Abstract
Purpose
Experimental evidence indicates a strong connection between oxidative damage, cancer, and aging. Epidemiological observations suggest that a diet rich in fruits and vegetables is associated with lower incidence of some cancers and longer life expectancy; since fruits and vegetables contain natural antioxidants, a considerable effort has been dedicated to understanding their effects in experimental studies and in human trials.
Results
A: Effects of antioxidant-containing food and supplements on oxidation damage in humans. Intervention trials employing a variety of biomarkers have shown either a slight decrease in oxidation damage or no effect. B: Effects of selected antioxidants on mortality and cancer incidence. β-carotene and α-tocopherol, alone or in combination, increase cardiovascular and all-cause mortality or have no effect. In some studies, β-carotene and retinyl palmitate significantly increase the progression of lung cancer and aggressive prostate cancer. Protection against cardiovascular mortality or no effect of vitamin E has been reported, with an increase of all-cause mortality at dosages greater than 150 IU/day. Selenium showed beneficial effects on gastrointestinal cancer and reduced the risk of lung cancer in populations with lower selenium status. For multivitamin and mineral supplementation, no significant reduction of mortality or cancer incidence was observed, but some reports indicate a possible preventive effect in cervical cancer.
Conclusions
The majority of supplementation studies indicate no variation of general mortality and of cancer incidence or a detrimental effect on both. Antioxidant supplements so far tested seem to offer no improvement over a well-balanced diet, possibly because of the choice of the substances tested or of an excessive dosage. However, new natural or synthetic compounds effective in vitro and in experimental studies might still be worth investigating in human trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The idea that aging could be the result of accumulated cell damage caused by free radicals originated with Harman more than 50 years ago [1] and has been a popular topic of investigation thereafter. Research in the 80s in the laboratory of Bruce Ames and others produced evidence indicating that oxidation damage and aging were strongly connected. A seminal paper, among many of that period, clearly showed that mice, rats, monkeys, and humans have typical metabolic rates that correspond to the level of oxidation damage in their DNA and proteins and correlate robustly and inversely with life span [2]. These observations stimulated a large effort on the basic mechanisms of the aging process, fueled by the hope of discovering natural compounds or drugs able to decrease oxidation damage in cells and organisms, thereby increasing life span. The possible applications to public health of any discovery in this field seemed staggering.
Oxidative damage to DNA may also be implicated in carcinogenesis, since it causes mutations, and—if these occur in appropriate genes—cell transformation. On the basis of animal and cell experiments and epidemiological results, Peto, Doll, and others [3] first suggested β-carotene to be possibly anti-carcinogenic in humans and suggested supplementation trials with β-carotene. Consequently, many studies were carried out in different countries using carotenoids and various other antioxidants, including long-term clinical trials on all-cause and cancer mortality or with chronic disease incidence as outcome, and in addition, supplementation trials using various biomarkers of oxidation damage.
Evidence from observational epidemiology
Antioxidants and aging
Fruits and vegetables are a fundamental component of a healthy diet. Epidemiological studies have examined whether vegetarians have a longer life span than carnivores. A review of the existing studies on this topic in Europe and North America [4] concluded that most evidences (except for one instance, discussed in Fortes et al. [5]) show that long-term vegetarians have a significant increase in life expectancy over carnivores (average variation: 3.6-years, 95 % confidence limits (CL): 1.4–5.8). Antioxidants might be causally related to this effect, though the connection is clouded by many confounding factors.
Observational studies of body antioxidant levels in relation to mortality, cancer, and heart disease
Epidemiological evidence links a higher consumption of fruits and vegetables with a lower risk of cancer. This connection is fully discussed for all major cancer types in the WCRF publications [6, 7] and will not be reviewed again here. According to general scientific wisdom, the protective effect of fruits and vegetables is explained by the presence of antioxidants. Therefore, human population studies in which plasma antioxidant levels were measured are of particular interest, since it is possible to verify whether subjects in the lowest percentiles of concentration of some antioxidants (like vitamin A, C, E and β-carotene) have an increased risk of cancer and/or an altered incidence of cardiovascular accidents. However, most evidence comes from case–control studies, and this type of epidemiological study is prone to artifacts, since a variation of a marker related to dietary intake (e.g., a low plasma level of a specific antioxidant) could be an effect rather than a cause of a specific disease. Prospective studies are more reliable, in which disease incidence can be related to biomarkers measured years previously.
It is not the purpose of this commentary to review the whole, extensive body of literature on this topic. In this section, we will comment only on studies of relatively large population groups (>500), with a long follow-up time (>5 years) and a robust experimental structure; for a more detailed analysis, we refer to the many recently published reviews and meta-analyses on each substance.
One of the first publications on the relation between antioxidant vitamin levels and human health was a 12-year mortality follow-up of 2,974 participants (the “Basel Study”, published in 1991), which showed a significant elevation of the relative risk (RR) for lung and bronchial cancer of subjects with low β-carotene plasma levels (<0.23 μmol/L); low plasma levels of β-carotene and vitamin A were associated with an increased risk of all types of cancer (RR: 2.47, p < 0.01); the risk of cerebrovascular death was also elevated with low plasma β-carotene and vitamin C (RR: 4.17, p < 0.01) [8].
In a study of 65 rural counties of China, published in 1992, it was also shown that plasma levels of some dietary antioxidants were correlated with cancer mortality. In particular, plasma levels of ascorbic acid were inversely correlated with the frequency of common cancers and low levels of selenium specifically with higher incidence of esophageal and stomach cancer. Higher levels of β-carotene (independently from retinol) had a protective effect, in particular for stomach cancer [9].
Greenberg et al. [10] followed a total of 1,188 men and 532 women for 8.2 years in the USA and reported a lower risk of death from all-causes (RR: 0.52; CL: 0.44–0.87) and from cardiovascular diseases (RR: 0.57; CL: 0.34–0.95) in subjects in the highest quartile of β-carotene who had been enrolled for the prevention of non-melanoma skin cancer.
It was later (1999) shown in an ecological study of 634 men (aged 40–49), sampled randomly from five regions in Japan, that plasma levels of β-carotene and α-tocopherol were inversely correlated with gastric cancer (r = −0.31 and −0.89, respectively) [11].
In 2006, partial results were published on a study involving 29,092 Finnish men (α-Tocopherol, β-Carotene Cancer Prevention (ATBC) Study [12]), showing that subjects in the highest quintiles of serum vitamin E had significantly lower risk of total, cause-specific and all-cause mortality, independently of supplementation (RR: 0.82; CL: 0.78–0.86).
Increased serum levels of vitamin C were also negatively correlated with gastric cancer among non-drinkers and non-smokers in a study of 18,244 older men in Shanghai, China [13].
Among prostate cancer cases in the ATBC Study in Finland, subjects in the highest quintile of α-tocopherol at baseline had improved survival (RR: 0.51; CL: 0.20–0.90) [14]. In the SENECA study [15], after a follow-up of 10 years of 1,168 European elderly men and women, plasma carotene concentrations were associated with a low risk of mortality from cancer (RR: 0.59; CL: 0.44–0.79) or cardiovascular disease with a body mass index <25 (RR: 0.67; CL: 0.49–0.94).
Within the Physicians’ Health Study (PHS) in the USA, a nested case–control study involving 1,286 cases and 1,267 controls showed an inverse relationship between high levels of selenium and prostate cancer mortality among subjects without a high-risk genotype (polymorphism of the selenoprotein SEP15 [16]).
A recent population-based study of 1,043 older adults living in Chianti, Italy, established that adults in the lowest quartile of plasma selenium at enrollment had a higher all-cause mortality compared with the highest quartile (RR: 1.60; CL: 1.04–2.47); adults in the highest tertile of plasma carotenoids at enrollment also had lower mortality compared with the lowest tertile (RR: 0.81; CL: 0.65–0.99) [17].
Recently, using data of the Third National Health and Nutrition Examination Survey in the USA, it was shown that among 13,393 participants, those belonging to the lowest plasma carotenoid quartile (<1.01 μmol/L) had significantly higher all-cause mortality (RR: 1.38, CL: 1.15–1.65) compared with the ones in the highest quartile (>1.75 μmol/L) [18].
In conclusion many studies, published over about two decades, conducted in different countries and on various populations, involving relatively large numbers of healthy or disease-carrying individuals, with a follow-up time sufficient to show delayed events, consistently indicated that higher body levels of antioxidant vitamins have a beneficial effect on health and, inversely, that low systemic levels are associated with a higher risk of several chronic diseases and/or mortality. However, it is not clear whether higher levels of antioxidant vitamins are important per se or are simply a marker of a well-balanced nutrition and of a healthy life-style. High levels of plasma β-carotene, vitamin C and E are in fact an indicator of the consumption of a diet rich in fruits and vegetables; accordingly, a Norwegian study indicated that plasma concentrations of α-carotene, β-carotene and lutein could be used accurately to assess fruits and vegetable intake [19]. However, it is also possible that healthier diets might contain additional active compounds which might have been disregarded in the studies published so far.
Observational studies based on biomarkers
Do higher levels of antioxidant intake correlate with lower levels of biomarkers of oxidative stress including oxidative damage to DNA? One possible answer to this question derives from the comparison of population groups with different intakes of fruits and vegetables.
Kazimirova et al. [20] compared groups of vegetarians and non-vegetarians, known from previous work to differ in plasma levels of antioxidants. Vegetarians (n = 24), with higher mean levels of vitamin C, β-carotene, and vitamin A compared with non-vegetarians (n = 24), had significantly (p = 0.005) lower levels of combined strand breaks (SBs) and oxidized purines (principally 7,8-dihydro-8-oxoguanine [8-oxoGua], measured with the comet assay plus formamidopyrimidine DNA glycosylase, FPG). The sub-group of lactovegetarians (n = 11) had markedly lower levels of oxidized pyrimidines (detected with endonuclease III) (p = 0.0017). There were no differences in frequencies of micronuclei or chromosome aberrations. Dhawan et al. [21] reported significantly (p < 0.001) lower levels of DNA SBs in vegetarians (n = 26) compared with non-vegetarians (n = 36). Similar groups were studied by Fenech and Rinaldi [22]; while vegetarians had higher plasma levels of vitamin C and folic acid, they were relatively low in vitamin B12 and had similar levels of vitamin E to non-vegetarians. There were no remarkable differences in micronucleus frequency between the two groups.
DNA strand breaks, oxidized purines or pyrimidines, conjugated dienes of fatty acids and carbonylated proteins were measured in young women aged 20–30 (46 vegetarians, 48 non-vegetarians) versus older women aged 60–70 (33 vegetarians, 34 non-vegetarians) [23]. In younger subjects, no differences in oxidative damage parameters or plasma β-carotene or vitamin C were observed between vegetarian and non-vegetarians. However, in older vegetarians significantly decreased DNA oxidation and lipid peroxidation were reported, with higher values of plasma vitamin C and β-carotene relative to the non-vegetarians (p < 0.05). Significant age-dependent increases in oxidative stress parameters were noted only in non-vegetarian (p < 0.05) [23]. A recent study of 100 healthy Indian subjects documented that serum malonialdehyde (MDA) levels were significantly increased (p < 0.001) in non-vegetarians compared with lacto-vegetarians and lacto-ovo-vegetarians; in this study, non-vegetarians had significantly lower levels of plasma glutathione peroxidase and vitamins A and E compared with lacto-vegetarians and lacto-ovo-vegetarians (p < 0.001) [24].
Another approach is to look for correlations between plasma micronutrients and markers of oxidative damage across a normal healthy population. Lymphocyte DNA damage, in the form of oxidized pyrimidines, was measured with the comet assay in a group of healthy subjects and found to show a significant negative correlation with the concentration of total carotenoids (p < 0.05) [25]. Notably, there were no subjects with a high concentration of carotenoids and a high level of DNA base oxidation. It should, however, be noted that the plasma carotenoid concentration is a biomarker of consumption of fruits and vegetables, and so it could be some other component of the foods that is responsible for protecting the DNA. Giovannelli et al. [26] did not find any significant correlation between oxidized purines, measured with the comet assay, and plasma antioxidants (6 carotenoids, retinol, and α- and γ-tocopherol) in a healthy population. Another observational study using the comet assay was carried out by Dusinska et al. [27]: significant negative correlations were found between plasma lycopene and SBs plus oxidized pyrimidines (r = −0.191, p = 0.051) and SBs plus endonuclease III-sensitive sites (r = −0.23 p = 0.016) and between vitamin C and SBs plus oxidized purines (r = −0.23 p = 0.016). Trace elements were also measured; selenium and zinc both have roles in enzymic antioxidant defences, but while selenium showed a negative correlation with SBs + FPG, strand breaks plus FPG-sensitive sites DNA oxidation (r = −0.75, p = 0.029), zinc was positively correlated (r = 0.78, p = 0.022).
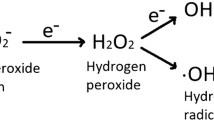
Experiments on aging
Following the early work in this field, it was shown that increases in 8-oxoGua and protein carbonyl content are associated with diminished life span in houseflies [28] and in mammals [29]; it was also demonstrated that Drosophila melanogaster age-resistant strains have enhanced superoxide dismutase (SOD) activity [30]; that human senescent fibroblasts have higher levels of 8-oxoGua in DNA; and that spin-trapping agents delay senescence in vitro [31]. More recently, overexpressing human catalase in transgenic mice, an increased life span and a reduced hydrogen peroxide production was observed [32].
The idea that oxygen damage is associated with cell aging is a sound result confirmed in a variety of living organisms. Later research has not challenged the theory connecting oxidation damage to aging, but has indicated that the process might be regulated by a complex system and not only by the steady state of intracellular oxidation. In fact, some strains of mice deficient in superoxide dismutase and glutathione peroxidase-1 have, as expected, increased oxidative damage, but no reduction in longevity. It is worth noting that tumor burden, but not incidence, is increased in these animals [33]. Recently, it has also been shown that specific mutants of C. elegans, characterized by slow metabolism and increased life span, have no increased resistance to oxidative stress or decreased oxidative damage, despite elevated levels of superoxide dismutase [34]. In these organisms, over-expression of SOD-1 seems to increase life span through the activation of longevity-promoting transcription factors [35].
A good example of the complexity of the aging processes is shown by the case of sirtuins. Over-expression of sirtuins was suggested as a mechanism of an increased life span in a variety of organisms. However, according to a recent report, these associations were due to the confounding effect of a varied genetic background. In fact, using more stringent genetic controls, no correlation was observed between over-expression of sir-2.1 and life span extension in C. elegans and D. melanogaster [36].
Considering results on life span extension by antioxidants and other supplements, despite a large body of published research, only a few controlled studies report convincing evidence. Among these, we can quote experiments on vitamin E in rats [37]; vitamin C and β-carotene in mice [38, 39]; vitamin E in Paramecium tetraurelia [40]; butylhydroxyanisole (BHA) in Callosobruchus maculatus [41]; the spin-trapping agent N-tert-α-phenyl-butylnitrone and β-catechin in senescence-accelerated mice [42, 43]; antioxidant vitamins in exercising rats [44]; Chinese traditional herbs in D. melanogaster [45]; and synthetic superoxide dismutase/catalase-mimetics in C. elegans [46].
Intervention studies based on biomarkers
There are many reports of studies in which subjects have been given antioxidant supplements and biomarkers of oxidative stress have been measured. It is helpful first to outline the various approaches taken.
The design of the study can be a single intervention, samples being taken at appropriate intervals over a day or so, or a trial of one to several weeks with (normally) daily administration of antioxidant(s). The simplest design of repeated intervention trial involves taking samples before and after the intervention. However, this is not recommended; a parallel group of matched subjects receiving a placebo should be run alongside the supplemented group to act as a control. The best design is probably the placebo-controlled crossover, in which two matched groups receive either placebo or supplement in a first phase, and then—after a washout period—the roles are reversed in phase two, so that all subjects ultimately have the same treatment.
Subjects can be healthy, or suffering from some disease or at risk of disease. Results with healthy individuals are more generally relevant. On the other hand, it is supposed that larger effects of antioxidants might be expected in subjects suffering from oxidative stress resulting from disease (though the supposition has not been confirmed by results).
Supplements can be either isolated antioxidants (or mixtures of antioxidants), or foods or drinks rich in antioxidants; the latter approach is more realistic, but less easy to carry out and the outcome is less easy to analyze because of the complexity of the food matrix.
Biomarkers of in vivo oxidative damage include lipid peroxidation products [F2-isoprostanes or malondialdehyde (MDA)] measured in blood or urine; protein carbonyls in plasma; oxidized DNA bases in lymphocytes; and oxidized nucleosides in urine. Questions are frequently raised concerning the validity of these biomarkers. Particular scrutiny was given in the ESCODD project [47] to 8-oxoGua (or its deoxyribonucleoside 8-oxodGuo) measured in the DNA of blood cells, because it was clear that reported levels of this lesion varied by orders of magnitude depending on the method used. Chromatographic methods are prone to oxidation of DNA during sample preparation, which results in a serious artifact. The comet assay and other methods that rely on release of 8-oxoGua by digestion with FPG seem not to suffer from this problem and give more accurate (though less precise) estimates of DNA damage. Reports of background damage levels exceeding about three 8-oxoGua per million guanine (Gua) in healthy subjects should be considered of doubtful value (and are not included in this review).
A distinct biomarker strategy is the ex vivo approach in which material (lymphocytes, plasma, etc.) is taken from the subjects before and after supplementation and tested for resistance to oxidation. H2O2 is a common challenging agent, inducing SBs in cellular DNA, the frequency of which reflects antioxidant status. The rate of oxidation of plasma lipids by ferrous iron and ascorbate is another indicator of susceptibility.
A comprehensive review of studies with biomarkers of DNA oxidation has been published by Møller and Loft [48]. Here, we will present just a few examples of repeated intervention trials.
In one of the first trials to use the comet assay to measure oxidized bases, a daily supplement of vitamins C and E and β-carotene or a placebo was given to smokers and non-smokers (25 in each group). After 20 weeks, significantly (p < 0.002) less oxidation of pyrimidines in lymphocyte DNA was seen in the supplemented groups, and their DNA was less damaged by H2O2 in vitro [49]. A four-week trial with vitamins C and E or placebo resulted in significant decreases in endonuclease III- and FPG-sensitive sites when vitamin C was administered in a slow release form, but not as a standard tablet [50]. In a crossover designed trial with different ‘doses’ of kiwifruit, significant decreases occurred in oxidized purines and pyrimidines in lymphocyte DNA, together with increases in resistance to H2O2 (p < 0.01) [51].
In another study, 246 women were randomly assigned to receive either 3.6 or 9.2 servings of fruits and vegetables per day for 2 weeks and a significant reduction in the urinary excretion of 8-iso-PGF2-α was observed in subjects on the high fruits and vegetables diet (p < 0.01) [52]. Purine oxidation in lymphocyte DNA was reported to be significantly decreased after one kiwifruit per day (p < 0.01); pyrimidine oxidation decreased after two fruits per day (p < 0.05) [53]. Consuming a portion of steamed broccoli (250 g/day) was recently associated with increased protection against H2O2-induced DNA SBs and lower oxidized DNA bases in lymphocytes from 27 young healthy smokers [54].
In contrast, a diet containing 600 g/day of fruits and vegetables (or the equivalent in antioxidants) [55] showed no effect; 2 months of dietary supplementation with vitamin C and vitamin E had also no significant effect on oxidative DNA damage measured as urinary 8-oxodGuo in non-smoking adults [56]. Various dosages of α-tocopherol for 8 weeks followed by an 8-week washout period had no effect on urinary lipid peroxidation in healthy adults [57].
There are some examples of trials with patients/stressed subjects: Vitamin C and E supplementation for 6 weeks in a small group of children with familial hypercholesterolemia restored endothelial function but not biomarkers of oxidative stress (antibodies to oxidized LDL, F2-isoprostanes, urinary 8-oxodGuo) [58]. In postmenopausal breast cancer survivors from the Women’s Healthy Eating and Living Study, a significant inverse association was found between total plasma carotenoid concentrations and urinary 8-oxodGuo and lipid peroxidation, (p = 0.001) but no protection by carotenoid supplementation [59]. A decrease in plasma F2-isoprostanes was found in 396 obese non-smokers who received vitamin C, vitamin E or placebo for 2 months, but only when baseline F2-isoprostane levels were >50 μg/mL (p = 0.01) [60]. Type 2 diabetes patients, given a flavonol (quercetin)-rich diet for 2 weeks in a crossover design, showed an increase in resistance to H2O2 attack on DNA (p = 0.037), but no effect on endogenous oxidized pyrimidines [61]. In a trial of 37 healthy, non-smoking postmenopausal women, randomly assigned to consume mixed carotenoids (beta-carotene, lutein, and lycopene; 4 mg each), 12 mg of a single carotenoid (β-carotene, lutein or lycopene), or placebo for 56 days, all carotenoid-supplemented groups showed significantly lower endogenous DNA damage (DNA breaks measured by the comet assay) than at baseline (p < 0.01), but there was no protection against H2O2-induced breaks [62].
Recently, 49 overweight, postmenopausal women were assigned to consume 2, 5, or 10 servings of fresh vegetables for 3 weeks with a 4-week washout period. Plasma carotenoids increased with number of servings, (overall p < 0.001); however, urinary concentrations of 8-isoprostane F2α, hexanoyl lysine, and serum C-reactive protein (all indicators of oxidative stress) were not affected [63].
Although a few years have elapsed, we may still conclude this section with the comments of Møller and Loft [48]. They reviewed repeated dose intervention trials measuring a variety of biomarkers of oxidative damage to DNA. Half of these were classified as having good design and realistic baseline values for DNA oxidation. None of the studies reported an increase in DNA damage, though many showed no effect. The reasons for null effects remain obscure; but Møller and Loft emphasized that ‘reduced levels of oxidatively damaged DNA in white blood cells… were reported in far more studies than expected by chance alone.’
Intervention studies with clinical endpoints
The possibility that the administration of antioxidant vitamins might decrease cell oxidative damage, thereby decreasing the incidence of degenerative diseases and cancer, was investigated with enthusiasm in the 90s and motivated many clinical studies. In fact, experimental work indicated a tumor-preventive effect of some antioxidants in animal models (see the review by Moon, [64]). An article published at the end of the century [65] listed about 50 promising compounds for future clinical trials on the basis of the literature published at that time.
A detailed review of this field is not the scope of the present commentary. However, it is evident that epidemiological considerations had their place in the choice of chemo-preventive compounds. Since a high consumption of fruits and vegetables was documented to affect common forms of cancers, it was reasonable to assume that antioxidant vitamins abundant in vegetables and fruits would have an effect on their own and that their chronic administration as supplements might result into a chemo-preventive effect in clinical trials [66].
Reviewing this material and the many review articles published in that period, it is hard to ignore the widespread assumption that natural antioxidants and vitamins had low inherent toxicity; therefore, clinical trials seemed to have few risks and possible big gains. In trials aimed at inhibiting cancer, also all-cause mortality and cardiovascular mortality was often recorded. These additional data are clearly of interest for the evaluation of the overall health effects of these supplementations.
Out of the large body of literature reporting results on intervention studies with clinically relevant endpoints, we selected for the present critical evaluation only data obtained from relatively large clinical trials (>1,000), with a long follow-up (>3 years), published up to 2011. We examined cardiovascular and all-cause mortality and cancer incidence/mortality as endpoints. Our aim was not to review in detail all the existing literature, a task accomplished by many available reviews and meta-analyses, but to comment on the most relevant information and suggest some general explanations for the results obtained.
Effects on mortality
α-tocopherol and β-carotene
One of the first studies involved 1,720 subjects in a program for skin cancer prevention (SCPS) in the USA; it was published in 1996 [10]. β-carotene (50 mg) was administered daily for 4.3 years and after a follow-up of 8.2 years no variation was reported for all-cause mortality (RR: 1.03; CL: 0.82–1.30). Similar results were reported in 1996 by the Physicians’ Health Study (PHS) [67], with the same dosage of β-carotene administered to 22,071 subjects on alternate days for 12.9 years, with a follow-up of 6.1 years (RR: 1.01; CL:0.93–1.1).
On the contrary, a clear detrimental effect was reported in the ATBC study in Finland, involving 1,862 males with previous myocardial infarction and 1,057 with previous stroke, administered α-tocopherol (50 mg) and/or β-carotene (20 mg) daily for 5.3 years [68, 69]. In this study the RR for total cardiovascular mortality with α-tocopherol was 1.33 (CL: 0.86–2.05) and for the combined treatment 1.58 (CL: 1.05–2.4). The same group reported [70] an increased risk for all-cause mortality on 29,133 male smokers with the same combined treatment for 6.1 years and a follow-up of 12.1 years (RR: 1.5; CL: 1–2.25).
The CARET study in the USA (2004), administering β-carotene (30 mg) and retinyl palmitate (25,000 IU) daily, singly or combined, for 6.1 years, ended up after 12.1 years recording a non-significant variation in all-cause mortality (RR: 1.08; CL: 0.99–1.17) [71].
It is also worth citing a large a cluster trial in Bangladesh published recently on 125,257 pregnant and postpartum women, in which retinol (7 mg) and β-carotene (42 mg) were administered, reporting no significant variation in maternal and newborn mortality (retinol: 1.15; CL: 0.75–1.76 and β-Carotene: 1.21; CL: 0.81–1.81) [72].
A clear protection against cardiovascular mortality was observed in the early CHAOS study in the UK (1996), on 2,002 subjects administered 400–800 IU vitamin E daily for 366 or 731 days and followed for 510 days (RR: 0.53; CL: 0.34–0.83) [73]. This study created strong expectations on the preventive effects of vitamin E in cardiovascular mortality, but unfortunately later studies did not confirm this favorable effect: the GISSI in Italy (1999), administering 300 mg vitamin E for 3.5 years to 2,830 infarction patients, reported a RR of 0.86; CL: 0.72–1.82) [74]; the HOPE study in Europe and the Americas (published in 2000) on 9,541 subjects administered 400 mg vitamin E for 4.5 years, followed for 6 years, also did not show effects on mortality (RR: 1.05; CL: 0.9–1.22) [75]; all-cause mortality was not varied in a large USA study (WHS) published in 2005 on 38,876 women administered vitamin E (400 IU) for 4.5 years (RR: 1.04; CL: 0.93–1.12) [76].
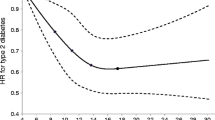
In 2005, a meta-analysis was published of 19 clinical trials of vitamin E supplementation, ranging from 16.5 to 2,000 IU/day, in which a relationship between the dosage of vitamin E administered and all-cause mortality was apparent, with significant increased risk with dosages greater than 150 IU/day [77].
Multivitamins and minerals
Controlled trials of with multivitamins and mineral supplementation devoid of apparent bias are comparatively fewer. An early large intervention study (1993) in China, administering various mixes of retinol, zinc, riboflavin, niacin, ascorbic acid, molybdenum, selenium, α-tocopherol, and β-carotene, registered a significant reduction of mortality only for the combination of the last three supplements (50 μg, 30 mg and 15 mg, respectively) in the group of subjects younger than 55 (RR: 0.88; CL: 0.82–0.95) [78].
A study on 4,753 participants with ocular disorders conducted in the USA (AREDS) with vitamin C (500 mg), vitamin E (400 IU), β carotene (15 mg), and zinc oxide (80 mg), supplemented daily, reported in 2004 after 6.5 years of follow-up that only participants randomly assigned to receive zinc had lower mortality (RR: 0.73; CI: 0.61–0.89). No significant effects were reported for the other supplements (RR: 1.15; CL: 0.90–1.48) [79].
A trial in the USA on folic acid (2.5 mg), vitamin B6 (50 mg), and vitamin B12 (1 mg) on 5,442 health professional women at risk [80] reported in 2008 no variation of cardiovascular mortality (RR: 1.01; CL: 0.76–1.35).
Two studies with daily supplementation of selenium (200 μg) in the USA, the first on 1,312 patients with skin carcinoma and the second on 1,004 healthy subjects, reported no significant changes in all-cause mortality (RR: 0.83; CL: 0.63–1.08 and 1.22; CL: 0.76–1.95, respectively) [81, 82].
Finally, in 2010, it was reported that in a large French study involving 12,741 subjects (SUVIMAX), supplementing with ascorbic acid (120 mg), vitamin E (30 mg), β-carotene (6 mg), selenium (100 μg), and zinc (20 mg) for 7 years, with a follow-up of 5 years, there was no significant effect on all-cause mortality (RR: 0.98; CL: (0.75–1.26) [83].
Effects on cancer
β-carotene, retinyl palmitate, vitamin E, vitamin C, and selenium
One of the earliest documented effects of these supplements originates in the Physicians Health Study in the USA. According to a paper published in 1996, β-carotene (50 mg) on alternate days for 12.9 years, with a follow-up of 6.1 years, administered to 22,071 American physicians, did not vary the occurrence of cancer (RR 0.98; CL: 0.91–1.06) [67].
The results of a study in the UK (MRC/BHF), published in 2002, reported that vitamin E (600 mg), vitamin C (250 mg and β-carotene (20 mg), administered daily to 20,536 adults with coronary disease and diabetes for 5 years and a follow-up of 7 years, similarly had no effect on the occurrence of cancer (RR: 0.98; CL: 0.89–1.08) [84].
In the ATBC trial in Finland on 29,133 male smokers, with daily supplements of β-carotene (20 mg), α-tocopherol (50 mg), or both, lung cancer risk was not varied by α-tocopherol (RR: 0.99; CL: 0.87–1.13), but β-carotene significantly increased risk (RR: 1.16, CL: 1.02-1.33); the effect was more evident in heavy smokers (RR:1.25; CL: 1.07–1.46) and heavy drinkers (RR: 1.35; CL: 1.01–1.81) [85, 86]. For prostate cancer incidence (n = 672), the RR was 0.88 (CL: 0.76–1.03) for participants receiving α-tocopherol [87–89].
In parallel, the results of the CARET study in the USA were published in 2004; daily supplementation of 18,318 smokers and asbestos-exposed subjects for 10 years with β-carotene (30 mg) and retinyl palmitate (25,000 IU), with a follow-up of 11 years, resulted in a significant increase in lung cancer (RR:1.28; CL: 1.04–1.57). Also an increase of aggressive prostate cancer was reported (RR: 1.52; CL: 1.03–2.24) [89, 90].
On the contrary, the previously quoted WHS group in the USA, supplementing 39,876 women daily for 2.1 years with β-carotene on, published in 2002 that the frequency of total cancer was not altered (in the highest quartile of plasma β-carotene the RR was 1.34 (CL: 0.81–2.22) [91].
A recent meta-analysis [92] considered the effect of β-carotene and related compounds on cancer in 9 randomized trials. No effect of β-carotene supplementation was observed on the incidence of all cancer (RR: 1.01; CL: 0.98–1.04). The incidence of lung and stomach cancers were significantly increased by β-carotene (RR: 1.16; CL: 1.06–1.27 and 1.34; CL: 1.06–1.70, respectively). Fritz et al. [93] analyzed 248 studies on treatment, primary and secondary prevention of lung cancer after supplementation. Although some studies demonstrated significant benefits, there was no overall convincing evidence for the efficacy of vitamin A or related retinoids in the treatment or prevention of lung cancer. Jeon et al. [94] recently reviewed 848 articles for a total of 40,544 participants, of which 20,290 were in β-carotene supplement groups and 20,254 in placebo groups. β-carotene supplements had no significant preventive effect on cancer incidence or mortality.
In conclusion, historic data and recent meta-analyses confirm that β-carotene and related compounds have no positive role in the prevention or treatment of cancer.
No significant protection of vitamin E against cancer was reported by the HOPE study in America and Europe [2000 with vitamin E (400 IU) daily × 4.5 years, follow-up 7 years, with 3,994 subjects in the intervention group and 738 in the passive follow-up; RR for all cancer: 0.94; CL 0.84–1.06] [75].
In 2005, the results of the WHS in the USA, in which Vitamin E (600 IU) was administered daily × 4.5 years to 39,876 women >45 years, similarly reported no effect on cancer incidence (RR: 1.01; CL: 0.94–1.08) [91].
The large PHS in the USA [95], administering vitamin C (400 mg) or vitamin E (400 mg) on alternate days to 14,641 physicians, starting in 1997 and completed in 2007, recorded no variation of prostate cancer incidence (RR: 0.97; CL: 0.85–1.09) or total cancer incidence (RR: 1.04; CL: 0.95–1.13) with vitamin E or with vitamin C supplementation (RR for prostate cancer: 1.02 (CL: 0.90–1.15; RR for total cancer: 1.01; CL: 0.92–1.10).
The report of the SELECT study in the USA (2011), administering selenium (200 μg) and vitamin E (400 IU) daily, alone or in combination, to 35,533 older men, showed on the contrary a slight, but significant, increase in the risk of prostate cancer with vitamin E (RR: 1.17; CL: 1004–1.36) and no variation with selenium (RR: 1.09; CL: 0.89–1.22) [96].
Bjelakovic et al. [97] published a meta-analysis on 20 randomized trials (including 211,818 participants), assessing beta-carotene (12 trials), vitamin A (4 trials), vitamin C (8 trials), vitamin E (10 trials), and selenium (9 trials). Antioxidant vitamin supplements were without significant effects on gastrointestinal cancers (RR: 0.94; 95 % CI 0.83–1.06).
Recently, Papaioannou et al. [98] reviewed twelve studies on the effects of vitamin A, C, and E, selenium, and β-carotene antioxidants in the chemoprevention of colorectal cancer and adenomas; in the nine studies comparing antioxidants with controls (recruited subjects: 148,922), there was no difference in the incidence of colorectal cancer (RR: 1.00, CL: 0.88–1.13). Of the 14 combinations of antioxidants employed, one reported a statistically significant increase in relative risk of adenoma after vitamin E (RR 1.74, CL: 1.09–1.79) or vitamin E plus β-carotene (RR 1.63, CL: 1.01–2.63).
Promising results on selenium alone were reported in 2002 by the Nutritional Prevention of Cancer Trial (NPCT) on 1,312 healthy USA subjects, using selenium (200 μg) daily for 4.5 year with a follow-up of 6.4 years. At the end of the treatment, selenium supplementation reduced significantly total cancer (RR: 0.75; CL: 0.58–0.97) and prostate cancer incidence (RR = 0.48; C: 0.28–0.80) [99].
A recent meta-analysis, considering the results of fifteen human studies of supplementation, concluded that selenium may reduce risk of lung cancers in populations with lower baseline selenium status (serum <106 ng/mL); however, an increase of lung cancer risk is observed with higher selenium serum levels (≥121.6 ng/mL). No statistically significant effects were reported for other cancers (RR: 1.51; CL: 0.7–3.24) [100].
According to another analysis of Bjelakovic et al. [97], selenium seemed to show significant beneficial effects on gastrointestinal cancer occurrence (RR: 0.59; CL: 0.46–0.75).
Multivitamins and minerals
During an early study in China (NIT), retinol (5,000 IU), zinc (22.5 mg), (factor A); riboflavin (3.2 mg), niacin (40 mg) (factor B); ascorbic acid (120 mg), molybdenum (30 μg) (factor C), selenium (50 μg), α-tocopherol (30 mg), β-carotene (15 mg) (factor D) were administered to 29,584 adults for the prevention of gastric and esophageal cancer for 6 years. The published report in 1994 showed no statistically significant effects of any treatment combination [101].
The WACS study in the USA, using ascorbic acid (500 mg), vitamin E (600 mg), β-carotene (50 mg), on alternate days on 8,171 health professional women, with a follow-up of 9.4 years, recorded no variation in total cancer with vitamin C (RR: 1.11; CL: 0.95–1.30), vitamin E (RR: 0.93 0.79–1.09) or β-carotene (RR: 1.0; CL: 0.85–1.17) [102]. The same group reported in 2008 that folic acid (2.5 mg), vitamin B6 (50 mg) and vitamin B12 (1 mg) daily, with a follow-up of 7.3 years, administered to 5,442 women, did not vary significantly the risk of total cancer (RR: 0.97; CL: 0.79–1.18) [103].
The previously mentioned SUVIMAX study in France, administering ascorbic acid (120 mg), vitamin E (30 mg), β-carotene (6 mg), selenium (100 μg), and zinc (20 mg) daily for 7 years to 12,741 subjects, with a follow-up of 5 years, registered no variation of total cancer (RR: 0.98; CL: 0.75–1.27) and a significant increase in skin cancer in females (RR:1.7; CL: 1.08–2.67) [83].
Myung and coworkers [104] recently published a meta-analysis on 22 case–control studies for a total of 10,073 participants, showing a significant preventive effect on cervical cancer for subjects supplemented with vitamin B12 (RR :0.35; CL 0.19–0.63; n = 2), vitamin C (RR 0.67, CL: 0.55–0.82; n = 8), vitamin E (RR: 0.56; CL: 0.35–0.88; n = 10), and β-carotene (RR: 0.68, CL 0.55–0.84; n = 9).
Conclusions
A summary review of the evidence obtained from major clinical trials with antioxidant vitamins and minerals (β-carotene, α-tocopherol, vitamin E, various vitamins and minerals, and selenium) indicates that most studies ended up with no significant variation in all-cause mortality. All-cause mortality is a robust indicator of effects on human health and is subject to little experimental error. In some supplementation studies, a significant increase in mortality was observed for certain antioxidants. In fact, a meta-analysis of 19 clinical trials of vitamin E supplementation, ranging from 16.5 to 2,000 IU/day, showed a relationship between the dosage of vitamin E administered and all-cause mortality, with significantly increased risk with dosages greater than 150 IU/day [77].
The main conclusions of this commentary regarding the effects of antioxidant vitamins on mortality coincide with the meticulous analysis of the Cochrane collaboration study on antioxidant supplementation [105]. This extensive meta-analysis included evidence published up to 2005 and was based upon forty-seven trials with a low risk of systematic bias, including a total of 180,938 participants. According to their report, antioxidant supplementation significantly increased mortality (RR: 1.05, CL: 1.02–1.08). In the same publication, the analysis of separate effects showed a significantly increased mortality by supplementation with vitamin A (RR: 1.16, CL: 1.10–1.24), β-carotene (RR: 1.07, CL: 1.02–1.11) and vitamin E (RR: 1.04, CL: 1.01–1.07), but no significant benefit or detrimental effect of vitamin C (RR: 1.06, CL: 0.94–1.20) or selenium (RR: 0.90, CL: 0.80–1.01).
Considering the effects of antioxidant supplementation on cancer incidence in clinical trials, it is clear that β-carotene supplementation significantly increased lung cancer incidence and aggressive prostate cancer [85–90].
Selenium on the contrary showed significant beneficial effects on gastrointestinal cancer and reduced the risk of lung cancer in subjects with lower baseline selenium status [99, 100].
For multivitamin and mineral supplements, no reduction in cancer incidence was observed, but some reports, needing to be confirmed, indicate a possible beneficial effect in cervical cancer [104].
As a whole, the evidence available shows sometimes a detrimental but mostly a null effect on mortality and on cancer incidence of supplements with β-carotene, α-tocopherol, vitamin E, various vitamins and minerals with the possible exception of selenium in individuals with low intake.
It is difficult not to regard this enormous amount of work as a disappointment. We can advance a series of hypotheses to explain it.
-
(A)
The dosages of antioxidants in the supplementation regimens were possibly too high. The case is well illustrated by β-carotene. In some trials, initial β-carotene plasma levels were low, given the unbalanced diet of the test populations (such as in Linxian, China, 5.9–6.8 μg × dL−1) [101]. In contrast, in countries with adequate or excessive nutrition, the plasma levels of β-carotene were considerably higher (10–34 μg × dL−1) [106–108]. Although in these studies, a plasma level-related effect was not detectable or statistically significant, it is possible that a supplementation with additional β-carotene might have exerted a detrimental effect in well-fed populations. This could be the case for β-carotene, vitamin E, and α-tocopherol, which have U-shaped dose–response curves.
-
(B)
The effect of food is complex and some disease-preventive effects of an optimal diet may not be reproduced with selected purified ingredients. Administering supplements instead of improving the diet is a shortcut that might not provide an adequate solution to dietary imbalances.
-
(C)
In different human populations, the association between a low/high level of antioxidant vitamins and the increase/decrease of a specific pathological process might be the indicator of a bad/good nutritional status and not causally connected with antioxidant vitamins themselves.
-
(D)
The choice of specific antioxidant supplements in many intervention studies might not have been ideal. The list of natural antioxidants with possible health-promoting effects is long, and the chosen supplements might not have been the best.
-
(E)
The hypothesis suggesting beneficial effects of increasing ab-externo cellular antioxidants might be simplistic. Increasing levels of antioxidants may actually have deleterious effects on cellular functions. For instance, in carcinogenesis, some recent evidence indicates that excessive oxidative damage might limit the growth of cancer cells through an increased apoptotic rate in the tumor or its metastases [109]. Decreasing oxidative damage with externally administered compounds at relatively high dosage may have detrimental effects, possibly increasing the growth of tumors. An increased incidence of cancer decreases life span, given its fundamental role in human mortality. At present, it is generally agreed that intracellular free radicals have important signaling functions, which might be needed for optimal cell homeostasis and cancer control.
-
(F)
Although some antioxidants increase cell survival in vitro, this does not necessarily mean an increase in life span by chronic administration in animals or humans, as demonstrated by the failure of resveratrol administration to extend life span in mice [110].
-
(G)
A preventive effect of antioxidant vitamins in chemically induced tumors of experimental animals may not automatically translate into an effect on spontaneous human cancer.
The contrast between the generally null or deleterious health effects of antioxidant vitamins and the protective effects of antioxidants shown in many studies as a decrease in the level of oxidation damage also demands explanation. At least in healthy individuals, the intrinsic antioxidant defences are sufficient to keep oxidation damage at a very low level, which likely reflects a tolerable, or even desirable balance. After all, as discussed above, evidence is accumulating that we need a certain amount of oxidative stress, since reactive oxygen is involved in various metabolic processes including the inflammatory response and cell signaling. A decrease in DNA oxidation might not have favorable effects if accompanied by imbalances in cell metabolism.
In conclusion, the efforts to find in the antioxidant vitamins the pill of eternal youth, protecting against cancer and cardiovascular diseases, have produced no striking results. Millions of people ingest the antioxidant supplements described in this commentary, convinced that they will improve their health and survival. Often these supplements are consumed at mega-doses, with probably more detrimental effect. As nutrition scientists, we should warn health authorities not to encourage, or even positively to discourage, these practices. An official warning to consumers was recently issued by the Ministry of Health of Italy [111].
At present, more than 1,700 clinical studies with antioxidant vitamins are recorded in PubMed. We hope that new agents will be more successful, but more information about the mechanisms of action and the effective dosages of these new compounds in experimental systems would improve the chances of finding useful human applications and reducing their possible harm.
References
Harman D (1956) Aging: a theory based on free radical and radiation chemistry. J Gerontol 11:298–300
Adelman R, Saul RL, Ames BN (1988) Oxidative damage to DNA: relation to species metabolic rate and lifespan. Proc Natl Acad Sci USA 85(8):2706–2708
Peto R, Doll R, Buckley JD, Sporn MB (1981) Can dietary beta-carotene materially reduce human cancer rates? Nature 290(5803):201–208
Singh PM, Sabaté J, Fraser GR (2003) Does low meat consumption increase life expectancy in humans. Am J Clin Nutr 78(suppl):526S–532S
Fortes C, Forastiere F, Farchi S, Rapiti E, Pastori G, Perucci CA (2000) Diet and overall survival in a cohort of very elderly people. Epidemiology 4:440–445
American Institute for Cancer Research/World Cancer Research Fund, American Institute for Cancer Research (1997) Food, nutrition, and the prevention of cancer: a global perspective. Washington DC, USA
American Institute for Cancer Research/World Cancer Research Fund, American Institute for Cancer Research (2007) Food, nutrition, PHYSICAL ACTIVITY and the prevention of cancer: a global perspective, Washington DC, USA
Stähelin HB, Gey KF, Eichholzer M, Lüdin E (1991) Beta-carotene and cancer prevention: the Basel Study. Am J Clin Nutr 53(1 Suppl):265S–269S
Chen J, Geissler C, Parpia B, Li J, Campbell TC (1992) Antioxidant status and cancer mortality in China. Int J Epidemiol 21(4):625–635
Greenberg ER, Baron JA, Karagas MR, Stukel TA, Nierenberg DW, Stevens MM, Mandel JS, Haile RW (1996) Mortality associated with low plasma concentration of beta carotene and the effect of oral supplementation. JAMA 275(9):699–703
Tsubono Y, Tsugane S, Gey KF (1999) Plasma antioxidant vitamins and carotenoids in five Japanese populations with varied mortality from gastric cancer. Nutr Cancer 34(1):56–61
Wright ME, Lawson KA, Weinstein SJ, Pietinen P, Taylor PR, Virtamo J, Albanes D (2006) Higher baseline serum concentrations of vitamin E are associated with lower total and cause-specific mortality in the α-Tocopherol, β-Carotene Cancer Prevention Study. Am J Clin Nutr 84(5):1200–1207
Yuan JM, Ross RK, Gao YT, Qu YH, Chu XD, Yu MC (2004) Prediagnostic levels of serum micronutrients in relation to risk of gastric cancer in Shanghai, China. Cancer Epidemiol Biomarkers Prev 13(11 Pt 1):1772–1780
Watters JL, Gail MH, Weinstein SJ, Virtamo J, Albanes D (2009) Associations between alpha-tocopherol, beta-carotene, and retinol and prostate cancer survival. Cancer Res 69(9):3833–3841
Buijsse B, Feskens EJ, Schlettwein-Gsell D, Ferry M, Kok FJ, Kromhout D, de Groot LC (2005) Plasma carotene and alpha-tocopherol in relation to 10-y all-cause and cause-specific mortality in European elderly: the Survey in Europe on Nutrition and the Elderly, a Concerted Action (SENECA). Am J Clin Nutr 82(4):879–886
Penney KL, Schumacher FR, Li H, Kraft P, Morris JS, Kurth T, Mucci LA, Hunter DJ, Kantoff PW, Stampfer MJ, Ma JA (2010) Large prospective study of SEP15 genetic variation, interaction with plasma selenium levels, and prostate cancer risk and survival. Cancer Prev Res (Phila) 3(5):604–610
Lauretani F, Semba RD, Dayhoff-Brannigan M, Corsi AM, Di Iorio A, Buiatti E, Bandinelli S, Guralnik JM, Ferrucci L (2010) Low total plasma carotenoids are independent predictors of mortality among older persons: the InCHIANTI study. Eur J Nutr 47(6):335–340
Shardell MD, Alley DE, Hicks GE, El-Kamary SS, Miller RR, Semba RD, Ferrucci L (2011) Low-serum carotenoid concentrations and carotenoid interactions predict mortality in US adults: the Third National Health and Nutrition Examination Survey. Nutr Res 31(3):178–189
Brevik A, Andersen LF, Karlsen A, Trygg KU, Blomhoff R, Drevon CA (2004) Six carotenoids in plasma used to assess recommended intake of fruits and vegetables in a controlled feeding study. Eur J Clin Nutr 58(8):1166–1173
Kažimírová A, Barancoková M, Volkovová K, Staruchová M, Krajcovicová-Kudlácková M, Wsólová L, Collins AR, Dušinská M (2004) Does a vegetarian diet influence genomic stability? Eur J Nutr 43:32–38
Dhawan A, Mathur N, Seth PK (2001) The effect of smoking and eating habits on DNA damage in Indian population as measured in the Comet assay. Mutat Res 474:121–128
Fenech M, Rinaldi J (1995) A comparison of lymphocyte micronuclei and plasma micronutrients in vegetarians and non-vegetarians. Carcinogenesis 16:223–230
Krajcovicová-Kudlácková M, Valachovicová M, Pauková V, Dusinská M (2008) Effects of diet and age on oxidative damage products in healthy subjects. Physiol Res 57(4):647–651
Somannavar MS, Kodliwadmath MV (2012) Correlation between oxidative stress and antioxidant defence in South Indian urban vegetarians and non-vegetarians. Eur Rev Med Pharmacol Sci 16(3):351–354
Collins AR, Olmedilla B, Southon S, Granado F, Duthie SJ (1998) Serum carotenoids and oxidative DNA damage in human lymphocytes. Carcinogenesis 19(12):2159–2162
Giovannelli L, Saieva C, Masala G, Testa G, Salvini S, Pitozzi V, Riboli E, Dolara P, Palli D (2002) Nutritional and lifestyle determinants of DNA oxidative damage: a study in a Mediterranean population. Carcinogenesis 23:1483–1489
Dusinska M, Vallova B, Ursinyova M, Hladikova V, Smolkova B, Wsolova L, Raslova K, Collins AR (2002) DNA damage and antioxidants; fluctuations through the year in a central European population group. Food Chem Toxicol 40:1119–1123
Agarwal S, Sohal RS (2004) DNA oxidative damage and life expectancy in houseflies. Proc Natl Acad Sci USA 91(25):12332–12335
Sohal RS, Kamzalov S, Sumien N, Ferguson M, Rebrin I, Heinrich KR, Forster MJ (2006) Effect of coenzyme Q10 intake on endogenous coenzyme Q content, mitochondrial electron transport chain, antioxidative defenses, and lifespan of mice. Free Radic Biol Med 40(3):480–487
Arking R, Burde V, Graves K, Hari R, Feldman E, Zeevi A, Soliman S, Saraiya A, Buck S, Vettraino J, Sathrasala K, Wehr N, Levine RL (2000) Forward and reverse selection for longevity in Drosophila is characterized by alteration of antioxidant gene expression and oxidative damage patterns. Exp Gerontol 35(2):167–185
Chen Q, Fischer A, Reagan JD, Yan LJ, Ames BN (1995) Oxidative DNA damage and senescence of human diploid fibroblast cells. Proc Natl Acad Sci USA 92(10):4337–4341
Schriner SE, Linford NJ, Martin GM, Treuting P, Ogburn CE, Emond M, Coskun PE, Ladiges W, Wolf N, Van Remmen H, Wallace DC, Rabinovitch PS (2005) Extension of murine lifespan by overexpression of catalase targeted to mitochondria. Science 308(5730):1909–1911
Zhang Y, Ikeno Y, Qi W, Chaudhuri A, Li Y, Bokov A, Thorpe SR, Baynes JW, Epstein C, Richardson A, Van Remmen H (2009) Mice deficient in both Mn superoxide dismutase and glutathione peroxidase-1 have increased oxidative damage and a greater incidence of pathology but no reduction in longevity. J Gerontol A Biol Sci Med Sci 64(12):1212–1220
Van Raamsdonk JM, Meng Y, Camp D, Yang W, Jia X, Bénard C, Hekimi S (2010) Decreased energy metabolism extends lifespan in Caenorhabditis elegans without reducing oxidative damage. Genetics 185(2):559–571
Cabreiro F, Ackerman D, Doonan R, Araiz C, Back P, Papp D, Braeckman BP, Gems D (2011) Increased lifespan from overexpression of superoxide dismutase in Caenorhabditis elegans is not caused by decreased oxidative damage. Free Radic Biol Med 51(8):1575–1582
Burnett C, Valentini S, Cabreiro F, Goss M, Somogyvári M, Piper MD, Hoddinott M, Sutphin GL, Leko V, McElwee JJ, Vazquez-Manrique RP, Orfila AM, Ackerman D, Au C, Riesen M, Howard K, Neri C, Bedalov A, Kaeberlein M, Soti C, Partridge L, Gems D (2011) Absence of effects of Sir2 overexpression on lifespan in C. elegans and Drosophila. Nature 477(7365):482–485
Porta EA, Joun NS, Nitta RT (1980) Effects of the type of dietary fat at two levels of vitamin E in Wistar male rats during development and aging. I. Lifespan, serum biochemical parameters and pathological changes. Mech Aging Dev 13(1):1–39
Massie HR, Aiello VR, Doherty TJ (1984) Dietary vitamin C improves the survival of mice. Gerontology 30(6):371–375
Massie HR, Ferreira JR Jr, DeWolfe LK (1986) Effect of dietary beta-carotene on the survival of young and old mice. Gerontology 32(4):189–195
Thomas J, Nyberg D (1988) Vitamin E supplementation and intense selection increase clonal lifespan in Paramecium tetraurelia. Exp Gerontol 23(6):501–512
Mahajan S, Garg SK, Lobana TS (1994) Effect of BHA on longevity, antioxygenic enzymes and peroxides in Callosobruchus maculatus. Exp Gerontol 29(5):585–591
Edamatsu R, Mori A, Packer L (1995) The spin-trap N-tert-alpha-phenyl-butylnitrone prolongs the lifespan of the senescence accelerated mouse. Biochem Biophys Res Commun 211(3):847–849
Kumari MV, Yoneda T, Hiramatsu M (1997) Effect of “beta CATECHIN” on the life span of senescence accelerated mice (SAM-P8 strain). Biochem Mol Biol Int 41(5):1005–1011
Holloszy JO (1998) Longevity of exercising male rats: effect of an antioxidant supplemented diet. Mech Aging Dev 100(3):211–219
Cui X, Dai XG, Li WB, Zhang BL, Fang YZ (1999) Effects of lu-duo-wei capsule on prolonging lifespan of housefly and Drosophila melanogaster. Am J Chin Med 27(3–4):407–413
Melov S, Ravenscroft J, Malik S, Gill MS, Walker DW, Clayton PE, Wallace DC, Malfroy B, Doctrow SR, Lithgow GJ (2000) Extension of lifespan with superoxide dismutase/catalase mimetics. Science 289(5484):1567–1569
ESCODD, Gedik CM, Collins A (2004) Establishing the background level of base oxidation in human lymphocyte DNA: results of an inter-laboratory validation study. FASEB J. www.fasebj.org/cgi/doi/10.1096/fj.04-1767fje
Møller P, Loft S (2004) Interventions with antioxidants and nutrients in relation to oxidative DNA damage and repair. Mutat Res 551:79–89
Duthie SJ, Ma A, Ross MA, Collins AR (1996) Antioxidant supplementation decreases oxidative DNA damage in human lymphocytes. Cancer Res 56(6):1291–1295
Møller P, Viscovich M, Lykkesfeld J, Loft S, Jensen A, Poulsen HE (2004) Vitamin C supplementation decreases oxidative DNA damage in mononuclear blood cells of smokers. Eur J Nutr 43:267–274
Collins AR, Harrington V, Drew J, Melvin R (2003) Nutritional modulation of DNA repair in a human intervention study. Carcinogenesis 24:511–515
Thompson HJ, Heimendinger J, Sedlacek S, Haegele A, Diker A, O’Neill C, Meinecke B, Wolfe P, Zhu Z, Jiang W (2005) 8-Isoprostane F2alpha excretion is reduced in women by increased vegetable and fruit intake. Am J Clin Nutr 82(4):768–776
Brevik A, Gaivão I, Medin T, Jørgenesen A, Piasek A, Eliasson J, Karlsen A, Blomhoff R, Veggan T, Duttaroy AK, Collins AR (2011) Supplementation of a western diet with golden kiwifruits (Actinidia chinensis var’.Hort 16A’:) effects on biomarkers of oxidation damage and antioxidant protection. Nutr J 18(10):54
Riso P, Martini D, Møller P, Loft S, Bonacina G, Moro M, Porrini M (2010) DNA damage and repair activity after broccoli intake in young healthy smokers. Mutagenesis 25(6):295–602
Møller P, Vogel U, Pedersen A, Dragsted LO, Sandström B, Loft S (2003) No effect of 600 grams fruit and vegetables per day on oxidative DNA damage and repair in healthy nonsmokers. Cancer Epi Biomark Prev 12:1016–1022
Huang HY, Helzlsouer KJ, Appel LJ (2000) The effects of vitamin C and vitamin E on oxidative DNA damage: results from a randomized controlled trial. Cancer Epidemiol Biomarkers Prev 7:647–652
Meagher EA, Barry OP, Lawson JA, Rokach J, FitzGerald GA (2001) Effects of vitamin E on lipid peroxidation in healthy persons. JAMA 285(9):1178–1182
Engler MM, Engler MB, Malloy MJ, Chiu EY, Schloetter MC, Paul SM, Stuehlinger M, Lin KY, Cooke JP, Morrow JD, Ridker PM, Rifai N, Miller E, Witztum JL, Mietus-Snyder M (2003) Antioxidant vitamins C and E improve endothelial function in children with hyperlipidemia: endothelial Assessment of Risk from Lipids in Youth (EARLY) Trial. Circulation 108(9):1059–1063
Thomson CA, Stendell-Hollis NR, Rock CL, Cussler EC, Flatt SW, Pierce JP (2007) Plasma and dietary carotenoids are associated with reduced oxidative stress in women previously treated for breast cancer. Cancer Epidemiol Biomarkers Prev 10:2008–2015
Block G, Jensen CD, Morrow JD, Holland N, Norkus EP, Milne GL, Hudes M, Dalvi TB, Crawford PB, Fung EB, Schumacher L, Harmatz P (2008) The effect of vitamins C and E on biomarkers of oxidative stress depends on baseline level. Free Radic Biol Med 45(4):377–384
Lean MEJ, Noroozi M, Kelly I, Burns J, Talwar D, Sattar N, Crozier A (1999) Dietary flavonols protect diabetic human lymphocytes against oxidative damage to DNA. Diabetes 48:176–181
Zhao X, Aldini G, Johnson EJ, Rasmussen H, Kraemer K, Woolf H, Musaeus N, Krinsky NI, Russell RM, Yeum KJ (2006) Modification of lymphocyte DNA damage by carotenoid supplementation in postmenopausal women. Am J Clin NutrJan 83(1):163–169
Crane TE, Kubota C, West JL, Kroggel MA, Wertheim BC, Thomson CA (2011) Increasing the vegetable intake dose is associated with a rise in plasma carotenoids without modifying oxidative stress or inflammation in overweight or obese postmenopausal women. J Nutr 141(10):1827–1833
Moon RC, Mehta RG (1989) Chemoprevention of experimental carcinogenesis in animals. Prev Med 18(5):576–591
Kelloff GJ, Crowell JA, Steele VE, Lubet RA, Boone CW, Malone WA, Hawk ET, Lieberman R, Lawrence JA, Kopelovich L, Ali I, Viner JL, Sigman CC (1999) Progress in cancer chemoprevention. Ann N Y Acad Sci 889:1–13
Abdulla M, Gruber P (2000) Role of diet modification in cancer prevention. BioFactors 12(1–4):45–51
Hennekens CH, Buring JE, Manson JE, Stampfer M, Rosner B, Cook NR, Belanger C, LaMotte F, Gaziano JM, Ridker PM, Willett W, Peto R (1996) Lack of effect of long-term supplementation with beta carotene on the incidence of malignant neoplasms and cardiovascular disease. N Engl J Med 334:1145–1149
Rapola JM, Virtamo J, Ripatti S, Huttunen JK, Albanes D, Taylor PR, Heinonen OP (1997) Randomised trial of alpha-tocopherol and beta-carotene supplements on incidence of major coronary events in men with previous myocardial infarction. Lancet 349(9067):1715–1720
Leppälä JM, Virtamo J, Fogelholm R, Huttunen JK, Albanes D, Taylor PR, Heinonen OP (2000) Controlled trial of alpha-tocopherol and beta-carotene supplements on stroke incidence and mortality in male smokers. Arterioscler Thromb Vasc Biol 1:230–235
Törnwall ME, Virtamo J, Korhonen PA, Virtanen MJ, Taylor PR, Albanes D, Huttunen JK (2004) Effect of alpha-tocopherol and beta-carotene supplementation on coronary heart disease during the 6-year post-trial follow-up in the ATBC study. Eur Heart J 25(13):1171–1178
Goodman GE, Thornquist MD, Balmes J, Cullen MR, Meyskens FL Jr, Omenn GS, Valanis B, Williams JH Jr (2004) The beta-carotene and retinol efficacy trial: incidence of lung cancer and cardiovascular disease mortality during 6-year follow-up after stopping beta-carotene and retinol supplements. J Natl Cancer Inst 96(23):1743–1750
West KP Jr, Christian P, Labrique AB, Rashid M, Shamim AA, Klemm RD, Massie AB, Mehra S, Schulze KJ, Ali H, Ullah B, Wu LS, Katz J, Banu H, Akhter HH, Sommer A (2011) Effects of vitamin A or beta carotene supplementation on pregnancy-related mortality and infant mortality in rural Bangladesh: a cluster randomized trial. JAMA 305(19):1986–1995
Stephens NG, Parsons A, Schofield PM, Kelly F, Cheeseman K, Mitchinson MJ (1996) Randomised controlled trial of vitamin E in patients with coronary disease: Cambridge Heart Antioxidant Study (CHAOS). Lancet 347(9004):781–786
GISSI (1999) Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto miocardico Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction: results of the GISSI-Prevenzione trial. Lancet 354(9177):447–455
Yusuf S, Dagenais G, Pogue J, Bosch J, Sleight P (2000) Vitamin E supplementation and cardiovascular events in high-risk patients. The heart outcomes prevention evaluation study investigators. N Engl J Med 342(3):154–160
Lee IM, Cook NR, Gaziano JM, Gordon D, Ridker PM, Manson JE, Hennekens CH, Buring JE (2005) Vitamin E in the primary prevention of cardiovascular disease and cancer: the women’s health study: a randomized controlled trial. JAMA 294(1):56–65
Miller ER 3rd, Pastor-Barriuso R, Dalal D, Riemersma RA, Appel LJ, Guallar E (2005) Meta-analysis: high-dosage vitamin E supplementation may increase all-cause mortality. Ann Intern Med 142(1):37–46
Qiao YL, Dawsey SM, Kamangar F, Fan JH, Abnet CC, Sun XD, Johnson LL, Gail MH, Dong ZW, Yu B, Mark SD, Taylor PR (2009) Total and cancer mortality after supplementation with vitamins and minerals: follow-up of the Linxian General Population Nutrition Intervention Trial. J Natl Cancer Inst 101(7):507–518
Clemons TE, Kurinij N, Sperduto RD (2004) AREDS Research Group. Associations of mortality with ocular disorders and an intervention of high-dose antioxidants and zinc in the age-related eye disease. Arch Ophthalmol 122(5):716–726
Zhang SM, Cook NR, Albert CM, Gaziano JM, Buring JE, Manson JE (2008) Effect of combined folic acid, vitamin B6, and vitamin B12 on cancer risk in women: a randomized trial. JAMA 300(17):2012–2021
Clark LC, Combs GF Jr, Turnbull BW, Slate EH, Chalker DK, Chow J, Davis LS, Glover RA, Graham GF, Gross EG, Krongrad A, Lesher JL Jr, Park HK, Sanders BB Jr, Smith CL, Taylor JR (1996) Effects of selenium supplementation for cancer prevention in patients with carcinoma of the skin. A randomized controlled trial. Nutritional Prevention of Cancer Study Group. JAMA 25; 276(24):1957–1963
Stranges S, Marshall JR, Trevisan M, Natarajan R, Donahue RP, Combs GF, Farinaro E, Clark LC, Reid ME (2006) Effects of selenium supplementation on cardiovascular disease incidence and mortality: secondary analyses in a randomized clinical trial. Am J Epidemiol 163(8):694–699
Hercberg S, Kesse-Guyot E, Druesne-Pecollo N, Touvier M, Favier A, Latino-Martel P, Briançon S, Galan P (2010) Incidence of cancers, ischemic cardiovascular diseases and mortality during 5-year follow-up after stopping antioxidant vitamins and minerals supplements: a post-intervention follow-up in the SU.VI.MAX study. Int J Cancer 127(8):1875–1881
Heart Protection Study Collaborative Group (2002) MRC/BHF Heart Protection Study of antioxidant vitamin supplementation in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet 360(9326):23–33
Albanes D, Heinonen OP, Taylor PR, Virtamo J, Edwards BK, Rautalahti M, Hartman AM, Palmgren J, Freedman LS, Haapakoski J, Barrett MJ, Pietinen P, Malila N, Tala E, Liippo K, Salomaa ER, Tangrea JA, Teppo L, Askin FB, Taskinen E, Erozan Y, Greenwald P, Huttunen JK (1996) Alpha-tocopherol and beta-carotene supplements and lung cancer incidence in the alpha-tocopherol, beta-carotene cancer prevention study: effects of base-line characteristics and study compliance. J Natl Cancer Inst 88(21):1560–1570
Woodson K, Stewart C, Barrett M (1999) Effect of Vitamin Intervention on the relationship between GSTM1, smoking, and lung cancer risk among male smokers. Cancer Epidemiol Biomarkers Prev 8:965–970
Virtamo J, Edwards BK, Virtanen M, Taylor PR, Malila N, Albanes D, Huttunen JK, Hartman AM, Hietanen P, Mäenpää H, Koss L, Nordling S, Heinonen OP (2000) Effects of supplemental alpha-tocopherol and beta-carotene on urinary tract cancer: incidence and mortality in a controlled trial (Finland). Cancer Causes Control 11(10):933–939
Virtamo J, Pietinen P, Huttunen JK, Korhonen P, Malila N, Virtanen MJ, Albanes D, Taylor PR, Albert P, ATBC Study Group (2003) Incidence of cancer and mortality following alpha-tocopherol and beta-carotene supplementation: a postintervention follow-up. JAMA 290(4):476–485
Omenn GS, Goodman GE, Thornquist MD, Balmes J, Cullen MR, Glass A, Keogh JP, Meyskens FL, Valanis B, Williams JH, Barnhart S, Hammar S (1996) Effects of a combination of β-carotene and vitamin A on lung cancer and cardiovascular disease. N Engl J Med 334(18):1150–1155
Neuhouser ML, Barnett MJ, Kristal AR, Ambrosone CB, King IB, Thornquist M, Goodman GG (2009) Dietary supplement use and prostate cancer risk in the Carotene and Retinol Efficacy Trial. Cancer Epidemiol Biomarkers Prev 18(8):2202–2206
Lee IM, Cook NR, Gaziano JM, Gordon D, Ridker PM, Manson JE, Hennekens CH, Buring JE (2005) Vitamin E in the primary prevention of cardiovascular disease and cancer: the women’s health study: a randomized controlled trial. JAMA 294(1):56–65
Druesne-Pecollo N, Latino-Martel P, Norat T, Barrandon E, Bertrais S, Galan P, Hercberg S (2010) Beta-carotene supplementation and cancer risk: a systematic review and metaanalysis of randomized controlled trials. Int J Cancer 127(1):172–184
Fritz H, Kennedy D, Fergusson D, Fernandes R, Doucette S, Cooley K, Seely A, Sagar S, Wong R, Seely D (2011) Vitamin A and retinoid derivatives for lung cancer: a systematic review and meta analysis. PLoS ONE 6(6):e21107
Jeon YJ, Myung SK, Lee EH, Kim Y, Chang YJ, Ju W, Cho HJ, Seo HG, Huh BY (2011) Effects of beta-carotene supplements on cancer prevention: meta-analysis of randomized controlled trials. Nutr CancerNov 63(8):1196–1207
Gaziano JM, Glynn RJ, Christen WG, Kurth T, Belanger C, MacFadyen J, Bubes V, Manson JE, Sesso HD, Buring JE (2009) Vitamins E and C in the prevention of prostate and total cancer in men: the physicians’ health study II randomized controlled trial. JAMA 301(1):52–62
Klein EA, Thompson IM Jr, Tangen CM, Crowley JJ, Lucia MS, Goodman PJ, Minasian LM, Ford LG, Parnes HL, Gaziano JM, Karp DD, Lieber MM, Walther PJ, Klotz L, Parsons JK, Chin JL, Darke AK, Lippman SM, Goodman GE, Meyskens FL Jr, Baker LH (2011) Vitamin E and the risk of prostate cancer: the Selenium and Vitamin E Cancer Prevention Trial (SELECT). JAMA 306(14):1549–1556
Bjelakovic G, Nikolova D, Simonetti RG, Gluud C (2008) Antioxidant supplements for preventing gastrointestinal cancers. Cochrane Database Syst Rev 16(3):CD004183
Papaioannou D, Cooper KL, Carroll C, Hind D, Squires H, Tappenden P, Logan RF (2011) Antioxidants in the chemoprevention of colorectal cancer and colorectal adenomas in the general population: a systematic review and meta-analysis. Colorectal Dis 13(10):1085–1099
Duffield-Lillico AJ, Reid ME, Turnbull BW, Combs GF Jr, Slate EH, Fischbach LA, Marshall JR, Clark LC (2002) Baseline characteristics and the effect of selenium supplementation on cancer incidence in a randomized clinical trial: a summary report of the Nutritional Prevention of Cancer Trial. Cancer Epidemiol Biomarkers Prev 11(7):630–639
Fritz H, Kennedy D, Fergusson D, Fernandes R, Cooley K, Seely A, Sagar S, Wong R, Seely D (2011) Selenium and lung cancer: a systematic review and meta analysis. PLoS One 6(11):e26259
Taylor PR, Li Bing, Dawsey Sanford M, Li Jun-Yao, Yang Chung S, Guo Wande, Blot William J (1994) Linxian Nutrition Intervention Trials Study Group Prevention of Esophageal Cancer: the Nutrition Intervention in Linxian, China. Cancer Res 54(suppl.):2029 s–2031 s
Lin J, Cook NR, Albert C, Zaharris E, Gaziano JM, Van Denburgh M, Buring JE, Manson JE (2009) Vitamins C and E and beta carotene supplementation and cancer risk: a randomized controlled trial. J Natl Cancer Inst 101(1):14–23
Zhang SM, Cook NR, Albert CM, Gaziano JM, Buring JE, Manson JE (2008) Effect of combined folic acid, vitamin B6, and vitamin B12 on cancer risk in women: a randomized trial. JAMA 300(17):2012–2021
Myung SK, Ju W, Kim SC (2011) Korean Meta-analysis (KORMA) Study Group. Vitamin or antioxidant intake (or serum level) and risk of cervical neoplasm: a meta-analysis. BJOG 118(11):1285–1291
Bjelakovic G, Nikolova D, Gluud LL, Simonetti RG, Gluud C (2010) Antioxidant supplements for prevention of mortality in healthy participants and patients with various diseases. The Cochrane Collaboration, issue 1, Wiley, New York
Omenn GS, Goodman GE, Thornquist MD, Balmes J, Cullen MR, Glass A, Keogh JP, Meyskens FL, Valanis B, Williams JH, Barnhart S, Hammar S (1996) Effects of a combination of β-carotene and vitamin A on lung cancer and cardiovascular disease. N Engl J Med 334(18):1150–1155
Blot WJ, Li J-Y, Taylor PR, Guo W, Dawsey S, Wang G-Q, Yang CS, Zheng S-F, Gail M, Li G-Y, Yu Y, Liu B-Q, Tangrea J, Sun Y-H, Liu F, Fraumeni JF, Zhang Y-H, Li B (1993) Nutrition intervention trials in Linxian, China: supplementation with specific vitamin/mineral combinations, cancer incidence, and disease specific mortality in the general population. J Natl Cancer Inst 85:1483–1492
The α-Tocopherol and β-Carotene Cancer Prevention Study Group (1994) The effect of vitamin E and β-carotene on the incidence of lung cancer and other cancers in male smokers. New Engl J Med 330:1029–1035
Raj L, Ide T, Gurkar AU, Foley M, Schenone M, Li X, Tolliday NJ, Golub TR, Carr SA, Shamji AF, Stern AM, Mandinova A, Schreiber SL, Lee SW (2011) Selective killing of cancer cells by a small molecule targeting the stress response to ROS. Nature 475(7355):231–234
Miller RA, Harrison DE, Astle CM, Baur JA, Boyd AR, de Cabo R, Fernandez E, Flurkey K, Javors MA, Nelson JF, Orihuela CJ, Pletcher S, Sharp ZD, Sinclair D, Starnes JW, Wilkinson JE, Nadon NL, Strong R (2011) Rapamycin, but not resveratrol or simvastatin, extends lifespan of genetically heterogeneous mice. J Gerontol A Biol Sci Med Sci 66(2):191–201
Dipartimento Sanita’ Pubblica Veterinaria, Sicurezza Alimentare E Organi Collegiali Per La Tutela Della Salute. Direzione Generale Igiene E Sicurezza Degli Alimenti E Della Nutrizione Commissione Unica Per La Dietetica E La Nutrizione. Uso Di Prodotti Naturali Come Tisane Ed Integratori Alimentari Da Parte Dei Gruppi Più Vulnerabili Della Popolazione Come Bambini E Donne In Gravidanza O Durante L’allattamento. Ministero Della Salute, Rome, Italy, 2012
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dolara, P., Bigagli, E. & Collins, A. Antioxidant vitamins and mineral supplementation, life span expansion and cancer incidence: a critical commentary. Eur J Nutr 51, 769–781 (2012). https://doi.org/10.1007/s00394-012-0389-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-012-0389-2