Abstract
Purpose
Cheese contains a high content of saturated fatty acids but also lists of potentially beneficial nutrients. How long-term cheese consumption affects the development of cardiovascular disease (CVD) is unclear. A meta-analysis of prospective observational studies was conducted to evaluate the risks of total CVD, coronary heart disease (CHD), and stroke associated with cheese consumption.
Methods
Potentially eligible studies were identified by searching PubMed and EMBASE databases and by carefully reviewing the bibliographies of retrieved publications and related reviews. The summary relative risks (RRs) with 95 % confidence intervals (CIs) were calculated using the random-effects model.
Results
The final analyses included 15 prospective studies. Most of the studies excluded prevalent CVD at baseline (14/15) and had a duration >10 years (13/15). The summary RR for high vs. low cheese consumption was 0.90 (95 % CI 0.82–0.99) for total CVD (7 studies, 8076 events), 0.86 (95 % CI 0.77–0.96) for CHD (8 studies, 7631 events), and 0.90 (95 % CI 0.84–0.97) for stroke (7 studies, 10,449 events), respectively. The restricted cubic model indicated evidence of nonlinear relationships between cheese consumption and risks of total CVD (P nonlinearity < 0.001) and stroke (P nonlinearity = 0.015), with the largest risk reductions observed at the consumption of approximately 40 g/d.
Conclusions
This meta-analysis of prospective studies suggests a nonlinear inverse association between cheese consumption and risk of CVD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cheese is a widely consumed, easily digestible, and well-tolerated dairy product, with each person consuming 15.5 kg cheese per year (~42.5 g/d) in the USA and 17.9 kg in the Europe (~49.0 g/d) [1]. Cheese is a rich source of dietary calcium, with each 50 g of hard cheese containing approximately 360 mg of calcium [2]. For the purpose of maintaining bone health, cheese may be a good alternative of milk for individual who are lactose intolerant. On the other hand, cheese also contains a high content of saturated fatty acids (SFA) that could contribute to elevated low-density lipoprotein cholesterol (LDL-C), a well-defined risk factor for cardiovascular disease (CVD) [3]. Dietary guidelines recommend increasing intake of low-fat dairy and avoiding high-fat dairy products as parts of a balanced diet to prevent CVD [4, 5]. Despite large body of research conducted to evaluate the health effect of SFA, no definite conclusion of a deleterious effect has been drawn [6–10]. There has been evidence that SFA intake may affect health differentially by food sources [11–13], with reduced risks of CVD and type 2 diabetes (T2D) by dairy SFA intake and increased risks by meat SFA intake [12, 13].
The potential cardiovascular effects of cheese have also received great attention over the past two decades, with considerable animal studies and human intervention trials investigating the effects of cheese on CVD risk factors [14–17], along with prospective observational studies that examined whether long-term cheese consumption affects the development of CVD [13, 18–31]. Currently, there are limited certainties achieved. Two recent meta-analyses [32, 33] reported inverse associations of cheese consumption with risks of coronary heart disease (CHD) and/or stroke. The summary relative risk (RR) was 0.84 (95 % confidence interval [CI] 0.71–1.00) for CHD in the analysis by Qin et al. [33] (seven cohorts), and the summary RR was 0.94 (95 % CI 0.89–1.00) for stroke in the one by Hu et al. [32] (six cohorts). However, since the amounts of cheese consumed varied substantially across different populations (e.g., individuals who were classified in the lowest category of cheese consumption in some studies [23, 26] may be classified as the highest category in others [19, 20, 28]), high vs. low analyses are less interpretable than dose–response analyses. A dose–response meta-analysis can provide a solution to the problem with distinct ranges of exposure in different studies and would better quantify the association. Furthermore, a number of other studies that evaluated the risk of CHD [20], stroke [22], or total CVD [13, 19, 30, 31] associated with cheese consumption were not included in the previous meta-analyses. In addition, potential nonlinear relationship between cheese consumption and risk of CVD remains to be determined. It is relevant to both scientific research and public to understand any threshold effects of cheese consumption on CVD development given the evidence that cheese consumption may be detrimental to certain diseases (e.g., prostate cancer and Parkinson’s disease) [34, 35]. To fill these scientific gaps, a meta-analysis was carried out.
Materials and methods
Data search
This study was planned, conducted, and reported in adherence to the guidelines of the “Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group” [36]. A literature search was performed on PubMed (January 1, 1966–December 15, 2015) and EMBASE (January 1, 1980–December 30, 2015) databases using the search strategy as follows: (dairy OR cheese) and (cardiovascular OR heart disease OR myocardial infarction OR stroke) and (cohort OR prospective OR nested). Bibliographies in the retrieved full articles and previous meta-analyses [11, 32, 33, 37] as well as related reviews [17] were also carefully hand searched for additional studies. Attempts were also made to contact relevant authors for additional information [13, 30, 31].
Study selection
Studies that met the following criteria were considered: (1) The study design was prospective; (2) the exposure of interest was cheese consumption; (3) the outcome of interest was fatal/nonfatal CVD, CHD, or stroke; (4) RRs with corresponding 95 % CIs were reported or could be estimated. When multiple publications from the same study were available, the one with the most comprehensive data (e.g., reporting disease subtypes or providing data for dose–response analysis) was selected. We only considered prospective studies because they collected exposure information before the diagnosis of disease and were less prone to biases (e.g., recall and selection biases) than retrospective case-control studies.
Data extraction and quality assessment
Using a standardized data-collection form, the following data were extracted from each included study: the first author’s last name, publication year, country of origin, study name, study duration, age and sex of participants, number of events and participants, categories of cheese consumption, the maximally adjusted RRs with 95 % CIs for each category of cheese consumption or for per unit increase in cheese consumption, prevalent diseases excluded at baseline, and variables accounted for in the statistical model. The study quality was evaluated using the 9-star Newcastle-Ottawa Scale (NOS) [38]. Literature selection, data extraction, and quality assessment were conducted independently by two authors (G-CC and L-QQ), with any disagreement resolved by consensus.
Statistical analysis
A DerSimonian and Laird random-effects model [39], which considers both within- and between-study variation, was assigned to calculate the summary risk estimates. Separate meta-analyses were conducted for the outcomes of overall CVD, CHD, and stroke across this study. Results reported by sex, CVD subgroup (CHD and stroke), or stroke subtype without an overall risk estimate were pooled with a fixed-effects model, and the combined estimates were included in the main analyses. First, we pooled estimates for the highest compared with lowest categories of cheese consumption. There were three studies [13, 30, 31] that reported results as per unit increase in cheese consumption. Attempts were made to contact relevant authors for the risk estimates comparing extreme categories of cheese consumption, but no eligible responses were received. Thus, RRs reported in the European Prospective Investigation into Cancer and Nutrition (EPIC)-Potsdam cohort [31] (for cheese per 30 g/d) and the Multi-Ethnic Study of Atherosclerosis [13] (for cheese per 1 serving/d) were directly used in the high versus low analysis because the levels of consumption in the two studies were each comparable with the means of the upper cheese categories in another EPIC cohort [27] (per 30.2 g/d) or in other two US cohorts [20, 22] (1 serving/d). For the Dutch cohort of the Hoorn Study [30] that reported results as per 23 g/d of cheese consumption, we calculated new RRs with 95 % CIs for a 43-g/d increment, which approximates the means of the highest categories of two studies [21, 27] from the Netherlands. A number of subgroup analyses were conducted according to area, disease outcome (fatal, or fatal and nonfatal combined), sex, duration of follow-up, fat content of cheese, quality score, age, prevalent diseases excluded at baseline.
Subsequently, we conducted a dose–response analysis by use of the method proposed by Greenland and Longnecker [40] and Orsini et al. [41]. Accordingly, the number of cases and person-years and the risk estimates with their variance for at least three quantitative exposure categories were extracted. Most studies reported cheese in weight (g), and we converted the intake into g by using 43 g as a serving size for the studies that reported the consumption in frequency without providing a serving size [34, 42]. Afterward, we pooled study-specific risk estimates with the random-effects model. To be consistent with previous meta-analyses [34, 42] on cheese consumption, the results of linear dose–response in the forest plot were presented for a 50-g/d increment. We further examined a potential nonlinear relationship between cheese consumption and CVD risk by modeling exposure levels using restricted cubic splines with three knots at percentiles 10, 50, and 95 % of the distribution [43, 44]. A P value for nonlinearity was calculated by testing the null hypothesis that the coefficient of the second spline is equal to zero.
Heterogeneity test was performed using Q and I 2 statistics [45]. For the Q statistic, P < 0.1 was considered as statistically significant; and for the I 2 statistic, the following cutoff points were used: <30 % (little or no heterogeneity), 30–75 % (moderate heterogeneity), and >75 % (high heterogeneity). Potential publication bias was investigated using Begg’s rank correlation test, Egger’s linear regression test, and Begg’s funnel plots [46, 47]. We also used the “trim-and-fill” method [48] to correct such a bias. All statistical analyses were performed using STATA software, version 11.0 (STATACorp, College Station, TX, USA).
Results
Study selection and characteristics
A flow chart of study selection is reported in Fig. 1. Briefly, a total of 377 independent citations were identified after duplicates exclusion, of which 27 were retrieved for more detailed reviews. Fourteen publications were excluded after carefully reading the full texts. Most of these reports were excluded because they studied total dairy without data on cheese consumption (N = 6), or cheese were included in specific diet patterns (N = 6). Further excluded were one publication [49] that was an overlapping report of another [27] with more comprehensive data for the dose–response analyses and one publication [50] where risk estimate cannot be extracted or calculated. Finally, 15 independent prospective studies that investigated the relationship between cheese consumption and risk of total and/or individual CVD were included in this meta-analysis.
The characteristics of the included studies are summarized in Supplementary Table 1. The 15 studies were published between 1997 and 2015. The studies were largely from Europe (N = 10) or the USA (N = 4), with the exception of one [19] that was conducted in Australia. Most of the studies included both sexes, but two [22, 26] consisted of merely women and one [23] included entirely of male smokers. All but two studies [13, 31] had a follow-up duration of at least 10 years, and all except one study [19] excluded prevalent CVD at baseline, both of which contributed to the high scores of included studies. The details of quality assessment according to the 9-star NOC are presented in Supplementary Table 2. Eight of these studies were given scores of ≥8. Overall, there were seven studies [13, 19, 21, 27, 29–31] on overall CVD (8076 events), eight studies [18, 20, 21, 25–29] on CHD (7631 events), and seven studies (six publications [21–24, 27, 29] including one [24] that contained two independent cohorts) on stroke (10,449 events).
Main analysis
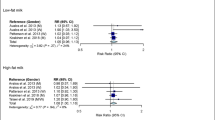
A meta-analysis of the included studies showed that the summary RR for the highest compared with lowest categories of cheese consumption was, respectively, 0.90 (95 % CI 0.82–0.99) for total CVD, 0.86 (95 % CI 0.77–0.96) for CHD, and 0.90 (95 % CI 0.84–0.97) for stroke, with little evidence of heterogeneity (P heterogeneity = 0.58, 0.31, and 0.42, respectively; and I 2 = 0, 14.9, and 0 %, respectively) (Fig. 2).
Subgroup and sensitivity analyses
Results of stratified analysis by various pre-specified study and population characteristics are shown in Table 1. Cheese consumption was inversely associated with CVD, CHD, and stroke in most of the subgroups. There was a suggestion that the observed cardiovascular benefits of cheese consumption may be sex-specific, with a significant inverse association in women but not in men. However, the differences between sexes were not statistically significant. Few studies reported findings by the fat content of cheese, and there was no indication of an adverse effect of high-fat cheese consumption on overall CVD risk (RR = 0.74, 95 % CI 0.44–1.24).
Dose–response analysis
Two studies [18, 22] were not eligible for this analysis because risk estimates for only two cheese categories were available. The dose-risk meta-analysis of the remaining studies showed that the summary RR for cheese consumption of 50 g/d was 0.92 (95 % CI 0.83–1.02) for total CVD, 0.90 (95 % CI 0.84–0.95) for CHD, and 0.94 (95 % CI 0.85–1.04) for stroke, respectively (Fig. 3). There was a somewhat U-shaped association between cheese consumption and risk of total CVD (P nonlinearity < 0.001) (Fig. 4), with the largest reductions in risk observed at cheese consumption of approximately 40 g/d. Stratifying by disease subtypes, the nonlinearity was found for the association with stroke (P nonlinearity = 0.015) but not with CHD (P nonlinearity = 0.427) (Fig. 4).
Publication bias
Neither Begg’s test nor Egger’s test suggested publication bias with regard to CVD or stroke risk associated with cheese consumption (all P values > 0.10). In terms of CHD risk, Egger’s test (P = 0.04) but not Begg’s test (P = 0.17) suggested evidence of a publication bias. The asymmetry in the Begg’s funnel plot (Fig. 5) indicates that smaller studies with null effects, which would be expected to locate at the lower right corner of the plot, may have been unpublished. Using “trim-and-fill” method to correct the bias, only the summary RR of CHD was slightly changed with three missing studies imputed (RR = 0.83, 95 % CI 0.73–0.94).
Discussion
In this large meta-analysis of 15 generally well-designed prospective studies, we found that high compared with low cheese consumption was significantly associated with 10–14 % lower risks of CVD and its subgroups. Furthermore, there was a somewhat U-shaped association between cheese consumption and overall CVD risk, with the largest risk reduction observed at cheese consumption of approximately 40 g/d. The lack of significance in the linear dose–response analyses of CVD or stroke in relation to cheese consumption may be because the linear model does not fit well with the data covering a nonlinear trend.
Potential mechanisms whereby cheese may reduce CVD have been well discussed by Hjerpsted and Tholstrup [17]. Cheese is a good source of dietary vitamins, minerals, and protein, all of which may be of cardiovascular protective properties. Interestingly, two recent meta-analyses of prospective studies reported a U-shaped association between dietary calcium and risk of CVD mortality [51] or risk of stroke [52], which are agreement with our results of a nonlinear relationship between cheese consumption and risk of CVD or stroke. Cheese is also rich in conjugated linoleic acid, which has been suggested to prevent the progression of atherosclerosis in animal models [53] and decrease inflammatory response in human [54]. Clinical trials showed that cheese intervention increased high-density lipoprotein cholesterol (HDL-C) and/or reduced LDL-C [14, 16], and one of the contributors to the improved lipid profile may be the probiotics (added or emerging during the fermentation process) in cheese [55, 56]. Evidence from prospective studies showed significant inverse associations between cheese consumption and risks of metabolic syndrome (MetS) [57] and T2D [42], and the association with T2D also appeared nonlinear, with the largest risk reduction around cheese consumption of 50–60 g/d [42].
Low-fat dairy are considered more favorable than high-fat dairy in dietary guidelines [4, 5], mainly because of their lower content of SFA. However, the health effects of SFA intake remain uncertain. Recent meta-analyses of long-term prospective studies showed neutral effects of SFA intake on risk of CVD or T2D [6, 7]. Conversely, more recent prospective findings reported increased risk of all-cause and/or case-specific mortality associated with SFA intake in a population at high risk for CVD [8], in nurses and health professionals [9], as well as in elderly women [10]. The source of SFA matters [11–13]. Prospective evidence suggests decreased risk of CVD and T2D by dairy SFA intake and increased risks by meat SFA intake [12, 13]. In a recent randomized controlled trial [15] of 153 participants, high-fat cheese intervention of 8 weeks did not increase total cholesterol or LDL-C, but reduced triglycerides among subjects with MetS at baseline. We observed a nonsignificant inverse association of high-fat cheese consumption with overall CVD risk (RR = 0.74, 95 % CI 0.44–1.24). Taken together, there has been limited evidence of an adverse effect of high-fat dairy consumption on major health outcomes.
Our subgroup analysis indicated that the cardiovascular benefits of cheese consumption may be sex-specific, although the difference between sexes was not statistically significant, possibly due to the limited power by including a small number of studies. In a large-scale, cross-sectional survey of 10,872 US population (NHANES III) [58], higher HDL-C and lower LDL-C were observed in women with high cheese consumption (P trend < 0.05) whereas men consuming higher cheese had higher adiposity measures, HDL-C and LDL-C, and diastolic blood pressure (P trend < 0.05). In the Malmo Diet and Cancer study [29], a cohort of 26,445 Swedish men and women, high versus low cheese consumption was associated with reduced risk of CVD in women (RR = 0.82, P trend = 0.03), but not in men (RR = 0.99, P trend = 0.98). Houston et al. [58] discussed that the difference may be due to the fact that women consumed more low-fat cheese than men, whereas Sonestedt et al. [29] tended to ascribe the difference to the less accurate measurement of cheese consumption in men than in women. We considered additional explanations including: (1) Some residual or unmeasured confounders differentially associated with cheese consumption and/or CVD risk in men and women; and (2) hormonal, genetic, and metabolic factors may affect the biology of how cheese consumption affects CVD risk.
This meta-analysis presents several strengths. Apart from the prospective design of original studies and the large number of events involved in the analyses, most of the individual studies had a long duration and excluded various chronic diseases (e.g., diabetes and CVD) at baseline. However, several limitations of this study should also be acknowledged. First, as this meta-analysis was based on observational studies, the potential impacts of residual/unknown confounders on our results cannot be completely excluded despite that most included studies have considered a wide range of confounders. Second, some misclassification of exposure in original studies appeared inevitable due to the use of self-reported food frequency questionnaires and the single collection of diet information at baseline. Such misclassification would most likely to be nondifferential and attenuate the true association. Third, whether the effects of cheese consumption on CVD vary according to fat content was not well addressed due to the limited data available. Fourth, the included studies were mostly from Europe and the USA, which limits the generalizability of our findings to other populations. Finally, our findings may have been affected by publication bias that results from a tendency to publish larger studies or studies with positive results.
In summary, this meta-analysis of prospective studies suggests a nonlinear inverse association between cheese consumption and risk of CVD. Future large prospective studies, in particular those investigating sex- and cheese subtype-specific differences, are warranted.
Change history
07 January 2019
In the original publication, the funding and conflict of interest statements were not correct.
07 January 2019
In the original publication, the funding and conflict of interest statements were not correct.
07 January 2019
In the original publication, the funding and conflict of interest statements were not correct.
References
Canadian Dairy Information Center. Global Consumption of Dairy Products (2013) http://www.dairyinfo.gc.ca/index_e.php?s1=dff-fcil&s2=cons&s3=consglo. Accessed 13 June 2016
Rozenberg S, Body JJ, Bruyere O, Bergmann P, Brandi ML, Cooper C, Devogelaer JP, Gielen E, Goemaere S, Kaufman JM, Rizzoli R, Reginster JY (2015) Effects of dairy products consumption on health: benefits and beliefs-a commentary from the Belgian Bone Club and the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases. Calcif Tissue Int 98:1–17
Mihaylova B, Emberson J, Blackwell L, Keech A, Simes J, Barnes EH, Voysey M, Gray A, Collins R, Baigent C (2012) The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet 380:581–590
Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren M, Albus C, Benlian P, Boysen G, Cifkova R, Deaton C, Ebrahim S, Fisher M, Germano G, Hobbs R, Hoes A, Karadeniz S, Mezzani A, Prescott E, Ryden L, Scherer M, Syvanne M, Scholte op Reimer WJ, Vrints C, Wood D, Zamorano JL, Zannad F (2012) European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Eur Heart J 33:1635–1701
Eckel RH, Jakicic JM, Ard JD, de Jesus JM, Houston Miller N, Hubbard VS, Lee IM, Lichtenstein AH, Loria CM, Millen BE, Nonas CA, Sacks FM, Smith SC Jr, Svetkey LP, Wadden TA, Yanovski SZ (2014) 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 63:2960–2984
de Souza RJ, Mente A, Maroleanu A, Cozma AI, Ha V, Kishibe T, Uleryk E, Budylowski P, Schunemann H, Beyene J, Anand SS (2015) Intake of saturated and trans unsaturated fatty acids and risk of all cause mortality, cardiovascular disease, and type 2 diabetes: systematic review and meta-analysis of observational studies. BMJ 351:h3978
Chowdhury R, Warnakula S, Kunutsor S, Crowe F, Ward HA, Johnson L, Franco OH, Butterworth AS, Forouhi NG, Thompson SG, Khaw KT, Mozaffarian D, Danesh J, Di Angelantonio E (2014) Association of dietary, circulating, and supplement fatty acids with coronary risk: a systematic review and meta-analysis. Ann Intern Med 160:398–406
Guasch-Ferre M, Babio N, Martinez-Gonzalez MA, Corella D, Ros E, Martin-Pelaez S, Estruch R, Aros F, Gomez-Gracia E, Fiol M, Santos-Lozano JM, Serra-Majem L, Bullo M, Toledo E, Barragan R, Fito M, Gea A, Salas-Salvado J, Investigators PS (2015) Dietary fat intake and risk of cardiovascular disease and all-cause mortality in a population at high risk of cardiovascular disease. Am J Clin Nutr 102:1563–1573
Wang DD, Li Y, Chiuve SE, Stampfer MJ, Manson JE, Rimm EB, Willett WC, Hu FB (2016) Association of specific dietary fats with total and cause-specific mortality. JAMA Intern Med. 176:1134–1145
Blekkenhorst LC, Prince RL, Hodgson JM, Lim WH, Zhu K, Devine A, Thompson PL, Lewis JR (2015) Dietary saturated fat intake and atherosclerotic vascular disease mortality in elderly women: a prospective cohort study. Am J Clin Nutr 101:1263–1268
O’Sullivan TA, Hafekost K, Mitrou F, Lawrence D (2013) Food sources of saturated fat and the association with mortality: a meta-analysis. Am J Public Health 103:e31–e42
Ericson U, Hellstrand S, Brunkwall L, Schulz CA, Sonestedt E, Wallstrom P, Gullberg B, Wirfalt E, Orho-Melander M (2015) Food sources of fat may clarify the inconsistent role of dietary fat intake for incidence of type 2 diabetes. Am J Clin Nutr 101:1065–1080
de Oliveira Otto MC, Mozaffarian D, Kromhout D, Bertoni AG, Sibley CT, Jacobs DR Jr, Nettleton JA (2012) Dietary intake of saturated fat by food source and incident cardiovascular disease: the Multi-Ethnic Study of Atherosclerosis. Am J Clin Nutr 96:397–404
Hjerpsted J, Leedo E, Tholstrup T (2011) Cheese intake in large amounts lowers LDL-cholesterol concentrations compared with butter intake of equal fat content. Am J Clin Nutr 94:1479–1484
Nilsen R, Hostmark AT, Haug A, Skeie S (2015) Effect of a high intake of cheese on cholesterol and metabolic syndrome: results of a randomized trial. Food Nutr Res. 59:27651
Thorning TK, Raziani F, Bendsen NT, Astrup A, Tholstrup T, Raben A (2015) Diets with high-fat cheese, high-fat meat, or carbohydrate on cardiovascular risk markers in overweight postmenopausal women: a randomized crossover trial. Am J Clin Nutr 102:573–581
Hjerpsted J, Tholstrup T (2016) Cheese and cardiovascular disease risk: a review of the evidence and discussion of possible mechanisms. Crit Rev Food Sci Nutr 56:1389–1403
Avalos EE, Barrett-Connor E, Kritz-Silverstein D, Wingard DL, Bergstrom JN, Al-Delaimy WK (2013) Is dairy product consumption associated with the incidence of CHD? Public Health Nutr. 16:2055–2063
Bonthuis M, Hughes MC, Ibiebele TI, Green AC, van der Pols JC (2010) Dairy consumption and patterns of mortality of Australian adults. Eur J Clin Nutr 64:569–577
Fraser GE, Shavlik DJ (1997) Risk factors for all-cause and coronary heart disease mortality in the oldest-old. The Adventist Health Study. Arch Intern Med 157:2249–2258
Goldbohm RA, Chorus AM, Galindo Garre F, Schouten LJ, van den Brandt PA (2011) Dairy consumption and 10-y total and cardiovascular mortality: a prospective cohort study in the Netherlands. Am J Clin Nutr 93:615–627
Iso H, Stampfer MJ, Manson JE, Rexrode K, Hennekens CH, Colditz GA, Speizer FE, Willett WC (1999) Prospective study of calcium, potassium, and magnesium intake and risk of stroke in women. Stroke 30:1772–1779
Larsson SC, Mannisto S, Virtanen MJ, Kontto J, Albanes D, Virtamo J (2009) Dairy foods and risk of stroke. Epidemiology 20:355–360
Larsson SC, Virtamo J, Wolk A (2012) Dairy consumption and risk of stroke in Swedish women and men. Stroke 43:1775–1780
Mann JI, Appleby PN, Key TJ, Thorogood M (1997) Dietary determinants of ischaemic heart disease in health conscious individuals. Heart 78:450–455
Patterson E, Larsson SC, Wolk A, Akesson A (2013) Association between dairy food consumption and risk of myocardial infarction in women differs by type of dairy food. J Nutr 143:74–79
Praagman J, Dalmeijer GW, van der Schouw YT, Soedamah-Muthu SS, Monique Verschuren WM, Bas Bueno-de-Mesquita H, Geleijnse JM, Beulens JW (2015) The relationship between fermented food intake and mortality risk in the European Prospective Investigation into Cancer and Nutrition-Netherlands cohort. Br J Nutr 113:498–506
Soedamah-Muthu SS, Masset G, Verberne L, Geleijnse JM, Brunner EJ (2013) Consumption of dairy products and associations with incident diabetes, CHD and mortality in the Whitehall II study. Br J Nutr 109:718–726
Sonestedt E, Wirfalt E, Wallstrom P, Gullberg B, Orho-Melander M, Hedblad B (2011) Dairy products and its association with incidence of cardiovascular disease: the Malmo diet and cancer cohort. Eur J Epidemiol 26:609–618
van Aerde MA, Soedamah-Muthu SS, Geleijnse JM, Snijder MB, Nijpels G, Stehouwer CD, Dekker JM (2013) Dairy intake in relation to cardiovascular disease mortality and all-cause mortality: the Hoorn Study. Eur J Nutr 52:609–616
von Ruesten A, Feller S, Bergmann MM, Boeing H (2013) Diet and risk of chronic diseases: results from the first 8 years of follow-up in the EPIC-Potsdam study. Eur J Clin Nutr 67:412–419
Hu D, Huang J, Wang Y, Zhang D, Qu Y (2014) Dairy foods and risk of stroke: a meta-analysis of prospective cohort studies. Nutr Metab Cardiovasc Dis 24:460–469
Qin LQ, Xu JY, Han SF, Zhang ZL, Zhao YY, Szeto IM (2015) Dairy consumption and risk of cardiovascular disease: an updated meta-analysis of prospective cohort studies. Asia Pac J Clin Nutr 24:90–100
Aune D, Navarro Rosenblatt DA, Chan DS, Vieira AR, Vieira R, Greenwood DC, Vatten LJ, Norat T (2015) Dairy products, calcium, and prostate cancer risk: a systematic review and meta-analysis of cohort studies. Am J Clin Nutr 101:87–117
Jiang W, Ju C, Jiang H, Zhang D (2014) Dairy foods intake and risk of Parkinson’s disease: a dose-response meta-analysis of prospective cohort studies. Eur J Epidemiol 29:613–619
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283:2008–2012
Soedamah-Muthu SS, Ding EL, Al-Delaimy WK, Hu FB, Engberink MF, Willett WC, Geleijnse JM (2011) Milk and dairy consumption and incidence of cardiovascular diseases and all-cause mortality: dose-response meta-analysis of prospective cohort studies. Am J Clin Nutr 93:158–171
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P (2013) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. www.ohri.ca/programs/clinical_epidemiology/oxford.htm
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Greenland S, Longnecker MP (1992) Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol 135:1301–1309
Orsini N, Bellocco R, Greenland S (2006) Generalized least squares for trend estimation of summarized dose-respose data. Stata J 6:40–57
Aune D, Norat T, Romundstad P, Vatten LJ (2013) Dairy products and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of cohort studies. Am J Clin Nutr 98:1066–1083
Orsini N, Li R, Wolk A, Khudyakov P, Spiegelman D (2012) Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol 175:66–73
Wang X, Ouyang Y, Liu J, Zhu M, Zhao G, Bao W, Hu FB (2014) Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: systematic review and dose-response meta-analysis of prospective cohort studies. BMJ 349:g4490
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088–1101
Duval S, Tweedie R (2000) Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56:455–463
Dalmeijer GW, Struijk EA, van der Schouw YT, Soedamah-Muthu SS, Verschuren WM, Boer JM, Geleijnse JM, Beulens JW (2013) Dairy intake and coronary heart disease or stroke–a population-based cohort study. Int J Cardiol 167:925–929
Gartside PS, Wang P, Glueck CJ (1998) Prospective assessment of coronary heart disease risk factors: the NHANES I epidemiologic follow-up study (NHEFS) 16-year follow-up. J Am Coll Nutr 17:263–269
Wang X, Chen H, Ouyang Y, Liu J, Zhao G, Bao W, Yan M (2014) Dietary calcium intake and mortality risk from cardiovascular disease and all causes: a meta-analysis of prospective cohort studies. BMC Med 12:158
Larsson SC, Orsini N, Wolk A (2013) Dietary calcium intake and risk of stroke: a dose-response meta-analysis. Am J Clin Nutr 97:951–957
Mitchell PL, McLeod RS (2008) Conjugated linoleic acid and atherosclerosis: studies in animal models. Biochem Cell Biol 86:293–301
Mullen A, Moloney F, Nugent AP, Doyle L, Cashman KD, Roche HM (2007) Conjugated linoleic acid supplementation reduces peripheral blood mononuclear cell interleukin-2 production in healthy middle-aged males. J Nutr Biochem 18:658–666
Cho YA, Kim J (2015) Effect of probiotics on blood lipid concentrations: a meta-analysis of randomized controlled trials. Med (Baltim) 94:e1714
Sofi F, Buccioni A, Cesari F, Gori AM, Minieri S, Mannini L, Casini A, Gensini GF, Abbate R, Antongiovanni M (2010) Effects of a dairy product (pecorino cheese) naturally rich in cis-9, trans-11 conjugated linoleic acid on lipid, inflammatory and haemorheological variables: a dietary intervention study. Nutr Metab Cardiovasc Dis 20:117–124
Chen GC, Szeto IM, Chen LH, Han SF, Li YJ, van Hekezen R, Qin LQ (2015) Dairy products consumption and metabolic syndrome in adults: systematic review and meta-analysis of observational studies. Sci Rep 5:14606
Houston DK, Driver KE, Bush AJ, Kritchevsky SB (2008) The association between cheese consumption and cardiovascular risk factors among adults. J Hum Nutr Diet 21:129–140
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chen, GC., Wang, Y., Tong, X. et al. Cheese consumption and risk of cardiovascular disease: a meta-analysis of prospective studies. Eur J Nutr 56, 2565–2575 (2017). https://doi.org/10.1007/s00394-016-1292-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-016-1292-z