp Physiol 281:23
Balasubramanyam M, Aravind S, Gokulakrishnan K, Prabu P, Sathishkumar C, Ranjani H, Mohan V (2011) Impaired miR-146a expression links subclinical inflammation and insulin resistance in Type 2 diabetes. Mol Cell Biochem 351:197–205. doi:10.1007/s11010-011-0727-3
Karimi G, Sabran MR, Jamaluddin R, Parvaneh K, Mohtarrudin N, Ahmad Z, Khazaai H, Khodavandi A (2015) The anti-obesity effects of Lactobacillus casei strain Shirota versus Orlistat on high fat diet-induced obese rats. Food Nutr Res 59:29273. doi:10.3402/fnr.v59.29273
Hsieh F-CC, Lee C-LL, Chai C-YY, Chen W-TT, Lu Y-CC, Wu C-SS (2013) Oral administration of Lactobacillus reuteri GMNL-263 improves insulin resistance and ameliorates hepatic steatosis in high fructose-fed rats. Nutr Metab 10:35. doi:10.1186/1743-7075-10-35
Ooi L-GG, Liong M-TT (2010) Cholesterol-lowering effects of probiotics and prebiotics: a review of in vivo and in vitro findings. Int J Mol Sci 11:2499–2522. doi:10.3390/ijms11062499
Corcos M, Guilbaud O, Paterniti S, Moussa M, Chambry J, Chaouat G, Consoli SM, Jeammet P (2003) Involvement of cytokines in eating disorders: a critical review of the human literature. Psychoneuroendocrinology 28:229–249
Kim K-AA, Gu W, Lee I-AA, Joh E-HH, Kim D-HH (2012) High fat diet-induced gut microbiota exacerbates inflammation and obesity in mice via the TLR4 signaling pathway. PloS One 7. doi:10.1371/journal.pone.0047713
Cani PD, Amar J, Iglesias MA, Poggi M, Knauf C, Bastelica D, Neyrinck AM, Fava F, Tuohy KM, Chabo C, Waget A, Delmée E, Cousin B, Sulpice T, Chamontin B, Ferrières J, Tanti J-FF, Gibson GR, Casteilla L, Delzenne NM, Alessi MC, Burcelin R (2007) Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes 56:1761–1772. doi:10.2337/db06-1491
Everard A, Cani PD (2013) Diabetes, obesity and gut microbiota. Best practice & research. Clin Gastroenterol 27:73–83. doi:10.1016/j.bpg.2013.03.007
Jayashree B, Bibin YS, Prabhu D, Shanthirani CS, Gokulakrishnan K, Lakshmi BS, Mohan V, Balasubramanyam M (2014) Increased circulatory levels of lipopolysaccharide (LPS) and zonulin signify novel biomarkers of proinflammation in patients with type 2 diabetes. Mol Cell Biochem 388:203–210. doi:10.1007/s11010-013-1911-4
Naito E, Yoshida Y, Makino K, Kounoshi Y, Kunihiro S, Takahashi R, Matsuzaki T, Miyazaki K, Ishikawa F (2011) Beneficial effect of oral administration of Lactobacillus casei strain Shirota on insulin resistance in diet-induced obesity mice. J Appl Microbiol 110:650–657. doi:10.1111/j.1365-2672.2010.04922.x
Amar J, Chabo C, Waget A, Klopp P, Vachoux C, Bermúdez-Humarán LG, Smirnova N, Bergé M, Sulpice T, Lahtinen S, Ouwehand A, Langella P, Rautonen N, Sansonetti PJ, Burcelin R (2011) Intestinal mucosal adherence and translocation of commensal bacteria at the early onset of type 2 diabetes: molecular mechanisms and probiotic treatment. EMBO Mol Med 3:559–572. doi:10.1002/emmm.201100159
D’Alessio DA, Denney AM, Hermiller LM, Prigeon RL, Martin JM, Tharp WG, Saylan ML, He Y, Dunning BE, Foley JE, Pratley RE (2009) Treatment with the dipeptidyl peptidase-4 inhibitor vildagliptin improves fasting islet-cell function in subjects with type 2 diabetes. J Clin Endocrinol Metab 94:81–88. doi:10.1210/jc.2008-1135
Mannucci E, Tesi F, Bardini G, Ognibene A, Petracca MG, Ciani S, Pezzatini A, BrogiM Dicembrini I, Cremasco F, Messeri G, Rotella CM (2004) Effects of metformin on glucagon-like peptide-1 levels in obese patients with and without Type 2 diabetes. Diab Nutr Metab 17:336–342
Lim GE, Huang GJ, Flora N, LeRoith D, Rhodes CJ, Brubaker PL (2009) Insulin regulates glucagon-like peptide-1 secretion from the enteroendocrine L cell. Endocrinology 150:580–591. doi:10.1210/en.2008-0726
Stenman LK, Waget A, Garret C, Briand F, Burcelin R, Sulpice T, Lahtinen S (2015) Probiotic B420 and prebiotic polydextrose improve efficacy of antidiabetic drugs in mice. Diabetol Metab Syndr 7:75. doi:10.1186/s13098-015-0075-7
Wong JM, de Souza R, Kendall CW, Emam A, Jenkins DJ (2006) Colonic health: fermentation and short chain fatty acids. J Clin Gastroenterol 40:235–243
S-i Karaki, Mitsui R, Hayashi H, Kato I, Sugiya H, Iwanaga T, Furness JB, Kuwahara A (2006) Short-chain fatty acid receptor, GPR43, is expressed by enteroendocrine cells and mucosal mast cells in rat intestine. Cell Tissue Res 324:353–360. doi:10.1007/s00441-005-0140-x
Pereira DI, Gibson GR (2002) Effects of consumption of probiotics and prebiotics on serum lipid levels in humans. Crit Rev Biochem Mol Biol 37:259–281. doi:10.1080/10409230290771519
Qin J, Li Y, Cai Z, Li S, Zhu J, Zhang F, Liang S, Zhang W, Guan Y, Shen D, Peng Y, Zhang D, Jie Z, Wu W, Qin Y, Xue W, Li J, Han L, Lu D, Wu P, Dai Y, Sun X, Li Z, Tang A, Zhong S, Li X, Chen W, Xu R, Wang M, Feng Q, Gong M, Yu J, Zhang Y, Zhang M, Hansen T, Sanchez G, Raes J, Falony G, Okuda S, Almeida M, LeChatelier E, Renault P, Pons N, Batto J-MM, Zhang Z, Chen H, Yang R, Zheng W, Li S, Yang H, Wang J, Ehrlich SD, Nielsen R, Pedersen O, Kristiansen K, Wang J (2012) A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature 490:55–60. doi:10.1038/nature11450
Forslund K, Hildebrand F, Nielsen T, Falony G, Le Chatelier E, Sunagawa S, Prifti E, Vieira-Silva S, Gudmundsdottir V, Krogh Pedersen H, Arumugam M, Kristiansen K, Voigt AY, Vestergaard H, Hercog R, Igor Costea P, Kultima JR, Li J, Jørgensen T, Levenez F, Dore J, consortium M, Nielsen HB, Brunak S, Raes J, Hansen T, Wang J, Ehrlich SD, Bork P, Pedersen O (2015) Disentangling type 2 diabetes and metformin treatment signatures in the human gut microbiota. Nature 528:262–266. doi:10.1038/nature15766
Mandard S, Zandbergen F, van Straten E, Wahli W, Kuipers F, Müller M, Kersten S (2006) The fasting-induced adipose factor/angiopoietin-like protein 4 is physically associated with lipoproteins and governs plasma lipid levels and adiposity. J Biol Chem 281:934–944. doi:10.1074/jbc.M506519200
Shen J, Obin MS, Zhao L (2013) The gut microbiota, obesity and insulin resistance. Mol Aspects Med 34:39–58. doi:10.1016/j.mam.2012.11.001
Bäckhed F, Manchester JK, Semenkovich CF, Gordon JI (2007) Mechanisms underlying the resistance to diet-induced obesity in germ-free mice. Proc Natl Acad Sci USA 104:979–984. doi:10.1073/pnas.0605374104
Aronsson L, Huang Y, Parini P, Korach-André M, Håkansson J, Gustafsson J-ÅÅ, Pettersson S, Arulampalam V, Rafter J (2010) Decreased fat storage by Lactobacillus paracasei is associated with increased levels of angiopoietin-like 4 protein (ANGPTL4). PloS One 5. doi:10.1371/journal.pone.0013087
Kim SW, Park KY, Kim B, Kim E, Hyun CK (2013) Lactobacillus rhamnosus GG improves insulin sensitivity and reduces adiposity in high-fat diet-fed mice through enhancement of adiponectin production. Biochem Biophys Res Commun 431:258–263. doi:10.1016/j.bbrc.2012.12.121
Flamment M, Hajduch E, Ferré P, Foufelle F (2012) New insights into ER stress-induced insulin resistance. Trend Endocrinol Metab 23:381–390. doi:10.1016/j.tem.2012.06.003
Lenin R, Sankaramoorthy A, Mohan V, Balasubramanyam M (2015) Altered immunometabolism at the interface of increased endoplasmic reticulum (ER) stress in patients with type 2 diabetes. J Leukocyte Biol 98:615–622. doi:10.1189/jlb.3A1214-609R
Park KY, Kim B, Hyun CK (2015) Lactobacillus rhamnosus GG improves glucose tolerance through alleviating ER stress and suppressing macrophage activation in db/db mice. J Clin Biochem Nutr 56:240–246. doi:10.3164/jcbn.14-116
Bleau C, Karelis AD, St-Pierre DH, Lamontagne L (2015) Crosstalk between intestinal microbiota, adipose tissue and skeletal muscle as an early event in systemic low-grade inflammation and the development of obesity and diabetes. Diabetes Metab Res Rev 31:545–561. doi:10.1002/dmrr.2617
Yoo SR, Kim YJ, Park DY, Jung UJ, Jeon SM, Ahn YT, Huh CS, McGregor R, Choi MS (2013) Probiotics L. plantarum and L. curvatus in combination alter hepatic lipid metabolism and suppress diet-induced obesity. Obesity (Silver Spring) 21:2571–2578. doi:10.1002/oby.20428
Firouzi S, Majid HA, Ismail A, Kamaruddin NA, Barakatun-Nisak M-YY (2016) Effect of multi-strain probiotics (multi-strain microbial cell preparation) on glycemic control and other diabetes-related outcomes in people with type 2 diabetes: a randomized controlled trial. Eur J Nutr. doi:10.1007/s00394-016-1199-8
Rajkumar H, Kumar M, Das N, Kumar SN, Challa HR, Nagpal R (2015) Effect of probiotic lactobacillussalivarius UBL S22 and prebiotic fructo-oligosaccharide on serum lipids, inflammatory markers, insulin sensitivity, and gut bacteria in healthy young volunteers: a randomized controlled single-blind pilot study. J Cardiovascularpharmacol Therap 20:289–298
Sun J, Buys NJ (2016) Glucose- and glycemic factor lowering effects of probiotics on diabetes: a meta-analysis of randomisedplacebo-controlled trials. Br J Nutr 115:1167–1177
Tonucci LB, Olbrich Dos Santos KM, Licursi de Oliveira L, Rocha Ribeiro SM, Duarte Martino HS (2015) Clinical application of probiotics in type 2 diabetes mellitus: A randomized, double-blind, placebo-controlled study. Clin Nutr. doi:10.1016/j.clnu.2015.11.011
Sáez-Lara MJ, Robles-Sanchez C, Ruiz-Ojeda FJ, Plaza-Diaz J, Gil A (2016) Effects of probiotics and synbiotics on obesity, insulin resistance syndrome, type 2 diabetes and non-alcoholic fatty liver disease: a review of human clinical trials. Int J Mol Sci 13;17: pii: E928. doi:10.3390/ijms17060928
Acknowledgments
Financial assistance from Department of Biotechnology (DBT, New Delhi, Government of India) is greatly acknowledged. BM acknowledges Council of Scientific and Industrial Research (CSIR), New Delhi for Research Associateship.
Authors contributions
MB conceived, designed, supervised, and commented on all drafts of this paper. BM, DP, PP, CS, SR, AS, NR and RK coordinated the animal study, conducted the overall experiments and participated in the data collection and analysis, molecular investigations and helped in the drafts. VM, SG, VKB, and MB contributed to data interpretation and manuscript completion.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was conducted as per the compliance of Committee for the Purpose of Control And Supervision of Experiments on Animals (CPCSEA) guidelines, Government of India.
Conflict of interest
The authors have no conflict of interest to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Balakumar, M., Prabhu, D., Sathishkumar, C. et al. Improvement in glucose tolerance and insulin sensitivity by probiotic strains of Indian gut origin in high-fat diet-fed C57BL/6J mice. Eur J Nutr 57, 279–295 (2018). https://doi.org/10.1007/s00394-016-1317-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-016-1317-7