Abstract
Purpose
Diet and dietary components have been studied previously in relation to mortality; however, little is known about the relationship between the inflammatory potential of overall diet and mortality.
Materials and methods
We examined the association between the Dietary Inflammatory Index (DII) and mortality among 33,747 participants in the population-based Swedish Mammography Cohort. The DII score was calculated based on dietary information obtained from a self-administered food frequency questionnaire. Mortality was determined through linkage to the Swedish Cause of Death Registry through 2013. Cox proportional hazard regression was used to estimate hazard ratios (HR). During 15 years of follow-up, 7095 deaths were identified, including 1996 due to cancer, 602 of which were due to digestive-tract cancer, and 2399 due to cardiovascular disease.
Results
After adjusting for age, energy intake, education, alcohol intake, physical activity, BMI, and smoking status, analyses revealed a positive association between higher DII score and all-cause mortality. When used as a continuous variable (range −4.19 to 5.10), DII score was associated with all-cause mortality (HRContinuous = 1.05; 95 % CI 1.01–1.09) and digestive-tract cancer mortality (HRContinuous = 1.15; 95 % CI 1.02–1.29). Comparing subjects in the highest quintile of DII (≥1.91) versus the lowest quintile (DII ≤ −0.67), a significant association was observed for all-cause mortality (HR = 1.25; 95 % CI 1.07–1.47, P trend = 0.003).
Conclusion
These results indicate that a pro-inflammatory diet, as indicated by higher DII score, was associated with all-cause and digestive-tract cancer mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inflammation is a result of the body’s response to tissue insult or injury, or the presence of inflammatory stimulants such as lipopolysaccharide, interleukins, and other cytokines [1, 2]. The acute inflammatory response represents an important step in the process of wound healing, immune responsiveness, and tissue regeneration that, under normal circumstances, will resolve within a few days [3, 4]. By contrast, chronic inflammation is characterized by positive feedback in which the normal modulating of signaling by cytokines does not “turn off” [5]. It is well known that dietary factors are necessary to mount a competent acute inflammatory response [2, 6], as well as contributing to an individual’s underlying state of chronic inflammation [7, 8].
Chronic inflammation is known to be associated with a variety of chronic health conditions including arthritis, diverticulitis, cardiovascular disease (CVD), diabetes [9–11], and common epithelial cancers, with colorectal [12–14] being the most extensively studied. Worldwide, CVD is the leading cause of mortality, accounting for about half of deaths among adults [15]. There is growing evidence that specific dietary components influence inflammation [16–18] and this may influence all-cause, cancer, and CVD mortality [19–22].
Research into the role of diet in inflammation and mortality suggests that diet represents a complicated set of exposures which often interact, and whose cumulative effect modifies both inflammatory responses and health outcomes. Several dietary indices exist to assess diet quality, but only one focuses on diet’s effects on inflammation. The Dietary Inflammatory Index (DII) was developed to characterize an individual’s diet on a continuum from maximally anti- to pro-inflammatory. The DII is grounded in peer-reviewed literature focusing on a specific health-related outcome (i.e., inflammation) and is standardized to dietary intake from numerous populations around the world; combining these developments helps to overcome shortcomings of previous dietary indices [23]. Thus far, the DII has been found to be associated with C-reactive protein [24, 25], interleukin-6 [26–28], and homocysteine [26]. Additionally, DII has been shown to be associated with glucose intolerance and dyslipidemia components of the metabolic syndrome [25, 29], anthropometric measurements in Spain [30], asthma in Australia [28], respiratory conditions in Italy [31], bone mineral density among postmenopausal women in Iran [28], colorectal cancer in two case–control studies in Spain and Italy [32, 33], and three cohort studies in the USA [34–36], pancreatic [37], prostate [38, 39] and esophageal cancers [40, 41] and mortality in a cohort among US women [42].
Until now, the DII has not yet been applied to mortality outcomes in a population outside USA. The purpose of this study was to examine the association between the DII and all-cause, overall cancer, digestive-tract cancer, and CVD mortality in a large population-based prospective cohort of Swedish women, the Swedish Mammography Cohort. We are interested in digestive-tract cancers, in particular those of lower gastrointestinal tract as they are strongly related to chronic inflammation [43, 44]. Our working hypothesis was that a higher DII score (indicating a pro-inflammatory diet) is associated with risk of death from any cause, as well as death from specific causes.
Methods
Study population
Recruitment procedures and characteristics of the Swedish Mammography Cohort (SMC) have been described previously [45]. In brief, the SMC is a population-based cohort of 66,651 women born between 1914 and 1948 who were recruited between 1987 and 1990 in Västmanland and Uppsala counties in central Sweden. In 1987, participants completed a questionnaire regarding diet, reproductive, and other factors. In 1997, a second questionnaire was extended to include dietary supplements, physical activity, and smoking status and was sent to participants who were still alive and residing in the study area; 39,227 (70 %) women returned this questionnaire. Completion and return of the self-administered questionnaire were treated as informed consent of study participants. The study was approved by the ethics committee at the Karolinska Institutet.
Because information on several potential confounders (i.e., cigarette smoking, physical activity) was first obtained in 1997, only women who completed the 1997 questionnaire were included in the present study (N = 38,984 after exclusion of those with an incorrect or missing national registration number). We excluded women with implausible total energy intake [3 standard deviations (SD) from the mean value for loge-transformed energy intake], a history of stroke, coronary heart disease, diabetes, or cancer (except nonmelanoma skin cancer) before the start of follow-up. This left 33,747 women for the present analysis.
Dietary assessment
Diet was assessed in 1997 using a 96-item food frequency questionnaire (FFQ) [46]. Participants were asked how often, on average, they had consumed each item during the previous year, with eight predefined frequency categories ranging from never to ≥3 times per day. Nutrient intakes were calculated by multiplying the frequency of consumption by the nutrient content of age-specific portion sizes by using composition values from the Swedish Food Administration Database [47]. Nutrient intakes were adjusted for energy using the residual method [48]. The questionnaire also asked about use of dietary supplements, including multivitamins with minerals, and some specific vitamin and mineral supplements. The FFQ had been validated previously [49].
Dietary Inflammatory Index (DII)
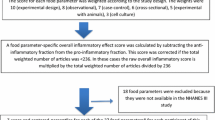
The DII is based on the literature published through 2010 linking diet to inflammation. Developing the DII involved review and scoring nearly 2000 scientific articles on diet and six inflammatory markers [i.e., CRP, interleukin (IL)-1β, IL-4, IL-6, IL-10, and tumor necrosis factor (TNF)-α] based on cell culture and laboratory animal experiments, and cross-sectional, longitudinal and intervention trials in humans. Individual intakes of food parameters on which the DII is based are then compared to a world standard database of dietary intake based on datasets from 11 different regions worldwide. A complete description of the DII is available elsewhere. Briefly, to calculate DII for the participants of this study, the dietary data were first linked to the world database that provided a robust estimate of a mean and standard deviation for each parameter [23]. These then become the multipliers to express an individual’s exposure relative to the “standard global mean” as a z-score. This is achieved by subtracting the “standard global mean” from the amount reported and dividing this value by the standard deviation. To minimize the effect of “right skewing,” this value is then converted to a centered percentile score. The centered percentile score for each food parameter for each individual was then multiplied by the respective food parameter effect score, which is derived from the literature review, in order to obtain a food parameter-specific DII score for an individual. All of the food parameter-specific DII scores are then summed to create the overall DII score for each participant in the study [23]. A description of validation of the DII, including comparing hs-CRP values to DII derived from both dietary recalls and a structured questionnaire similar to an FFQ, is available elsewhere [24]. Twenty-seven of the 45 food parameters that could be used for DII calculation were available from this study [23]. The 27 food parameters were energy, carbohydrate, protein, fat, alcohol, fiber, cholesterol, saturated fatty acid, monounsaturated fatty acid, polyunsaturated fatty acid, niacin, thiamin, riboflavin, vitamin B12, vitamin B6, iron, magnesium, zinc, selenium, vitamin A, vitamin C, vitamin D, vitamin E, folic acid, beta carotene, omega 6, and omega 3. Of the remaining 18 food parameters missing, there are some that are consumed in smaller amounts in Sweden, such as turmeric, rosemary, pepper, garlic, and ginger.
Outcome assessment
Date and cause(s) of death were identified through linkage to the Swedish Cause of Death Registry at National Board of Health and Welfare. It is estimated that 93 % of all deaths in Sweden are reported within 10 days and 100 % are reported within 30 days [50]. Cause of death was determined by International Classification of Diseases (ICD) codes.
Statistical analysis
Cox proportional hazard models were used to calculate hazard ratios (HRs) and 95 % confidence intervals (95 % CIs) for death. Participants contributed person-time from September 15, 1997, until death from any cause, or end of follow-up on December 31, 2013. We also examined death from any cancer, digestive-tract cancer, and cardiovascular disease as the endpoints with end of follow-up on December 31, 2012, as information on the specific cause of death was not available after this time. The DII was categorized into quintiles, with the lowest quintile serving as the reference group.
We adjusted our multivariable models for age in 1997 (continuous), total energy intake (continuous), BMI (<25, 25–29.9, ≥30 kg/m2), education (primary school, high school, university), smoking status (never, former <20 pack-years, former ≥20 pack-years, current <20 pack-years, current ≥20 pack-years), physical activity (quartiles of metabolic equivalent [MET] hours/day; <38.9, 38.9–42.2, 42.3–45.9, >45.9), and alcohol intake (nondrinker or <3.4, 3.4–9.9, ≥10 g/day). Categories were created for missing data.
The covariates were chosen a priori as they previously had been shown to be strong risk factors for mortality in this cohort. Other covariates commonly reported to alter inflammation (NSAIDS, aspirin) or mortality (sedentary time) were explored and not shown to be significant and thus not included in the models. Tests for linear trend were performed by assigning the median value of each category to each participant in that group. All tests of statistical significance were two-sided, and analyses were performed using SAS version 9.2 (SAS Institute Inc., Cary, NC, USA).
Results
DII had a mean ± SD value of 0.64 ± 1.45, with a range from −4.19 (most anti-inflammatory score) to +5.10 (most pro-inflammatory score). Women in higher quintiles had lower age, BMI, physical activity (MET hours/day), percentage of women with postsecondary education, nonalcohol drinkers, and higher total energy intake and percentage of current smokers. Similarly, total, cancer, digestive-tract cancer, and CVD deaths were associated with higher DII values (Table 1). Table 2 describes the distribution of servings of 30 food groups across DII quintiles, with percentage difference between quintiles 5 and 1. Compared to first quintile, women in fifth quintile reported lower consumption of green leafy vegetables or potatoes (65 %), green leafy vegetables (64 %), and fruits (60 %). Similarly, women in fifth quintile reported higher consumption of beer (24 %), French fries (25 %), sweets (not including chocolate) (32 %), liquor (50 %), whole grains (58 %), refined grains (69 %), chocolate (100 %), high-fat diary (142 %), and soft drinks/soda (150 %).
In total, 7095 total deaths were identified during the 15 years of follow-up, including 1996 all cancer deaths, 602 digestive-tract cancer deaths, and 2399 CVD deaths. In age- and energy-adjusted analyses using continuous DII, a 1-unit increment in DII (corresponding to 11 % range in this cohort study) showed significant positive associations with risk of all-cause mortality (HR = 1.08; 95 % CI 1.04–1.11), cancer mortality (HR = 1.06; 95 % CI 1.00–1.12), digestive-tract cancer mortality (HR = 1.14; 95 % CI 1.02–1.28), and CVD mortality (HR = 1.06; 95 % CI 1.00–1.13). The results were almost identical after additional adjustment for education, alcohol intake, physical activity, BMI, and smoking status, for all-cause mortality (HR = 1.05; 95 % CI 1.01–1.09) and digestive-tract cancer mortality (HR = 1.15; 95 % CI 1.02–1.29). The results were in the hypothesized direction for cancer mortality and CVD mortality. The direction of associations was along expected lines for all-cause and digestive-tract cancer mortality; however, results did not achieve statistical significance.
Age- and energy-adjusted analyses with DII categorized as quintiles revealed significantly higher risk for subjects in the fifth quintile compared to those in the first quintile for all-cause mortality (HR = 1.41; 95 % CI 1.21–1.64, P trend < 0.0001), cancer mortality (HR = 1.32; 95 % CI 1.02–1.72, P trend = 0.03), digestive-tract cancer mortality (HR = 1.38; 95 % CI 0.81–2.33, P trend = 0.04), and CVD mortality (HR = 1.35; 95 % CI 1.01–1.81, P trend = 0.02). Multivariate analyses revealed significantly higher risk among subjects in the fifth quintile compared to those in the first quintile for all-cause mortality (HR = 1.25; 95 % CI 1.07–1.47, P trend = 0.003) (Table 3).
Discussion
In this large, nationally representative, prospective cohort study of women, consumption of a more pro-inflammatory diet, as reflected by higher DII scores, was associated with increased risk of death from any cause and deaths due to digestive-tract cancers. Compared to women in the first quintile, women in the fifth quintile were 25 % more likely to die from any cause. Similarly, for every one-unit increase in DII, the risk of dying from any cause and from digestive-tract cancer increased by 5 and 15 %, respectively. Among digestive-tract cancers, colorectal cancer is known to be strongly related to inflammation [51–54] and represents the majority of digestive-tract cancers [55, 56]. We also observed that higher intake of healthy food items such as fruits and vegetables was observed among women with lower quintiles of DII, whereas higher intake of less healthy food items such as French fries and refined grains was seen among women in lower quintiles.
The DII is different from other dietary indices, virtually all of which fall into three main categories: (1) those derived from specific dietary recommendations based on some external standard (e.g., Healthy Eating Index (HEI) which was derived from the adherence to the US Dietary guidelines [57]); (2) those derived empirically from findings within particular study populations (e.g., computing a pattern using principal component analysis (PCA) [58]); or (3) those that link to particular cultural patterns of dietary intake (e.g., the Mediterranean diet score [59]). Studies have been conducted examining various dietary patterns and indices in relation to mortality [60–62]. In the NHANES III cohort study, the HEI was found to be inversely associated with overall and CVD mortality [61]. In a study conducted in the National Institutes of Health-AARP Diet and Health Study, the Mediterranean diet score was associated with reduced all-cause and cause-specific mortality [60], while another report from the National Institutes of Health-AARP Diet and Health Study showed various indices [HEI-2010, the Alternative Healthy Eating Index-2010 (AHEI-2010), the alternate Mediterranean Diet (aMED), and Dietary Approaches to Stop Hypertension (DASH)] to be protective against all-cause mortality, CVD, and cancer mortality [63]. In contrast, in the Whitehall cohort study, which was conducted in UK with a predominantly European population, the AHEI was not associated with cancer mortality or noncancer/non-CVD mortality [62].
Previous studies also have examined the effect of specific food items on mortality, including high-fat dairy [66, 67], and nutrients such as magnesium [68], and vitamin E [69], and the results have been inconsistent. High-fat dairy is rich in saturated fat and total fat which form the pro-inflammatory components in DII calculation. Vitamin E and magnesium have an anti-inflammatory effect score in the DII calculation [23]. No association was observed between magnesium and calcium and cancer-related mortality in the EPIC-Heidelberg study [68]. In a prospective study conducted by Pocobelli et al. [69], vitamin E was found to significantly reduce CVD mortality; however, no association was observed with cancer mortality. A limitation of examining individual food items or nutrients is that whole foods or nutrients are usually consumed with other food items and nutrients; thus, dietary inter-correlations may attenuate or accentuate the actual effects of the individual food or nutrient under study. A very high correlation between nutrients and among foods can result in instability in risk estimation and possible loss of statistical power. In formulating the DII [23], an entirely different approach was taken by focusing on the functional effects of foods and nutrients. As such, it relies on a careful review and scoring of the medical literature in specific relation to inflammation. Also, it standardizes individuals’ dietary intakes of pro- and anti-inflammatory food constituents to world referent values.
The effect of red meat is in the opposite direction of expectation. However, it should be noted that red meat is one among several other food items that influence inflammation. There are other food items such as vegetables, fruits, and fish that exert strong anti-inflammatory effects per unit exposure, and their distributions are along expected lines. Because the DII takes into account diet as a whole, and red meat eaters also consumed these other vegetable components, spices, etc., the totality of their diet was anti-inflammatory. Red meat was positively correlated with both energy and sum of fruit and vegetable intake (r = 0.40 and 0.14, respectively). In addition to this, the percentage decrease across quintiles is 6 % which is very low compared to decrease in other food items like fruits (60 %) and green leafy vegetables (64 %).
However, our previous experience with using the DII indicates that those conditions that we know from other lines of research (e.g., laboratory animal experiments) to be most strongly related to inflammation tend to produce the most strongly positive results. Most notably, this includes colorectal cancer (which, because of its relatively high incidence, drives digestive-tract cancer rates) [32, 34–36], pancreatic cancer [37], and asthma, lung and other respiratory conditions [28, 31]. In contrast, results have been equivocal for factors related to metabolic syndrome and thereby for cardiovascular outcomes as well [25, 26, 29]. This makes sense given the fact that cardiovascular outcomes are strongly determined by other, nondietary factors, most notably physical activity [60, 61].
Although the actual mechanism of how a healthy diet reduces mortality is not clearly known, one of the possible mechanisms for this inverse association might be through the effect of a pro-inflammatory diet on insulin resistance by increasing systemic inflammation [70, 71]. Consumption of food items such as meat and butter has been shown to increase systemic inflammation by increasing levels of high-sensitivity CRP, E-selectin, and soluble vascular cell adhesion molecule-1 [70], which are then responsible for increasing insulin resistance [71]. Insulin resistance caused by increasing circulating levels of insulin, triglycerides, and nonesterified fatty acids [43, 44] is associated with digestive-tract cancers and various cardiovascular diseases, all of which, if left uncontrolled, result in death. As mentioned previously, there are various dietary factors that have different effects on inflammation; for example, red meat consumption increases inflammation while green leafy vegetables reduce inflammation [43, 44]. In support of our findings, previous work in the SMC examining diet and mortality, have shown significant inverse associations between anti-inflammatory food parameters such as fruits and vegetables [72], which is consistent with results from other studies such as ARIC [73], 2001–2008 Health Surveys for England [74], and a cohort in Taiwan [75]. Previous analyses in the SMC also have shown increasing vitamin C and selenium intake to be inversely associated with breast cancer-related mortality [76, 77], and consumption of red meat was associated with shorter overall survival [78]. Vitamin C and selenium are among anti-inflammatory components of DII [23]. At the same time, there are also other studies that have shown no association between red meat, vitamin C, and selenium; and inflammation [79–81] and mortality [82, 83].
Our study has several strengths. First, it is population-based and employs a prospective design. It also benefits from a large sample size, complete ascertainment of deaths through the National Cause of Death Registry, and detailed information on diet. The small fraction of missing data reported on single items, which were treated with the zero-consumption approach, is unlikely to represent a source of bias for the observed findings [84]. This study also had a long follow-up with a large number of events for the outcomes studied. This is the first time the DII has been used in a cohort study outside USA with mortality as outcome. The main limitation of this study was that information on diet was self-reported, which can lead to a potential misclassification of the exposure. Classification errors in our prospective study, however, were nondifferential with respect to the occurrence of death and most likely led to an attenuation of the results. Dietary assessment was available only at one time point. Participants’ dietary habit might have changed during the follow-up period. However, previous studies reported that dietary pattern classification is moderately stable over long periods of time during adulthood [85–90]. Other limitations of the study include nonavailability of screening data, stage of disease at diagnosis for most cancers, and no evidence of DII being associated with inflammatory markers in this study. While it is true we do not have screening data, the universal health care system of Sweden makes this less of an issue than in a country such as the USA where access to healthcare is confounded by many other unmeasured factors.
In conclusion, individuals who reported consumption of a more pro-inflammatory diet were at greater risk of dying from any cause and from digestive-tract cancers compared to individuals who reported a more anti-inflammatory dietary intake. Our results provide further evidence for the benefits of a diet in high anti-inflammatory foods such as vegetables and fruits, nuts, low-fat dairy products, and fish, and low in fried foods, processed meats, and refined grains. Future steps might include investigating how the DII predicts mortality in cohort studies among men and how it behaves longitudinally in an intervention trial among individuals who have had cancer or CVD to examine if improvement in the DII scores over time is associated with reduced risk of inflammation-associated disease and/or death.
References
Keibel A, Singh V, Sharma MC (2009) Inflammation, microenvironment, and the immune system in cancer progression. Curr Pharm Des 15(17):1949–1955
Pan MH, Lai CS, Dushenkov S, Ho CT (2009) Modulation of inflammatory genes by natural dietary bioactive compounds. J Agric Food Chem 57(11):4467–4477
Thun MJ, Henley SJ, Gansler T (2004) Inflammation and cancer: an epidemiological perspective. Novartis Found Symp 256:6–21; discussion 22–28, 49–52, 266–269
Warnberg J, Gomez-Martinez S, Romeo J, Diaz LE, Marcos A (2009) Nutrition, inflammation, and cognitive function. Ann N Y Acad Sci 1153:164–175
Baniyash M, Sade-Feldman M, Kanterman J (2014) Chronic inflammation and cancer: suppressing the suppressors. Cancer Immunol Immunother 63(1):11–20. doi:10.1007/s00262-013-1468-9
Ferencik M, Ebringer L (2003) Modulatory effects of selenium and zinc on the immune system. Folia Microbiol 48(3):417–426
Lin OS (2009) Acquired risk factors for colorectal cancer. Methods Mol Biol 472:361–372. doi:10.1007/978-1-60327-492-0_16
Wogan GN, Hecht SS, Felton JS, Conney AH, Loeb LA (2004) Environmental and chemical carcinogenesis. Semin Cancer Biol 14(6):473–486. doi:10.1016/j.semcancer.2004.06.010
Ouchi N, Parker JL, Lugus JJ, Walsh K (2011) Adipokines in inflammation and metabolic disease. Nat Rev Immunol 11(2):85–97. doi:10.1038/nri2921
Calabro P, Golia E, Yeh ET (2009) CRP and the risk of atherosclerotic events. Semin Immunopathol 31(1):79–94. doi:10.1007/s00281-009-0149-4
Miller MA, Cappuccio FP (2007) Inflammation, sleep, obesity and cardiovascular disease. Curr Vasc Pharmacol 5(2):93–102
Chung Y-C, Chang Y-F (2003) Serum interleukin-6 levels reflect the disease status of colorectal cancer. J Surg Oncol 83(4):222–226
Terzic J, Grivennikov S, Karin E, Karin M (2010) Inflammation and colon cancer. Gastroenterology 138 (6):2101–2114 e2105
Toriola AT, Cheng TY, Neuhouser ML, Wener MH, Zheng Y, Brown E, Miller JW, Song X, Beresford SA, Gunter MJ, Caudill MA, Ulrich CM (2013) Biomarkers of inflammation are associated with colorectal cancer risk in women but are not suitable as early detection markers. Int J Cancer 132(11):2648–2658. doi:10.1002/ijc.27942
World Health Organization (2008) The global burden of disease: 2004 update. WHO, Geneva
de Mello VD, Schwab U, Kolehmainen M, Koenig W, Siloaho M, Poutanen K, Mykkanen H, Uusitupa M (2011) A diet high in fatty fish, bilberries and wholegrain products improves markers of endothelial function and inflammation in individuals with impaired glucose metabolism in a randomised controlled trial: the Sysdimet study. Diabetologia 54(11):2755–2767
Khoo J, Piantadosi C, Duncan R, Worthley SG, Jenkins A, Noakes M, Worthley MI, Lange K, Wittert GA (2011) Comparing effects of a low-energy diet and a high-protein low-fat diet on sexual and endothelial function, urinary tract symptoms, and inflammation in obese diabetic men. J Sex Med 8(10):2868–2875
Luciano M, Mottus R, Starr JM, McNeill G, Jia X, Craig LC, Deary IJ (2012) Depressive symptoms and diet: their effects on prospective inflammation levels in the elderly. Brain Behav Immun 26(5):717–720
Chang AR, Lazo M, Appel LJ, Gutierrez OM, Grams ME (2014) High dietary phosphorus intake is associated with all-cause mortality: results from NHANES III. Am J Clin Nutr 99(2):320–327. doi:10.3945/ajcn.113.073148
Cheung CL, Sahni S, Cheung BM, Sing CW, Wong IC (2014) Vitamin K intake and mortality in people with chronic kidney disease from NHANES III. Clin Nutr. doi:10.1016/j.clnu.2014.03.011
Cohen HW, Hailpern SM, Alderman MH (2008) Sodium intake and mortality follow-up in the Third National Health and Nutrition Examination Survey (NHANES III). J Gen Intern Med 23(9):1297–1302. doi:10.1007/s11606-008-0645-6
Deng X, Song Y, Manson JE, Signorello LB, Zhang SM, Shrubsole MJ, Ness RM, Seidner DL, Dai Q (2013) Magnesium, vitamin D status and mortality: results from US National Health and Nutrition Examination Survey (NHANES) 2001 to 2006 and NHANES III. BMC Med 11:187. doi:10.1186/1741-7015-11-187
Shivappa N, Steck SE, Hurley TG, Hussey JR, Hebert JR (2014) Designing and developing a literature-derived, population-based dietary inflammatory index. Pub Health Nutr 17(8):1689–1696. doi:10.1017/S1368980013002115
Shivappa N, Steck SE, Hurley TG, Hussey JR, Ma Y, Ockene IS, Tabung F, Hebert JR (2014) A population-based dietary inflammatory index predicts levels of C-reactive protein in the Seasonal Variation of Blood Cholesterol Study (SEASONS). Pub Health Nutr 17(8):1825–1833. doi:10.1017/S1368980013002565
Wirth MD, Burch J, Shivappa N, Violanti JM, Burchfiel CM, Fekedulegn D, Andrew ME, Hartley TA, Miller DB, Mnatsakanova A, Charles LE, Steck SE, Hurley TG, Vena JE, Hebert JR (2014) Association of a dietary inflammatory index with inflammatory indices and metabolic syndrome among police officers. J Occup Environ Med 56(9):986–989. doi:10.1097/JOM.0000000000000213
Shivappa N, Hebert JR, Rietzschel ER, De Buyzere ML, Langlois M, Debruyne E, Marcos A, Huybrechts I (2015) Associations between dietary inflammatory index and inflammatory markers in the Asklepios Study. Br J Nutr 113(4):665–671. doi:10.1017/S000711451400395X
Tabung FK, Steck SE, Zhang J, Ma Y, Liese AD, Agalliu I, Hingle M, Hou L, Hurley TG, Jiao L, Martin LW, Millen AE, Park HL, Rosal MC, Shikany JM, Shivappa N, Ockene JK, Hebert JR (2015) Construct validation of the dietary inflammatory index among postmenopausal women. Ann Epidemiol. doi:10.1016/j.annepidem.2015.03.009
Wood LG, Shivappa N, Berthon BS, Gibson PG, Hebert JR (2015) Dietary inflammatory index is related to asthma risk, lung function and systemic inflammation in asthma. Clin Exp Allergy 45(1):177–183. doi:10.1111/cea.12323
Alkerwi A, Shivappa N, Crichton G, Hebert JR (2014) No significant independent relationships with cardiometabolic biomarkers were detected in the Observation of Cardiovascular Risk Factors in Luxembourg study population. Nutr Res 34(12):1058–1065. doi:10.1016/j.nutres.2014.07.017
Ruiz-Canela M, Zazpe I, Shivappa N, Hebert JR, Sanchez-Tainta A, Corella D, Salas-Salvado J, Fito M, Lamuela-Raventos RM, Rekondo J, Fernandez-Crehuet J, Fiol M, Santos-Lozano JM, Serra-Majem L, Pinto X, Martinez JA, Ros E, Estruch R, Martinez-Gonzalez MA (2015) Dietary inflammatory index and anthropometric measures of obesity in a population sample at high cardiovascular risk from the PREDIMED (PREvencion con DIeta MEDiterranea) trial. Br J Nutr 1–12. doi:10.1017/S0007114514004401
Maisonneuve P, Shivappa N, Hébert J, Bellomi M, Rampinelli C, Bertolotti R, Spaggiari L, Palli D, Veronesi G, Gnagnarella P (2015) Dietary inflammatory index and risk of lung cancer and other respiratory conditions among heavy smokers in the COSMOS screening study. Eur J Nutr 1–11. doi:10.1007/s00394-015-0920-3
Zamora-Ros R, Shivappa N, Steck SE, Canzian F, Landi S, Alonso MH, Hebert JR, Moreno V (2015) Dietary inflammatory index and inflammatory gene interactions in relation to colorectal cancer risk in the Bellvitge colorectal cancer case–control study. Genes Nutr 10(1):447. doi:10.1007/s12263-014-0447-x
Shivappa N, Zucchetto A, Montella M, Serraino D, Steck SE, La Vecchia C, Hebert JR (2015) Inflammatory potential of diet and risk of colorectal cancer in a case-control study from Italy. Br J Nutr 114(1):152–158. doi:10.1017/S0007114515001828
Shivappa N, Prizment AE, Blair CK, Jacobs DR Jr, Steck SE, Hebert JR (2014) Dietary inflammatory index and risk of colorectal cancer in the Iowa Women’s Health Study. Cancer Epidemiol Biomark Prev 23(11):2383–2392. doi:10.1158/1055-9965.EPI-14-0537
Tabung FK, Steck SE, Ma Y, Liese AD, Zhang J, Caan B, Hou L, Johnson KC, Mossavar-Rahmani Y, Shivappa N, Wactawski-Wende J, Ockene JK, Hebert JR (2015) The association between dietary inflammatory index and risk of colorectal cancer among postmenopausal women: results from the Women’s Health Initiative. Cancer Causes Control 26(3):399–408. doi:10.1007/s10552-014-0515-y
Wirth MD, Shivappa N, Steck SE, Hurley TG, Hébert JR (2015) The dietary inflammatory index is associated with colorectal cancer in the National Institutes of Health–American Association of Retired Persons Diet and Health Study. Br J Nutr FirstView 1–9. doi:10.1017/S000711451500104X
Shivappa N, Bosetti C, Zucchetto A, Serraino D, La Vecchia C, Hebert JR (2014) Dietary inflammatory index and risk of pancreatic cancer in an Italian case-control study. Br J Nutr 1–7. doi:10.1017/S0007114514003626
Shivappa N, Bosetti C, Zucchetto A, Montella M, Serraino D, La Vecchia C, Hebert JR (2014) Association between dietary inflammatory index and prostate cancer among Italian men. Br J Nutr 1–6. doi:10.1017/S0007114514003572
Shivappa N, Jackson M, Bennett F, Hebert J (2015) Increased Dietary Inflammatory Index (DII) is associated with increased risk of prostate cancer in Jamaican Men. Nutr Cancer. doi:10.1080/01635581.2015.1062117
Lu Y, Shivappa N, Lin Y, Lagergren J, Hebert JR (2015) Diet-related inflammation and esophageal cancer by histological type: a nationwide case–control study in Sweden. Eur J Nutr. doi:10.1007/s00394-015-0987-x
Shivappa N, Zucchetto A, Serraino D, Rossi M, La Vecchia C, Hebert JR (2015) Dietary Inflammatory Index and risk of esophageal squamous cell cancer in a case-control study from Italy. Cancer Causes Control. doi:10.1007/s10552-015-0636-y
Shivappa N, Blair C, Prizment A, Jacobs D Jr, Steck S, Hébert J (2015) Association between inflammatory potential of diet and mortality in the Iowa Women’s Health study. Eur J Nutr 1–12. doi:10.1007/s00394-015-0967-1
Bruce WR, Wolever TM, Giacca A (2000) Mechanisms linking diet and colorectal cancer: the possible role of insulin resistance. Nutr Cancer 37(1):19–26. doi:10.1207/S15327914NC3701_2
Bruce WR, Giacca A, Medline A (2000) Possible mechanisms relating diet and risk of colon cancer. Cancer Epidemiol Biomark Prev 9(12):1271–1279
Wolk A, Larsson SC, Johansson J-E, Ekman P (2006) Long-term fatty fish consumption and renal cell carcinoma incidence in women. JAMA 296(11):1371–1376. doi:10.1001/jama.296.11.1371
Rautiainen S, Levitan EB, Mittleman MA, Wolk A (2015) Fruit and vegetable intake and rate of heart failure: a population-based prospective cohort of women. Eur J Heart Fail 17(1):20–26. doi:10.1002/ejhf.191
Bergström L, Kylberg E, Hagman U, Erikson H, Bruce Å (1991) The food composition database KOST: the National Food Adminstration’s Information System for nutritive values of food. Vår Fö da 43:439–447
Willett W, Stampfer MJ (1986) Total energy intake: implications for epidemiologic analyses. Am J Epidemiol 124(1):17–27
Messerer M, Johansson S-E, Wolk A (2004) The Validity of Questionnaire-based micronutrient intake estimates is increased by including dietary supplement use in Swedish men. J Nutr 134(7):1800–1805
Ludvigsson J, Otterblad-Olausson P, Pettersson B, Ekbom A (2009) The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol 24(11):659–667. doi:10.1007/s10654-009-9350-y
Erlinger TP, Platz EA, Rifai N, Helzlsouer KJ (2004) C-reactive protein and the risk of incident colorectal cancer. JAMA 291(5):585–590
Gunter MJ, Stolzenberg-Solomon R, Cross AJ, Leitzmann MF, Weinstein S, Wood RJ, Virtamo J, Taylor PR, Albanes D, Sinha R (2006) A prospective study of serum C-reactive protein and colorectal cancer risk in men. Cancer Res 66(4):2483–2487
Otani T, Iwasaki M, Sasazuki S, Inoue M, Tsugane S, Japan Public Health Center-Based Prospective Study G (2006) Plasma C-reactive protein and risk of colorectal cancer in a nested case-control study: Japan Public Health Center-based prospective study. Cancer Epidemiol Biomark Prev 15(4):690–695
Nikiteas NI, Tzanakis N, Gazouli M, Rallis G, Daniilidis K, Theodoropoulos G, Kostakis A, Peros G (2005) Serum IL-6, TNFalpha and CRP levels in Greek colorectal cancer patients: prognostic implications. World J Gastroenterol 11(11):1639–1643
Herszenyi L, Tulassay Z (2010) Epidemiology of gastrointestinal and liver tumors. Eur Rev Med Pharmacol Sci 14(4):249–258
Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F (2013) GLOBOCAN 2012 v1.1, cancer incidence and mortality worldwide: IARC CancerBase no. 11. International Agency for Research on Cancer, Lyon. http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx. Accessed on 23/01/2015
Kennedy ET, Ohls J, Carlson S, Fleming K (1995) The Healthy Eating Index: design and applications. J Am Diet Assoc 95(10):1103–1108
Miller PE, Lazarus P, Lesko SM, Muscat JE, Harper G, Cross AJ, Sinha R, Ryczak K, Escobar G, Mauger DT, Hartman TJ (2010) Diet index-based and empirically derived dietary patterns are associated with colorectal cancer risk. J Nutr 140(7):1267–1273. doi:10.3945/jn.110.121780
Panagiotakos DB, Pitsavos C, Stefanadis C (2006) Dietary patterns: a Mediterranean diet score and its relation to clinical and biological markers of cardiovascular disease risk. Nutr Metab Cardiovasc Dis 16(8):559–568
Mitrou PN, Kipnis V, Thiebaut AC, Reedy J, Subar AF, Wirfalt E, Flood A, Mouw T, Hollenbeck AR, Leitzmann MF, Schatzkin A (2007) Mediterranean dietary pattern and prediction of all-cause mortality in a US population: results from the NIH-AARP diet and Health Study. Arch Intern Med 167(22):2461–2468. doi:10.1001/archinte.167.22.2461
Rathod AD, Bharadwaj AS, Badheka AO, Kizilbash M, Afonso L (2012) Healthy Eating Index and mortality in a nationally representative elderly cohort. Arch Intern Med 172(3):275–277. doi:10.1001/archinternmed.2011.1031
Akbaraly TN, Ferrie JE, Berr C, Brunner EJ, Head J, Marmot MG, Singh-Manoux A, Ritchie K, Shipley MJ, Kivimaki M (2011) Alternative Healthy Eating Index and mortality over 18 y of follow-up: results from the Whitehall II cohort. Am J Clin Nutr 94(1):247–253. doi:10.3945/ajcn.111.013128
Reedy J, Krebs-Smith SM, Miller PE, Liese AD, Kahle LL, Park Y, Subar AF (2014) Higher diet quality is associated with decreased risk of all-cause, cardiovascular disease, and cancer mortality among older adults. J Nutr. doi:10.3945/jn.113.189407
Warburton DE, Nicol CW, Bredin SS (2006) Health benefits of physical activity: the evidence. Can Med Assoc J 174(6):801–809. doi:10.1503/cmaj.051351
Van Horn L (1997) Fiber, lipids, and coronary heart disease. A statement for healthcare professionals from the Nutrition Committee, American Heart Association. Circulation 95(12):2701–2704
van Aerde MA, Soedamah-Muthu SS, Geleijnse JM, Snijder MB, Nijpels G, Stehouwer CD, Dekker JM (2013) Dairy intake in relation to cardiovascular disease mortality and all-cause mortality: the Hoorn Study. Eur J Nutr 52(2):609–616. doi:10.1007/s00394-012-0363-z
Kroenke CH, Kwan ML, Sweeney C, Castillo A, Caan BJ (2013) High- and low-fat dairy intake, recurrence, and mortality after breast cancer diagnosis. J Natl Cancer Inst 105(9):616–623. doi:10.1093/jnci/djt027
Li K, Kaaks R, Linseisen J, Rohrmann S (2011) Dietary calcium and magnesium intake in relation to cancer incidence and mortality in a German prospective cohort (EPIC-Heidelberg). Cancer Causes Control 22(10):1375–1382
Pocobelli G, Peters U, Kristal AR, White E (2009) Use of supplements of multivitamins, vitamin C, and vitamin E in relation to mortality. Am J Epidemiol 170(4):472–483
Esmaillzadeh A, Kimiagar M, Mehrabi Y, Azadbakht L, Hu FB, Willett WC (2007) Dietary patterns and markers of systemic inflammation among Iranian Women. J Nutr 137(4):992–998
Festa A, D’Agostino R, Howard G, Mykkänen L, Tracy RP, Haffner SM (2000) Chronic subclinical inflammation as part of the insulin resistance syndrome: the insulin resistance atherosclerosis study (IRAS). Circulation 102(1):42–47. doi:10.1161/01.cir.102.1.42
Bellavia A, Larsson SC, Bottai M, Wolk A, Orsini N (2013) Fruit and vegetable consumption and all-cause mortality: a dose–response analysis. Am J Clin Nutr 98(2):454–459. doi:10.3945/ajcn.112.056119
Steffen LM, Jacobs DR Jr, Stevens J, Shahar E, Carithers T, Folsom AR (2003) Associations of whole-grain, refined-grain, and fruit and vegetable consumption with risks of all-cause mortality and incident coronary artery disease and ischemic stroke: the Atherosclerosis Risk in Communities (ARIC) Study. Am J Clin Nutr 78(3):383–390
Oyebode O, Gordon-Dseagu V, Walker A, Mindell JS (2014) Fruit and vegetable consumption and all-cause, cancer and CVD mortality: analysis of Health Survey for England data. J Epidemiol Community Health 68(9):856–862. doi:10.1136/jech-2013-203500
Lo YT, Chang YH, Wahlqvist ML, Huang HB, Lee MS (2012) Spending on vegetable and fruit consumption could reduce all-cause mortality among older adults. Nutr J 11:113. doi:10.1186/1475-2891-11-113
Harris HR, Bergkvist L, Wolk A (2013) Vitamin C intake and breast cancer mortality in a cohort of Swedish women. Br J Cancer 109(1):257–264. doi:10.1038/bjc.2013.269
Harris HR, Bergkvist L, Wolk A (2012) Selenium intake and breast cancer mortality in a cohort of Swedish women. Breast Cancer Res Treat 134(3):1269–1277. doi:10.1007/s10549-012-2139-9
Bellavia A, Larsson SC, Bottai M, Wolk A, Orsini N (2014) Differences in survival associated with processed and with nonprocessed red meat consumption. Am J Clin Nutr 16:086249
Andersen V, Egeberg R, Tjonneland A, Vogel U (2012) Interaction between interleukin-10 (IL-10) polymorphisms and dietary fibre in relation to risk of colorectal cancer in a Danish case-cohort study. BMC Cancer. doi:10.1186/1471-2407-12-183
Schwab S, Zierer A, Schneider A, Heier M, Koenig W, Kastenmuller G, Waldenberger M, Peters A, Thorand B (2015) Vitamin E supplementation is associated with lower levels of C-reactive protein only in higher dosages and combined with other antioxidants: The Cooperative Health Research in the Region of Augsburg (KORA) F4 study. Br J Nutr 113(11):1782–1791. doi:10.1017/S0007114515000902 (Epub 0007114515002015 Apr 0007114515000921)
Xun P, Liu K, Morris JS, Daviglus ML, Stevens J, Jacobs DR Jr, He K (2010) Associations of toenail selenium levels with inflammatory biomarkers of fibrinogen, high-sensitivity c-reactive protein, and interleukin-6: the CARDIA trace element study. Am J Epidemiol 171(7):793–800. doi:10.1093/aje/kwq1001 (Epub 2010 Mar 1010)
Stepaniak U, Micek A, Grosso G, Stefler D, Topor-Madry R, Kubinova R, Malyutina S, Peasey A, Pikhart H, Nikitin Y, Bobak M, Pajak A (2015) Antioxidant vitamin intake and mortality in three Central and Eastern European urban populations: the HAPIEE study. Eur J Nutr. doi:10.1007/s00394-015-0871-8
Rohrmann S, Overvad K, Bueno-de-Mesquita HB, Jakobsen MU, Egeberg R, Tjonneland A, Nailler L, Boutron-Ruault MC, Clavel-Chapelon F, Krogh V, Palli D, Panico S, Tumino R, Ricceri F, Bergmann MM, Boeing H, Li K, Kaaks R, Khaw KT, Wareham NJ, Crowe FL, Key TJ, Naska A, Trichopoulou A, Trichopoulos D, Leenders M, Peeters PH, Engeset D, Parr CL, Skeie G, Jakszyn P, Sanchez MJ, Huerta JM, Redondo ML, Barricarte A, Amiano P, Drake I, Sonestedt E, Hallmans G, Johansson I, Fedirko V, Romieux I, Ferrari P, Norat T, Vergnaud AC, Riboli E, Linseisen J (2013) Meat consumption and mortality—results from the European Prospective Investigation into Cancer and Nutrition. BMC Med 11:63
Hansson LM, Galanti MR (2000) Diet-associated risks of disease and self-reported food consumption: how shall we treat partial nonresponse in a food frequency questionnaire? Nutr Cancer 36(1):1–6. doi:10.1207/S15327914NC3601_1
Jain M, Howe GR, Harrison L, Miller AB (1989) A study of repeatability of dietary data over a seven-year period. Am J Epidemiol 129(2):422–429
Jensen OM, Wahrendorf J, Rosenqvist A, Geser A (1984) The reliability of questionnaire-derived historical dietary information and temporal stability of food habits in individuals. Am J Epidemiol 120(2):281–290
Lindsted KD, Kuzma JW (1989) Long-term (24-year) recall reliability in cancer cases and controls using a 21-item food frequency questionnaire. Nutr Cancer 12(2):135–149
Mursu J, Steffen LM, Meyer KA, Duprez D, Jacobs DR Jr (2013) Diet quality indexes and mortality in postmenopausal women: the Iowa Women’s Health Study. Am J Clin Nutr 98(2):444–453
Sijtsma FP, Meyer KA, Steffen LM, Shikany JM, Van Horn L, Harnack L, Kromhout D, Jacobs DR Jr (2012) Longitudinal trends in diet and effects of sex, race, and education on dietary quality score change: the Coronary Artery Risk Development in Young Adults study. Am J Clin Nutr 95(3):580–586
Thompson FE, Metzner HL, Lamphiear DE, Hawthorne VM (1990) Characteristics of individuals and long term reproducibility of dietary reports: the Tecumseh Diet Methodology Study. J Clin Epidemiol 43(11):1169–1178
Acknowledgments
Funding
Drs. Shivappa and Hébert were supported by Grant Number R44DK103377 from the US National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Wolk was supported by the Distinguished Professor Award from Karolinska Institute. The Swedish Mammography Cohort is maintained by grants from the Swedish Research Council Committee for infrastructure. Dr Harris was supported by a grant from the Swedish Cancer Foundation.
Disclosure
Dr. James R. Hébert owns controlling interest in Connecting Health Innovations LLC (CHI), a company planning to license the right to his invention of the Dietary Inflammatory Index (DII) from the University of South Carolina in order to develop computer and smart phone applications for patient counseling and dietary intervention in clinical settings. Dr. Nitin Shivappa is an employee of CHI. The subject matter of this paper will not have any direct bearing on that work, nor has that activity exerted any influence on this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared no conflicts of interest.
Rights and permissions
About this article
Cite this article
Shivappa, N., Harris, H., Wolk, A. et al. Association between inflammatory potential of diet and mortality among women in the Swedish Mammography Cohort. Eur J Nutr 55, 1891–1900 (2016). https://doi.org/10.1007/s00394-015-1005-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-015-1005-z