Abstract
Introduction
Chronic inflammation is associated with increased risk of cancer, cardiovascular disease (CVD), and diabetes. The role of pro-inflammatory diet in the risk of cancer mortality and CVD mortality in prediabetics is unclear. We examined the relationship between diet-associated inflammation, as measured by dietary inflammatory index (DII) score, and mortality, with special focus on prediabetics.
Methods
This prospective cohort study used data from the Third National Health and Nutrition Examination Survey (NHANES III). We categorized 13,280 eligible participants, ages 20–90 years, according to glycosylated hemoglobin (HgbA1c) level and identified 2681 with prediabetes, defined as a glycosylated hemoglobin percentage of 5.7–6.4. Computation of DII scores and all statistical analyses were conducted in 2015. The DII was computed based on baseline dietary intake assessed using 24-h dietary recalls (1988–1994). Mortality was determined from the National Death Index records through 2006. Over follow-up ranging between 135 and 168 person-months, a total of 3016 deaths were identified, including 676 cancer, 192 lung cancer, 176 digestive-tract cancer, and 1328 CVD deaths. Cox proportional hazard regression was used to estimate hazard ratios.
Results
The prevalence of prediabetes was 20.19 %. After controlling for age, sex, race, HgbA1c, current smoking, physical activity, BMI, and systolic blood pressure, DII scores in tertile III (vs tertile I) was significantly associated with mortality from all causes (HR 1.39, 95 % CI 1.13, 1.72), CVD (HR 1.44, 95 % CI 1.02, 2.04), all cancers (HR 2.02, 95 % CI 1.27, 3.21), and digestive-tract cancer (HR 2.89, 95 % CI 1.08, 7.71). Findings for lung cancer (HR 2.01, 95 % CI 0.93, 4.34) suggested a likely effect. These results were moderately enhanced after additional adjustment for serum low-density lipoprotein and triglyceride and following eliminating deaths during the first year.
Conclusions
A pro-inflammatory diet, as indicated by higher DII scores, is associated with an increased risk of all-cause, CVD, all-cancer, and digestive-tract cancer mortality among prediabetic subjects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prediabetes is a condition characterized by an elevated blood glucose level that is not high enough to warrant a diagnosis of type 2 diabetes mellitus (T2DM). Prediabetes is defined by the presence of impaired fasting glucose (IFG) and/or impaired glucose tolerance (IGT) [1–3]. According to the National Health and Nutrition Examination Survey (NHANES), in 2005–2006, 35 % of US adults ≥20 years of age had prediabetes (50 % of adults ≥ 65 years) [4, 5]. It is estimated that up to 70 % of people with prediabetes may develop T2DM during their lifetimes [5–7]. Without lifestyle change, 15–30 % people with prediabetes will develop T2DM within 5 years [5–7]. Epidemiologic studies have shown that prediabetes is associated with an increased risk of CVD and certain types of cancer, especially liver, endometrial, stomach, and colorectal cancers [8, 9].
Although prediabetes, T2DM, CVD, and cancer share numerous common risk factors, such as age, obesity, lack of physical activity, and poor diet, the etiology and pathogenesis underlying the association between T2DM, CVD, and cancer are not clear [3, 10, 11]. There is accumulating evidence that chronic inflammation plays a role in the development of T2DM, cancer, and CVD [12–16]. Diet is an important regulatory factor in chronic inflammation. There is considerable evidence to suggest that “healthy” fats, such as omega-3 fatty acids, olive oil, and flaxseed oil, and high-fiber foods, such as whole grain and most fruits and vegetables, have anti-inflammatory potential [17–24]. On the other hand, most diets include pro-inflammatory components such as red meat and dairy products such as processed cheese and butter, which are rich in saturated fatty acids and trans-fatty acids [17–25].
The Dietary Inflammatory Index (DII) is a new tool to assess overall inflammatory potential of diet. The DII is based on an extensive literature search incorporating cell culture, animal, and epidemiologic studies on the effect of one or more of six inflammatory markers [i.e., C-reactive protein (CRP), interleukin (IL)-1beta, IL-4, IL-6, IL-10, and tumor necrosis factor (TNF)-α] [26, 27]. The DII is not limited to micronutrients and macronutrients, but also incorporates commonly consumed components of the diet including flavonoids, spices, and tea [26, 27]. The DII has been shown to be associated with inflammation [28–30], cancer [31–33], and CVD [34] outcomes.
The role of pro-inflammatory diet in the risk of cancer mortality and CVD mortality in people with prediabetes is unclear. The objective of this study is to examine the relationship between pro-inflammatory diet, as indicated by a high DII score, and the risk of all-cause, CVD, all-cancer, and cancer-site-specific cancer mortality in the NHANES population with a focus on prediabetic individuals.
Methods
The data source was the Third National Health and Nutrition Examination Survey (NHANES III), which was conducted between 1988 and 1994 by the National Center for Health Statistics (NCHS) of the Centers for Disease Control and Prevention (CDC). It is a nationally representative sample of the civilian, non-institutionalized US population. Details of the survey design have been reported previously [35]. The current study was restricted to participants, ages 20–90 years, with complete data on mortality status, diet, and relevant covariates (n = 13,280). The participants were categorized based on glycosylated hemoglobin percentage as normal group (n = 9631, HgbA1c < 5.7 %), prediabetic group (n = 2681, HgbA1c: 5.7–6.4 %), and diabetic group (n = 968, HgbA1c > 6.4 %) [2]. Glycosylated hemoglobin measurements for NHANES III were performed by the Diabetes Diagnostic Laboratory at the University of Missouri–Columbia using the Diamat Analyzer System (Bio-Rad Laboratories, Hercules, CA) [35]. CRP level was analyzed by a modification of the Behring Latex-Enhanced CRP assay on the Behring Nephelometer Analyzer System™ (Behring Diagnostics, Westwood, MA) [35]. Average systolic blood pressure (SBP) and diastolic blood pressure (DBP) were the arithmetic means of six or fewer measurements obtained at the household interview (maximum of three) and the Mobile Examination Center (maximum of three) [35]. Standing height and weight were obtained during the physical examination and were used to calculate body mass index [BMI = weight (kg)/weight (m)2]. Ethical approval was obtained from CDC/NCHS Ethics Review Board, and informed consent was obtained from all participants.
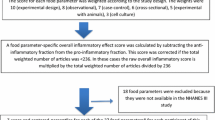
All NHANES participants are eligible for the dietary interview component. The dietary interviewer records detailed information about the foods and beverages reported using a computer-assisted dietary interview software program [35]. Computation of DII scores and all statistical analyses were conducted in 2015. Dietary data collected from 24-h diet recall interviews (24HR) were used to calculate DII scores for all participants as previously described [26, 27]. Briefly, total intake of food energy (calories), nutrients, and non-nutrient food components from foods and beverages that were consumed during the 24-h period prior to the interview (midnight to midnight) were estimated from the 24HR. Following the 24HR, a short questionnaire was administered to ascertain whether the person’s intake on the previous day was usual or unusual, the source of tap water consumed, use of salt, special diet use, and frequency of fish and shellfish consumption during the past 30 days. To calculate DII scores for the participants, the dietary data were first linked to the world database that provided an estimate of a mean and standard deviation for each parameter [26, 27]. These then become the multipliers to express an individual’s exposure relative to the “standard global mean” as a z score. This is achieved by subtracting the “standard global mean” from the amount reported and dividing this value by the standard deviation. To minimize the effect of “right skewing,” this value is then converted to a centered percentile score. The centered percentile score for each food parameter for each individual was then multiplied by the respective food parameter effect score, which is derived from the literature review, in order to obtain a food parameter-specific DII score for an individual. All of the food parameter-specific DII scores are then summed to create the overall DII score for every participant in the study [26, 27]. Across the 11 datasets that comprise the standard global mean, the DII scores ranged from –8.87 (maximally anti-inflammatory) to +7.98 (maximally pro-inflammatory) and the median was +0.23 [26, 27]. In most studies, the values range from about −4.5 to +4.5. For this study, 27 of the 45 food parameters were available for DII calculation: energy, carbohydrate, protein, fat, alcohol, fiber, cholesterol, saturated fatty acid, mono-unsaturated fatty acid, poly-unsaturated fatty acid, niacin, thiamin, riboflavin, vitamin B12, vitamin B6, iron, magnesium, zinc, selenium, vitamin A, vitamin C, vitamin D, vitamin E, folic acid, beta carotene, omega 6, and omega 3. DII was further categorized as tertiles: I (<−0.20), II (−0.20 to 2.0), and III (>2.0). In previous validation work in the SEASONS Study, there was no drop off in predictive ability with a reduction in parameters of this magnitude [36].
In the NHANES III cohort study, mortality information is derived on the basis of a probabilistic match between NHANES III and the National Death Index records through 31 December, 2006, by the National Center. For overall mortality, we included deaths from all causes; for CVD-related mortality, we included diseases of the heart and circulation system (ICD-10 = I00-I178); for cancer-specific mortality, we included deaths from malignant neoplasms which were coded from C00-C97 in the International Classification of Diseases, 10th Edition, Clinical Modification System codes (ICD-10). Digestive-tract cancers included malignant neoplasms from the front of the mouth to the rectum and malignant neoplasms of pancreas and hepato-biliary system (ICD-10 = C00-C16, C18-C22, C25). For lung cancer, we included malignant neoplasms of trachea, bronchus, and lung (C33-C34).
The HgbA1c level, CRP level, SBP level, DBP level, demographic factors (age, sex, race), lifestyle factors (current smoking, leisure time physical activity), and BMI among the three different groups were examined using ANOVA models or χ2 tests (see Table 1 for specific variables). DII scores were analyzed as a categorical variable by tertiles of exposure in relation to various mortality outcome variables, including all-cause, overall cancer, digestive-tract cancer and CVD-related mortalities, and lung cancer mortalities. Hazard ratios and 95 % confidence intervals (HR; 95 % CI) were estimated using Cox proportional hazards regression models, adjusting only for age, gender, and race in the crude model and additionally adjusting for BMI, current smoking, SBP, HgbA1c, and leisure physical activity. A linear test for trend was conducted by including the median value for each DII tertile as a continuous term into the regression model. The assumption of proportional hazards was tested by adding to the model an interaction term between follow-up time and DII; there was no evidence that these assumptions were violated. Sensitivity analysis was done by eliminating mortality during the first year after inclusion/providing recall data. Further analysis was done by additionally adjusting for serum low-density lipoprotein (LDL) and triglycerides (TG).
Data were weighted to account for the unequal probability of selection that resulted from the survey cluster design, non-response, and oversampling of certain target populations [35]. Sampling weights were used to calculate population estimates, and sampling strata and primary sampling units were accounted for to estimate variances and test for significant differences. All results are presented as unweighted counts (n), weighted percentages, and hazard ratios. Statistical tests were performed using SAS® 9.3, (SAS Institute Inc., Cary, NC); all statistical tests were two-sided, and p < 0.05 was considered statistically significant.
Results
A total of 13,280 participants, ages 20–90 years, with complete information of mortality and other covariates were included in the current study. Table 1 displays the baseline population characteristics from this nationally representative sample of normal individuals and individuals with prediabetes or T2DM. At baseline (1988–1994), according to glycosylated hemoglobin level, 7 % of them were classified as diabetic, 20 % prediabetic, and 73 % normal. There were more males than females in the prediabetic group (53.93 vs. 46.07 %) and T2DM group (59.36 vs. 40.64 %). A higher percentage of non-Hispanic Blacks were observed in the T2DM group (16.36 %) and prediabetic group (19.39 %) than in the normal group (8.10 %). The prediabetic group had the highest percentage current smokers at 33.41 %. The mean age, CRP level, HgbA1c level, BMI, systolic blood pressure, diastolic blood pressure, and DII score were significantly higher in the diabetes group compared to the normal and prediabetic group (Table 1). The average CRP levels were significantly different between groups, with the normal group having the lowest CRP level at 2.89, the diabetes group having the highest CRP level at 4.00, and the prediabetes group having an intermediate level at 3.47. The mean DII scores among the T2DM group (DII score = 0.88) or prediabetic group (DII score = 0.90) were significantly higher than for the normal group (DII score = 0.68). There was no significant difference in the mean DII score between the prediabetes and the T2DM group (Table 1).
Table 2 displays the mortality characteristic across different groups. The follow-up period ranged between 135 and 168 person-months. A total of 3016 deaths were identified, including 676 cancer deaths, 192 lung cancer deaths, 176 digestive-tract cancer deaths, and 1328 CVD deaths. A higher percentage of all-cause, CVD, all-cancer, digestive-tract cancer, and lung cancer deaths were observed in the T2DM group and the prediabetic group than the normal.
The association between pro-inflammatory diet, measured by high-tertile DII score and the risk of all-cause, CVD, all-cancer, digestive-tract cancer, and lung cancer mortality in the normal, prediabetes, and T2DM groups (tertile III vs. tertile I) was investigated in different models by adjusting different variables. After accounting for age, sex, and race as showed in Table 3, we observed a significantly higher risk for subjects in the third tertile compared to those in the first tertile for overall mortality in both the normal group (HR 1.46; 95 % CI 1.23–1.73, P trend < 0.0001) and the prediabetic group (HR 1.52; 95 % CI 1.26–1.85, P trend < 0.0001); for CVD mortality in both the normal group (HR 1.70; 95 % CI 1.31–2.21, P trend = 0.0001) and in the prediabetes group (HR 1.52, 95 % CI 1.10–2.11, P trend = 0.013); and for lung cancer mortality in both the normal (HR 1.77; 95 % CI 1.03–3.05; P trend = 0.002) and the prediabetes group (HR 2.45; 95 % CI 1.15–5.22; P trend = 0.002). The significantly higher risk of all-cancer mortality (HR 2.25; 95 % CI 1.39–3.65; P trend = 0.0014) and digestive-tract cancer mortality (HR 3.24; 95 % CI 1.21–8.64; P trend = 0.02) was only observed in the prediabetic group. The risk of all-cause, CVD, all-cancer, and digestive-tract cancer mortality was moderately attenuated after additional adjustment for HgbA1c, BMI, SBP, leisure time physical activity, and cigarette smoking. The risk of lung cancer mortality became nonsignificant after additional adjustment for other covariates. After adjustment for age, sex, race, HgbA1c, BMI, SBP, physical activity, and cigarette smoking in the prediabetic group as showed in Table 4, individuals with DII scores in tertile III had a 39 % higher risk of all-cause mortality (HR 1.39; 95 % CI 1.13–1.72; P trend = 0.003), a 44 % higher risk of CVD mortality (HR 1.44; 95 % CI 1.02–2.04; P trend = 0.04), a 102 % higher risk of all-cancer mortality (HR 2.02; 95 % CI 1.27–3.21; P trend = 0.003), and a 189 % higher risk of digestive-tract cancer mortality (HR 2.89; 95 % CI 1.08–7.71; P trend = 0.04) than individuals with DII scores in tertile I.
Sensitivity analysis was done by eliminating mortality during first year after inclusion/providing recall data, and the risk for subjects in the third tertile compared to those in the first tertile did not alter substantially for all-cause mortality(HR 1.36; 95 % CI 1.09–1.70; P trend 0.0006) and all-cancer mortality (HR 2.08; 95 % CI 1.31–3.31; P trend < 0.0001) in the prediabetes group as showed in supplement data Table 5, while the risk of CVD mortality (HR 1.38; 95 % CI 0.96–1.99; P trend = 0.08) became non-significant. Further analysis was done by additionally adjusting for serum low-density lipoprotein (LDL) and triglycerides (TG). As showed in supplement data Table 6, the risk of all-cause mortality (HR 1.80; 95 % CI 1.28–2.54; P trend 0.001), CVD mortality (HR 1.97; 95 % CI 1.14–3.41; P trend 0.02), all-cancer mortality (HR 2.25; 95 % CI 1.22–4.17; P trend 0.02), and digestive-tract cancer mortality (HR 5.29; 95 % CI 1.11–25.15; P trend 0.05) was moderately enhanced in the prediabetic group after additional adjustment for LDL and TG.
Discussion
This is the first study to focus the DII on prediabetic subjects in a large, nationally representative, prospective sample. In the current study, people with prediabetes who consumed a more pro-inflammatory diet, as reflected in higher DII scores, had an increased risk of death from any cause, malignant cancer, digestive-tract cancer, and CVD. Compared to subjects in tertile I, those in tertile III were 39 % more likely to die from any cause, 109 % more likely to die from malignant cancers, 189 % more likely to die from digestive-tract cancers, and 44 % more likely to die from CVD.
Chronic subclinical systemic inflammation is now considered a key etiologic factor in the development and progression of prediabetes, T2DM, CVD, and certain types of cancers [12–16]. Effective interventions to prevent diabetes, such as weight loss, exercise, or metformin have all been shown to exhibit anti-inflammatory effects [3, 10, 11, 37]. Elevated plasma concentrations of systemic inflammatory markers such as CRP, TNF-α, and IL-6 have been reported to be associated with an increased risk of CVD and T2DM [13, 16, 21]. Our study similarly demonstrated that the average CRP in the T2DM group and prediabetic group is higher than the normal group at the baseline. Previous studies reported that the DII predicts CRP levels and there is positive correlation between DII score and CRP level [26, 27, 31]. In the current study, it was observed that both average DII score and CRP levels were higher in both the T2DM group and prediabetic group, compared to the normal group. The result suggests that diet-induced subclinical inflammation may contribute to impaired glucose levels or insulin resistance. Previous findings of elevated CRP levels with increasing DII scores point to the role of increasing systemic inflammation [17, 19, 22–24]. A dietary pattern characterized by consumption of high-fat foods and processed meats (fats, oils, processed meats, fried potatoes, salty snacks) has been shown to increase systemic inflammation by increasing levels of high-sensitivity CRP, E-selectin, and soluble vascular cell adhesion molecule-1 [22, 23, 38]. In contrast, a pattern characterized by high consumption of whole grains and fruit (whole grains, fruit, nuts, and green leafy vegetables) was found to be inversely associated with CRP, IL-6, and homocysteine [22, 23, 38]. Evaluation of the effects of dietary patterns or consumption of single food components and CVD risk is complicated, as foods are not consumed in isolation and the effects of single foods are often small. There is considerable evidence that foods and food patterns act synergistically to influence the risk of several chronic diseases [39, 40]. The DII is particularly useful to evaluate quantitatively the inflammatory potential of whole food components consumed [26, 27].
A recent study has shown that a higher DII score was prospectively associated with higher systolic and diastolic blood pressure and triglycerides (TG), and with lower HDL cholesterol [33]. Both LDL and TG have been shown as strong predictors of the risk of CVD morbidity and mortality among individuals with or without T2DM [41–43]. Our results showed that high DII score diet increases the risk of all-cause mortality, CVD mortality, all-cancer mortality, and digestive-tract cancer mortality in the prediabetic group independently of serum TG and LDL.
The results of our study are consistent with several previous studies of the association between overall dietary pattern and risk of all-cause mortality, CVD morality, and cancer mortality [44–47]. In the Nurses’ Health Study (NHS), it has been shown that the prudent pattern, characterized by a high intake of vegetables, fruit, legumes, fish, poultry, and whole grains, deceased the risk of CVD and total mortality [44]. However, the Western pattern, characterized by a high intake of red and processed meat, refined grains, French fries, and sweets and desserts, increased the risk of CVD, cancer, and total mortality [44–47]. High intake of red and processed meat, refined grains, French fries, and sweets and desserts is positively associated with high DII score and elevated systemic markers [27, 36]. On the other hand, high intake of vegetables, fruit, legumes, fish, poultry, and whole grains is inversely associated with the DII score [27, 36]. The association between pro-inflammatory diet, as indicated by higher DII scores, and risk of digestive-tract cancer mortality is consistent with a previously published report that pro-inflammatory diet increases the risk of developing colorectal cancer [31–33].
Our study has several strengths. The NHANES III cohort study is a large, prospective, multiethnic, nationally representative study with well-characterized data on multiple risk factors and confounders. Nevertheless, there are limitations. We defined prediabetes and T2DM on the basis of the HgbA1c test. The advantage of HgbA1c is that it reflects average blood glucose level over the past 3–4 months and exhibits greater specificity and pre-analytic stability than other diagnostic markers, such as fasting plasma glucose (FPG) and oral glucose tolerance test (OGTT). However, the limitation is that the sensitivity of HgbA1c test is lower than FPG test and OGTT test [2]. This likely explains why the unweighted percentage of prediabetes and diabetes were only 20 and 7 %, respectively, which is below the estimated prevalence at the national level based on the 2005–2006 NHANES report [2, 4]; though strict exclusion criteria and national trends in the prevalence of prediabetes and diabetes probably also contribute to the difference. The main limitation of this study was that dietary intake was estimated based on single self-reported 24HR, which may not reflect the long-term dietary habits, and hence can lead to potential misclassification bias. This would tend to reduce the probability of detecting an effect. Dietary assessment was available only at one time point, and participants’ dietary habits might have changed during the follow-up period. However, several previous studies reported that dietary pattern classification is moderately stable over time [48–51]. There are several possible reasons that the associations seen in the prediabetic population were not seen in diabetic patients, who also had higher CRP and DII scores. First of all, diabetic patients might be on certain anti-inflammatory medications such as aspirin for the prevention of CVD which may have attenuated the inflammatory response to a pro-inflammatory diet. Secondly, diabetic patients might change their dietary pattern as directed by their primary care physician. Finally, it may be that the direct effects of T2DM on mortality are so great that they overwhelm the impact of dietary inflammation.
A final limitation is that information was available for only 27 of the 45 food parameters ideally used for DII calculation. Thus far, we have published more than 40 DII-related manuscripts. On average, we have had data on 27 food parameters. In instances where we can compare across methods [30, 36] we have not observed any change in the predictive ability of DII when going from ~45 to <30 parameters. Also, in a recent publication in NHANES III, DII scores calculated from the same 27 food parameters were found to be associated with mortality [52]. Therefore, it appears that these 27 parameters are sufficient for creating a reasonable estimate of the inflammatory effects of diet. This is possibly due to the fact that some of the missing food parameters (such as turmeric, saffron, and ginger) are likely consumed in small quantities and hence may not have a much impact on the overall DII.
In conclusion, individuals with prediabetes who consumed a more pro-inflammatory diet were at increased risk of dying from all causes, from all cancers, from digestive-tract cancer, and from CVD compared to individuals who consumed a more anti-inflammatory diet. Directions for future research should include an examination of how DII behaves longitudinally in an intervention trial among individuals with prediabetes to see if the reduction of the DII scores over time (i.e., by increasing intake of vegetables and fruits, nuts, low-fat dairy, fish, and whole grains) would delay the development and progress of diabetes, CVD, and cancer. As mentioned above, approximately 35 % of US adults ≥20 years have prediabetes. Interventions to promote reductions in dietary inflammation have the potential to reduce mortality in this large portion of the population.
References
Mellitus D (2005) Diagnosis and classification of diabetes mellitus. Diabetes Care 28:S37
Olson DE, Rhee MK, Herrick K, Ziemer DC, Twombly JG, Phillips LS (2010) Screening for diabetes and pre-diabetes with proposed A1C-based diagnostic criteria. Diabetes Care 33(10):2184–2189
Rydén L, Standl E, Bartnik M et al (2007) Guidelines on diabetes, pre-diabetes, and cardiovascular diseases: executive summary. The task force on diabetes and cardiovascular diseases of the European Society of Cardiology (ESC) and of the European Association for the Study of Diabetes (EASD). Eur Heart J 28(1):88–136
Cowie CC, Rust KF, Ford ES et al (2009) Full accounting of diabetes and pre-diabetes in the US population in 1988–1994 and 2005–2006. Diabetes Care 32(2):287–294
Control CfD Prevention, Control CfD Prevention (2011) National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, 201
Nelson KM, Reiber G, Boyko EJ (2002) Diet and exercise among adults with type 2 diabetes findings from the third national health and nutrition examination survey (NHANES III). Diabetes Care 25(10):1722–1728
Orozco LJ, Buchleitner AM, Gimenez-Perez G, Roqué i Figuls M, Richter B, Mauricio D (2008) Exercise or exercise and diet for preventing type 2 diabetes mellitus. The Cochrane Library, Chichester
Shikata K, Ninomiya T, Kiyohara Y (2013) Diabetes mellitus and cancer risk: review of the epidemiological evidence. Cancer Sci 104(1):9–14
Zhou X, Qiao Q, Zethelius B et al (2010) Diabetes, prediabetes and cancer mortality. Diabetologia 53(9):1867–1876
Colberg SR, Sigal RJ, Fernhall B et al (2010) Exercise and type 2 diabetes the American College of Sports Medicine and the American Diabetes Association: joint position statement. Diabetes Care 33(12):e147–e167
Hu FB, Manson JE, Stampfer MJ et al (2001) Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N Engl J Med 345(11):790–797
Coussens LM, Werb Z (2002) Inflammation and cancer. Nature 420(6917):860–867
Festa A, D’Agostino R, Howard G, Mykkänen L, Tracy RP, Haffner SM (2000) Chronic subclinical inflammation as part of the insulin resistance syndrome the Insulin Resistance Atherosclerosis Study (IRAS). Circulation 102(1):42–47
Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CH (1997) Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med 336(14):973–979
Shacter E, Weitzman SA (2002) Chronic inflammation and cancer. Oncology 16(2):217–232
Wang X, Bao W, Liu J et al (2013) Inflammatory markers and risk of type 2 diabetes a systematic review and meta-analysis. Diabetes Care 36(1):166–175
Galland L (2010) Diet and inflammation. Nutr Clin Pract 25(6):634–640. doi:10.1177/0884533610385703
Geraldo JM, Alfenas RC (2008) Role of diet on chronic inflammation prevention and control: current evidences. Arq Bras Endocrinol Metabol 52(6):951–967
Hardman WE (2014) Diet components can suppress inflammation and reduce cancer risk. Nutr Res Pract 8(3):233–240. doi:10.4162/nrp.2014.8.3.233
Lee H, Lee IS, Choue R (2013) Obesity, inflammation and diet. Pediatr Gastroenterol Hepatol Nutr 16(3):143–152. doi:10.5223/pghn.2013.16.3.143
Uusitupa M, Schwab U (2013) Diet, inflammation and prediabetes-impact of quality of diet. Can J Diabetes 37(5):327–331. doi:10.1016/j.jcjd.2013.07.029
Esmaillzadeh A, Kimiagar M, Mehrabi Y, Azadbakht L, Hu FB, Willett WC (2007) Dietary patterns and markers of systemic inflammation among Iranian women. J Nutr 137(4):992–998
Lopez-Garcia E, Schulze MB, Fung TT et al (2004) Major dietary patterns are related to plasma concentrations of markers of inflammation and endothelial dysfunction. Am J Clin Nutr 80(4):1029–1035
Mozaffarian D, Pischon T, Hankinson SE et al (2004) Dietary intake of trans fatty acids and systemic inflammation in women. Am J Clin Nutr 79(4):606–612
Lichtenstein AH, Erkkilä AT, Schwab US, Jalbert SM, Ausman LM (2003) Influence of hydrogenated fat and butter on CVD risk factors: remnant-like particles, glucose and insulin, blood pressure and C-reactive protein. Atherosclerosis 171(1):97–107
Cavicchia PP, Steck SE, Hurley TG et al (2009) A new dietary inflammatory index predicts interval changes in serum high-sensitivity C-reactive protein. J Nutr 139(12):2365–2372
Shivappa N, Steck SE, Hurley TG, Hussey JR, Hébert JR (2014) Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr 17(08):1689–1696
Shivappa N, Hébert JR, Rietzschel ER et al (2015) Associations between dietary inflammatory index and inflammatory markers in the Asklepios Study. Br J Nutr 113(04):665–671
Wood LG, Shivappa N, Berthon BS, Gibson PG, Hebert JR (2015) Dietary inflammatory index is related to asthma risk, lung function and systemic inflammation in asthma. Clin Exp Allergy 45(1):177–183
Tabung FK, Steck SE, Zhang J et al (2015) Construct validation of the dietary inflammatory index among postmenopausal women. Ann Epidemiol 25(6):398–405
Shivappa N, Prizment AE, Blair CK, Jacobs DR, Steck SE, Hébert JR (2014) Dietary inflammatory index and risk of colorectal cancer in the Iowa Women’s Health Study. Cancer Epidemiol Biomark Prev 23(11):2383–2392
Tabung FK, Steck SE, Ma Y et al (2014) The association between dietary inflammatory index and risk of colorectal cancer among postmenopausal women: results from the Women’s Health Initiative. Cancer Causes Control 26(3):399–408
Neufcourt L, Assmann K, Fezeu L et al (2015) Prospective association between the dietary inflammatory index and metabolic syndrome: findings from the SU. VI. MAX study. Nutr Metab Cardiovasc Dis 25(11):988–996
Garcia-Arellano A, Ramallal R, Ruiz-Canela M et al (2015) Dietary inflammatory index and incidence of cardiovascular disease in the PREDIMED Study. Nutrients 7(6):4124–4138
Control CfD Prevention (1996) The Third National Health and Nutrition Examination Survey (NHANES III, 1988–1994): reference manuals and reports. Maryland
Shivappa N, Steck SE, Hurley TG et al (2014) A population-based dietary inflammatory index predicts levels of C-reactive protein in the Seasonal Variation of Blood Cholesterol Study (SEASONS). Public Health Nutr 17(08):1825–1833
Stevens JW, Khunti K, Harvey R et al (2015) Preventing the progression to type 2 diabetes mellitus in adults at high risk: a systematic review and network meta-analysis of lifestyle, pharmacological and surgical interventions. Diabetes Res Clin Pract 107(3):320–331. doi:10.1016/j.diabres.2015.01.027
Nettleton JA, Steffen LM, Mayer-Davis EJ et al (2006) Dietary patterns are associated with biochemical markers of inflammation and endothelial activation in the Multi-Ethnic Study of Atherosclerosis (MESA). Am J Clin Nutr 83(6):1369–1379
Jacobs DR, Steffen LM (2003) Nutrients, foods, and dietary patterns as exposures in research: a framework for food synergy. Am J Clin Nutr 78(3):508S–513S
Drake I, Wallström P, Wirfält E (2013) What do review papers conclude about food and dietary patterns? Food Nutr Res 57:1–14
Howard BV, Robbins DC, Sievers ML et al (2000) LDL cholesterol as a strong predictor of coronary heart disease in diabetic individuals with insulin resistance and low LDL the Strong Heart Study. Arterioscler Thromb Vasc Biol 20(3):830–835
Isomaa B, Almgren P, Tuomi T et al (2001) Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care 24(4):683–689
Lu W, Resnick HE, Jablonski KA et al (2003) Non-HDL cholesterol as a predictor of cardiovascular disease in type 2 diabetes the strong heart study. Diabetes Care 26(1):16–23
Heidemann C, Schulze MB, Franco OH, van Dam RM, Mantzoros CS, Hu FB (2008) Dietary patterns and risk of mortality from cardiovascular disease, cancer, and all causes in a prospective cohort of women. Circulation 118(3):230–237
Mitrou PN, Kipnis V, Thiébaut AC et al (2007) Mediterranean dietary pattern and prediction of all-cause mortality in a US population: results from the NIH-AARP Diet and Health Study. Arch Intern Med 167(22):2461–2468
Osler M, Heitmann BL, Gerdes LU, Jørgensen LM, Schroll M (2001) Dietary patterns and mortality in Danish men and women: a prospective observational study. Br J Nutr 85(02):219–225
Shimazu T, Kuriyama S, Hozawa A et al (2007) Dietary patterns and cardiovascular disease mortality in Japan: a prospective cohort study. Int J Epidemiol 36(3):600–609
Jain M, Howe G, Harrison L, Miller A (1989) A study of repeatability of dietary data over a seven-year period. Am J Epidemiol 129(2):422–429
Jensen OM, Wahrendorf J, Rosenqvist A, Geser A (1984) The reliability of questionnaire-derived historical dietary information and temporal stability of food habits in individuals. Am J Epidemiol 120(2):281–290
Sijtsma FP, Meyer KA, Steffen LM et al (2012) Longitudinal trends in diet and effects of sex, race, and education on dietary quality score change: the coronary artery risk development in young adults study. Am J Clin Nutr 95(3):580–586
Thompson FE, Metzner HL, Lamphiear DE, Hawthorne VM (1990) Characteristics of individuals and long term reproducibility of dietary reports: the Tecumseh Diet Methodology Study. J Clin Epidemiol 43(11):1169–1178
Shivappa N, Steck SE, Hussey JR, Ma Y, Hebert JR (2015) Inflammatory potential of diet and all-cause, cardiovascular, and cancer mortality in National Health and Nutrition Examination Survey III Study. Eur J Nutr. doi:10.1007/s00394-015-1112-x
Acknowledgments
Drs. Shivappa and Hébert were supported by grant number R44DK103377 from the United States National Institute of Diabetes and Digestive and Kidney Diseases.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Dr. James R. Hébert owns controlling interest in Connecting Health Innovations LLC (CHI), a company planning to license the right to his invention of the dietary inflammatory index (DII) from the University of South Carolina in order to develop computer and smart phone applications for patient counseling and dietary intervention in clinical settings. Dr. Nitin Shivappa is an employee of CHI. The authors have declared no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Deng, F.E., Shivappa, N., Tang, Y. et al. Association between diet-related inflammation, all-cause, all-cancer, and cardiovascular disease mortality, with special focus on prediabetics: findings from NHANES III. Eur J Nutr 56, 1085–1093 (2017). https://doi.org/10.1007/s00394-016-1158-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-016-1158-4