Abstract
Purpose
To examine whether a body shape index (ABSI) calculated by using waist circumference (WC) adjusted for height and weight could improve the predictive performances for cardiovascular disease (CVD) of the Framingham’s general CVD algorithm and to compare its predictive performances with other anthropometric measures.
Methods
We analyzed data on a 10-year population-based follow-up of 8,248 (4,471 women) individuals aged ≥30 years, free of CVD at baseline. CVD risk was estimated for a 1 SD increment in ABSI, body mass index (BMI), waist-to-hip ratio (WHpR) and waist-to-height ratio (WHtR), by incorporating them, one at a time, into multivariate accelerated failure time models.
Results
ABSI was associated with multivariate-adjusted increased risk of incident CVD among both men (1.26, 95 % CI 1.09–1.46) and women (1.17, 1.03–1.32). Among men, for a one-SD increment, ABSI conferred a greater increase in the hazard of CVD [1.26 (1.09–1.46)] than did BMI [1.06 (0.94–1.20)], WC [1.15(1.03–1.28)], WHpR [1.02 (1.01–1.03)] and WHtR [1.16 (1.02–1.31)], and the corresponding figures among women were 1.17 (1.03–1.32), 1.02 (0.90–1.16), 1.11 (0.98–1.27), 1.03 (1.01–1.05) and 1.14 (0.99–1.03), respectively. ABSI as well as other anthropometric measures failed to add to the predictive ability of the Framingham general CVD algorithm either.
Conclusions
Although ABSI could not improve the predictability of the Framingham algorithm, it provides more information than other traditional anthropometric measures in settings where information on traditional CVD risk factors are not available, and it can be used as a practical criterion to predict adiposity-related health risks in clinical assessments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is no consensus on the definition and specific aspects of obesity that contribute to the risk of CVD [1]. The precise measurement of the total amount of body fat and its regional distribution is possible by using computed tomography (CT) and dual-energy X-ray absorption. Magnetic resonance imaging (MRI) also can separate visceral fat from subcutaneous fat with no radiation. However, these methods are costly and not routinely available.
Accordingly, there is a need for simple techniques that can distinguish regional fat. Amato et al. [2] created a novel sex-specific index to indirectly express visceral fat based on waist circumference (WC), body mass index (BMI), triglycerides (TGs) and high-density lipoprotein cholesterol (HDL-C), and termed it the visceral adiposity index (VAI). We have demonstrated that using VAI instead of simple anthropometric measures of adiposity may lead to loss of considerable information needed for predicting incident CVD [3]. Statistically speaking, information means the amount of variation in a variable of outcome explained by predictors. In regression analyses, this is usually measured by predictive performances of different models. Measures of predictive performances vary by the type of regression procedure implemented [4–6]. When the predictive performance of a model incorporating variable A is inferior to the predictive performance of the model incorporating variable B, then using model A instead of model B means choosing the inferior predictive performance, which causes considerable loss of information [7–12]. Most recently, Krakauer et al. [13] developed a new measure index “a body shape index (ABSI)” based on WC adjusted for height and weight.
Using data from a large community-based prospective study, we examined whether ABSI could improve the CVD prediction by Framingham general CVD algorithm and also whether ABSI could outperform simple anthropometric measures of adiposity, i.e., BMI, waist-to-height ratio (WHtR) or waist-to-hip ratio (WHpR).
Methods
Study design
Detailed descriptions of the Tehran lipid and glucose study (TLGS) have been reported elsewhere [14]. In brief, the TLGS is a large scale, long-term, community-based prospective study performed on a representative sample of residents of district 13 of Tehran, the capital of Iran. The TLGS has two major components: a cross-sectional prevalence study of non-communicable disease and associated risk factors, implemented between March 1999 and December 2001, and a prospective follow-up study. Data collection is ongoing, designed to continue for at least 20 years, on triennial basis. Parallel with cyclic examinations, participants are followed annually for any medical condition by trained nurses via telephone calls. Currently, there are at least 27 million fixed telephone lines in Iran with 77 million populations. A trained physician collects complementary data during a home visit and a visit to the respective hospital to collect data from the participants’ medical files.
We hereby certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research. Informed written consent was obtained from all participants and the Ethical Committee of Research Institute for Endocrine Sciences approved this study.
Study population
A total of 27,340 residents aged ≥3 years were invited by telephone call, of which 15,010 residents participated in the first examination cycle and another 3,551 residents were first examined at the second examination cycle. Participants were categorized into the cohort (n = 10,394) and intervention groups (n = 8,167), the latter to be educated for implementation of lifestyle modifications. For the current study, among participants aged ≥30 years at their baseline examination (9,814) who attended the follow-up study till 31 March 2010, we selected subjects free of CVD at baseline for whom complete data were available on outcome and risk factors (n = 8,248). At the time of this study, the median follow-up time was 10.1 years.
Lifestyle modification intervention
The design of the lifestyle intervention in the TLGS has been published before [14]. Interventions were aimed at lifestyle modification through primary preventions for non-communicable diseases by improving nutrition and dietary pattern, increasing physical activity levels and reducing cigarette smoking. Nutrition education classes were held 4 days a week. Twelve adults on average participated in these educational sessions. Educational programs included face-to-face consultation, educational videos and slides, and nutritional education and consultation, which involved demonstrations of healthy food preparation. During religious ceremonies (sessions in mosques, particularly during the holy month of Ramadan), lectures were given to participants about the main topics of intervention. Public conferences on occasions such as World Diabetes Day or World No-Tobacco Day were held to promote the importance of healthy lifestyle behaviors. The school-based lifestyle modification program was also designed as a multidisciplinary health promotion program using a population approach. The program was intended to influence anti-tobacco, healthy nutrition and physical activity practices [15].
We included all participants to capture full statistical power of the study sample. Meanwhile, we were also able to study the interaction in the effects of variables of interest and the population-based lifestyle modification interventions. However, as lifestyle modification was evenly distributed across different levels of ABSI and did not contribute to the outcome of interest, we therefore have not looked at its effect.
Clinical and laboratory measurements
Using a pretested questionnaire, a trained interviewer collected information on demographic data, family history of premature CVD, past medical history of CVD, drug history and smoking status. Details of anthropometric and biochemical measurements, as well as blood pressure measurements, were addressed elsewhere [14].
Outcome measurements
Details of cardiovascular outcomes have been published elsewhere [16]. In this ongoing study, every TLGS participant was first called by telephone and preliminary information was collected by a trained nurse regarding any medical conditions. Complementary data were then collected by a trained physician during a home visit and a visit to the respective hospital to collect data from the participants’ medical files. Collected data were evaluated by an outcome committee consisting of a principal investigator, an internist, an endocrinologist, a cardiologist, an epidemiologist and the physician who collected the outcome data. A specific outcome for each event is assigned according to International Statistical Classification of Diseases and Related Health Problems criteria (10th revision) and the American Heart Association classification for cardiovascular events [14]. Coronary heart disease (CHD) includes cases of definite myocardial infarction (MI) diagnosed by electrocardiogram (ECG) and biomarkers, probable MI (positive ECG findings plus cardiac symptoms or signs and biomarkers showing negative or equivocal results), unstable angina pectoris (new cardiac symptoms or changing symptom patterns and positive ECG findings with normal biomarkers), angiographic proven CHD and CHD death. CVD is specified as a composite measure of any CHD events, stroke or cerebrovascular death.
We have also conducted a study to assess the validity of outcome measurement in the TLGS [17].
Definition of terms
Following Krakauer et al. [13], we defined ABSI as:
A previous history of CVD reflected any prior diagnosis of CVD by a physician. A current smoker was defined as a person who smokes cigarettes daily or occasionally. Diabetes was ascertained in participants with FPG ≥ 7.0 mmol l−1 or 2 h-PCPG ≥ 11.1 mmol l−1 [18] or use of oral hypoglycemic agents or insulin. For each participant who was free of CVD at baseline, the baseline risk of CVD was calculated by re-estimating the Framingham’s “general CVD risk prediction algorithm [19, 20]”.
Statistics analysis
Findings on covariate variables are expressed as means (SD) or percentages for continuously and categorically distributed variables, respectively. We tested for trends across ABSI quintiles by using the median in each quartile as a predictor, separately for each sex. Statistical significance in trends was examined by implementing age-adjusted general linear models. The Cox proportional hazard regression model was used to test the significance of trends in incident rates.
In the analysis of CVD outcome, ABSI, BMI, WC, WHpR and WHtR were assessed using accelerated failure time method: Weibull survival regression model. Survival time was the time from start of the follow-up period to the date of the first incident CVD event (failure). The censoring time of an individual was the time from entry into the study to loss to follow-up or the end of the study, whichever happened first. Censored observation also meant the individuals either refused to participate further in the study (lost to follow-up), died (from non-CVD causes), when death was not the study outcome (competing risk) or continued until the study was ended (administrative censoring). Valid comparison of hazards ratios (HRs) for different continuous measures requires that the units of both variables be comparable. We, therefore, estimated sex-specific unadjusted and multivariate-adjusted HRs, with 95 % confidence intervals (95 % CIs) for CVD events for a one-SD increment in ABSI and each respective anthropometric parameter. The multivariate regression analyses were controlled for confounding bias due to potential confounders from Framingham general CVD algorithm, i.e., age, systolic blood pressure, use of antihypertensive drugs, total and HDL cholesterol, diabetes and smoking [20].
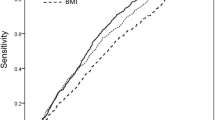
We compared the predictive performance of the ABSI with those of the studied anthropometric variables in terms of the effect size (HR), calibration, discrimination, and added predictive ability.
Wald tests of the linear hypotheses concerning the Weibull survival regression models coefficients (paired homogeneity test) were performed to test the null hypotheses that the hazard ratios (effect size) for ABSI were equal to those for anthropometric measures. We assessed collinearity of BMI, WC, WHpR, and WHtR, with VAI using the variance inflation factor (VIF). VIFs > 10 warrant caution [21]. VIFs were all <10, and therefore, collinearity did not appear to be a problem.
Assessment of model performance
We used several criteria to compare the overall diagnostic values of alternative models. Calibration of a model, as it is phrased in Ref. [4], describes how closely predicted probabilities agree numerically with actual outcomes [22, 23]. A test very similar to the Hosmer–Lemeshow test has been proposed by Nam and D’Agostino. We calculated the Nam–D’Agostino χ 2to examine calibration for prediction models [4]. As suggested by Nam and D’Agostino, calibration χ 2 values >20 (P < 0.01) suggest lack of adequate calibration [4].
In the survival analysis, Harrell’s C statistic measures the probability that a randomly selected person who developed an event at the certain specific time has a higher risk score than a randomly selected person who did not develop an event during the same, specified follow-up interval [24]. The maximum value for Harrell’s C statistic is 1.0, thereby indicating a (theoretically) perfect test (i.e., 100 % sensitive and 100 % specific). A Harrell’s C statistic value of 0.5 indicates no discriminative value (i.e., 50 % sensitive and 50 % specific).
Discriminations measures are not sensitive to changes in absolute risk [25]. Therefore, we calculated absolute and relative integrated discrimination improvement index (IDI) and cut-point-based and cut-point-free net reclassification improvement index (NRI). IDI and NRI are measures of predictive ability added to an old model by a newer one [25]. Bootstrapping method was implemented in order to obtain bias-corrected 95 % CIs.
In order to be able to capture a potential nonlinear association of ABSI with CVD, multivariate restricted cubic splines with four knots defined at the 5th, 25th, 75th and 95th percentile were used. This method enabled us to flexibly model ABSI while preventing instability and the generation of artificial features to some extent [26].
The statistical significance level was set at a two-tailed type I error of 0.05. All statistics analyses were performed using STATA version 12 (STATA, College Station, Texas, USA) and SAS 9.2 (SAS Institute Inc., Cary, NC, USA).
Ethics
Informed written consent was obtained from all participants, and the Ethical Committee of Research Institute for Endocrine Sciences approved this study.
Results
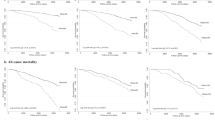
A total of 8,248 (4,471 women) adult participants of the TLGS contributed to a total of 75,975 person-years follow-up, with the median follow-up time for the current analysis being 10.1 years. We documented 671 (women 261) CVD events with the annual incidence rate of CVD events being 9.7 (95 % 8.9–10.6) per 1,000 persons: women 6.2 (5.5–7.0) and men 12.1 (11.0–13.4).
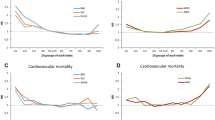
Tables 1 and 2 present the baseline characteristics of participants according to quintiles of ABSI. In general, CVD risk factor levels at baseline increased in stepwise fashion across ABSI quintiles; except for smoking and TC among men and anti-hypertensive drug usage and smoking among women. The annual incidence rate of CVD events showed an increasing trend across quintiles of ABSI among both men and women (P < 0.001).
For a one-SD increment, ABSI conferred a greater increase in the hazard of CVD than did BMI, WC, WHpR and WHpR (Table 3). The results were consistent among both men and women. An increased risk of future CVD was observed across increasing levels of ABSI; the increased risk resisted adjustments for the traditional CVD risk factors like age, systolic blood pressure, using antihypertensive drugs, total and HDL cholesterol, diabetes and smoking.
As shown in Table 4, among women, ABSI failed to attain consistent superiority for predicting CVD over any other anthropometric measures as indicated by contradictory results from absolute and relative IDI and cut-point-based and cut-point-free NRI. However, among men, the predictive ability of ABSI was superior to BMI, WC and WHpR, but not to WHtR.
As shown in Table 5, ABSI as well as other anthropometric measures investigated failed to add to the predictive ability of the Framingham general CVD algorithm. In fact, when anthropometric measures were added to the algorithm, the values for NRI and IDI were negative; indicating that the basic Framingham general CVD algorithm without any anthropometric measure predicted 10-year risk of developing CVD far better than the enhanced algorithms with anthropometric measures added each at a time.
Multivariate restricted cubic splines regression analysis demonstrated that ABSI–CVD dose–response relations had no threshold and yielded straight lines when risk of disease was plotted on a logarithmic scale. As such, hazard ratios have been reported so as to indicate the strength of linear associations.
HRs for incident CVD of the lifestyle modification intervention measures were 1.04 (95 % CIs 0.85–1.26, P value = 0.732) among men and 1.07 (95 % CIs 0.83–1.37, P value = 0.587) among women. Intervention measures did not contribute to the risk of CVD; neither did the intervention measures modify the effects of ABSI on the risk of incident CVD (P for interaction: men 0.784 and women 0.544).
Discussion
In this large community-based cohort of a West Asian population, we investigated the association of ABSI with 10-year risk of developing incident CVD. In general, ABSI was observed to be associated with traditional CVD risk factors. The risk of developing CVD increased in a linear fashion with increasing levels of ABSI among both men and women, without any threshold being detectable. We observed that the magnitude of HR for CVD conferred by ABSI was higher than those conferred by other anthropometric measures. However, clinically speaking, ABSI was not found to consistently add to the predictive values of anthropometric measures. None of the anthropometric measures were found to improve the predictive performances of Framingham general CVD algorithm. Although ABSI could not improve the predictability of Framingham algorithm, it did provide more information than other traditional anthropometric measures.
Epidemiologic studies have found strong association between obesity and a series of diseases particularly CVD and diabetes, as well as increasing in death rates from CVD and all causes [27–30]. In order to develop appropriate preventative strategies to tackle CVD and other obesity complications, there is a deep need for understanding the association between measures of adiposity and cardio-metabolic risk factors such as blood levels of cholesterol and TGs. To understand these associations, the distribution of fat should be studied along with the total amount of body fat [31]. Some studies showed that central fat (accumulation of fat in the abdominal area) is more strongly related to cardiovascular risk than peripheral fat [32, 33]. Therefore, achieving a reliable and accurate estimation of body fatness and fat distribution is essential in both clinical and epidemiological settings [34]. Some techniques for body composition assessment such as densitometry, dual-energy X-ray absorptiometry and MRI provide more accurate information on fat masses and its regional distribution; however, they are expensive, time consuming and impractical for use in routine clinics and epidemiological studies [35]. Furthermore, these measures are not routinely accessible [3]. For the last 30 years, obesity has been measured by BMI [29]. However, some limitations restricted the utility of BMI for stratifying cardio-metabolic risks [36]. An important limitation of the BMI is its inability to distinguish between fat and lean mass, which show opposing relations with health risk. Therefore, compared with direct measurement of percent body fat, BMI significantly underestimates the prevalence of obesity [37]. Furthermore, BMI is a measure of general body mass, not central adiposity, which has been shown to be a stronger predictor of CVD [27, 38]. It has been shown that measures of adiposity are correlated with cardiovascular risk, but no single adiposity measure has been shown to be the best predictor [39]. To more accurately measure central adiposity, some studies suggest using of WC, WHpR or WHtR instead of BMI [34, 40]. A global agreement on a single measure that best represents the adiposity-associated health risk continues to be lacking.
ABSI, which is a new obesity measure based on WC adjusted for height and weight, was expected to improve the assessment of obesity [13]. High ABSI indicates that WC is higher than expected for a given height and weight and corresponds to a more central accumulation of body volume [13, 41]. ABSI has been postulated to contribute to defining the risk of sarcopenia among those who are overweight or obese. In other words, there is an inverse relationship between “a body shape index” (ABSI) and fat-free mass among both women and men [42]. Sarcopenic obesity is generally defined as high fat to fat-free mass ratio. Skeletal muscle may be negatively influenced by the pro-inflammatory milieu associated with visceral fat, while the loading effect induced by a heavier BMI may enhance muscle anabolism [43–45]. Previous studies indicated that height has been inversely associated with CVD [46]. As such, it may be prudent to correct WC for height especially in men with lower WC and higher height [47, 48]. There is a weak correlation between ABSI and height [49]. Putting together the impact of different anthropometric measures (i.e., the effects of general, central and gluteal adiposity altogether) can help more precisely exploring explore how body size and obesity might contribute to the risk of CVD [50].
In the current study, we observed that ABSI was a better predictor of CVD compared with other anthropometric indices. However, the superiority of ABSI in predicting CVD decreased after considering the traditional CVD risk factors in multivariate models. As such, much of ABSI superiority might have possibly stemmed from the amount of information (or statistically speaking, variations) that it shared with the traditional CVD risk factors. Despite having weaknesses in conferring any additional predictability to Framingham general CVD algorithm, ABSI provides more information than other traditional anthropometric measures in settings where information on traditional CVD risk factors is not available. Therefore, it can still be used as a practical criterion to predict adiposity-related health risks in clinical assessments.
There are few studies investigating the predictability of ABSI for different metabolic disturbances. The predictability of the ABSI for mortality might not hold across all sub-groups. For example, although ABSI shows good correlation with surgical complications in patients with gastric cancer [51], it is not independently associated with mortality among patients on renal replacement therapy [52]. In some studies, no superiority has been found for ABSI over other anthropometric measures in prediction of CVD and metabolic syndrome [41, 49]. Yin Bun Cheung, in the study conducted in a middle-age and older Indonesian population, reported that ABSI was less strongly associated with incident hypertension than were WC and BMI [53]. In contrast, in a sample of Portuguese adolescents, ABSI explained a greater amount of the variance in blood pressure than did WC and BMI. As such, when examining the effect of weight status on BP, it would be justified to consider use of ABSI alongside BMI [54]. Krakauer et al. [13] showed that ABSI was an independent predictor of 5-year mortality in a US population of non-pregnant adults. Data from the Spanish EPIC cohort study support the suggestion of using more than one obesity index (ABSI and other obesity indices together) in the study of stroke risk prediction [50]. Future studies are needed to delineate the limits of ABSI’s utility in different ethnic groups [13, 41].
A marker strongly associated with outcome is generally assumed to be effective for classifying persons according to their current or future outcome. However, for this assumption to be true, the associated relative risk must be of a magnitude rarely seen in epidemiologic studies. As such, the relative clinical utility of risk factors could not be fully captured by merely comparing the magnitude of their hazard ratios [25, 55–61]. We found that ABSI, despite having larger HRs, failed to attain consistent superiority, in terms of predictive capacity for CVD, over any other anthropometric measures as indicated by contradictory results from absolute and relative IDI and cut-point-based and cut-point-free NRI among women. The predictive abilities of these anthropometric measures for CVD risks did not differ significantly.
ABSI is not a direct surrogate measure of adiposity, rather it has been developed using a mathematical model with an intention to combine the effects of different surrogates of adiposity. What we have studied here is whether or not such a modeling strategy for combining the effects of different anthropometric measures could be any superior to what could be generally done via traditional regression models. The effect of the ABSI or other anthropometric measurements on health status might have been mediated by some components of the Framingham algorithm. This may explain why these measures failed to achieve superiority over the algorithm. On the other hand, variations in each individual component of the Framingham algorithm might not have been accounted for by variations in the anthropometric measures. As such, they may have been able to explain the variation in CVD above and beyond what could have been done by anthropometric measures. For example, hypertension; while associated with adiposity, it is affected by many other factors that are independent of adiposity. Consequently, the contribution of hypertension to CVD could not be explained by adiposity. However, hypertension can reflect a pathway through which adiposity affects the cardiovascular health status. Finally, there are some predictors, such as smoking, in the CVD risk score that predict CVD independently of the adiposity. Therefore, it is not surprising that a combination of all these predictors as mirrored in “Framingham general CVD risk algorithms” performs better than any other anthropometric measures do.
The strength of our prospective study lies in a reasonable sample size, length of follow-up and direct measurement of the anthropometric measures rather than relying on the self-reported measurements. The large sample size enables us to investigate the sex-specific contribution of ABSI to the risk of incident CVD. To the best of our knowledge, this is the first study that examined the sex-specific predictive ability of ABSI as standalone or as a component of a prediction model in concert with other CVD risk factors. Furthermore, we have extended our investigation beyond merely comparing the magnitude of the relative risks and have explored the clinical usefulness of competing markers using the novel statistical approaches of NRI and IDI. However, data for the current study were secured from a Middle Eastern population, and further studies will be required to investigative reproducibility of our findings across different ethnicities.
In conclusion, we observed that ABSI, independently of traditional risk factors, can predict the 10-year incidence of CVD in both adult men and women. Although ABSI could not improve the predictability of Framingham algorithm, it provides more information than do other traditional anthropometric measures in settings where information on traditional CVD risk factors are not available, and it may be used as a practical criterion to predict adiposity-related health risks in clinical assessments.
Abbreviations
- ABSI:
-
A body shape index
- BMI:
-
Body mass index
- CHD:
-
Coronary heart disease
- CVD:
-
Cardiovascular disease
- CT:
-
Computed tomography
- ECG:
-
Electrocardiography
- HDL-C:
-
High-density lipoprotein cholesterol
- MI:
-
Myocardial infarction
- MRI:
-
Magnetic resonance imaging
- TGs:
-
Triglycerides
- TLGS:
-
Tehran lipid and glucose study
- VIF:
-
Variance inflation factor
- WC:
-
Waist circumference
- WHpR:
-
Waist-to-hip ratio
- WHtR:
-
Waist-to-height ratio
- FPG:
-
Fasting plasma glucose
- 2 h-PCPG:
-
2-h post-challenge plasma glucose
References
Litwin SE (2008) Which measures of obesity best predict cardiovascular risk? J Am Coll Cardiol 52(8):616–619. doi:10.1016/j.jacc.2008.05.017
Amato MC, Giordano C, Galia M, Criscimanna A, Vitabile S, Midiri M, Galluzzo A, Group ftAS (2010) visceral adiposity index. Diabetes Care 33(4):920–922. doi:10.2337/dc09-1825
Mohammadreza B, Farzad H, Davoud K, Prof AF (2012) Prognostic significance of the complex” visceral adiposity index” vs. simple anthropometric measures: Tehran lipid and glucose study. Cardiovasc Diabetol 11:20
D’Agostino RB, Nam BH (2004) Evaluation of the performance of survival analysis models: discrimination and calibration measures. In: Balakrishnan N, Rao CR (eds) Handbook of statistics, survival methods, vol 23. Elsevier, Amsterdam, pp 1–25. doi:10.16/S0169-7161(03)23001-7
D’Agostino RB Sr, Grundy S, Sullivan LM, Wilson P (2001) Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA 286(2):180–187
D’Agostino RB Sr, Pencina MJ (2012) Invited commentary: clinical usefulness of the Framingham cardiovascular risk profile beyond its statistical performance. Am J Epidemiol 176(3):187–189. doi:10.1093/aje/kws203
Steyerberg EW (2009) Clinical prediction models: a practical approach to development, validation, and updating. Springer, New York
Harrell FE (2001) Regression modeling strategies. Springer, New York
Harrell FE Jr, Lee KL, Mark DB (1996) Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 15(4):361–387. doi:10.1002/(SICI)1097-0258(19960229)15:4<361:AID-SIM168>3.0.CO;2-4
Altman DG, Bland JM (1994) Statistics Notes: Diagnostic tests 2: predictive values. BMJ 309(6947):102
Altman DG, Royston P (2000) What do we mean by validating a prognostic model? Stat Med 19(4):453–473. doi:10.1002/(SICI)1097-0258(20000229)19:4<453:AID-SIM350>3.0.CO;2-5
Altman DG, Vergouwe Y, Royston P, Moons KG (2009) Prognosis and prognostic research: validating a prognostic model. BMJ 338:b605
Krakauer NY, Krakauer JC (2012) A new body shape index predicts mortality hazard independently of body mass index. PLoS ONE 7(7):e39504. doi:10.1371/journal.pone.0039504
Azizi F, Ghanbarian A, Momenan AA, Hadaegh F, Mirmiran P, Hedayati M, Mehrabi Y, Zahedi-Asl S (2009) Prevention of non-communicable disease in a population in nutrition transition: Tehran lipid and glucose study phase II. Trials 10(1):5. doi:10.1186/1745-6215-10-5
Harati H, Hadaegh F, Momenan AA, Ghanei L, Bozorgmanesh MR, Ghanbarian A, Mirmiran P, Azizi F (2010) Reduction in incidence of type 2 diabetes by lifestyle intervention in a middle eastern community. Am J Prev Med 38(6):628–636. doi:10.1016/j.amepre.2010.03.003 e621
Hadaegh F, Harati H, Ghanbarian A, Azizi F (2006) Association of total cholesterol versus other serum lipid parameters with the short-term prediction of cardiovascular outcomes: Tehran lipid and glucose study. Eur J Cardiovasc Prev Rehabil 13(4):571–577. doi:10.1097/01.hjr.0000216552.81882.ca
Khalili D, Mosavi-Jarrahi A, Eskandari F, Mousavi-Jarrahi Y, Hadaegh F, Mohagheghi M, Azizi F (2012) Evaluation of cause of deaths’ validity using outcome measures from a prospective, population based cohort study in Tehran, Iran. PLoS One 7(2):e31427. doi:10.1371/journal.pone.0031427
Genuth S, Alberti KG, Bennett P, Buse J, Defronzo R, Kahn R, Kitzmiller J, Knowler WC, Lebovitz H, Lernmark A, Nathan D, Palmer J, Rizza R, Saudek C, Shaw J, Steffes M, Stern M, Tuomilehto J, Zimmet P (2003) Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care 26(11):3160–3167
D’Agostino RB Sr, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WB (2008) General cardiovascular risk profile for use in primary care: the Framingham heart study. Circulation 117(6):743–753. doi:10.1161/circulationaha.107.699579
Bozorgmanesh M, Hadaegh F, Azizi F (2011) Predictive accuracy of the ‘Framingham’s general CVD algorithm’ in a Middle Eastern population: Tehran lipid and glucose study. Int J Clin Pract 65(3):264–273. doi:10.1111/j.1742-1241.2010.02529.x
Abbate LM, Stevens J, Schwartz TA, Renner JB, Helmick CG, Jordan JM (2006) Anthropometric measures, body composition, body fat distribution, and knee osteoarthritis in women. Obesity (Silver Spring) 14(7):1274–1281. doi:10.1038/oby.2006.145
Hosmer DW, Lemeshow S (2000) Applied logistic regression. Wiley-Interscience, New Jersey
Hosmer DW, Lemeshow S, May S (2008) Applied survival analysis : regression modeling of time-to-event data, 2nd edn. Wiley-Interscience, Hoboken
Hlatky MA, Greenland P, Arnett DK, Ballantyne CM, Criqui MH, Elkind MSV, Go AS, Harrell FE Jr, Hong Y, Howard BV, Howard VJ, Hsue PY, Kramer CM, McConnell JP, Normand S-LT, O’Donnell CJ, Smith SC Jr, Wilson PWF, on behalf of the American Heart Association Expert Panel on Subclinical Atherosclerotic D, Emerging Risk F, the Stroke C (2009) Criteria for evaluation of novel markers of cardiovascular risk: a scientific statement from the American Heart Association. Circulation 119(17):2408–2416. doi:10.1161/circulationaha.109.192278
Pencina MJ, D’Agostino RB Sr, D’Agostino RB Jr, Vasan RS (2008) Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med 27(2):157–172; discussion 207–112. doi:10.1002/sim.2929
Royston P, Sauerbrei W (2007) Multivariable modeling with cubic regression splines: a principled approach. Stata J 7(1):45–70
Gwynn RC, Berger M, Garg RK, Waddell EN, Philburn R, Thorpe LE (2011) Measures of adiposity and cardiovascular disease risk factors, New York City Health and Nutrition Examination Survey, 2004. Prev Chronic Dis 8(3):A56
Bergman RN, Stefanovski D, Buchanan TA, Sumner AE, Reynolds JC, Sebring NG, Xiang AH, Watanabe RM (2011) A better index of body adiposity. Obesity 19(5):1083–1089
Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell M, Korinek J, Allison TG, Batsis J, Sert-Kuniyoshi F, Lopez-Jimenez F (2008) Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes 32(6):959–966
Goto M, Morita A, Goto A, Deura K, Sasaki S, Aiba N, Shimbo T, Terauchi Y, Miyachi M, Noda M, Watanabe S (2013) Reduction in adiposity, beta-cell function, insulin sensitivity, and cardiovascular risk factors: a prospective study among Japanese with obesity. PLoS ONE 8(3):e57964. doi:10.1371/journal.pone.0057964
Guasch-Ferre M, Bullo M, Martinez-Gonzalez MA, Corella D, Estruch R, Covas MI, Aros F, Warnberg J, Fiol M, Lapetra J, Munoz MA, Serra-Majem L, Pinto X, Babio N, Diaz-Lopez A, Salas-Salvado J (2012) Waist-to-height ratio and cardiovascular risk factors in elderly individuals at high cardiovascular risk. PLoS ONE 7(8):e43275. doi:10.1371/journal.pone.0043275
Pi-Sunyer FX (2000) Obesity: criteria and classification. In: Proceedings-nutrition society of London, Cambridge University Press, pp 505–509
Coutinho T, Goel K, de Sá DC, Carter RE, Hodge DO, Kragelund C, Kanaya AM, Zeller M, Park JS, Kober L (2013) Combining body mass index with measures of central obesity in the assessment of mortality in subjects with coronary disease role of “normal weight central obesity”. J Am Coll Cardiol 61(5):553–560
Bibiloni Mdel M, Pons A, Tur JA (2013) Defining body fatness in adolescents: a proposal of the afad—a classification. PLoS ONE 8(2):e55849. doi:10.1371/journal.pone.0055849
Haroun D, Taylor SJ, Viner RM, Hayward RS, Darch TS, Eaton S, Cole TJ, Wells JC (2010) Validation of bioelectrical impedance analysis in adolescents across different ethnic groups. Obesity 18(6):1252–1259
Heymsfield SB, Cefalu WT (2013) Does body mass index adequately convey a patient’s mortality risk? JAMA 309(1):87–88
Shah NR, Braverman ER (2012) Measuring adiposity in patients: the utility of body mass index (BMI), percent body fat, and leptin. PLoS ONE 7(4):e33308
Mokha JS, Srinivasan SR, DasMahapatra P, Fernandez C, Chen W, Xu J, Berenson GS (2010) Utility of waist-to-height ratio in assessing the status of central obesity and related cardiometabolic risk profile among normal weight and overweight/obese children: the Bogalusa Heart Study. BMC pediatr 10(1):73
Knowles KM, Paiva LL, Sanchez SE, Revilla L, Lopez T, Yasuda MB, Yanez ND, Gelaye B, Williams MA (2011) Waist circumference, body mass index, and other measures of adiposity in predicting cardiovascular disease risk factors among Peruvian adults. Int J Hypertens. doi:10.4061/2011/931402
Ashwell M, Gunn P, Gibson S (2012) Waist‐to‐height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta‐analysis. Obesity reviews
He S, Chen X (2013) Could the new body shape index predict the new onset of diabetes mellitus in the Chinese population? PLoS ONE 8(1):e50573
Biolo G, Di Girolamo FG, Breglia A, Chiuc M, Baglio V, Vinci P, Toigo G, Lucchin L, Jurdana M, Praznikar ZJ, Petelin A, Mazzucco S, Situlin R (2014) Inverse relationship between “a body shape index” (ABSI) and fat-free mass in women and men: insights into mechanisms of sarcopenic obesity. Clin Nutr (Edinburgh, Scotland). doi:10.1016/j.clnu.2014.03.015
Dufour AB, Hannan MT, Murabito JM, Kiel DP, McLean RR (2013) Sarcopenia definitions considering body size and fat mass are associated with mobility limitations: the Framingham Study. J Gerontol A Biol Sci Med Sci 68(2):168–174. doi:10.1093/gerona/gls109
Batsis JA, Mackenzie TA, Barre LK, Lopez-Jimenez F, Bartels SJ (2014) Sarcopenia, sarcopenic obesity and mortality in older adults: results from the National Health and Nutrition Examination Survey III. Eur J Clin Nutr 68(9):1001–1007. doi:10.1038/ejcn.2014.117
Kim TN, Yang SJ, Yoo HJ, Lim KI, Kang HJ, Song W, Seo JA, Kim SG, Kim NH, Baik SH, Choi DS, Choi KM (2009) Prevalence of sarcopenia and sarcopenic obesity in Korean adults: the Korean sarcopenic obesity study. Int J Obes 33(8):885–892
Langenberg C, Shipley MJ, Batty GD, Marmot MG (2005) Adult socioeconomic position and the association between height and coronary heart disease mortality: findings from 33 years of follow-up in the Whitehall Study. Am J Public Health 95(4):628
Schneider HJ, Friedrich N, Klotsche J, Pieper L, Nauck M, John U, Dorr M, Felix S, Lehnert H, Pittrow D (2010) The predictive value of different measures of obesity for incident cardiovascular events and mortality. J Clin Endocrinol Metab 95(4):1777–1785
Ashwell M, Hsieh SD (2005) Six reasons why the waist-to-height ratio is a rapid and effective global indicator for health risks of obesity and how its use could simplify the international public health message on obesity. Int J Food Sci Nutr 56(5):303–307
Haghighatdoost F, Sarrafzadegan N, Mohammadifard N, Asgary S, Boshtam M, Azadbakht L (2014) Assessing body shape index as a risk predictor for cardiovascular diseases and metabolic syndrome among Iranian adults. Nutrition 30(6):636–644
Abete I, Arriola L, Etxezarreta N, Mozo I, Moreno-Iribas C, Amiano P, Egüés N, Goyenechea E, de Munain AL, Martinez M (2014) Association between different obesity measures and the risk of stroke in the EPIC Spanish cohort. Eur J Nutr:1–11
Eom BW, Joo J, Yoon HM, Ryu KW, Kim YW, Lee JH (2014) A body shape index has a good correlation with postoperative complications in gastric cancer surgery. Ann Surg Oncol 21(4):1115–1122. doi:10.1245/s10434-013-3409-4
Afsar B, Elsurer R, Kirkpantur A (2013) Body shape index and mortality in hemodialysis patients. Nutrition 29(10):1214–1218
Cheung YB (2014) “A body shape index” in middle-age and older Indonesian population: scaling exponents and association with incident hypertension. PLoS ONE 9(1):e85421
Duncan MJ, Mota J, Vale S, Santos MP, Ribeiro JC (2013) Associations between body mass index, waist circumference and body shape index with resting blood pressure in Portuguese adolescents. Ann Hum Biol 40(2):163–167. doi:10.3109/03014460.2012.752861
Pencina MJ, D’Agostino RB, Vasan RS (2010) Statistical methods for assessment of added usefulness of new biomarkers. Clin Chem Lab Med 48(12):1703
Pencina MJ, D’Agostino RB Sr (2012) Thoroughly modern risk prediction? Sci Transl Med 4(131):131fs110. doi:10.1126/scitranslmed.3004127
Pencina MJ, D’Agostino RB Sr, Demler OV (2012) Novel metrics for evaluating improvement in discrimination: net reclassification and integrated discrimination improvement for normal variables and nested models. Stat Med 31(2):101–113. doi:10.1002/sim.4348
Pencina MJ, D’Agostino RB, Demler OV, Janssens AC, Greenland P (2012) Pencina et al. respond to “the incremental value of new markers” and “clinically relevant measures? A note of caution. Am J Epidemiol. doi:10.1093/aje/kws206
Pepe MS (2000) An interpretation for the ROC curve and inference using GLM procedures. Biometrics 56(2):352–359
Pepe MS (2011) Problems with risk reclassification methods for evaluating prediction models. Am J Epidemiol 173(11):1327
Pepe MS, Janes H, Longton G, Leisenring W, Newcomb P (2004) Limitations of the odds ratio in gauging the performance of a diagnostic, prognostic, or screening marker. Am J Epidemiol 159(9):882–890
Acknowledgments
This study was supported by grant No. 121 from the National Research Council of the Islamic Republic of Iran. We thank Michael J. Pencina, PhD, Department of Mathematics and Statistics, Boston University, Boston, MA, for statistical help and the constructive comments. We express our appreciation to the participants of district 13 of Tehran for their enthusiastic support in this study.
Conflict of interest
None to declare.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bozorgmanesh, M., Sardarinia, M., Hajsheikholeslami, F. et al. CVD-predictive performances of “a body shape index” versus simple anthropometric measures: Tehran lipid and glucose study. Eur J Nutr 55, 147–157 (2016). https://doi.org/10.1007/s00394-015-0833-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-015-0833-1