Abstract
Purpose
Folic acid supplementation has been suggested to reduce the risk of preterm birth. However, results from previous epidemiologic studies have been inconclusive. We investigated the hypothesis that folic acid supplementation and dietary folate intake during pre- and post-conception reduces the risk of preterm birth.
Methods
We analyzed data from a birth cohort study conducted between 2010 and 2012 in Lanzhou, China, including 10,179 pregnant women with live singleton births.
Results
Compared to non-users, folic acid supplement users with >12-week duration had a reduced risk of preterm birth (OR 0.67, 95 % CI 0.55–0.83) with a significant dose–response relationship (P for trend = 0.01). A similar pattern was observed for spontaneous preterm birth. Stronger associations were seen for ever use of folic acid supplement and very preterm birth (OR 0.50, 95 % CI 0.36–0.69) and spontaneous very preterm birth (OR 0.42, 95 % CI 0.29–0.63). Dietary folate intake during preconception and pregnancy were also associated with reduced risk of preterm birth (OR 0.68, 95 % CI 0.56–0.83, OR 0.57, 95 % CI 0.47–0.70 for the highest quartiles, respectively), particularly for spontaneous very preterm (OR 0.41, 95 % CI 0.24–0.72, OR 0.26, 95 % CI 0.15–0.47 for the highest quartiles, respectively). There were also decreased risks of preterm birth observed per 10-µg increase in dietary folate intake, and similar associations were found after stratification by folic acid supplementation status.
Conclusions
Our results suggest that folic acid supplementation and higher dietary folate intake during preconception and pregnancy reduces the risk of preterm birth, and the protective effect varies by preterm subtypes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Preterm birth (PB) is the leading cause of neonatal morbidity and mortality [1], and the second leading cause of death in children <5 years of age [2]. Neonatal morbidity and mortality are inversely associated with gestational age at delivery, with most adverse outcomes associated with delivery before 32 weeks gestation [1]. Infants born PB are also more likely to be diagnosed with motor, cognitive, visual, hearing, behavioral, health, and growth problems compared to term infants [3, 4]. Approximately 15 million PB infants are born each year worldwide [5, 6], and the numbers continue to increase [7]. The World Health Organization’s Millennium development goals have named prevention of preterm birth as a global health priority [6].
Folate plays an essential role in DNA synthesis, repair, and methylation [8]. It is particularly important in pregnancy and infancy, which involve rapid cell division and growth. Folic acid supplementation before conception and during the first trimester of pregnancy has been recommended for prevention of neural tube defects [9]. Its role in other pregnancy outcomes, however, has been largely controversial [10]. Randomized controlled trials linking maternal folic acid supplementation to PB have reported inconsistent findings [10–16]. Epidemiologic studies examining folic acid supplementation/dietary folate and PB have also reported mixed results, including positive [17], negative [18–27], and null findings [28–30].
China has one-fifth of the world population, and also the second largest number of PB [31] with PB rates ranges from 4.1 to 18.9 % [7]. A recent study reported that dietary folate intake among Chinese women of childbearing age was far from optimal, especially among women living in northern China [32]. Although taking 400 µg of folic acid daily has been recommended to women of childbearing age by the Chinese Ministry of Health since 1993 [32], the percentage of women who actually took folic acid supplements before and during pregnancy was only around 12 % based on a recent national survey [33]. While folic acid fortification of certain staple foods began in the USA in 1998 [34], no such fortification has been instituted in China. A recent Chinese study found that preconception folic acid supplementation use decreased risk of PB; however, the study did not address dietary folate intake or qualify duration of use [26].
Because studies examining the association between PB and folic acid supplements have provided inconsistent results, and limited studies have been conducted in the Chinese population, we conducted a birth cohort study in Lanzhou, China, to systemically examine the association between folic acid supplementation, dietary folate, and risk of PB.
Materials and methods
Study population
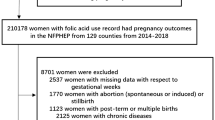
The study population has been described previously [35–37]. In brief, a birth cohort study was conducted during 2010–2012 at the Gansu Provincial Maternity & Child Care Hospital, the largest maternity and child care hospital in Lanzhou, China. Eligible women were recruited upon their arrival at the hospital for delivery. After obtaining written consent, an in-person interview was conducted at the hospital by trained study interviewers using a standardized and structured questionnaire to collect information on demographic, environmental, and lifestyle factors. The majority of women (84 %) were interviewed within 1–3 days after delivery. Information on birth outcomes and maternal complications was abstracted from medical records. A total of 14,359 eligible women were approached for participation, and 10,542 (73.4 %) women completed in-person interviews, with 10,179 women having singleton live birth. All study procedures were approved by the Human Investigation Committees at the Gansu, Provincial Maternity & Child Care Hospital and Yale University.
Preterm birth
Gestational age was calculated in completed weeks from the first day of the last menstrual period until delivery based on medical records and self-reported questionnaire. According to the World Health Organization, a child born before 37 completed weeks of gestation is defined as PB [6]. Term birth is defined as a child born ≥37 completed weeks of gestation. According to gestational age, PB was divided into moderate PB (32 to <37 completed weeks of gestation), very PB (28 to <32 completed weeks), and extremely PB (<28 completed weeks). We combined very and extremely PB together as very PB to increase statistical power. PB was further classified as medically indicated or spontaneous [38, 39]. A medically indicated PB occurs when a placental, uterine, fetal, or maternal condition exists prompting the medical team to proceed with delivery after the risks and benefits of continuing pregnancy versus early delivery are weighed. Examples of risky conditions prompting a decision include: placental abruption, placenta accreta, placenta or vasa previa, prior classical cesarean, uterine rupture or dehiscence, fetal intrauterine growth restriction, select fetal anomalies, severe preeclampsia, uncontrolled gestational or chronic hypertension, complicated pregestational diabetes, and oligohydramnios. Medically indicated PB does not include pregnancies delivered as a result of spontaneous PB labor with or without PB premature rupture of membranes (PPROM).
Folic acid supplementation and dietary folate intake
Data collection on folic acid supplementation and dietary folate intake has been described previously [37]. Briefly, information on folic acid supplements was asked for the following four time periods: preconception (12 months before pregnancy), first trimester (1–13 weeks), second trimester (14–27 weeks), and third trimester (>27 weeks). For each time period, duration and frequency of folic acid supplement use alone and folic acid-containing multivitamins were ascertained. Folic acid supplement users were defined as those who took folic acid supplements alone or folic acid-containing multivitamins during preconception and/or pregnancy. Non-users were defined as those who never took folic acid supplements alone or folic acid-containing multivitamins during preconception and pregnancy. Dietary information was collected via a semi-quantitative food frequency questionnaire. Daily dietary folate intake was estimated from the frequency of consumption and portion size of food items using the Chinese Standard Tables of Food Consumption [40], for each time period [37].
Statistical analyses
Chi-square tests were employed to compare selected characteristics between PB and term-birth groups. Unconditional logistic regression models were used to estimate odds ratios (OR) and 95 % confidence intervals (95 % CI) for the associations between use of folic acid supplements, dietary folate intake, and risk of PB and its clinical subtypes. Folic acid supplements were classified into two levels by midpoint of duration of use, dietary folate intake was categorized to quartiles, and dose–response relationship (P for trend) was calculated based on those categorical levels. Potential confounding variables included maternal age (≤24, 25–29, ≥30 years), education level (<college, ≥college), household monthly income per capita (<3000, ≥3000 RMB), parity (primiparous, multiparous), maternal pre-pregnancy body mass index (BMI) (<18.5, 18.5–23.9, ≥24), employment status during pregnancy (yes, no), maternal diabetes (yes, no), preeclampsia (yes, no), and previous PB (yes, no). Additional adjustment for active and passive smoking, alcohol consumption, cesarean section (C-section), history of abortion, infant gender, and physical activity did not result in material changes in the observed associations, and thus these covariates were not included in the final models. The analyses examining dietary folate intake excluded subjects with missing dietary data (N = 212). All analyses were performed using SAS software, version 9.3 (SAS Institute, Inc., Cary, North Carolina).
Results
Of the 10,179 women in our study, 1019 women had PB (<37 completed weeks of gestation). Distributions of selected characteristics for study population are presented in Table 1. Compared to women who delivered term birth, women who delivered PB were more likely to be either younger (<25 year-old) or older (≥30 year-old), have lower education and income, be unemployed, and be smokers. Women who delivered PB were also more likely to be multiparous, have higher BMI, less weight gain during pregnancy, previous PB, and C-section, and be diagnosed with preeclampsia and maternal diabetes. Distributions of alcohol consumption, history of abortion, physical activity during pregnancy, and infant’s gender were similar between term and PB groups.
A total of 7864 women reported to be folic acid supplement users, and 2315 women reported to be non-users (Table 2). Compared to non-users, users were more likely to be older, be employed, have higher education and income, have more weight gain during pregnancy, and physically active during pregnancy. Women who reported using folic acid supplement were less likely to be multiparous, be diagnosed preeclampsia and maternal diabetes.
Compared to non-users, folic acid supplement users had a reduced risk of PB (OR 0.80, 95 % CI 0.68–0.94, Table 3). The significant reduced risk was mainly seen for those who had used folic acid supplements for more than 12 weeks (OR 0.67, 95 % CI 0.55–0.83) with a significant dose–response (P for trend = 0.01). After stratifying by time periods of use, significant associations were observed for those who took supplements during both preconception and pregnancy (OR 0.75, 95 % CI 0.61–0.92) or during pregnancy only (OR 0.82, 95 % CI 0.69–0.97). A significant dose–response for duration of use was only observed for those who used during pregnancy only (P for trend = 0.005). No significant association was observed among women who took supplements during preconception only.
After stratifying by PB subtypes (Table 3), significant protective effects of folic acid supplement use were seen for very PB (OR 0.50, 95 % CI 0.36–0.69 for ever users; OR 0.47, 95 % CI 0.30–0.75 for during both preconception and pregnancy; OR 0.21, 95 % CI 0.59–0.88 for during preconception only; and OR 0.53, 95 % CI 0.37–0.75 for during pregnancy only) and spontaneous PB (OR 0.77, 95 % CI 0.64–0.93 for ever users; OR 0.73, 95 % CI 0.57–0.93 for during both preconception and pregnancy; and OR 0.77 95 % CI 0.63–0.94 for during pregnancy only). A significantly reduced risk of moderate PB was also seen for ever users who used for more than 12 weeks (OR 0.74, 95 % CI 00.59–0.94) and users who used during pregnancy only for more than 8 weeks (OR 0.79, 95 % CI 0.63–0.99).
Reduced risk of PB was also associated with higher estimated intake of dietary folate (Table 4). During preconception, a significant protective effect was seen for the highest quartile of dietary folate intake compared to the lowest quartile (OR 0.68, 95 % CI 0.56–0.83). Similar associations were observed for each clinical subtype. During pregnancy, a protective effect was shown for higher levels of dietary folate intake (OR 0.70, 95 % CI 0.59–0.84 for the second quartile; OR 0.67, 95 % CI 0.55–0.80 for the third quartile; and OR 0.57, 95 % CI 0.47–0.70 for the highest quartile) with significant dose–response (P for trend <0.001), and there was 0.2 % increased risk observed per 10-µg increase in dietary folate. Similar patterns were observed for moderate PB, medically indicated PB, and spontaneous PB. Stronger protective effect was seen for very PB (OR 0.62, 95 % CI 0.43–0.90 for the second quartile; OR 0.33, 95 % CI 0.21–0.52 for the third quartile; OR 0.28, 95 % CI 0.17–0.47 for the highest quartile, P for trend <0.001; and OR 0.949, 95 % CI 0.931–0.968 per 10-µg increase in dietary folate).
Although similar associations were observed for spontaneous PB with and without PPROM (Table 5), significantly reduced risk was observed for spontaneous PB with PPROM for folic acid users (OR 0.49, 95 % CI 0.33–0.73) and spontaneous PB without PPROM for higher estimated dietary folate intake (OR 0.60, 95 % CI 0.44–0.81 for the highest quartile level during preconception; OR 0.47, 95 % CI 0.35–0.63 for the highest quartile level during pregnancy; and OR 0.979, 95 % CI 0.969–0.990 per 10-µg increase in dietary folate).
We also stratified medically indicated and spontaneous PB into moderate and very PB (Table 6). The strongest association with folic acid supplements and estimated dietary folate intake was mainly seen for spontaneous very PB (OR 0.43, 95 % CI 0.29–0.63 for ever use folic acid supplements; OR 0.40 95 % CI 0.23–0.70 for the highest quartile intake of dietary folate during preconception with P for trend = 0.001; OR 0.26, 95 % CI 0.14–0.46 for the highest quartile intake of dietary folate during pregnancy with P for trend <0.001; and OR 0.942, 95 % CI 0.920–0.965 per 10-µg increase in dietary folate).
Stratified analysis by folic acid supplementation was also conducted (Table 7). Similar effects of estimated dietary intake on risk of preterm birth were found between folic acid supplement users and non-users, although slightly stronger protective effects were observed among non-users.
We explored potential effect modifications of maternal age, pre-pregnancy BMI, and parity on the associations between folic acid supplements and dietary folate intake and risk of PB. None of these variables modified the associations (data not shown). We did not observe a synergistic effect between dietary folate intake and folic acid supplement use (data not shown). Fewer subjects were folic acid-containing multivitamin users compared to folic acid supplement-alone users (21 vs. 79 %), and similar inverse associations were observed for using either type of folic acid supplements (data not shown).We analyzed the data by excluding birth defects and reached the same conclusion (data not shown). We also conducted a sensitivity analysis for dietary folate intake to exclude poor quality of either under- or over-reporting of the calculated energy intake [41], 892 (8.8 %) participants with energy intake of <4.5 MJ/day (1075 kcal/day) and 50 (0.5 %) participants with energy intake of >20 MJ/day (4777 kcal/day) were excluded, and similar results were observed (data not shown).
Discussion
Our study results suggest that folic acid supplements and high dietary folate intake are associated with a reduced risk of PB, and the reduced risk may vary by PB subtype.
Earlier epidemiological studies investigating the associations between PB and folic acid supplements/dietary folate intake have provided conflicting results [17–30, 42]; among them, Dunlop et al. [43] investigated plasma level of folate. While ten studies have reported a protective effect of folic acid supplements/dietary folate intake on PB [18–27], one study reported that risk of PB associated with folic acid supplement use varied by time periods of use (preconception, first trimester, and second trimester) [17] and four studies found no association [28–30, 42]. Variations in dosage of folic acid use, selected pregnancy period of use, definitions of PB by gestational age, and lack of consideration of PB clinical subtypes among different populations might partially contribute to the inconsistent results.
PB is a complex phenotype and different subtypes may have different etiologies [44]. Our study found a stronger reduced risk of spontaneous very preterm associated with folic acid supplements, which was consistent with some of the previous reports [19, 21]. Spontaneous very PB has been strongly associated with intrauterine infection [45]. Bacterial vaginosis has been shown to double the risk of spontaneous preterm delivery [46–48]. Lower folate concentration in maternal blood has been associated with impaired immune function, and subsequent high prevalence of urinary tract infection and bacterial vaginosis in pregnancy [43, 49]. Therefore, it is biologically plausible that folic acid supplements reduce the risk of spontaneous PB through promotion of immune function and prevention of infection [50].
Our study suggested that starting folic acid supplementation during preconception and early pregnancy, but not late pregnancy, decreased the risk of PB. Studies have suggested that intrauterine infection may occur early in pregnancy and remain undetected for months, resulting in spontaneous preterm labor or rupture of the membranes [45]. Folate concentration in serum continues to decrease for several weeks after pregnancy [51, 52] with folate total body half-life of 100 days [53]. Starting folic acid supplementation from preconception or the first trimester would maximize folate concentration in plasma and suppression of inflammatory processes as early as possible. Insufficient folic acid supplementation leads to lower concentrations of folate in plasma or red blood cells [54, 55].
Our study also found significant association between duration of folic acid supplementation and risk of overall PB and spontaneous PB during preconception and pregnancy, indicating that longer duration of intake had a beneficial effect on reduction in PB risk. Bukowski et al. [19] reported that women with ≥1 year of preconception folic acid supplementation have a reduction in the risk of PB, compared to <1 year of intake. Other studies did not explore this association by duration of maternal supplementation.
Consistent with several earlier studies [22, 23, 27], but not all [17, 20, 29, 30], we found that higher dietary folate intake during pregnancy was associated with reduced risk of PB and certain subtypes. We did not observe a synergistic effect between dietary folate and folic acid supplements.
A major strength of our cohort is that we collected detailed information on both folic acid supplements and dietary folate intake. While our study had a relatively large sample size, statistical power was limited for stratified analyses. Although many important confounding factors have been adjusted for, we cannot rule out the potential for residual confounding. Because information on dietary folate and folic acid supplementation was collected through in-person interview at delivery, there was potential for recall bias. However, the relationships between folic acid supplementation, dietary folate intake, and risk of PB have not been well established and were unlikely to be known by the general public. Therefore, if there was any recall bias, it was likely to be non-differential and resulted in underestimation of the observed associations. Although the study was hospital based, which might impact generalizability, the PB rate (10.0 %) in our study population or (12.2 %) in the whole birth cohort were within the range of the reported rates (4.1–18.9 %) in other Chinese populations, as reviewed by Blencowe et al. [7]. A total of 87.4 % of the folic acid supplement users took 400 µg folic acid daily; therefore, we had limited power to examine the relationship with other doses. Recommendation of taking folic acid supplements starting from 3 months before pregnancy through the end of first trimester pregnancy has been exercised in China since 2009 to prevent neural tube defects [56]. While 77.2 % of women reported being folic acid users in our study population, only 29.0 % of women adhered to the recommendation. A survey in China conducted in 2008 reported an intake rate of 12 % among all women from the national-level poverty counties [33]. The higher intake rate in our study population could be because our study only focused on pregnant women in Lanzhou, which is an urban city in China with relatively higher education and income levels. Future studies are needed to identify women who would most benefit from folic acid supplementation.
In conclusion, our study supports the hypothesis that both folic acid supplementation and high dietary folate intake prior to and during pregnancy reduce the risk of PB, with stronger protective effect for spontaneous PB and very PB. The findings from our study have important public health implications and may facilitate acceptance of taking folic acid supplements during preconception and pregnancy.
Abbreviations
- PB:
-
Preterm birth
- PPROM:
-
Preterm premature rupture of membranes
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- BMI:
-
Body mass index
References
Behrman RE, Butler AS, Institute of Medicine (US), Committee on understanding premature birth and assuring healthy outcomes (eds) (2007) Preterm birth: causes, consequences, and prevention. National Academies Press (US), Washington, DC
Liu L, Johnson HL, Cousens S (2012) Child Health Epidemiology Reference Group of WHO and UNICEF. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet 379:2151–2161
Moster D, Lie RT, Markestad T (2008) Long-term medical and social consequences of preterm birth. N Engl J Med 359:262–273. doi:10.1056/NEJMoa0706475
Yao RYZY, Li HY, Yuan CJ, Hu CL et al (2007) Intelligence development of preterm infants in adolescence. Chin J Sch Health 28:440
Beck S, Wojdyla D, Say L, Betran AP, Merialdi M, Requejo JH, Rubens C, Menon R, Van Look PF (2010) The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity. Bull World Health Organ 88:31–38. doi:10.2471/BLT.08.062554
Howson CP, Kinney MV, McDougall L, Lawn JE, the Born Too Soon Preterm Birth Action Group (2013) Born too soon: preterm birth matters. Reprod Health 10(suppl 1):S1. doi:10.1186/1742-4755-10-S1-S1
Blencowe H, Cousens S, Oestergaard MZ, Chou D, Moller AB, Narwal R, Adler A, Vera Garcia C, Rohde S, Say L, Lawn JE (2012) National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet 379:2162–2172. doi:10.1016/S0140-6736(12)60820-4
Selhub J (1999) Homocysteine metabolism, annual review of nutrition, vol 19, pp 217–246. doi:10.1146/annurev.nutr.19.1.217
World Health Organization, Department of Making Pregnancy Safer, Department of Reproductive Health and Research (2007) Prevention of neural tube effects. In: Standards for maternal and neonatal care. Group 1: General standards of care for healthy pregnancy and childbirth. http://www.who.int/reproductivehealth/publications/maternal_perinatal_health/a91272/en/
Fekete K, Berti C, Trovato M, Lohner S, Dullemeijer C, Souverein OW, Cetin I, Decsi T (2012) Effect of folate intake on health outcomes in pregnancy: a systematic review and meta-analysis on birth weight, placental weight and length of gestation. Nutr J 11:75. doi:10.1186/1475-2891-11-75
Fletcher J, Gurr A, Fellingham FR, Prankerd TA, Brant HA, Menzies DN (1971) The value of folic acid supplements in pregnancy. J Obstet Gynaecol Br Commonw 78:781–785
Fleming AF, Martin JD, Stenhouse NS (1974) Pregnancy anaemia, iron and folate deficiency in Western Australia. Med J Aust 2:479–484
Charles DH, Ness AR, Campbell D, Smith GD, Whitley E, Hall MH (2005) Folic acid supplements in pregnancy and birth outcome: re-analysis of a large randomised controlled trial and update of Cochrane review. Paediatr Perinat Epidemiol 19:112–124. doi:10.1111/j.1365-3016.2005.00633.x
Czeizel AE, Dudas I, Metneki J (1994) Pregnancy outcomes in a randomised controlled trial of periconceptional multivitamin supplementation. Final report. Arch Gynecol Obstet 255:131–139
Baumslag N, Edelstein T, Metz J (1970) Reduction of incidence of prematurity by folic acid supplementation in pregnancy. Br Med J 1:16–17
Fawzi WW, Msamanga GI, Spiegelman D, Urassa EJ, McGrath N, Mwakagile D, Antelman G, Mbise R, Herrera G, Kapiga S, Willett W, Hunter DJ (1998) Randomised trial of effects of vitamin supplements on pregnancy outcomes and T cell counts in HIV-1-infected women in Tanzania. Lancet 351:1477–1482
Sengpiel V, Bacelis J, Myhre R, Myking S, Pay AD, Haugen M, Brantsaeter AL, Meltzer HM, Nilsen RM, Magnus P, Vollset SE, Nilsson S, Jacobsson B (2013) Folic acid supplementation, dietary folate intake during pregnancy and risk for spontaneous preterm delivery: a prospective observational cohort study. BMC Pregnancy Childbirth 13:160. doi:10.1186/1471-2393-13-160
Papadopoulou E, Stratakis N, Roumeliotaki T, Sarri K, Merlo DF, Kogevinas M, Chatzi L (2013) The effect of high doses of folic acid and iron supplementation in early-to-mid pregnancy on prematurity and fetal growth retardation: the mother-child cohort study in Crete, Greece (Rhea study). Eur J Nutr 52:327–336. doi:10.1007/s00394-012-0339-z
Bukowski R, Malone FD, Porter FT, Nyberg DA, Comstock CH, Hankins GD, Eddleman K, Gross SJ, Dugoff L, Craigo SD, Timor-Tritsch IE, Carr SR, Wolfe HM, D’Alton ME (2009) Preconceptional folate supplementation and the risk of spontaneous preterm birth: a cohort study. PLoS Med 6:e1000061. doi:10.1371/journal.pmed.1000061
Shaw GM, Carmichael SL, Nelson V, Selvin S, Schaffer DM (2004) Occurrence of low birthweight and preterm delivery among California infants before and after compulsory food fortification with folic acid. Public Health Rep 119:170–173
Catov JM, Bodnar LM, Ness RB, Markovic N, Roberts JM (2007) Association of periconceptional multivitamin use and risk of preterm or small-for-gestational-age births. Am J Epidemiol 166:296–303. doi:10.1093/aje/kwm071
Scholl TO, Hediger ML, Schall JI, Khoo CS, Fischer RL (1996) Dietary and serum folate: their influence on the outcome of pregnancy. Am J Clin Nutr 63:520–525
Siega-Riz AM, Savitz DA, Zeisel SH, Thorp JM, Herring A (2004) Second trimester folate status and preterm birth. Am J Obstet Gynecol 191:1851–1857. doi:10.1016/j.ajog.2004.07.076
Rolschau J, Kristoffersen K, Ulrich M, Grinsted P, Schaumburg E, Foged N (1999) The influence of folic acid supplement on the outcome of pregnancies in the county of Funen in Denmark. Part I. Eur J Obstet Gynecol Reprod Biol 87:105–110 (discussion 103–104)
Czeizel AE, Puho EH, Langmar Z, Acs N, Banhidy F (2010) Possible association of folic acid supplementation during pregnancy with reduction of preterm birth: a population-based study. Eur J Obstet Gynecol Reprod Biol 148:135–140. doi:10.1016/j.ejogrb.2009.10.016
Li Z, Ye R, Zhang L, Li H, Liu J, Ren A (2014) Periconceptional folic acid supplementation and the risk of preterm births in China: a large prospective cohort study. Int J Epidemiol 43:1132–1139. doi:10.1093/ije/dyu020
Shaw GM, Carmichael SL, Yang W, Siega-Riz AM, National Birth Defects Prevention S (2011) Periconceptional intake of folic acid and food folate and risks of preterm delivery. Am J Perinatol 28:747–752. doi:10.1055/s-0031-1280855
Timmermans S, Jaddoe VW, Hofman A, Steegers-Theunissen RP, Steegers EA (2009) Periconception folic acid supplementation, fetal growth and the risks of low birth weight and preterm birth: the Generation R Study. Br J Nutr 102:777–785. doi:10.1017/S0007114509288994
Nilsen RM, Vollset SE, Monsen AL, Ulvik A, Haugen M, Meltzer HM, Magnus P, Ueland PM (2010) Infant birth size is not associated with maternal intake and status of folate during the second trimester in Norwegian pregnant women. J Nutr 140:572–579. doi:10.3945/jn.109.118158
Alwan NA, Greenwood DC, Simpson NA, McArdle HJ, Cade JE (2010) The relationship between dietary supplement use in late pregnancy and birth outcomes: a cohort study in British women. BJOG 117:821–829. doi:10.1111/j.1471-0528.2010.02549.x
WHO (2012) Preterm birth. Accessed Nov 2013. http://www.who.int/mediacentre/factsheets/fs363/en/
Zhao Y, Hao L, Zhang L, Tian Y, Cao Y, Xia H, Deng Y, Wang T, Yu M, Li Z (2009) Plasma folate status and dietary folate intake among Chinese women of childbearing age. Matern Child Nutr 5:104–116. doi:10.1111/j.1740-8709.2008.00172.x
Zeng Z, Zhu J (2010) Low folic acid supplement intake rate among women in northern China with a high-prevalence of neural tube defects, 2008. Prev Med 51:338–339. doi:10.1016/j.ypmed.2010.07.015
Williams LJ, Rasmussen SA, Flores A, Kirby RS, Edmonds LD (2005) Decline in the prevalence of spina bifida and anencephaly by race/ethnicity: 1995–2002. Pediatrics 116:580–586. doi:10.1542/peds.2005-0592
Qiu J, He X, Cui H, Zhang C, Zhang H, Dang Y, Han X, Chen Y, Tang Z, Zhang H, Bai H, Xu R, Zhu D, Lin X, Lv L, Xu X, Lin R, Yao T, Su J, Liu X, Wang W, Wang Y, Ma B, Liu S, Huang H, Lerro C, Zhao N, Liang J, Ma S, Ehrenkranz RA, Liu Q, Zhang Y (2014) Passive smoking and preterm birth in urban China. Am J Epidemiol 180:94–102. doi:10.1093/aje/kwu092
Zhao N, Qiu J, Zhang Y, He X, Zhou M, Li M, Xu X, Cui H, Lv L, Lin X, Zhang C, Zhang H, Xu R, Zhu D, Lin R, Yao T, Su J, Dang Y, Han X, Zhang H, Bai H, Chen Y, Tang Z, Wang W, Wang Y, Liu X, Ma B, Liu S, Qiu W, Huang H, Liang J, Chen Q, Jiang M, Ma S, Jin L, Holford T, Leaderer B, Bell ML, Liu Q, Zhang Y (2015) Ambient air pollutant PM10 and risk of preterm birth in Lanzhou, China. Environ Int 76:71–77. doi:10.1016/j.envint.2014.12.009
Wang Y, Zhao N, Qiu J, He X, Zhou M, Cui H, Lv L, Lin X, Zhang C, Zhang H, Xu R, Zhu D, Dang Y, Han X, Zhang H, Bai H, Chen Y, Tang Z, Lin R, Yao T, Su J, Xu X, Liu X, Wang W, Ma B, Liu S, Qiu W, Huang H, Liang J, Wang S, Ehrenkranz RA, Kim C, Liu Q, Zhang Y (2015) Folic acid supplementation and dietary folate intake, and risk of preeclampsia. Eur J Clin Nutr. doi:10.1038/ejcn.2014.295
American College of O, Gynecologists (2013) ACOG committee opinion no. 560: medically indicated late-preterm and early-term deliveries. Obstet Gynecol 121:908–910. doi:10.1097/01.AOG.0000428648.75548.00
Spong CY, Mercer BM, D’Alton M, Kilpatrick S, Blackwell S, Saade G (2011) Timing of indicated late-preterm and early-term birth. Obstet Gynecol 118:323–333. doi:10.1097/AOG.0b013e3182255999
Institute of Nutrition and Food Hygiene, Chinese Academy of Preventive Medicine (1999) Table of food components (national representative values). People’s Hygiene Press, Beijing
Meltzer HM, Brantsaeter AL, Ydersbond TA, Alexander J, Haugen M (2008) Methodological challenges when monitoring the diet of pregnant women in a large study: experiences from the Norwegian Mother and Child Cohort Study (MoBa). Matern Child Nutr 4:14–27. doi:10.1111/j.1740-8709.2007.00104.x
Dunlop AL, Taylor RN, Tangpricha V, Fortunato S, Menon R (2012) Maternal micronutrient status and preterm versus term birth for black and white US women. Reprod Sci 19:939–948. doi:10.1177/1933719112438442
Dunlop AL, Taylor RN, Tangpricha V, Fortunato S, Menon R (2011) Maternal vitamin D, folate, and polyunsaturated fatty acid status and bacterial vaginosis during pregnancy. Infect Dis Obstet Gynecol 2011:216217. doi:10.1155/2011/216217
Pennell CE, Jacobsson B, Williams SM, Buus RM, Muglia LJ, Dolan SM, Morken NH, Ozcelik H, Lye SJ, Relton C (2007) Genetic epidemiologic studies of preterm birth: guidelines for research. Am J Obstet Gynecol 196:107–118. doi:10.1016/j.ajog.2006.03.109
Goldenberg RL, Hauth JC, Andrews WW (2000) Intrauterine infection and preterm delivery. N Engl J Med 342:1500–1507. doi:10.1056/NEJM200005183422007
Eschenbach DA, Gravett MG, Chen KC, Hoyme UB, Holmes KK (1984) Bacterial vaginosis during pregnancy. An association with prematurity and postpartum complications. Scand J Urol Nephrol Suppl 86:213–222
Hillier SL, Nugent RP, Eschenbach DA, Krohn MA, Gibbs RS, Martin DH, Cotch MF, Edelman R, Pastorek JG 2nd, Rao AV et al (1995) Association between bacterial vaginosis and preterm delivery of a low-birth-weight infant. The Vaginal Infections and Prematurity Study Group. N Engl J Med 333:1737–1742. doi:10.1056/NEJM199512283332604
Meis PJ, Goldenberg RL, Mercer B, Moawad A, Das A, McNellis D, Johnson F, Iams JD, Thom E, Andrews WW (1995) The preterm prediction study: significance of vaginal infections. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Am J Obstet Gynecol 173:1231–1235
Greenberg JA, Bell SJ, Guan Y, Yu YH (2011) Folic Acid supplementation and pregnancy: more than just neural tube defect prevention. Rev Obstet Gynecol 4:52–59
Christian P, Jiang T, Khatry SK, LeClerq SC, Shrestha SR, West KP Jr (2006) Antenatal supplementation with micronutrients and biochemical indicators of status and subclinical infection in rural Nepal. Am J Clin Nutr 83:788–794
Bruinse HW, van den Berg H (1995) Changes of some vitamin levels during and after normal pregnancy. Eur J Obstet Gynecol Reprod Biol 61:31–37
Smith AM, Picciano MF, Deering RH (1983) Folate supplementation during lactation: maternal folate status, human milk folate content, and their relationship to infant folate status. J Pediatr Gastroenterol Nutr 2:622–628
Nijhout HF, Reed MC, Budu P, Ulrich CM (2004) A mathematical model of the folate cycle: new insights into folate homeostasis. J Biol Chem 279:55008–55016. doi:10.1074/jbc.M410818200
Malinow MR, Rajkovic A, Duell PB, Hess DL, Upson BM (1998) The relationship between maternal and neonatal umbilical cord plasma homocyst(e)ine suggests a potential role for maternal homocyst(e)ine in fetal metabolism. Am J Obstet Gynecol 178:228–233
Martin JD, Davis RE, Stenhouse N (1967) Serum folate and vitamin B12 levels in pregnancy with particular reference to uterine bleeding and bacteriuria. J Obstet Gynaecol Br Commonw 74:697–701
Policy and Research Team, Save the Children China Programme. Laws and policies for matyernal and young child health care in China. Accessed 12 April 2015. http://resourcecentre.savethechildren.se/sites/default/files/documents/3378.pdf
Acknowledgments
Research supported by internal funding from the Gansu Provincial Maternity and Child Care Hospital, and by the National Institutes of Health Grants (K02HD70324 and R01ES019587).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Xiaohui Liu, Ling Lv, Hanru Zhang and Nan Zhao have contributed equally to the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liu, X., Lv, L., Zhang, H. et al. Folic acid supplementation, dietary folate intake and risk of preterm birth in China. Eur J Nutr 55, 1411–1422 (2016). https://doi.org/10.1007/s00394-015-0959-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-015-0959-1