Abstract
Purpose
Recently, apprehension has been raised regarding “A1/A2 hypothesis” suggesting relationship between consumption of A1 “like” variants of cow β-casein and various physiological disorders. The information available is based on either the human epidemiological data of milk consumption or in vitro trials on cell lines with β-casomorphin peptides. The direct scientific evidence establishing the link between consumption of A1/A2 “like” milk and health is scanty. Thus, under present investigation, in vivo trials in mice were undertaken to study the effect of feeding three genetic variants (A1A1, A1A2 and A2A2) of cow β-casein milk on gastrointestinal immune system as it is the first and foremost site of immunological interactions.
Methods
Animals were divided into four groups for feeding with basal diet (control) and β-casein isolated from milk of genotyped (A1A1, A1A2 and A2A2) dairy animals, respectively. Gut immune response was analyzed by spectrophotometric assessment of MPO activity, quantitative sandwich ELISA of inflammatory cytokines (MCP-1 and IL-4), antibodies (total IgE, IgG, sIgA, IgG1 and IgG2a) and qRT-PCR of mRNA expression for toll-like receptors (TLR-2 and TLR-4). Histological enumeration of goblet cells, total leukocytes and IgA+ cells was also carried out.
Results
It was observed that consumption of A1 “like” variants (A1A1 and A1A2) significantly increased (p < 0.01) the levels of MPO, MCP-1, IL-4, total IgE, IgG, IgG1, IgG2a and leukocyte infiltration in intestine. TLR-2 and TLR-4 mRNA expression was also up-regulated (p < 0.01) on administration of A1 “like” variants. However, no changes in sIgA, IgA+ and goblet cell numbers were recorded on consumption of any of the β-casein variants.
Conclusion
It is reasonable to conclude that consumption of A1 “like” variants of β-casein induced inflammatory response in gut by activating Th2 pathway as compared to A2A2 variants. The present study thus supports the purported deleterious impacts of consumption of A1 “like” variants of β-casein and suggests possible aggravation of inflammatory response for etiology of various health disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
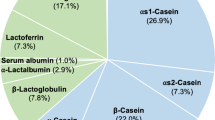
Casein is the major component of milk proteins that is composed of α, β and κ forms. Many reports show casein-derived bioactive peptides with antioxidant, antimicrobial, immunomodulatory, mineral binding, antithrombotic and antihypertensive properties [1]. Among these caseins, β-casein has 209 amino acids with at least 12 genetic variants that differ at different amino acid positions [2]. As a result of a point mutation on exon VII of bovine β-casein gene on 6th chromosome, a conversion from cytosine to adenine leads to replacement of proline (A2 allele, codon; CCT) by histidine (A1 allele, codon; CAT) at position 67 [3]. Based on this variation, milk can be divided into two groups, i.e., A1 and A2 “like” depending on the presence of proline or histidine on 67th position of β-casein protein. A1 “like” milk involves β-casein with A1, B, C, F or G alleles having a common amino acid at His67 (–Tyr60–Pro61–Phe62–Pro63–Gly64–Pro65–Ile66–His67–), but variations at other positions of amino acids. A2 “like” milk (–Tyr60–Pro61–Phe62–Pro63–Gly64–Pro65–Ile66–Pro67) consists of β-casein with A2, A3, D, H1, H2 and I alleles having a common amino acid residue at Pro67, but variations at other positions [4]. During the last decade, some epidemiological data have been generated that correlate consumption of A1 β-casein with various adverse biological responses such as type 1 diabetes mellitus, heart diseases and neurological disorders such as autism and schizophrenia and sudden infant death syndrome [5]. It is thought that an opioid peptide β-casomorphin-7 (BCM-7) released from the A1 “like” variants of β-casein may play a role in the development of these diseases and is therefore considered a hypothetical risk factor. But, on the other hand, controversial reports are available that link consumption of BCM-7 with physiological aspects that are beneficial to animals such as protective effects against diabetes and oxidative stress and modulation of intestinal mucus discharge and defense against noxious agents [6]. However, all the information available is based on either the epidemiological data taken from humans or in vitro trials on cell lines. There are few studies that reveal more release of BCM-7 on digestion from A1A1 homozygous than A1A2 heterozygous and A2A2 homozygous variants of β-casein [7]. In 2000, A2 Corporation Ltd. was established in New Zealand to market A2 milk as a premium brand in New Zealand, Australia, Asia and the USA. However, there is considerable uncertainty about the benefits of such an approach because of lack of an authentic validation and appropriate mechanism. Keeping in view the foregoing discussion, present study has been conducted on mice to evaluate the impact of feeding β-casein variants on gut that is the first target site of immune interactions after ingestion.
Materials and methods
Genotyping of animals and collection of milk samples
Previously, in our laboratory, we screened crossbred cattle (Karan Fries) carrying A1A1, A1A2 and A2A2 genotypes. The animals were maintained at Cattle Yard, National Dairy Research Institute, India. The DNA was isolated from the blood of animals by phenol–chloroform extraction method, and genotyping was performed with polymerase chain reaction–amplification created restriction site (PCR–ACRS) [8]. Accordingly, whole milk was procured from these genotyped dairy animals under present investigation.
Fractionation of β-casein
Separation of total casein was carried out by isoelectric precipitation method. The resultant precipitate was separated by filtration through four layers of cheese cloth and washed 3–4 times with distilled water, until the pH came to 7.0. Isoelectric casein was fractionated into α, β and κ caseins by differential solubility method in urea [9]. The sugars and salts were removed from this preparation by dialysis using 8 kDa cutoff cellulose membrane at 4 °C for 24 h. β-Casein in the extract was filtered, dried at room temperature and stored at −20 °C until used for feeding of mice.
SDS–PAGE of fractionated β-casein for purity analysis
The purity of β-casein fractionated from total cow casein as shown in Fig. 1 was checked with SDS–PAGE using 15 % resolving gel of polyacrylamide by the method of Laemmli [10] after loading equal concentration of (20 μg/well) fractionated β-casein in each well. The concentration of the proteins was estimated by the method of Lowry et al. [11].
Animals
Male Swiss albino mice (20–25 g) were maintained in the Small Animal House of the National Dairy Research Institute (NDRI), India. The animals were kept in plastic propylene cages and kept at room temperature in a sterilized condition. All procedures were approved by the Institutional Animal Ethics Committee.
Experimental design and sample collection
Animals were divided into four groups of six mice each. The negative control group was kept on basal diet (18.4 % starch, 65 % Bengal gram, 2.55 % oil, 2.05 % mineral mixture, 1 % vitamin mixture and 11 % cellulose). The experimental groups were fed with basal diet and β-casein variants (A1A1, A2A2 and A1A2) at a dose of 85 mg/animal/day suspended in 200 μl phosphate-buffered saline (PBS). This amount was calculated through dose-translation formula (human/mouse) using ratio of body weight (kg) to body surface area (m2) [12]. Negative control group mice were intubated orally with saline to avoid variations due to handling stress. No anesthesia was used during intubation procedure. All the variants of β-casein were isolated from milk of Karan Fries cattle and were orally intubated for 30 days. After 30 days of feeding, mice were killed after overnight fasting and their intestines were collected.
Collection of intestinal fluid
The tissue (ileum, 2 cm) was flushed with 2 ml of PBS followed by teasing with sterile needles in the same medium to separate the cells and then centrifuged at 2,000×g for 20 min at 4 °C. The resultant supernatant, i.e., intestinal fluid, was recovered and stored at −80 °C until the use of measurement of biochemical parameters.
Inflammatory molecules
Myeloperoxidase (MPO)
MPO activity was measured according to Bradley et al. [13] with some modifications. Briefly, the intestinal tissues were homogenized in nine volumes of ice-cold potassium phosphate buffer (50 mM, pH 6.0) containing 0.5 % cetyl trimethyl ammonium bromide (CTAB) followed by sonication (10 s) and freeze–thaw (3 times). The suspension was centrifuged at 35,000×g for 15 min, and the supernatant was analyzed for MPO activity by mixing assay buffer (50 mM potassium phosphate buffer, pH 6.0) containing 0.5 mM o-dianisidine dihydrochloride and 0.0005 % H2O2 as substrates. The breakdown of H2O2 is directly proportional to oxidation of o-dianisidine dihydrochloride that was measured at 460 nm (UV-visible double-beam spectrophotometer, UVD-3500, Labomed Inc., USA). The concentration of oxidized o-dianisidine dihydrochloride was calculated from its molar extinction coefficient (1.13 × 104/cmM). One unit of MPO activity was defined as amount of enzyme that produces one millimole of oxidized o-dianisidine dihydrochloride in the presence of H2O2/min at 25 °C and expressed as units/mg protein.
Monocyte chemotactic protein (MCP-1) and interleukin-4 (IL-4)
MCP-1 and IL-4 in the murine intestinal fluid were determined using quantitative sandwich ELISA kits (eBioscience, San Diego, CA, USA). The procedures were strictly adopted according to the manufacturer’s instructions. In brief, plates were coated with 100 μl of 1× capture antibody (goat anti-mouse MCP-1/goat anti-mouse IL-4). The samples were diluted 16 times for MCP-1, while undiluted samples were added in the experimental wells for detection of IL-4, respectively, followed by the addition of detection antibody and 100 μl of avidin-horseradish peroxidase (HRP). Plates were allowed to develop with the TMB substrate (3,3,5,5-tetramethyl diamine benzidine containing 0.03 % H2O2), and the reaction was finally stopped with 50 μl of 2 M H2SO4. Plates were read at 450 nm.
Humoral response
Total IgE, IgG and IgA
Total IgE, IgG and IgA in intestinal fluid were determined using quantitative sandwich ELISA kits (Koma Biotech, Seoul, Korea). To detect these antibodies, plates were coated with 1 μg/ml of goat anti-mouse IgE, IgG and IgA. The samples were diluted eight (IgE), 300 (IgG) and 1,000 (IgA) times before adding in experimental wells followed by the addition of 100 μl of HRP-conjugated goat anti-mouse IgE, IgG and IgA, respectively. Plates were allowed to develop with the TMB substrate, and reaction was finally stopped with 100 μl of 2 M H2SO4. Plates were read at 450 nm.
IgG subtypes (IgG1 and IgG2a)
IgG1 and IgG2a in intestinal fluid were determined using quantitative sandwich ELISA kits (eBioscience, San Diego, CA, USA). In brief, plates were coated with 100 μl of 1× capture antibodies (goat anti-mouse IgG1 and IgG2a). Samples were diluted 40 times (IgG1) and 16 times (IgG2a), respectively, before adding in the experimental wells followed by the addition of 50 μl HRP-conjugated antibodies (detection antibodies). After 3 h of incubation at room temperature, plates were allowed to develop with the TMB substrate and reaction was finally stopped with 50 μl of 2 M H2SO4. Plates were read at 450 nm.
Histological parameters
Goblet cells and total leukocytes
Two centimeters of tissues from murine small intestine (ileum) were used for histological slides for determination of goblet cells and total leukocytes by the method of Kiernan [14]. The 3-μm sections of the tissues were cut with Senior Rotary Microtome (Radical, RMT-30, Ambala, India). The slides were stained with hematoxylin and eosin stain. The numbers of goblet cells and total leukocytes were counted in seven fields (200×) and 10 fields (400×), respectively, on an inverted light microscope (Olympus, CKX41, Japan). The results were expressed as the number of goblet cells per five intestinal villi and number of total leukocytes per five fields of vision.
IgA+ cells
The unstained histological slides were prepared for direct immunofluorescence assay of IgA+ cells as described above. After deparaffinization using xylene and rehydration in a decreasing gradient of ethanol, sections were blocked in 2 % bovine serum albumin (BSA) for 1 h. The slides were washed 2–3 times with PBS, sections were incubated with a 1:100 dilution of α-chain mono-specific antibody conjugated with fluorescein isothiocyanate (FITC) (Cayman Chemical, Michigan, USA) for 1 h and observed with a fluorescent light microscope (Olympus, CKX41, Japan). The number of fluorescent cells was counted in 30 fields at 200× magnification. The results were expressed as the number of positive fluorescent cells per five fields of vision.
Expression of toll-like receptors (TLRs) by real-time RT-PCR
RNA isolation and cDNA preparation
The tissue from murine intestine was teased with needle in PBS and centrifuged at 2,000×g for 20 min at 4 °C. The sediment (cells) was washed three times with PBS before being used for RNA extraction.
Total RNA content was extracted by Tri Reagent (Sigma, St Louis, MO, USA) according to the manufacturer’s instructions. RNA concentration was quantified by NanoQuant (Tecan, Germany), and RNA integrity was checked on 1.4 % agarose. RNA concentrations were adjusted to 500 ng/μl for the synthesis of cDNA. Two micrograms of total RNA was reverse transcribed by initiation at 65 °C for 5 min followed by incubation at 42 °C for 1 h in a 25 μl mixture consisting 200 U RevertAid M-MuLV reverse transcriptase, 20 U RiboLock RNase inhibitor, 0.5 μg oligo (dT)18, 4 μl 5× reaction buffer and 0.8 mM dNTP mixture. The reaction was terminated at 70 °C for 5 min.
Amplification of TLR-2 and TLR-4 fragments
PCR was performed to amplify target gene TLR-2, TLR-4 and reference gene GAPDH of 199, 201 and 200 bp length fragments, respectively, on Real Time Thermocycler (Biorad CFX96™, C1000™) with Maxima SYBER Green/Fluorescein qPCR master mix (Thermo Scientific, Lithuania) using forward and reverse primers specific for GAPDH, 5′ TCAAGAAGGTGGTGAAGCAG3′ and 5′AAAGATGGAAGCTAAGACCC3′; TLR-2, 5′ AAGAGGAAGCCCAAGAAAGC3′ and 5′CGATGGAATCGATGATGTTG3′; and TLR-4, 5′ACCTGGCTGGTTTACACGTC3′ and 5′CTGCCAGAGACATTGCAGAA3′. One microliter of cDNA was used for PCR in a final volume of 20 μl, containing 10 μl 2× SYBER Green master mix, 0.2 μM of each forward and reverse primers and 8 μl nuclease free water. The PCR amplification was carried out using one cycle of initial denaturation at 94 °C for 5 min, 35 cycles of denaturation (94 °C for 30 s), annealing (53 °C for 30 s) and extension (72 °C for 45 s), and a final extension cycle at 72 °C for 4 min. After amplification, threshold (C t) values of both control and experimental groups with reference genes were taken for calculating fold change in target-gene expression.
Statistical analysis
Data were analyzed using the GraphPad Prism (version 5.01). Experimental results are mean ± SEM (standard error mean). Data were subjected to analysis of variance (ANOVA), and the Tukey test was used to separate the means (p < 0.05) that were considered statistically significant.
Results
Inflammatory molecules
Myeloperoxidase is released from stimulated polymorphonuclear neutrophils (PMNs) that produce the powerful oxidant hypochlorous acid that has microbicidal activity in addition to tissue damage such as acute or chronic inflammation. Therefore, it serves as a marker of inflammation. In the present study, it was found that feeding of A1A1 and A1A2 β-casein variants increased MPO activity in murine intestine (p < 0.01) by 204.20 and 43.54 %, respectively, compared to control group mice. This increase in activity was also found to be significant (p < 0.01) on feeding either of the β-casein variants (179.06 and 31.68 %) as compared to A2A2. Moreover, above results clearly depict much higher increase (111.92 %) in MPO activity on feeding A1A1 variant compared to A1A2 variant. However, no changes in MPO activity were observed in the mice group fed with A2A2 variant of β-casein compared to control group mice (Fig. 2A).
MCP-1 is a potent chemoattractant released from monocytes that regulates migration and infiltration of basophils, monocytes and macrophages in response to inflammation. The present study revealed an increase (p < 0.01) in the levels of MCP-1 in murine intestine after feeding of all the three variants of β-casein irrespective of their genetic variants. However, this increase was more pronounced after consumption of A1A1 (95.83 %) followed by A1A2 (79.16 %) and A2A2 (43.05 %) β-casein variants compared to control group mice. On comparing A1A1 to A2A2 response, the increase in MCP-1 level was higher (p < 0.01) by 36.89 % (Fig. 2B).
CD4 T cells secrete IL-4 that differentiates Th0–Th2 cells and induces class-switching recombination to IgG and IgE isotopes. The current study revealed an increase (p < 0.01) in IL-4 levels in murine intestinal fluid on consumption of A1A1 and A1A2 β-casein variants by 266.12 and 277.41 % compared to control group mice. Further, these results also indicated an increase (p < 0.01) in IL-4 levels on feeding A1A1 and A1A2 β-casein variants by 272.13 and 282.29 %, respectively, compared to A2A2 consumption. However, no changes were observed on feeding A2A2 β-casein variant compared to control group mice (Fig. 2C).
Humoral response
IgE production occurs in type I hypersensitivity that manifests various allergic diseases including food allergy, therefore, plays a critical role in allergic reactions. Current study revealed a considerable increase (p < 0.001) in total IgE levels in the intestinal fluid of mice fed with A1A1 and A1A2 β-casein variants by 50.67 and 46.75 %, respectively, compared to control group mice. Also, it was found that feeding A1A1 and A1A2 β-casein variants remarkably increased (p < 0.001) total IgE levels by 50.38 and 46.46 %, respectively, compared to A2A2 consumption. However, insignificant changes in IgE levels were observed in mice that consumed A2A2 β-casein variant compared to control (Fig. 3A).
Effect of feeding cow β-casein variants on humoral response of mice gut. A Total IgE, B total IgG, C IgG1, D IgG2a, E ratio of IgG1/IgG2a and F total IgA levels in intestinal fluid of mice. The values are expressed as mean ± SEM (n = 6 animals). Different letters indicate significant differences (p < 0.05)
IgG antibodies are found in all body fluids and considered the most important antibodies for fighting various infections, and this class of antibodies against food antigens are suggested to cause low-grade inflammation in gut mucosa. Present investigation depicted an increase (p < 0.05) in total IgG levels in the intestinal fluid of mice fed with A1A1 and A1A2 β-casein by 77.56 and 24.09 %, respectively, compared to control group mice. It was also found that IgG levels increased in the intestinal fluid on consumption of A1A1 and A1A2 β-casein by 91.08 % (p < 0.001) and 33.54 % (p < 0.01), respectively, compared to A2A2 consumption. Further, it was observed that feeding of A1A1 variant increased (p < 0.01) total IgG levels by 43.08 % compared to A1A2 consumption. However, insignificant changes were observed after A2A2 consumption compared to control (Fig. 3B).
Further analysis of IgG subtypes (IgG1 and IgG2a) has also shown similar results to total IgG. Consumption of A1A1 and A1A2 β-casein variants increased (p < 0.01) IgG1 levels (145.65 and 82.60 %) and IgG2a levels (81.07 and 66.23 %), respectively, as compared to control. This increase in the two subtypes of IgG were also found statistically significant (p < 0.01) (IgG1 98.24 and 47.36 %) and (IgG2a 68.96 and 55.11 %) in A1A1 and A1A2-fed groups, respectively, as compared to A2A2 (Fig. 3C, D). Thus, the ratio of IgG1/IgG2a also increased significantly (p < 0.05) in A1A1 group as compared to control group. However, no such changes were observed in A1A2 and A2A2 groups with respect to control (Fig. 3E).
On the other hand, IgA is the most abundant antibody produced in gut mucosal system. It has a pivotal role in gut mucosal immunity against ingested pathogens and causes an inhibitory effect on inflammatory reactions due to other immunoglobulins. Results of this study showed no changes (p > 0.05) in IgA levels in the intestinal fluid of mice fed with A1A1, A1A2 and A2A2 β-casein variants (Fig. 3F).
Histological parameters
The gastrointestinal tract (GIT) is shielded with mucus gel formed predominantly of mucins that are secreted by goblet cells. Alterations in goblet cell functions and mucin release are related to various GIT dysfunctions with change in normal microbiota as well as food allergy. Under present investigation, it was observed that feeding of all the three variants of β-casein (A1A1, A2A2 and A1A2) did not alter (p > 0.05) the number of goblet cells in the murine intestine (Fig. 4A, B). On the other hand, consumption of A1A1and A1A2 β-casein variants remarkably increased (p < 0.001) the number of total leukocytes by 178.51 and 159.50 %, respectively, compared to control. Also a considerable increase (p < 0.001) was observed on feeding A1A1 and A1A2 β-casein variants by 153 and 135.73 %, respectively, compared to A2A2 consumption. However, no change was depicted on A2A2 consumption compared to control (Fig. 4C, D).
Histology of mice intestine after feeding β-casein variants. A Optical microscopy (200×) of intestinal villi from a control, b A2A2, c A1A2 and d A1A1; B no. of goblet cells in intestinal villi; C optical microscopy (400×) of intestinal villi depicting total leukocytes; D number of total leukocytes in intestine; E florescent microscopy (200×) of intestinal villi with FITC-labeled rabbit anti-mouse IgA for IgA+ cells; F number of IgA+ cells in intestine. The values are expressed as mean ± SEM (n = 6 animals). Different letters indicate significant differences (p < 0.05)
In mice gut, IgA+ plasma cells have repertoire protective functions, largely being the secretion of IgA antibodies as well as synthesis of antimicrobial mediators. Localization of IgA+ in murine intestinal tissue was done with direct immunofluorescence assay as depicted in Fig. 4E. In this work, we could not observe any change (p > 0.05) in the number of IgA+ cells in murine intestine after feeding all the three variants β-casein (A1A1, A2A2 and A1A2) as shown in Fig. 4F.
Toll-like receptor (TLR) mRNA expression
The functional response of TLR-4 and TLR-2 in murine intestine on consumption of different β-casein variants is shown in Fig. 5A, B, respectively. Results indicated that consumption of A1A1 and A1A2 β-casein remarkably increased (p < 0.001) the TLR-4 expression by 414 and 408 %, respectively, compared to control. Also a considerable increase (p < 0.001) in TLR-4 expression was observed on feeding A1A1 and A1A2 variants by 176.34 and 173.11 %, respectively, compared to A2A2 consumption. Similarly, A1A1 β-casein consumption remarkably increased (p < 0.001) TLR-2 expression by 141.39, 220.71 and 349 % compared to A1A2, A2A2 and control group mice, respectively. However, no change was observed on consumption of A2A2 and A1A2 β-casein compared with control group mice.
Discussion
Bovine milk and other dairy products have long been main ingredients of the human diet to fulfill nutritional as well as physiological roles. It is the first food for newborn mammals, and caseins, and the major proteins in milk have been considered principal agents that regulate human health positively. Despite its health benefits, the consumption of cow’s milk has been under scrutiny for its reported links to the risk of chronic diseases. These negative correlations do not always prove causality and require further investigation. Initially, these risks were labeled with pasteurization and homogenization that subsequently were tagged to bovine growth hormone and antibiotics in commercial dairy products. However, more recently, the major milk proteins, i.e., caseins have been associated with chronic diseases [15]. Initially, cow milk proteins were thought to be diabetogenic agents [16], but later, a possible link was speculated between type 1 diabetes and release of a hexapeptide from β-casein rather than the whole protein [17]. On the one hand, Wong et al. [18] reported inhibitory effects of bovine β-casein on ovine neutrophil chemotaxis associated with increased superoxide production in culture, but there was no consideration of genetic variants responsible for release of opioids during digestion. On the other, whole casein has been regarded as a chemoattractant for human neutrophils and monocytes [19]. In the present investigation, an increase (p < 0.01) in MPO activity and MCP-1 levels in intestinal cells/fluid along with leukocyte infiltration in villi on feeding A1 “like” β-casein variants was observed. These elevations in inflammatory molecules may be attributed to the release of BCMs from A1 “like” β-casein variants, as both A1A1 and A1A2 are potent releasers of BCMs [20]. It has been reported that incubation of peripheral blood mononuclear cells (PBMCs) with bovine BCM-7 in nano- and pico-molar concentrations resulted in secretion of interleukin-8 [21]. IL-8 is a strong chemoattractant for neutrophils that stimulates the activation of G-proteins and several downstream serine or threonine kinases, responsible for chemotaxis, degranulation and production of superoxide anions during phagocytosis [22]. These previous observations clearly support our present results. To the best of our knowledge, there have been only two in vivo studies to explore association between consumption of A1/A2 β-casein variants and their physiological effects. All other findings are a result of either powdered acid caseins (irrespective of their genetic variants) or in vitro trials with chemically synthesized BCMs. The first animal (rabbit) trial to consider genetic variants of β-casein provided strong evidence that in the absence of dietary cholesterol, A1 β-casein consumption produced significantly higher serum cholesterol, LDL, HDL, triglyceride, percent surface area of aorta covered by fatty streaks and the thickness of the fatty streak lesions in the aortic arch than those fed with A2 variant of β-casein [23]. A positive correlation was thus observed between consumption of A1/A2 β-casein and progression of arterial lesions suggesting clinically important implications of A1 β-casein consumption on cardiovascular disorders. However, Kaminski et al. [24] reported that supplementation of concentrate feed with A1 and A2 milk to sibling gilts resulted in non-significant changes in the morphology of blood cells, lipid profile (triglyceride, LDL and HDL), liver enzymes (alanine transaminase and aspartate aminotransferase), creatinine and urea due to increased activity of dipeptidyl peptidase IV. Hence, the in vivo effects of A1/A2 “like” variants of β-casein remain controversial and warrant further validation. Earlier, it has been established that bovine BCM-7 at higher concentrations (above femtomolar) reduces interferon-γ (IFN-γ) secretion but induces IL-4 expression from PBMCs [21]. The increase (p < 0.01) in IL-4 levels on feeding A1 “like” variants of β-casein in the current study also confirms previous findings and suggests a mechanism that may lead to differentiation of naive helper T cells to Th2 cells for induction of humoral immune response toward increased production of immunoglobulins with class-switching activity [25]. Indeed, a significant increase (p < 0.01) in IgE, IgG, IgG1 and IgG2a levels were observed in intestinal fluid on feeding A1 “like” β-casein variants associated with release of BCMs compared to A2 “like” variants. The increased ratio of IgG1/IgG2a as revealed in present study further strengthens the Th2-biased immune response on consumption of A1A1 β-casein and validates the elevated levels of IgE, as the latter is also involved in induction of Th2 immune response-mediated food allergic reactions [26]. However, we could not detect any significant changes in intestinal sIgA levels that were further corroborated by lack of variation in IgA+ cells in the intestine. This could be attributed to the fact that the majority of class switching taking place toward IgG, IgG1, IgG2a and IgE that are directly associated with non-desirous inflammatory responses. Together, these findings demonstrate an enhanced Th2 response mediated by increased levels of IL-4 and immunoglobulin production. Activation of the Th2 pathway on feeding β-casein variants may also be related to the observations of Rungkat-Zakaria et al. [27] who found that feeding of total casein (100 mg/day) to mice increased histamine release from peritoneal mastocytes as a result of casein-derived peptides. Histamine is a pharmacologically active inflammatory molecule that favors Th2 cytokines to produce antibodies [28]. Kurek et al. [29] also observed a concentration-dependent histamine release from peripheral blood leukocytes with BCM-7 that was later confirmed by wheal and flare reactions in the skin of healthy children [30]. Also, in our laboratory, it was established that incubation of BCM-5 with bone marrow-derived mast cells caused histamine release [31]. All these studies point toward histamine-mediated Th2 skewness as a result of BCM-7 released from A1 “like” variants of β-casein. In various inflammatory diseases such as atherosclerosis, diabetes and cancer, MCP-1 has a vital role to play as a chemokine secreted from monocytes, T cells and endothelial cells that causes initiation of inflammation through recruitment of monocytes [32–34]. Epidemiologically, these diseases have also been correlated with the consumption of A1 “like” variants of β-casein that further verify our data. As already reported, MCP-1 is induced in a variety of cell types in vitro by cytokines, TNF-α, IL-1and IL-4 [35–38]. The increase in IL-4 and MCP-1 levels in the present study points toward the Th2 pathway-mediated gut inflammation on consumption of A1 “like” variants of β-casein than A2A2 variants. The GIT contains goblet cells that produce secretory and membrane-bound mucins with different physiological or pathological implications [39]. In most intestinal infections, the acute phase of inflammation results in induction of goblet cells, whereas the chronic phase causes depletion of goblet cells [40]. However, the present investigation showed that none of the three variants of β-casein resulted in major changes in goblet cell numbers. Studies demonstrating secretion of rMuc2 and rMuc3 in rat DHE, MUC5AC in human HT29-MTX cell lines and mucus discharge from isolated perfused rat jejunum with BCM-7 do exist [41, 42]. However, there are no reports establishing a correlation between goblet cell numbers, different genetic variants of β-casein and chemically synthesized BCMs. Therefore, initiation of the inflammatory response has been proposed with A1 “like” variants of β-casein through mucus discharge but independently of goblet cell number. On the other hand, weak mRNA expression of TLR-2 and TLR-4 was reported in healthy intestinal epithelial cells (IECs) and lamina propria mononuclear cells (LPMNCs) in vivo but in inflammatory responses, these receptors are unregulated [43]. Both in vivo and in vitro studies have demonstrated that histamine is released from peritoneal mastocytes, mast cells and peripheral blood leukocytes after incubation with BCM-7, BCM-5 and total casein [27–30]. Previous studies established that in vitro culture of human gingival fibroblasts (HGFs) and human umbilical vein endothelial cells (HUVEC) with 100 and 10 μM histamine, respectively, resulted in the increase of TLR-2 and TLR-4 expression and further stimulation of HGFs with lipoteichoic acid or lipopolysaccharide showed an increased expression of cyclo-oxygenase-2 and prostaglandin E2 [44, 45]. Moreover, morphine (an agonist of BCM) has been reported to have a role in glial cell (major immune inflammatory cells of central nervous system) activation and inflammation through TLR-2 and TLR-4 [46, 47]. The above observations further support the present findings where consumption of A1 “like” variants increased (p < 0.01) the expression of TLR-2 and TLR-4.
In conclusion, data presented in this paper clearly establish that feeding of A1 “like” variants (A1A1 and A1A2) of β-casein as compared to A2A2 induce inflammatory immune responses in the murine gut, most likely through Th2 pathway. This was confirmed by up-regulation of inflammation-associated molecules (MPO, MCP-1 and IL-4), humoral immune response (IgE, IgG, IgG1, IgG2a and IgG1/IgG2a), infiltration of leukocytes in intestinal villi and expression of toll-like receptors (TLR-2 and TLR-4). However, further studies are required to delineate the molecular mechanisms involved in interactions between intestinal opioid receptors and β-casein peptides that generate signaling cascade of inflammatory responses. If the cellular data of the future support a role of A1 “like” milk in inducing inflammatory disorders, then it will be imperative to minimize its risk globally by reducing its production through sound-breeding policies.
References
FitzGerald RJ, Meisel H (2000) Milk protein-derived peptide inhibitors of angiotensin-I-converting enzyme. Br J Nutr 84(S1):S33–S37
Farrell HM Jr, Jimenez-Flores R, Bleck GT, Brown EM, Butler JE, Creamer LK, Hicks CL, Hollar CM, Ng-Kwai-Hang KF, Swaisgood HE (2004) Nomenclature of the proteins of cow’s milk—sixth revision. J Dairy Sci 87(6):1641–1674
Groves ML (1969) Some minor components of casein and other phosphoproteins in milk. A review. J Dairy Sci 52(8):1155–1165
Roginski H (2003) Encyclopedia of dairy sciences. Academic Press, London
Woodford K, Cowan T (2009) Devil in the milk: illness, health and the politics of A1 and A2 milk. Chelsea Green Press, USA
Raies MH, Kapila R, Shandilya UK, Kapila S (2012) Impact of milk derived β-casomorphins on physiological functions and trends in research. A review. Int J Food Prop (in press)
Jinsmaa Y, Yoshikawa M (1999) Enzymatic release of neocasomorphin and β-casomorphin from bovine β-casein. Peptides 20(8):957–962
Raies MH, Kapila R, Shandilya UK, Dang AK, Kapila S (2012) Detection of A1 and A2 genetic variants of β-casein in Indian crossbred cattle by PCR-ACRS. Milchwissenschaft 67(4):396–398
Fox PF, Guiney J (1972) A procedure for the partial fractionation of αS-casein complex. J Dairy Sci 39(1):49–53
Laemmli UK (1970) Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature 227(5259):680–685
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ (1951) Protein measurement with the Folin phenol reagent. J Biol Chem 193(1):265–275
Reagan-Shaw S, Nihal M, Ahmad N (2007) Dose translation from animal to human studies revisited. FASEB J 22(3):659–661
Bradley PP, Priebat DA, Christensen RD, Rothstein G (1982) Measurement of cutaneous inflammation: estimation of neutrophil content with an enzyme marker. J Invest Dermatol 78(3):206–209
Kiernan JA (2008) Histological and histochemical methods theory and practice, 4th edn. Scion, Bloxham
Bell SJ, Grochoski GT, Clarke AJ (2006) Health implications of milk containing β-casein with A2 genetic variant. Crit Rev Food Sci Nutr 46(1):93–100
Elliot RB, Martin JM (1984) Dietary protein: a trigger of insulin-dependent diabetes in the BB rat? Diabetologia 26(4):297–299
Elliott RB, Wasmuth H, Hill J (1997) Immunosuppressing effects of cow milk β-casomorphins in prediabetic mice and humans. In: 16th IDF congress, Helsinki
Wong CW, Seow HF, Liu AH, Husband AJ, Smithers GW, Watson DL (1996) Modulation of immune responses by bovine β-casein. Immunol Cell Biol 74(4):323–329
Lewis SL, Van Epps DE (1983) Demonstration of specific receptors for fluoresceinated casein on human neutrophils and monocytes using flow cytometry. Inflammation 7(4):363–375
De Noni I (2008) Release of β-casomorphins-5 and -7 during simulated gastro-intestinal digestion of bovine β-casein variants and milk-based infant formulas. Food Chem 110(4):897–903
Fiedorowicz E, Jarmołowska B, Iwan M, Kostyra E, Obuchowicz R, Obuchowicz M (2011) The influence of μ-opioid receptor agonist and antagonist peptides on peripheral blood mononuclear cells (PBMCs). Peptides 32(4):707–712
Waugh DJ, Wilson C (2008) The interleukin-8 pathway in cancer. Clin Cancer Res 14(21):6735–6741
Tailford KA, Berry CL, Thomas AC, Campbell JH (2003) A casein variant in cow’s milk is atherogenic. Atherosclerosis 170(1):13–19
St Kaminski, Kostyra E, Cieslinska A, Fiedorowicz E (2012) Consumption of bovine β-casein variants (A1 or A2) does not affect basic hematological and biochemical indices. Milchwissenschaft 67(3):238–241
Kashiwada M, Levy DM, McKeag L, Murray K, Schröder AJ, Canfield SM, Traver G, Rothman PB (2010) IL-4-induced transcription factor NFIL3/E4BP4 controls IgE class switching. Proc Natl Acad Sci USA 107(2):821–826
Dupont C, Heyman M (2000) Food protein-induced enterocolitis syndrome: laboratory perspectives. J Pediatr Gastroenterol Nutr 30S:S50–S57
Rungkat-Zakaria F, Belleville F, Nabet F, Linden G (1992) Allergenicity of bovine casein. I: specific lymphocyte proliferation and histamine accumulation in the mastocyte as a result of casein feeding in mice. Food Agric Immunol 4(1):41–50
Schneider E, Rolli-Derkinderen M, Arock M, Dy M (2002) Trends in histamine research: new functions during immune responses and hematopoiesis. Trends Immunol 23(5):255–263
Kurek M, Przybilla B, Hermann K, Ring J (1992) A naturally occurring opioid peptide from cow’s milk, β-casomorphine-7, is a direct histamine releaser in man. Int Arch Allergy Immunol 97(2):115–120
Kurek M, Czerwionka-Szaflarska M, Doroszewska G (1995) Pseudoallergic skin reactions to opiate sequences of bovine casein in healthy children. Rocz Akad Med Bialymst 40(3):480–485
Reddi S, Kapila R, Dang AK, Kapila S (2011) Evaluation of allergenic response of milk bioactive peptides using mouse mast cell. Milchwessienschaft 67(2):117–121
Conti P, DiGioacchino M (2001) MCP-1 and RANTES are mediators of acute and chronic inflammation. Allergy Asthma Proc 22(3):133–137
O’Hayre M, Salanga CL, Handel TM, Allens SJ (2008) Chemokines and cancer: migration, intracellular signaling and intercellular communication in the microenvironment. Biochem J 409(3):635–649
Yadav A, Saini V, Arora S (2010) MCP-1: chemoattractant with a role beyond immunity: a review. Clin Chim Acta 411(21–22):1570–1579
Proost P, Wuyts A, Van Damme J (1996) Human monocyte chemotactic proteins-2 and -3: structural and functional comparison with MCP-1. J Leukoc Biol 59:67–74
Rollins BJ, Pobert JS (1991) Interleukin-4 induces the synthesis and secretion of MCP-1/JE by human endothelial cells. Am J Pathol 138(6):1315–1319
Thornhill MH, Kyan-Aung U, Haskard DO (1990) IL-4 increases human endothelial cell adhesiveness for T cells but not for neutrophils. J Immunol 144(8):3060–3065
Rollins BJ, Sunday ME (1991) Suppression of tumor formation in vivo by expression of the JE gene in malignant cells. Mol Cell Biol 11(6):3125–3131
Corfield AP, Carroll D, Myerscough N, Probert CS (2001) Mucins in the gastrointestinal tract in health and disease. Front Biosci 6:D1321–D1357
Dharmani P, Srivastava V, Kissoon-Singh V, Chadee K (2009) Role of intestinal mucins in innate host defense mechanisms against pathogens. J Innate Immun 1(2):123–135
Zoghbi S, Trompette A, Claustre J, El Homsi M, Garzon J, Jourdan G, Scoazec JY, Plaisancie P (2006) β-Casomorphin-7 regulates the secretion and expression of gastrointestinal mucins through a μ-opioid pathway. Am J Physiol Gastrointest Liver Physiol 290(6):G1105–G1113
Trompette A, Claustre J, Caillon F, Jourdan G, Chayvialle JA, Plaisancie P (2003) Milk bioactive peptides and β-casomorphins induce mucus release in rat jejunum. J Nutr 133(11):3499–3503
Hausmann M, Kiessling S, Mestermann S, Webb G, Spöttl T, Andus T, Schölmerich J, Herfarth H, Ray K, Falk W, Rogler G (2002) Toll-like receptors-2 and -4 are up-regulated during intestinal inflammation. Gastroenterology 122(7):1987–2000
Gutiérrez-Venegas G, Cruz-Arrieta S, Villeda-Navarro M, Méndez-Mejía JA (2011) Histamine promotes the expression of receptors TLR-2 and TLR-4 and amplifies sensitivity to lipopolysaccharide and lipoteichoic acid treatment in human gingival fibroblasts. Cell Biol Int 35(10):1009–1017
Talreja J, Kabir MH, Filla MB, Stechschulte DJ, Dileepan KN (2004) Histamine induces toll-like receptor-2 and -4 expression in endothelial cells and enhances sensitivity to gram-positive and gram-negative bacterial cell wall components. Immunology 113(2):224–233
Hutchinson MR, Zhang Y, Shridhar M, Evans JH, Buchanan MM, Zhao TX, Slivka PF, Coats BD, Rezvani N, Wieseler J, Hughes TS, Landgraf KE, Chan S, Fong S, Phipps S, Falke JJ, Leinwand LA, Maier SF, Yin H, Rice KC, Watkins LR (2010) Evidence that opioids may have toll-like receptor 4 and MD-2 effects. Brain Behav Immun 24(1):83–95
Zhang L, Li L, Zhang G (2011) A Crassostrea gigas toll-like receptor and comparative analysis of TLR pathway in invertebrates. Fish Shellfish Immunol 30(3):653–660
Acknowledgments
The authors are grateful to the Director of National Dairy Research Institute (ICAR), Karnal, for providing funding and laboratory facilities to carry out this piece of work.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Haq, M.R.U., Kapila, R., Sharma, R. et al. Comparative evaluation of cow β-casein variants (A1/A2) consumption on Th2-mediated inflammatory response in mouse gut. Eur J Nutr 53, 1039–1049 (2014). https://doi.org/10.1007/s00394-013-0606-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-013-0606-7