Abstract
Purpose
Early feeding habits may have a significant impact on later body composition and health. The knowledge on dietary habits is, however, still limited for older infants and toddlers. Therefore, we aimed to: (1) assess the average daily energy and macronutrient intakes and to identify their major foods sources; (2) compare it to the nationally and internationally recommended dietary intake (RDI).
Methods
A food survey (January–February 2012) was conducted in a cohort of healthy infants and toddlers, stratified for age, gender, region, occupation and socio-economic status of the mother and week and weekend days. The national dietary software programme Nubel® was used to analyse nutritional values.
Results
We included 92 (19.8 %) 6-to 12-month-olds, 200 (43.0 %) 13- to 24-month-olds and 173 (37.2 %) 25- to 36-month-olds in the analysis. Median energy intake was 15–20 % above the RDI of 79–82 kcal/kg/day. Nearly, all children had a protein intake above the RDI, and for 156 (33.5 %), this was above the upper tolerable limit of 15 % of total energy intake. The median fat intake increased with increasing age and was slightly below the RDI. Mean water and carbohydrate intake were in accordance with the RDI. Fibre intake was below the RDI of 15 g/d for 93.1 % of the oldest and 83.5 % of the middle age group (p < 0.01). Milk is the most important source for energy en macronutrients until the age of 2 years.
Conclusions
Energy and especially protein intakes are too high, while fat and fibre intakes are too low in Belgian infants and toddlers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During the first 2 years of life, children acquire gross and fine motor skills which are required for self-feeding [1, 2]. Toddlers make a transition from a milk-dependent diet in infancy to a more varied independent diet in toddlerhood. Nutrition in late infancy and early toddlerhood may have a significant impact on body composition and health in childhood [3–6] and adult life [7, 8].
A rising prevalence of childhood obesity has been reported worldwide in the last decades [9–11], and several longitudinal cohort studies have linked the exposure to risk factors in childhood with adverse outcome in adulthood [12, 13]. Weber et al. [14] showed that toddlers with a very high protein intake (14 and 20 g protein/day at 3 and 6 months of age, respectively) have a greater risk of becoming obese.
Prevention is the only feasible approach to control the problem of over-nutrition in children and is best started early in life. Survey data from the North American Feeding Infants and Toddlers Study revealed that infants and toddlers, 2- to 24-month-olds, are consuming too many calories: the reported caloric intakes in this survey exceeded energy requirements by 20 % [15].
Since dietary habits can vary among different countries, it is important to adapt prevention programmes to these prevailing local differences. A thorough understanding of national food consumption patterns of very young children can help tailor these recommendations.
However, knowledge of feeding habits in older infants and toddlers is still limited. Therefore, the objectives of this research were as follows: (1) to gain detailed insight into the macronutrient intake of 6- to 36-month-old infants and toddlers in Belgium; (2) to compare the diet in our study population to national feeding recommendations; and (3) to identify the major food sources for energy, protein, carbohydrates and fat in Belgian infants and toddlers.
Methods
Study population
A food survey was conducted between the 13 January and the 27 February 2012 in a nationally stratified cross-sectional study sample involving 500 Belgian mothers of children aged 6 36-month-olds. Study participants were recruited via an independent research marketing bureau (Ipsos) via telephone. Participating parents were given a fee of 7.5 €. In order to obtain representative samples, approximately 50 children were included per 3-month age group (ten groups of 50 children). These age groups were also stratified for gender, region (north/south), occupation and socio-economic status of the mother (based on the category of income) and day of the week for the diary completion. Only healthy infants and toddlers, born at a full-term gestational age, were included. The recruitment was done until the number of 500 stratified children was reached. To avoid missing data in the food diaries due to language difficulties, we decided to only include non-immigrant families in our study. The parents and caregivers did not receive specific recommendations prior to our study, which reflected the genuine daily food consumption of the children according to the children’s and their parents’ choices.
Our study was approved by our local ethical committee and performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All caregivers gave verbal consent for participation in the study.
Collection and analysis of dietary intake data
Participating caregivers were asked to complete a nutritional diary in which they registered all the food and drinks consumed by their baby or toddler during a period of four consecutive days. The caregivers were instructed to specify all ingredients per eating moment. Detailed guidance notes, including a quantity table with an overview of ingredients along with their measurement unit (ml, gr, spoons, etc), were provided for all caregivers and to the day care centres. Location (with parent, other family member/friend or at day care), hour of the day and type of meal (breakfast, lunch, in-between, etc) were also specified for each eating moment.
Fourteen (2.8 %) of the 500 children in our population were at least partially breastfed. In case of breastfeeding, the estimated amount of mother milk was based on the average daily amount of milk intake in the corresponding age category. In case the child drank mother milk and any other kind of milk, the amount of consumed milk was subtracted from the estimated amount of mother milk.
The information gathered in these diaries was then entered in the dietary software programme (Nubel®) to analyse the nutritional value of the diet and the detailed intake of the different nutrients. Nubel® is a Belgian non-profit organisation responsible for the management of the national food composition database (containing brand names as well as product names) in Belgium, which started to collect data from the food industry, food distribution and scientific literature since 1985 onwards. The mean daily energy and nutrient intakes for each child over the registration period were calculated and used for analysis. The results were reported per age group: 6-month- to 1-year-old, 1- to 2-year-old and 2- to 3-year-old children. We also reported that the number of children had a registered intake outside the norm, as determined by the Belgian recommendations. These recommendations reflect the recommended dietary intake (RDI), which is the average requirement +2 SD for all nutrients and the average requirement for energy intake [16]. All different food products were categorized by two researchers (KH and DL), including a registered dietician, into the following food categories: bread and bread products, cereals, potatoes and potato products, pasta and pasta products, ready-made dinners, fish, meat, added fats and oils, cakes and sweets, fruit and vegetables, cheese and milk products, milk, soft drinks, fruit juice, water and soup and others.
Data on body length and weight were acquired using orally reported values.
Calculation, statistical analysis and ethical statement
Weight for age (WFA) and height for age (HFA) data were compared with the reference population described by Roelants et al. [17] and translated into z-scores. Weight and height were missing in one and three children, respectively. Since only healthy children were included, z-scores >3 or <−3 were considered as incorrect and thus removed for weight (n = 34) and height (n = 59).
Because the RDI is sometimes expressed relative to the body weight, children with unknown and/or incorrect weight data (n = 35) were removed, leaving 465 infants and toddlers for statistical analysis. For the calculation of the major food sources for energy and the macronutrients, the median contribution of each food category relative to the total amount of energy and macronutrients over the registration period was used. A Chi-square test or a Fisher’s exact test was performed to compare proportions between groups. Since there was no significant difference in energy intake in any of the age categories (p values ranging from 0.12 to 0.98), no corrections for the number of weekend days were made in the analyses. The means and medians of continuous variables were compared using a Student t test or a Mann–Whitney U test, respectively. A p value of <0.05 was considered significant. The SPSS v 22.0 (SPSS Inc, Chicago Ill., USA) software was used.
Results
Population characteristics
Our study sample consisted of 465 children and was divided into three age categories: 92 (19.8 %) 6- to 12-month-olds, 200 (43.0 %) 13- to 24-month-olds and 173 (37.2 %) 25- to 36-month-olds. As displayed in Table 1, there was no significant difference in any of the investigated population characteristics among different age categories, except for a lower median amount of days in day care for the oldest age category (1 day vs. 2 days in the lower age categories; p = 0.01). The children from the northern part of the country also spent less time in day care than those from the southern part (median (range) number of days 1 (1–5) vs. 2 (1–5), p < 0.01, respectively. The socio-economic status (SES) of the mothers was not significantly different in the three age categories, but there was a slight difference in mean (SD) SES of mothers from the northern versus the southern part of Belgium [2.3 (1.2) vs. 1.9 (1.0); mean difference (95 % CI) of 0.37 (0.2–0.6); p < 0.01, respectively].
Energy and macronutrient intakes
An overview of energy and macronutrient intakes is provided per age category in Table 2. Overall, 326 (70.1 %) children had an energy intake (E intake) above the RDI: 65 (70.7 %) of the 6- to 12-month-old, 152 (76.0 %) of the 13- to 24–month-old and 109 (63.0 %) of the 25- to 36-month-old children. A significant difference (p = 0.04) between both genders could only be observed in the 24- to 36-month-old children, although there was no difference in the percentage of children with an E intake above the RDI (p = 0.10).
Median protein intake (P intake) in the youngest age category was significantly lower than in the middle (boys: p < 0.01, girls: p = 0.01) and oldest age category (boys: p < 0.01, girls: p < 0.01). There was no significant gender difference in any of the age categories (p values between 0.26 and 0.48). All except one (a 6-month-old boy) had a P intake above the RDI, and for 156 (33.5 %) of the children, the P intake was above the upper tolerable limit (UL) of 15 % of total energy intake that was proposed by ESPGHAN (although a slightly lower limit of 14 % of total energy intake was found in earlier research) [18, 19]. The percentage of children with a P intake >UL was significantly (p < 0.01) different among different age categories: 13 (14.1 %) of the children from the youngest, 67 (33.5 %) from the middle and 76 (43.9 %) from the oldest age category. In the 13- to 24-month-old children, there was a strong trend (p = 0.05) for a higher proportion of boys (n = 39; 40.2 %) than girls (n = 28; 27.2 %) with a P intake above the UL. The same difference could not be seen among the youngest (p = 0.37) and oldest (p = 0.32) children.
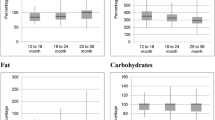
Median fat intake (F intake) increased significantly with increasing age for boys and girls, although the F intake expressed as a percentage of total energy consumption was not significantly different between children from the middle and oldest age category (boys: p = 0.05; girls: p = 0.45). Significantly, more (p = 0.03) children aged >2 years had a F intake below the RDI: 56 (32.4 %) versus 42 (21.0 %) of the 1- to 2-year-olds and 20 (21.7 %) of the children aged <1 years.
Mean daily carbohydrate intake (CH intake) was in accordance with the RDI and decreased (expressed as a percentage of total energy intake) significantly with increasing age category. The percentage of children with a CH intake below the RDI increased, however, significantly (p < 0.01) with increasing age categories: 19 (20.7 %) of the 6- to 12-month-olds, 96 (48.0 %) of the 13- to 24-month-olds and 109 (63.0 %) of the 25- to 36-month-olds.
There was a significantly (p < 0.01) higher median fibre intake (Fb intake) in 6- to 12-month-old boys than in 13- to 24-month-old boys. Significantly (p < 0.01), more 2- to 3-year-olds (n = 161; 93.1 %) than 1- to 2-year-olds (n = 167; 83.5 %) had a Fb intake below the RDI of 15 g/d.
Mean water intake was within the norms for all age categories.
Major food sources of energy and macronutrients
The major food sources for energy and macronutrients are shown in Fig. 1. We provided a more detailed overview of the five most important food sources for each macronutrient in Supplementary file 1. Energy came mainly from: milk (41.3 % of total energy intake (TE intake)), fruits and vegetables (17.9 % of TE) and cakes and sweets (8.5 % of TE intake) in the youngest group; milk (25.4 % of TE), cakes and sweets (14.1 % of TE intake) and bread and bread products (10.3 %) in the middle age group; and cakes and sweets (21.3 % of TE intake), milk (16.8 % of TE intake) and meat (9.5 % of TE intake) in the oldest group. Milk was the main energy source for 84 (91.3 %) of the 6- to 12-month-old children, for 126 (63.0 %) of the 13–24 month-olds and for 54 (31.2 %) of the 25–36 month-olds.
The main sources for protein were as follows: milk (33.0 % of total protein intake (TP intake)), meat (17.3 % of TP intake) and fruits and vegetables (12.0 % of TP intake) in the children <1 year old; milk (24.3 % of TP intake), meat (22.7 % of TP intake) and bread and bread products (9.4 % of TP intake) in the 1- to 2-year-old children; and meat (26.9 % of TP intake), milk (21.7 % of TP intake) and bread and bread products (8.1 % of TP intake) in the 2- to 3-year-old children. For 68 (73.9 %) of the children <1 year, 86 (43.0 %) of the 1- to 2-year-olds and 58 (33.5 %) of the 2- to 3-year-olds, milk intake was the largest contributor of protein intake. Meat was the major protein source in 99 (57.2 %) of the oldest, 84 (42.0 %) of the middle and 18 (19.6 %) of the youngest age group.
Total fat intake (TF intake) was mainly derived from: milk (64.6 % of TF intake), added fats and oils (6.7 % of TF intake) and cakes and sweets (5.5 % of TF intake) in the youngest age group; milk (32.6 % of TF intake), cakes and sweets (13.1 % of TF intake) and added fats and oils (11.5 % of TF intake) in the middle age group; and cakes and sweets (22.9 % of TF intake), meat (15.7 % of TF intake) and added fats and oils (10.4 % of TF intake) in the oldest age group. Milk was the main contributor of fat intake for almost all (n = 86; 93.5 %) of the youngest children, for 124 (62.0 %) of the children in the middle age group and for 51 (29.5 %) of the oldest children.
The major food sources for carbohydrates were mainly from: milk (32.6 % of total carbohydrate intake (TCH intake)), fruits and vegetables (27.7 % of TCH intake) and cakes and sweets (10.0 % of TCH intake) in the 6- to 12-month-olds; milk (21.7 % of TCH intake), fruits and vegetables (16.4 % of TCH intake) and cakes and sweets (16.1 % of TCH intake) in the 13- to 24-month-olds; and cakes and sweets (23.1 % of TCH intake), milk (14.2 % of TCH intake) and bread and bread products (12.5 % of TCH intake) in the 25- to 36-month-olds. Carbohydrates were derived mainly from milk for 52 (56.5 %) of the youngest children, 77 (38.5 %) of the 1- to 2-year-olds and 37 (21.4 %) of the oldest children.
Total fibre intake (total Fb intake) was mainly derived from fruits and vegetables for all age categories (55.3, 45.8 and 36.0 % of total Fb intake in the youngest, middle and oldest children, respectively), followed by potatoes and potato products (18.0, 13.8 and 12.9 % of total Fb intake in the youngest, middle and oldest children respectively). Fruits and vegetables were the major Fb sources for 92.4 % of the 6- to 12-month-olds, 79.5 % of the 13- to 24-month-olds and 69.9 % of the 25- to 36-month-olds.
Discussion
This is the first study on dietary intake of infants and young toddlers in Belgium, and one of the few in this age group. We have shown that almost three quarters of the children had an energy intake above the RDI and that, especially in the 1–2 year-olds, there was a high median daily energy intake. Protein intake was above the RDI for all except one child, and for one-third, it was above the safe UL 15 % of total energy intake [19]. The median fat intake increased with increasing age and was slightly below the RDI. Mean water and carbohydrate intake were in accordance with the RDI. Fibre intake was too low for a large majority of the children. Milk is the most important source for energy and macronutrients until the age of 2 years. For older toddlers, the importance of cakes and sweets increases significantly for the provision of energy and macronutrients.
The results show that only one-third of the infants and toddlers in our population ingest energy amounts within the RDI, which is equal to the estimated average intake in the case of energy. These results are comparable with the few other comparable European studies investigating the diet of infants and toddlers [20–23]. Mean energy intake in the Finnish study, based on a three-day food record, was between 907 and 1134 kcal/d in the 1- to 2-year-olds (1104 kcal/d in our study) and between 1134 and 1244 kcal/d in the 2- to 3-year-olds (1227 kcal/d in our study) [20]. The mean energy intake was slightly higher in a recent Dutch cohort of 2- to 3-year-olds, based on dietary recall data (1315–1383 kcal/d) [23]. Even though the mean daily energy intake of our oldest toddler group is comparable to the MEE of the 2.5- to 4-year-old girls in the Flemish study of Huybrechts and De Henauw (96.7 kcal/kg/d) and even lower for our male toddler population (107.7 vs. 88.8 kcal/kg/d), their conclusions differ greatly from ours: they reported that the mean energy intake of this age group approached the recommended energy intake [24]. Their data were compared, however, with the previous edition of the Belgian food recommendations. The RDI for energy in different European countries is presented in Table 3. The current Belgian recommendations are the same as the most recent WHO guidelines [16, 25], which are up to 20 % lower than those published in 1985 [25, 26]. The difference is mainly due to the fact that the older guidelines were based solely on observed intakes of healthy children growing normally, whereas the current recommendations were derived using a factorial method, based on resting energy expenditure multiplied with the physical activity level. In infants, total energy expenditure was estimated by a regression equation based on doubly labelled water data, plus the energy needs for growth. A similar strategy has been used recently in the European guidelines [27] and other recent European recommendations [28, 29].
Protein intake was above the RDI for nearly all children. The RDI for protein (presented for different institutions in Table 3) has decreased with time. In 1985, the WHO recommended an RDI that was 20–25 % higher than the current recommendations [26, 30]. The current WHO recommendation for a safe level of protein intake is based on the factorial method, in which the mean dietary requirement (the amount needed for maintenance plus the dietary requirement for growth) is summed with 1.96 times the standard deviation. The Dutch guidelines do mention not only an RDI, but also an UL for protein intake: based on studies reporting no adverse effect on health in adults consuming protein contents as high as 25 % of total energy intake [31, 32], the Committee has decided that there should be a gradual increase in the UL for different age groups. An UL of 15 % of total energy intake was set for infants from 6 to 11 months and 20 % for children in the 1–3 year age group [29]. More recently, Agostoni et al. [18, 19] found that high protein intake in 8- to 24-month-old children was associated with later overweight, whereas this association was not seen with dietary protein intakes below 14 % of total energy, which led ESPGHAN to conclude that a protein intake of 15 % of total energy can be considered as the UL. These data were, however, considered insufficient to adopt this UL in the most recent European guidelines [33]. Nonetheless, the mean daily protein intake that has been reported for other European countries has been consentingly high and flirts with the UL: Finnish one- to three-year-olds had an average protein intake of 15.3–16.3 % of total energy intake [20]; for Greek 1- to 5-year-old children, the protein intake was even reported to be as high as 17.1 % of total energy intake [21]. An Italian study of children until the age of 3 reported a mean protein intake of 14.7 % [22], whereas Dutch 2- to 3-year-olds seem to have a slightly lower intake (13 %) [23].
Fat intake in our population was 5–20 % below the RDI, which is in accordance with data from the Netherlands (mean fat intake 18 % below the RDI), Finland and Belgium (both 15 % below the RDI) and Ireland (7 % below the RDI) [20, 23, 24, 34], whereas mean fat intake in Italy and Greece has been reported to be within the norms [21, 22]. The low fibre intake is in accordance with reported low intakes in other European countries (mean European intakes varying between 7.6 and 13 g/day) [20, 22–24, 34].
An import finding of our study was that milk remained the major source for energy and all investigated macronutrients until the age of 2 years. After this age, cakes and sweets gain importance in providing energy, protein and fat. Our findings are confirmed by the results of a recent study of 24-hour recalls in 3022 American infants and toddlers 4–24 months of age, which showed that infant formula (especially in the youngest children) and milk (especially in the oldest children) are the major contributors of energy and most nutrients in the diets of these children [35]. The same findings are reported in the Irish National Preschool Nutrition Survey: whereas milk provided 28.5 % of total energy in the 1-year-olds, it decreased to 13.1 % in the 3-year-olds. The 4-year-old children on the other hand gathered 12.5 % of their energy intake from cakes, pastries, biscuits, desserts, sweets, etc. [34].
Our results show that the diet that is presently consumed by infants and toddlers in Belgium does not meet the nutritional requirements. The current pandemic of obesity in mind seems only sensible to steer feeding habits towards a healthy direction from early on in life. For instance, protein intake at 1 year of age has been associated with overweight at 5 years [36], and lowering the protein content in infant formula has been shown to reduce the body mass index and obesity risk at school age [14]. Recently, a Belgian consensus statement on GUM milks has been published, stating that altering milk intake behaviour in 12- to 36-month-old children can be part of a more global approach when trying to change feeding habits [37]. Two recent studies have shown that the protein intake was lower in GUM-consuming 1- to 2-year-olds than in non-GUM-consuming children [38, 39]. Walton and Flynn also reported a significantly higher fibre intake in the GUM group [39]. The cheapest and likely best solution would be to encourage mothers to prolong the duration of breast feeding along with appropriate complementary food, as only 2.8 % of the children in our population were still breastfed. Prolonged breastfeeding would decrease energy and protein intakes in comparison with non-breastfed infants. A recent Italian cohort study demonstrated that 6-month-olds that were still breastfed had a significantly lower caloric and protein intake than non-breastfed infants [40]. Although it remains important to have an understanding of individual macro- and micronutrient intakes, reference intakes reflect the current knowledge and have been shown to change substantial from one edition to the next. Practical guidelines that focus on eating patterns (which have been shown to correlate with nutrient intakes [41]) of toddlers might therefore be a more sensible approach when providing recommendations to caregivers. There is some data that suggest a beneficial effect of lowering the protein quantity in infant formula on the occurrence of overweight later on in childhood [14]. More similar intervention studies are needed to investigate the effect of increasing the fibre intake (e.g. via fibre-enriched formula feeding or increasing the consumption of fruits and vegetables) or decreasing energy intake through a limitation of the cakes and sweets intake.
The strengths of this study are that it was designed to form a representative image of the daily dietary habits of healthy Belgian infants and toddlers, as our population was stratified for age, gender, region, occupation and socio-economic status of the mother. The technique of dietary records that we used provided us with more detailed data in comparison with studies that used food frequency questionnaires or 24-hour dietary recall for data collection. Although a ‘desirability bias’ is still possible with self-administered dietary records, there is no recall bias as opposed to 24-hour dietary recall [42]. Secondly, our study assessed the available data in two ways: it not only provides insight on how recommendations for energy and macronutrient intakes are being followed, but also provides important information on the food groups from which energy and macronutrients are derived. This can help tailor information campaigns on nutritional habits of infants and toddlers.
This study also has some limitations. First, the fact that we included only non-immigrant families in our study population may lead to a bias in our results when we want to generalize our findings for the entire Belgian population. Studies in other European countries suggest that this would likely lead to underestimation of the inadequate feeding habits in toddlers of minority cultures [43, 44], although a lower protein intake was found in toddlers of Pakistani immigrant families in Italy [45]. Second, parent-reported values were used for the weight and height data. We are, however, confident that in this age range, the bias is minimal. This believe is strengthened by recent reports comparing parents’ reported height and weight data with measured data which have indicated that the bias in reported weight values is larger among older than younger children [46, 47].
In conclusion, the diet that is presently consumed by infants and toddlers in Belgium does not meet the nutritional requirements. Energy and especially protein intakes are far too high, whereas the intake of fibre and dietary fats is too low. Milk is the main contributor of energy and macronutrients until the age of 2 years, whereafter the importance of cakes and sweets increases in energy and macronutrient supply increases. Stimulating mothers to continue breastfeeding after the introduction of complementary feeding might be beneficial in lowering the energy and protein intakes in infants and toddlers. When breastfeeding is no longer possible in older children, tailored nutritional advice is needed for adherence to the nutritional recommendations.
References
Carruth BR, Skinner JD (2002) Feeding behaviors and other motor development in healthy children (2–24 months). J Am Coll Nutr 21(2):88–96
Carruth BR, Ziegler PJ, Gordon A, Hendricks K (2004) Developmental milestones and self-feeding behaviors in infants and toddlers. J Am Diet Assoc 104(1 Suppl 1):51–56. doi:10.1016/j.jada.2003.10.019
Bernard JY, De Agostini M, Forhan A, Alfaiate T, Bonet M, Champion V, Kaminski M, de Lauzon-Guillain B, Charles MA, Heude B (2013) Breastfeeding duration and cognitive development at 2 and 3 years of age in the EDEN mother–child Cohort. J Pediatr. doi:10.1016/j.jpeds.2012.11.090
Kiefte-de Jong JC, de Vries JH, Franco OH, Jaddoe VW, Hofman A, Raat H, de Jongste JC, Moll HA (2012) Fish consumption in infancy and asthma-like symptoms at preschool age. Pediatrics 130(6):1060–1068. doi:10.1542/peds.2012-0875
Magalhaes TC, Vieira SA, Priore SE, Ribeiro AQ, Lamounier JA, Franceschini SC, Sant’Ana LF (2012) Exclusive breastfeeding and other foods in the first 6 months of life: effects on nutritional status and body composition of Brazilian children. Sci World J 2012:468581. doi:10.1100/2012/468581
Ohlund I, Hernell O, Hornell A, Stenlund H, Lind T (2010) BMI at 4 years of age is associated with previous and current protein intake and with paternal BMI. Eur J Clin Nutr 64(2):138–145. doi:10.1038/ejcn.2009.132
Shepherd AA (2008) Nutrition through the life-span. Part 2: children, adolescents and adults. Br J Nurs 17(21):1332–1338
Scowen P (2007) The child is father of the man. J Fam Health Care 17(6):186
Lobstein TJ, James WP, Cole TJ (2003) Increasing levels of excess weight among children in England. Int J Obes 27(9):1136–1138. doi:10.1038/sj.ijo.0802324
Ogden CL, Carroll MD, Kit BK, Flegal KM (2012) Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA J Am Med Assoc 307(5):483–490. doi:10.1001/jama.2012.40
Rolland-Cachera MF, Deheeger M, Thibault H (2001) Epidemiologic bases of obesity. Archives de pediatrie: organe officiel de la societe francaise de pediatrie 8(Suppl 2):287s–289s
Baker JL, Olsen LW, Sorensen TI (2007) Childhood body-mass index and the risk of coronary heart disease in adulthood. New Engl J Med 357(23):2329–2337. doi:10.1056/NEJMoa072515
Magnussen CG, Koskinen J, Chen W, Thomson R, Schmidt MD, Srinivasan SR, Kivimaki M, Mattsson N, Kahonen M, Laitinen T, Taittonen L, Ronnemaa T, Viikari JS, Berenson GS, Juonala M, Raitakari OT (2010) Pediatric metabolic syndrome predicts adulthood metabolic syndrome, subclinical atherosclerosis, and type 2 diabetes mellitus but is no better than body mass index alone: the Bogalusa Heart Study and the Cardiovascular Risk in Young Finns Study. Circulation 122(16):1604–1611. doi:10.1161/circulationaha.110.940809
Weber M, Grote V, Closa-Monasterolo R, Escribano J, Langhendries JP, Dain E, Giovannini M, Verduci E, Gruszfeld D, Socha P, Koletzko B (2014) Lower protein content in infant formula reduces BMI and obesity risk at school age: follow-up of a randomized trial. Am J Clin Nutr 99(5):1041–1051. doi:10.3945/ajcn.113.064071
Saavedra JM, Deming D, Dattilo A, Reidy K (2013) Lessons from the feeding infants and toddlers study in North America: what children eat, and implications for obesity prevention. Ann Nutr Metab 62(Suppl 3):27–36. doi:10.1159/000351538
Hoge Gezondheidsraad (2009) Voedingsaanbevelingen voor België, 2009, nr. 8309. Hoge Gezondheidsraad, Brussel
Roelants M, Hauspie R, Hoppenbrouwers K (2009) References for growth and pubertal development from birth to 21 years in Flanders, Belgium. Ann Hum Biol 36(6):680–694. doi:10.3109/03014460903049074
Agostoni C, Scaglioni S, Ghisleni D, Verduci E, Giovannini M, Riva E (2005) How much protein is safe? Int J Obes 29(Suppl 2):S8–S13
Agostoni C, Decsi T, Fewtrell M, Goulet O, Kolacek S, Koletzko B, Michaelsen KF, Moreno L, Puntis J, Rigo J, Shamir R, Szajewska H, Turck D, van Goudoever J (2008) Complementary feeding: a commentary by the ESPGHAN Committee on nutrition. J Pediatr Gastroenterol Nutr 46(1):99–110. doi:10.1097/01.mpg.0000304464.60788.bd
Kyttala P, Erkkola M, Kronberg-Kippila C, Tapanainen H, Veijola R, Simell O, Knip M, Virtanen SM (2010) Food consumption and nutrient intake in Finnish 1–6-year-old children. Public Health Nutr 13(6a):947–956. doi:10.1017/s136898001000114x
Manios Y, Grammatikaki E, Papoutsou S, Liarigkovinos T, Kondaki K, Moschonis G (2008) Nutrient intakes of toddlers and preschoolers in Greece: the GENESIS study. J Am Diet Assoc 108(2):357–361. doi:10.1016/j.jada.2007.10.042
Sette S, Le Donne C, Piccinelli R, Arcella D, Turrini A, Leclercq C (2011) The third Italian national food consumption survey, INRAN-SCAI 2005-06–part 1: nutrient intakes in Italy. Nutr Metab Cardiovasc Dis NMCD 21(12):922–932. doi:10.1016/j.numecd.2010.03.001
Ocké MC vRC, Fransen HP, Buurma EJM, de Boer EJ, Brandts HAM, Niekerk EM, van der Laan JD, Drijvers JJMM, Ghameshlou Z (2008) Dutch National Food Consumption Survey-Young children 2005/2006. National Institute for Public Health and the Environment
Huybrechts I, De Henauw S (2007) Energy and nutrient intakes by pre-school children in Flanders-Belgium. Br J Nutr 98(3):600–610. doi:10.1017/s000711450773458x
FOA/WHO/UNU (Food and Agriculture Organization of the United States/World Health Organization/United Nations University) (2004) Human energy requirements: report of a joint FAO/WHO/UNU expert consultation. Food and Nutrition technical report series. FOA/WHO/UNU, Rome
FOA/WHO/UNU (Food and Agriculture Organization of the United States/World Health Organization/United Nations University) (1985) Energy and protein requirements: report of a joint FAO/WHO/UNU expert consultation. WHO Technical Report Series. FOA/WHO/UNU, Rome
EFSA Panel on Dietetic Products NaAN (2013) Scientific opinion on dietary reference values for energy. EFSA J 11(1):3005. doi:10.2903/j.efsa.2013.3005
Scientific Advisory Committee on Nutrition (SACN) (2011) Dietary reference values for energy. SACN
Health Council of the Netherlands (2001) Dietary reference intakes: energy, proteins, fats, and digestible carbohydrates. Health council of the Netherlands, The Hague
FOA/WHO/UNU (Food and Agriculture Organization of the United States/World Health Organization/United Nations University) (2002) Protein and amino acid requirements in human nutrition: a report of a joint FAO/WHO/UNU expert consultation. WHO technical report series. WHO, Geneva
Hu FB, Stampfer MJ, Manson JE, Rimm E, Colditz GA, Speizer FE, Hennekens CH, Willett WC (1999) Dietary protein and risk of ischemic heart disease in women. Am J Clin Nutr 70(2):221–227
Skov AR, Toubro S, Ronn B, Holm L, Astrup A (1999) Randomized trial on protein vs carbohydrate in ad libitum fat reduced diet for the treatment of obesity. Int J Obes 23(5):528–536
EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA) (2012) Scientific opinion on dietary reference values for protein. EFSA J 10(2):66. doi:10.2903/j.efsa.2012.2557
Walton J e (2012) National pre-school nutrition survey-summary report. www.iuna.net. Accessed 01 Aug 2014
Fox MK, Reidy K, Novak T, Ziegler P (2006) Sources of energy and nutrients in the diets of infants and toddlers. J Am Diet Assoc 106(1 Suppl 1):28–42. doi:10.1016/j.jada.2005.09.034
Koletzko B, von Kries R, Closa R, Escribano J, Scaglioni S, Giovannini M, Beyer J, Demmelmair H, Gruszfeld D, Dobrzanska A, Sengier A, Langhendries JP, Rolland Cachera MF, Grote V (2009) Lower protein in infant formula is associated with lower weight up to age 2 y: a randomized clinical trial. Am J Clin Nutr 89(6):1836–1845. doi:10.3945/ajcn.2008.27091
Vandenplas Y, De Ronne N, Van De Sompel A, Huysentruyt K, Robert M, Rigo J, Scheers I, Brasseur D, Goyens P (2014) A Belgian consensus-statement on growing-up milks for children 12–36 months old. Eur J Pediatr 173(10):1365–1371. doi:10.1007/s00431-014-2321-7
Ghisolfi J, Fantino M, Turck D, de Courcy GP, Vidailhet M (2013) Nutrient intakes of children aged 1–2 years as a function of milk consumption, cows’ milk or growing-up milk. Public Health Nutr 16(3):524–534. doi:10.1017/s1368980012002893
Walton J, Flynn A (2013) Nutritional adequacy of diets containing growing up milks or unfortified cow’s milk in Irish children (aged 12–24 months). Food Nutr Res. doi:10.3402/fnr.v57i0.21836
Pani P, Carletti C, Knowles A, Parpinel M, Concina F, Montico M, Cattaneo A (2014) Patterns of nutrients’ intake at 6 months in the northeast of Italy: a cohort study. BMC Pediatr 14:127. doi:10.1186/1471-2431-14-127
Smithers LG, Golley RK, Brazionis L, Emmett P, Northstone K, Lynch JW (2012) Dietary patterns of infants and toddlers are associated with nutrient intakes. Nutrients 4(8):935–948. doi:10.3390/nu4080935
Shim JS, Oh K, Kim HC (2014) Dietary assessment methods in epidemiologic studies. Epidemiol Health 36:e2014009. doi:10.4178/epih/e2014009
Kocturk TO, Mjones S (1986) Consumption pattern of infant foods by Turkish immigrants. Scand J Prim Health Care 4(1):13–18
Miguel-Gil B, Cruz-Rodriguez C, Masvidal-Aliberch RM, de Frutos-Gallego E, Estabanell-Buxo A, Riera-Vidal D (2012) Infant feeding in recent immigrant population. Enferm Clin 22(3):118–125. doi:10.1016/j.enfcli.2012.03.002
Venuta A, Rovesti S (2009) Children feeding practices in Pakistani families immigrant to Italy. La Pediatria medica e chirurgica: Med Surg Pediatr 31(4):165–167
Dubois L, Girad M (2007) Accuracy of maternal reports of pre-schoolers’ weights and heights as estimates of BMI values. Int J Epidemiol 36(1):132–138. doi:10.1093/ije/dyl281
O’Connor DP, Gugenheim JJ (2011) Comparison of measured and parents’ reported height and weight in children and adolescents. Obesity 19(5):1040–1046. doi:10.1038/oby.2010.278
Department of Health (1991) Dietary reference values for food energy and nutrients in the United Kingdom. HMSO, London
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
YV is a consultant for Biocodex and United Pharmaceuticals. The other authors have no conflict of interest to declare. DL and TVA received funding from Nutricia BE for their independent research.
Sources of funding
Nutricia Belgium provided the funding for the data gathering, which was performed independently by Ipsos. Nutricia had no role in the analysis and interpretation of the data, or in the writing of the article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Huysentruyt, K., Laire, D., Van Avondt, T. et al. Energy and macronutrient intakes and adherence to dietary guidelines of infants and toddlers in Belgium. Eur J Nutr 55, 1595–1604 (2016). https://doi.org/10.1007/s00394-015-0978-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-015-0978-y