Abstract
Purpose
Red yeast rice (RYR), sugar cane-derived policosanols (SCdP) and artichoke leaf extracts (ALEs) are currently incorporated alone or in combination into dietary supplements for their potential low-density-lipoprotein cholesterol (LDL-cholesterol)-lowering effects. Yet, there is no information supporting the efficacy of this association on the reduction in LDL-cholesterol. The main objective of this study was to investigate the effects of a new dietary supplement (DS) with RYR, SCdP and ALEs on LDL-cholesterol.
Methods
In a double-blind, randomized, parallel controlled study, 39 subjects from 21 to 55 years with moderate hypercholesterolemia without drug treatment were assigned to 2 groups and then consumed either a DS containing RYR, SCdP and ALEs or a placebo over a 16-week period. Plasma concentrations of lipids [LDL-cholesterol, total cholesterol (TC), high-density-lipoprotein cholesterol (HDL-cholesterol), triacylglycerols (TG)] and plasma levels of vitamins C and E, total polyphenols and malondialdehyde were determined at baseline and after 4, 8, 12 and 16 weeks.
Results
LDL-cholesterol and TC were reduced by, respectively, 21.4 % (95 % CI, −13.3 to −24.9 %, p < 0.001) and 14.1 % (95 % CI, −10.1 to −18.0 %, p < 0.001) at week 16 in the DS group compared with baseline. Similar results were obtained at weeks 4, 8 and 12. TG decreased by 12.2 % after 16 weeks in the DS group (95 % CI: −24.4 to −0.1 %, p < 0.05). For the vitamin E/TC ratio, a difference was observed between groups at week 16 (p < 0.05). Other parameters were not modified.
Conclusions
Daily consumption of this new DS decreased LDL-cholesterol and TC and is therefore an interesting, convenient aid in managing mild to moderate hypercholesterolemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epidemiological data have clearly shown that elevated plasma levels of low-density-lipoprotein cholesterol (LDL-C) increase the risk of cardiovascular diseases. Lowering LDL-C plasma levels (by dietary modification or drugs) would generally reduce the risk of cardiovascular events in both primary and secondary prevention [1]. In recent meta-analyses, it was calculated that the cardiovascular risk was reduced by 20 % for each 1 mmol L−1 of LDL-C reduction, regardless of the therapy [2, 3].
Data obtained from various countries have shown that the primary aim of studies has been to match the intensity of LDL-C-lowering therapy with absolute risk of cardiovascular diseases (CVD). Firstly, anyone with an elevated LDL-C was advised lifestyle changes, which, when followed, generally proved effective in lowering LDL-C levels. People at relatively high risk of CVD were also candidates for drug treatment, which proved very effective [4] but engendered significant additional expenses. Therapeutic lifestyle changes include dietary changes, particularly a reduction in saturated fat and cholesterol consumption, increased intake of fruits and vegetables, and moderate physical activity. The use of food additives such as phytosterols/stanols and dietary supplements is also suggested, and in fact, their use is becoming increasingly popular [5]. Nevertheless, if different guidelines advise consumption of phystosterols/stanols as a further option for decreasing LDL-C [6], the use of dietary supplements is controversial and only a few have withstood the rigors of randomized controlled trials [7].
Several plant extracts have also been tested for their potential LDL-C-lowering effect including red yeast rice (RYR), sugar cane-derived policosanols (SCdP) or artichoke leaf extracts (ALEs).
Numerous clinical studies performed in hyperlipidemic subjects have shown a beneficial effect of RYR extract supplements [8] resulting in a decrease in plasma total cholesterol (TC), LDL-C and triacylglycerols (TG) [3, 9–11]. In some cases, an increase of high-density-lipoprotein cholesterol (HDL-C) was also demonstrated [12]. RYR is a medicinal agent used by the Chinese and made from Monascus purpureus with rice. Depending on the Monascus strains use and the conditions of fermentation, they may contain polyketides called monacolins [13]. Monacolin K is pharmaceutically known as Lovastatin®, commonly prescribed as a lipid-lowering drug.
Sugar cane-derived policosanols have shown beneficial effects in patients with hyperlipidemia. A data review and a meta-analysis also revealed a more favorable action of policosanols on serum lipids compared with phytosterols and stanols, and an equivalent effect to statins [14, 15]. However, most of these clinical studies were conducted in Cuba by the same group of researchers.
Some clinical trials on ALEs have shown a beneficial effect on cholesterol levels, but the evidence is not yet convincing [16].
One consequence of high LDL-C levels results from its oxidation. Oxidized LDL-cholesterol [17, 18] and lipid peroxidation products [19, 20] are found in elevated concentrations in atherosclerotic plaques and are thought to play an important role in the development and progression of atherosclerosis. Intake of antioxidants such as vitamin E and pro-anthocyanidin oligomers appears to be interesting in limiting plasma cholesterol oxidation. It has been shown that men and women supplemented with daily doses exceeding 100 IU of vitamin E for over 2 years showed a significant reduction in heart attacks [21–23].
Based on this evidence, we decided to test a new dietary supplement containing RYR, SCdP, ALEs, oligomers procyanidins and vitamin E on blood lipid profiles and systemic oxidative stress in untreated subjects with moderate hypercholesterolemia.
The primary objective of this randomized, placebo-controlled trial was to evaluate whether this dietary supplement can lower LDL-C after a 16-week treatment. Secondary aims include measurements of several parameters: LDL-C after 4, 8 and 12 weeks supplementation, TC, HDL-C, TG, fasting plasma glucose, blood pressure, vitamins E and C, total polyphenols, malondialdehyde and safety parameters (aspartame aminotransferase, alanine aminotransferase, alkaline phosphatase, and conjugated bilirubin).
Subjects and methods
Trial design
This was a mono-centric, double-blind, placebo-controlled, parallel-group study conducted in France. It was conducted by the CIC (Centre d’Investigation Clinique, Hôpital de la Conception, Marseille, France) and performed according to Good Clinical Practice. This clinical trial was approved by the South I Mediterranean Committee for Human Research and the French Health Products Safety Agency (2008-A01169-46). Procedures followed were in accord with the ethical standards of the Helsinki Declaration of 1975 as revised in 1983. The study protocol was also registered at clinicaltrials.gov under the number NCT01354327.
Subjects
Thirty-nine healthy male and female volunteers with moderate untreated hypercholesterolemia were recruited from the Marseille area (France) between December 2008 and December 2009 via newspaper advertisements or were selected from the study center’s (Centre d’Investigation Clinique, Hôpital de la Conception, Marseille, France) volunteer database. Inclusion criteria were as follows: male or female aged 18–55 years with a body mass index ≥18.5 and <27.5 kg m−2, non or light smoker (<10 cigarettes/day); subjects with stable weight, eating patterns and physical activity during the 3 months preceding the start of the protocol, and agreeing to maintain these habits during the study; a plasma TC concentration >5.68 mmol L−1; for premenopausal women: non-estrogen contraceptive taken for at least 2 cycles preceding the start of the study, agreeing not to change during the protocol; postmenopausal women with no estrogen replacement therapy. Other requirements for inclusion were the express desire to participate during the entire duration of the trial and the subject’s written informed consent. Exclusion criteria included the following: previous or current use of lipid-lowering therapies; diabetes treated or detected at the inclusion visit; severe chronic diseases; severe medical conditions that could interfere with the study, such as digestive tract surgery; uncontrolled hypertension (systolic blood pressure >160 mmHg and diastolic blood pressure >90 mmHg; a fasting glycemia level >1.2 g L−1; an aspartate aminotransferase (AST) level >40 UI L−1; an ALanine aminoTransferase (ALT) level >45 UI L−1; a gamma-glutamyl transpeptidase (γGT) level >5 μmol L−1; a conjugated bilirubin level >5 μmol L−1; an alkaline phosphatase level >100 UI L−1; a hemoglobin A1c level >6 %; pregnant or lactating women and those trying to get pregnant; dietary supplements or functional food consumption (e.g., sterols, stanols and n-3 fatty acids products); any medical treatment that, according to the investigators, might interfere with the outcome measures; vegetarian or vegan subjects; subjects with extreme eating habits and/or with a significant history of anorexia nervosa, bulimia and other eating disorders; known or suspected food allergies, related to the compounds of the food supplement; subjects consuming more than 2 alcoholic beverages per day (every day). All subjects were advised of the potential side effects of the study medication. Participants gave their written informed consent before the beginning of the trial.
Trial protocol
The participants were screened for eligibility first through a phone call. All potential candidates underwent a pre-screening visit during which the inclusion/exclusion criteria were detailed, the study explained and the procedures to be followed laid out. The study coordinator answered any questions posed by the subjects, and their written informed consent was obtained. Thereafter, a medical examination, a general health questionnaire and blood samples were performed to confirm eligibility. Eligible subjects were randomly assigned to take either the placebo (PLA) or dietary supplement (DS). The block randomization schedule was performed using SAS® programming (SAS®9.1.). The study coordinator assigned the participants to the supplement specified by the schedule in the chronological order they joined. Assignments into each study group remained concealed until all enrolments were completed.
Study assessments took place 1 week before starting the medication, at baseline and at weeks 4, 8, 12 and 16. The study participants were asked to maintain their usual dietary habits and not to change their food selections or exercise in order not to modify their lipid concentrations. To check diet stability, the subjects were instructed to record their food intake for 3 successive days just after baseline and 3 days before weeks 4, 8, 12 and 16. To help them do this, they were given an instruction booklet with an example day menu. Moreover, the participants were helped to complete their intake diary at baseline with a dietician. Food diary records were analyzed using Nutrilog® 2.10 software. Data analyses were as follows: total energy (kcal day−1), total protein (g day−1), total carbohydrate (g day−1), total fat (g day−1), saturated fatty acids (g day−1), monounsaturated fatty acids (g day−1), polyunsaturated fatty acids (g day−1), cholesterol (g day−1), percentage energy from fats, carbohydrates and proteins, soluble and insoluble fibers (g day−1), vitamin E (mg day−1), vitamin C (mg day−1), total polyphenols (mg day−1) and carotenoids (mg day−1).
The subjects were asked not to consume any food supplements or functional foods during the study, as well as not to modify their medical treatment or start any new one unless necessary. All their control visits included a clinical examination, and blood samples were taken after a 12-h overnight fast. Compliance with the products was established by calculation, considering packages distributed at baseline, week 4, week 8 and week 12 and those returned at weeks 4, 8, 12 and 16. The volunteers reported adverse events and eventual concomitant treatments by filling in a questionnaire during each visit. TC, LDL-C, HDL-C, TG, fasting glycemia and blood pressure were determined at all visits. Vitamins C and E, total polyphenols and MalonDiAldehyde (MDA) were measured at baseline, week 8 and week 16. AST, ALT, γGT, conjugated bilirubin and alkaline phosphatase were measured at baseline and week 16.
Endpoints
The primary outcome was the change in the concentration of plasma LDL-C between baseline and week 16 in the DS group. Secondary endpoints were as follows: LDL-C at weeks 4, 8 and 12; TC, HDL-C, TG, fasting glycemia and blood pressure at all visits; vitamins C and E, total polyphenols and MDA at baseline, week 8 and week 16; AST, ALT, γGT, conjugated bilirubin and alkaline phosphatase at baseline and week 16.
Products
The participants were asked to take 3 tablets of PLA or DS daily (1 tablet 3 times a day during meals). The dietary supplement (Limicol®, Laboratoire Lescuyer, Aytré, France) was composed of the following compounds (per tablet): red yeast rice 166.67 mg (0.4 % monacolin K), sugar cane extract 3.70 mg (90 % policosanols–octacosanol 60 %), artichoke leaf dry extract 200 mg (5–6 % chlorogenic acid), garlic dry extract 10 mg (0.8 % allicin, 1.8 % alliin), pine bark extract 6.67 mg (90 % oligomeric proanthocyanidins), vitamins E 12.86 mg, B2 1.60 mg, B3 (inositol hexanicotinate) 2.92 mg, dicalcium phosphate 199 mg, microcrystalline cellulose 87.36 mg, calcium citrate 63.22 mg, tricalcium phosphate 34 mg and magnesium stearate 22 mg. The PLA composition was as follows (per tablet): dicalcium phosphate 250 mg, microcrystalline cellulose 242.50 mg, maltodextrin 105 mg, calcium citrate 65 mg, tricalcium phosphate 58 mg, beet powder 47.50 mg and magnesium stearate 22 mg. The dietary supplement and the PLA were produced by an ISO 22000-certified laboratory. Moreover, as part of the quality control process, an independent laboratory (NOVEAL Laboratoire Services, Valanjou, France) was commissioned to verify the composition of the DS.
Determination of plasma lipids
Blood samples were collected in vacutainer tubes. Plasma TC, HDL-C and TG concentrations were measured using a DxC Beckman Coulter by enzymatic methods using a cholesterol oxidase method (synchron CHOL) for TC, a direct homogeneous method (synchron HDLd) for HDL-C and a lipase/glycerol kinase method (synchron TG GPO) for TG. The LDL subfraction was indirectly quantified using the Friedewald equation [24].
Determination of safety parameters and fasting glycemia
ASpartate aminoTransferase and ALanine aminoTransferase concentrations were evaluated using an automated Synchron DxC Beckman Coulter according to the International Federation of Clinical Chemistry (IFCC) procedure with the addition of pyridoxal phosphate at 37 °C (Beckman Coulter Inc., Fullerton, CA, USA). Alkaline phosphatase concentrations were measured using automated Synchron DxC Beckman Coulter with p-nitrophenylphosphate (p-NPP) buffer and AMP (Beckman Coulter Inc., Fullerton, CA, USA). Direct bilirubin concentrations were evaluated using automated Synchron DxC Beckman Coulter and the diazotized sulfanilic acid procedure (Beckman Coulter Inc., Fullerton, CA, USA).
Plasma glucose concentrations were determined by a hexokinase method using a Synchron DxC Beckman Coulter. Finally; HbA1c concentrations were evaluated on a HPLC Variant II analyzer equipped with the new kit 270-2101 NU (Bio-Rad Laboratories, Hercules, CA, USA).
Determination of plasma vitamins C and E, total polyphenols and MDA
Vitamin C and total polyphenols were extracted together from the plasma samples. To 1,100 μL of the plasma sample, 250 μL of 25 % TCA and 250 μL of acetone were added. After a 10-min centrifugation at 13,000 rpm (4 °C), 250 μL of H2O was added to the supernatants.
Folin–Ciocalteu’s reagent was used for the colorimetric measurements of polyphenolic antioxidants. The color produced is proportional to the amount of polyphenols present in the sample (maximum absorption at 760 nm). Briefly, 250 μL of H2O and 2.5 mL of Folin reagent (diluted 1/10) were added to 250 μL of the polyphenolic sample extract. After vortex and a 2-min incubation at room temperature, 2 mL of sodium carbonate (75 g L−1) was added. After an additional 5 min of incubation at 50 °C, optical density of the samples was determined at 760 nm. The amounts of polyphenols present were expressed as gallic acid equivalents (GAE). Ascorbic acid was oxidized to dehydroascorbic acid (DHA). This method is based on the rapid, specific reaction of DHA with o-phenylendiamine (OPDA) to form a fluorescent quinoxine derivative (FQD) that is quantified by HPLC. Briefly, 140 μL of sodium acetate (pH 6.2) and a spatula of ascorbate oxidase were added to 1 mL of the extraction of samples containing ascorbic acid. After incubation for 8 min at 37 °C, the ascorbate oxidase was removed and 170 μL of OPDA were added. After incubation for 30 min at 37 °C and filtration (0.45 μm), FQD was quantified by HPLC coupled to a fluorimeter (Exc: 350 nm–Em: 430 nm).
Plasma vitamin E was determined using HPLC coupled to a UV–visible spectrometer. To 500 μL of sample, 3 mL of a mix of hexane, acetone, ethanol and BHT, 20 μL of 8′-apocarotenal (internal standard) and 1 mL of H2O were added. This was vortexed for 5 min and centrifuged at 13,000 rpm for 50 min at 4 °C. The supernatant was collected and evaporated under nitrogen before being taken up in 300 μL of methanol/MTBE.
Samples were analyzed by reverse-phase HPLC using a HP 1100 system equipped with a quaternary pump, an autosampler and a fluorimeter. Separation was achieved using an Atlantis dC 18 150 × 4.6 mm column (Waters, Saint-Quentin-en-Yvelines, France). The mobile phase consisted of methanol, and acetonitrile and was run at a flow rate of 1 mL min−1. Initial composition was methanol/acetonitrile (65/35; v/v), and methanol was decreased to 23 % over a 30-min period. Alpha-tocopherol was detected at 4.3 min and quantified by fluorimetry (lambda excitation = 295 nm, lambda emission = 330 nm).
The measurement of plasma MDA was performed by the method of thiobarbituric acid reactive substances (TBARS). One millilitre of water containing 15 % trichloroacetic acid (TCA) and 0.375 % thiobarbituric acid (TBA) was added to 500 μL of plasma. After 50 min of incubation at 100 °C and cooling in iced water, the samples were centrifuged for 10 min at 1,200g at 4 °C. The absorbance was then read in a spectrophotometer at 535 nm. Calibration was performed with an external calibration of TEP (1,1,3,3-tetramethoxypropane) for the range 0.005–2.5 μg mL−1 following the same protocol.
Statistical methods
The results are presented as mean values ± standard deviation (SD). No sample size calculation was performed prior to the study. Statistical distribution of all variables of interest was approximately Gaussian. Between-treatment comparisons were done to verify that randomization had produced sufficiently homogenous groups. The average difference in LDL-C and other variables in the 2 treatment arms (PLA and DS) before and after 4, 8, 12 and 16 weeks of supplementation were assessed with a Student’s t test. The within-group change in LDL-C and other variables from baseline to study completion were assessed with paired t tests. For plasma antioxidants and MDA levels, analyses were based on the per-protocol principle. Other analyses were based on the intention-to-treat principles. SAS® software version 9.1 was used for the statistical analysis. A level of significance was set at 0.05 for all cases.
Results
Subject participation throughout the study
Thirty-nine healthy (20 PLA and 19 DS) moderately hypercholesterolemic subjects of the 88 potential subjects met the entry requirements and were enrolled in the study. Thirty-five (18 PLA and 17 DS) of the participants completed the study, with 2 dropouts in the PLA group and 2 in the DS group (Fig. 1).
Safety and tolerance
The study found that the dietary supplement was as well tolerated as the PLA with no adverse events occurring in either group during the study. No significant changes in our safety measurements were noted either before or after treatment (data not shown).
Compliance
Compliance with the study treatments was 91.3 % in the PLA and 92.5 % in the DS groups.
Baseline characteristics
Basal anthropometric and clinical characteristics are shown in Table 1. Most of our participants were women and coincidentally were evenly allocated to the two groups (PLA group: 5 men and 15 women; DS group: 6 men and 13 women). No significant differences in the anthropometric, lipid variables or body mass index values were observed between the groups. Only systolic blood pressure was significantly different in the DS group (117.1 ± 9.5 vs. 110.0 ± 9.1 mmHg, p = 0.023) compared with PLA. Neither was any significant difference in antioxidant status or lipid peroxidation, as measured by MDA levels, observed at baseline between the groups.
Analysis of food records showed no significant difference in food intake between the two groups at baseline (Table 2). Moreover, statistical analysis of the monthly food surveys showed no difference in food habits in either group between the beginning and the end of the study (data not shown). Inspection of the subjects’ diaries did not indicate any deviations from the protocol that may have affected the results.
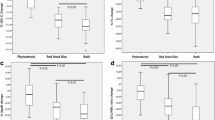
Plasma lipid profile
The mean plasma lipid concentrations at baseline and after 4, 8, 12 and 16 weeks’ supplementation with the PLA or DS are shown in Table 3. The ITT analysis showed that subjects who took three DS tablets daily showed significantly decreased LDL-C by 21.4 ± 9.8 % (p < 0.001) after 4 weeks, with this then stabilizing over the remaining study period to reach −19.1 ± 12.0 % (p < 0.001) at the end of the study. No significant change was observed in the PLA group (−2.2 ± 18.1 at week 4, p = 0.59, and +2.8 ± 13.7 % at week 16, p = 0.37, compared with baseline).
A significant decrease in TC was observed in the DS group (−15.3 ± 9.3 % after 4 weeks, p < 0.001, and stabilized at −14.1 ± 8.1 % at the end, p < 0.001, as compared with baseline). No significant changes appeared in the PLA group (+1.3 ± 8.8 % at week 16 compared with baseline, p = 0.53). In contrast, HDL-C levels remained the same in both groups (week 16 compared at baseline: PLA, +2.0 ± 18.1 %, p = 0.62; DS, −0.3 ± 11.4 %, p = 0.90). Finally, TG concentrations significantly decreased at week 16 compared with baseline in the DS group (−12.2 ± 25.4 %, p < 0.05) although there was a general increase in these values in the PLA group.
Antioxidant profile
Table 4 shows the antioxidant vitamins E and C, and polyphenols concentrations at baseline and after 8 and 16 weeks of supplementation, as well as the plasma MDA concentrations. No changes in vitamins C and E plasma levels were observed in the course of the current study. However, when we calculated the vitamin E/TC ratio, a significant difference was observed between groups at week 16 (PLA, 12.7 ± 3.0 vs. DS, 15.3 ± 4.1, p = 0.038). A significant increase in plasma concentrations of polyphenols was observed in both groups (PLA, +20.7 % and DS, +12.6 %, p < 0.05) at the end of study compared with baseline. Finally, the oxidation of lipids, determined by the extent of MDA, showed no differences either within or between groups.
Discussion
The role of nutrition in the prevention of CVD has been extensively reviewed [25, 26]. There is strong evidence showing that dietary factors may influence atherogenesis directly or through effects on traditional risk factors such as lipid levels, blood pressure or glucose levels [27]. Dietary supplements and functional foods can be used either as alternatives or in addition to lipid-lowering drugs [28]. The use of dietary supplements for the management of dyslipidemias is mentioned in the European Society of Cardiology/European Atherosclerosis Society guidelines in the chapter of lifestyle modifications [27]. They concluded that policosanols were not effective and that the efficacy of RYR was less established by evidence/opinion.
In the present randomized controlled study, we evaluated the beneficial effect of a new dietary supplement based on plant extracts (containing, among other components, RYR, SCdP, ALEs, oligomeric procyanidins and vitamin E) on blood lipid profiles and systemic oxidative stress. The effects of the dietary supplement on lipids were independent of the diet as both groups showed no difference in caloric and lipid intake during the protocol.
The principal component, RYR, has been studied for its potential interest in cholesterol management. RYR extract contains monacolin K (also known as lovastatin®), which acts by inhibiting 3-Hydroxy-3-MethylGlutaryl Coenzyme A (HMG-CoA) reductase [29]. Several trials have investigated RYR efficacy in the treatment of hypercholesterolemic patients, and a consistent LDL-C decrease (22–27 %) has been demonstrated [8–10, 30, 31], in both adults and hypercholesterolemic children [32]. Our results, although not radically different, were slightly below those obtained in other studies. This may be explained by the daily amount of monacolin K used. We administered a daily dose of 2 mg while these other studies used between 3 and 9 mg per day [12]. This is also true for the decrease in TC concentrations.
Concerning sugar cane-derived policosanols, several studies have shown beneficial effects after supplementation in patients with hyperlipidemia. A daily intake of 10-40 mg has shown a significant decrease in plasma TC concentrations, LDL-C and TG with increases in the plasma concentrations of HDL-C [33–36]. The beneficial effects of policosanols in the prevention of atherosclerosis and thromboembolic disorders have been related to the inhibition of sterol biosynthesis possibly by regulating the activity of HMGCoA reductase mediated by AMP-dependent kinase AMPK [37]. However, we did not find any significant difference in HDL-C between the supplemented and PLA groups, either before or after supplementation. The same result was observed by Guardamagna et al. using a combination of RYR (200 mg) and policosanols (10 mg) and by Marazzi et al. [38], using a combination of berberine (500 mg), RYR (200 mg) and policosanols (10 mg) in elderly hypercholesterolemic patients. More recent studies have led to less conclusive results regarding the effectiveness of policosanols [39–41]. The effects of policosanols also remain very controversial.
The potential anti-atheromatous effect of artichoke seemed to be mainly due to two mechanisms: as an antioxidant reducing oxidation of LDL-C and its action on the synthesis of cholesterol. Indeed, one study has shown that artichoke extract reduces cholesterol synthesis by indirectly inhibiting the activity of HMG-CoA reductase [42]. Some clinical studies [43, 44] and a Cochrane review [16] have shown a decrease in blood lipid levels after consumption of an extract of artichoke.
Nevertheless, it is impossible in the present study to distinguish the individual contribution of each of the components (RYR, SCdP and ALEs).
Oxidative stress generated by an imbalance between pro- and antioxidants can lead to the oxidization of molecules such as ADN, proteins and lipids. Experimental studies suggesting that LDL oxidation may be an important process in the development of atherosclerosis have led to the notion that decreasing oxidative stress may help in preventing these diseases or slow their progression [45]. Fruit and vegetable consumption has been shown to protect against CVD in many observational studies [46, 47]. Our subjects did not modify their pattern of consumption during the study period and had an adequate intake of vitamins E and C, coherent with the INCA2 study [48]. Oxidative stress values as measured via the MDA seem lower compared with those usually found in hypercholesterolemics [49] and did not differ between groups either at baseline or after 16 weeks of supplementation. One hypothesis to explain this is that our volunteers, while they were moderately hypercholesterolemic, did not have excessive oxidative stress at baseline, maybe due to sufficient intake of antioxidants. Although the supplementation supplies vitamin E (30 mg day−1), this does not modify plasma oxidative status. This result is in line with Meagher et al. [50] who showed that supplying different doses of vitamin E (200–2,000 UI/day) over an 8-week period did not modulate oxidative stress markers in healthy adults. Finally, even if vitamin E supplements had no impact on plasma oxidative status, nevertheless they permitted the significant increase in the vitamin E/cholesterol ratio in the DS group that became significantly different to the PLA group at week 16, supporting the notion that a higher quantity of vitamin E/lipid particles should result in better protection against lipoperoxidation.
A weakness of this study is represented by the small number of subjects involved. This new dietary supplement with a combination of plant extracts including red yeast rice, sugar cane-derived policosanols and artichoke leaf extracts seems to be satisfactory in terms of efficacy, tolerability and safety as this short-term trial has demonstrated. Present results are interesting and pave the way for future trials.
In conclusion, present results need to be confirmed by more extensive studies to establish whether this combination could represent a good option for the management of mild to moderate hypercholesterolemia in the context of therapeutic lifestyle changes.
References
Wilson PW, Castelli WP, Kannel WB (1987) Coronary risk prediction in adults (the Framingham Heart Study). Am J Cardiol 59:91G–94G
Robinson JG, Smith B, Maheshwari N, Schrott H (2005) Pleiotropic effects of statins: benefit beyond cholesterol reduction? A meta-regression analysis. J Am Coll Cardiol 46:1855–1862
Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, Kirby A, Sourjina T, Peto R, Collins R, Simes R (2005) Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 366:1267–1278
Vondrakova D, Ostadal P, Kruger A (2010) Immediate effect of intensive atorvastatin therapy on lipid parameters in patients with acute coronary syndrome. Lipids Health Dis 9:71
Kelly JP, Kaufman DW, Kelley K, Rosenberg L, Anderson TE, Mitchell AA (2005) Recent trends in use of herbal and other natural products. Arch Intern Med 165:281–286
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (2001) Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 285:2486–2497
Nijjar PS, Burke FM, Bloesch A, Rader DJ (2010) Role of dietary supplements in lowering low-density lipoprotein cholesterol: a review. J Clin Lipidol 4:248–258
Bogsrud MP, Ose L, Langslet G, Ottestad I, Strom EC, Hagve TA, Retterstol K (2010) HypoCol (red yeast rice) lowers plasma cholesterol: a randomized placebo controlled study. Scand Cardiovasc J 44:197–200
Lin CC, Li TC, Lai MM (2005) Efficacy and safety of Monascus purpureus Went rice in subjects with hyperlipidemia. Eur J Endocrinol 153:679–686
Heber D, Yip I, Ashley JM, Elashoff DA, Elashoff RM, Go VL (1999) Cholesterol-lowering effects of a proprietary Chinese red-yeast-rice dietary supplement. Am J Clin Nutr 69:231–236
Huang CF, Li TC, Lin CC, Liu CS, Shih HC, Lai MM (2007) Efficacy of Monascus purpureus Went rice on lowering lipid ratios in hypercholesterolemic patients. Eur J Cardiovasc Prev Rehabil 14:438–440
Liu J, Zhang J, Shi Y, Grimsgaard S, Alraek T, Fonnebo V (2006) Chinese red yeast rice (Monascus purpureus) for primary hyperlipidemia: a meta-analysis of randomized controlled trials. Chin Med 1:4
Heber D, Lembertas A, Lu QY, Bowerman S, Go VL (2001) An analysis of nine proprietary Chinese red yeast rice dietary supplements: implications of variability in chemical profile and contents. J Altern Complement Med 7:133–139
Chen JT, Wesley R, Shamburek RD, Pucino F, Csako G (2005) Meta-analysis of natural therapies for hyperlipidemia: plant sterols and stanols versus policosanol. Pharmacotherapy 25:171–183
Gouni-Berthold I, Berthold HK (2002) Policosanol: clinical pharmacology and therapeutic significance of a new lipid-lowering agent. Am Heart J 143:356–365
Wider B, Pittler MH, Thompson-Coon J, Ernst E (2009) Artichoke leaf extract for treating hypercholesterolaemia. Cochrane Database Syst Rev CD003335
Kaplan M, Aviram M (1999) Oxidized low density lipoprotein: atherogenic and proinflammatory characteristics during macrophage foam cell formation. An inhibitory role for nutritional antioxidants and serum paraoxonase. Clin Chem Lab Med 37:777–787
Toshima S, Hasegawa A, Kurabayashi M, Itabe H, Takano T, Sugano J, Shimamura K, Kimura J, Michishita I, Suzuki T, Nagai R (2000) Circulating oxidized low density lipoprotein levels. A biochemical risk marker for coronary heart disease. Arterioscler Thromb Vasc Biol 20:2243–2247
Bowen PE, Borthakur G (2004) Postprandial lipid oxidation and cardiovascular disease risk. Curr Atheroscler Rep 6:477–484
Romero FJ, Bosch-Morell F, Romero MJ, Jareno EJ, Romero B, Marin N, Roma J (1998) Lipid peroxidation products and antioxidants in human disease. Environ Health Perspect 106(Suppl 5):1229–1234
Losonczy KG, Harris TB, Havlik RJ (1996) Vitamin E and vitamin C supplement use and risk of all-cause and coronary heart disease mortality in older persons: the Established Populations for Epidemiologic Studies of the Elderly. Am J Clin Nutr 64:190–196
Rimm EB, Stampfer MJ, Ascherio A, Giovannucci E, Colditz GA, Willett WC (1993) Vitamin E consumption and the risk of coronary heart disease in men. N Engl J Med 328:1450–1456
Stampfer MJ, Hennekens CH, Manson JE, Colditz GA, Rosner B, Willett WC (1993) Vitamin E consumption and the risk of coronary disease in women. N Engl J Med 328:1444–1449
Friedewald WT, Levy RI, Fredrickson DS (1972) Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18:499–502
Hu FB, Willett WC (2002) Optimal diets for prevention of coronary heart disease. JAMA 288:2569–2578
Mente A, de Koning L, Shannon HS, Anand SS (2009) A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med 169:659–669
Reiner Z, Catapano AL, De Backer G, Graham I, Taskinen MR, Wiklund O, Agewall S, Alegria E, Chapman MJ, Durrington P, Erdine S, Halcox J, Hobbs R, Kjekshus J, Filardi PP, Riccardi G, Storey RF, Wood D, Bax J, Vahanian A, Auricchio A, Baumgartner H, Ceconi C, Dean V, Deaton C, Fagard R, Filippatos G, Funck-Brentano C, Hasdai D, Hoes A, Kearney P, Knuuti J, Kolh P, McDonagh T, Moulin C, Poldermans D, Popescu BA, Sechtem U, Sirnes PA, Tendera M, Torbicki A, Vardas P, Widimsky P, Windecker S, Berkenboom G, De Graaf J, Descamps O, Gotcheva N, Griffith K, Guida GF, Gulec S, Henkin Y, Huber K, Kesaniemi YA, Lekakis J, Manolis AJ, Marques-Vidal P, Masana L, McMurray J, Mendes M, Pagava Z, Pedersen T, Prescott E, Rato Q, Rosano G, Sans S, Stalenhoef A, Tokgozoglu L, Viigimaa M, Wittekoek ME, Zamorano JL (2011) ESC/EAS guidelines for the management of dyslipidaemias: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur Heart J 32:1769–1818
Sirtori CR, Galli C, Anderson JW, Arnoldi A (2009) Nutritional and nutraceutical approaches to dyslipidemia and atherosclerosis prevention: focus on dietary proteins. Atherosclerosis 203:8–17
Endo A (1979) Monacolin K, a new hypocholesterolemic agent produced by a Monascus species. J Antibiot (Tokyo) 32:852–854
Becker DJ, Gordon RY, Halbert SC, French B, Morris PB, Rader DJ (2009) Red yeast rice for dyslipidemia in statin-intolerant patients: a randomized trial. Ann Intern Med 150:830–839
Journoud M, Jones PJ (2004) Red yeast rice: a new hypolipidemic drug. Life Sci 74:2675–2683
Guardamagna O, Abello F, Baracco V, Stasiowska B, Martino F (2011) The treatment of hypercholesterolemic children: efficacy and safety of a combination of red yeast rice extract and policosanols. Nutr Metab Cardiovasc Dis 21:424–429
Reiner Z, Tedeschi-Reiner E, Romic Z (2005) Effects of rice policosanol on serum lipoproteins, homocysteine, fibrinogen and C-reactive protein in hypercholesterolaemic patients. Clin Drug Investig 25:701–707
Castano G, Mas R, Fernandez L, Illnait J, Gamez R, Alvarez E (2001) Effects of policosanol 20 versus 40 mg/day in the treatment of patients with type II hypercholesterolemia: a 6-month double-blind study. Int J Clin Pharmacol Res 21:43–57
Castano G, Fernandez L, Mas R, Illnait J, Mesa M, Fernandez JC (2003) Comparison of the effects of policosanol and atorvastatin on lipid profile and platelet aggregation in patients with dyslipidaemia and type 2 diabetes mellitus. Clin Drug Investig 23:639–650
Prat H, Roman O, Pino E (1999) Comparative effects of policosanol and two HMG-CoA reductase inhibitors on type II hypercholesterolemia. Rev Med Chil 127:286–294
Singh DK, Li L, Porter TD (2006) Policosanol inhibits cholesterol synthesis in hepatoma cells by activation of AMP-kinase. J Pharmacol Exp Ther 318:1020–1026
Marazzi G, Cacciotti L, Pelliccia F, Iaia L, Volterrani M, Caminiti G, Sposato B, Massaro R, Grieco F, Rosano G (2011) Long-term effects of nutraceuticals (berberine, red yeast rice, policosanol) in elderly hypercholesterolemic patients. Adv Ther 28:1105–1113
Francini-Pesenti F, Brocadello F, Beltramolli D, Nardi M, Caregaro L (2008) Sugar cane policosanol failed to lower plasma cholesterol in primitive, diet-resistant hypercholesterolaemia: a double blind, controlled study. Complement Ther Med 16:61–65
Cubeddu LX, Cubeddu RJ, Heimowitz T, Restrepo B, Lamas GA, Weinberg GB (2006) Comparative lipid-lowering effects of policosanol and atorvastatin: a randomized, parallel, double-blind, placebo-controlled trial. Am Heart J 152(982):e981–e985
Berthold HK, Unverdorben S, Degenhardt R, Bulitta M, Gouni-Berthold I (2006) Effect of policosanol on lipid levels among patients with hypercholesterolemia or combined hyperlipidemia: a randomized controlled trial. JAMA 295:2262–2269
Gebhardt R (1998) Inhibition of cholesterol biosynthesis in primary cultured rat hepatocytes by artichoke (Cynara scolymus L.) extracts. J Pharmacol Exp Ther 286:1122–1128
Bundy R, Walker AF, Middleton RW, Wallis C, Simpson HC (2008) Artichoke leaf extract (Cynara scolymus) reduces plasma cholesterol in otherwise healthy hypercholesterolemic adults: a randomized, double blind placebo controlled trial. Phytomedicine 15:668–675
Englisch W, Beckers C, Unkauf M, Ruepp M, Zinserling V (2000) Efficacy of Artichoke dry extract in patients with hyperlipoproteinemia. Arzneimittelforschung 50:260–265
Glass CK, Witztum JL (2001) Atherosclerosis. The road ahead. Cell 104:503–516
Bazzano LA, Serdula MK, Liu S (2003) Dietary intake of fruits and vegetables and risk of cardiovascular disease. Curr Atheroscler Rep 5:492–499
Hung HC, Joshipura KJ, Jiang R, Hu FB, Hunter D, Smith-Warner SA, Colditz GA, Rosner B, Spiegelman D, Willett WC (2004) Fruit and vegetable intake and risk of major chronic disease. J Natl Cancer Inst 96:1577–1584
French Study (2009) Etude individuelle nationale des consommations alimentation: INCA2, AFSSA
Nagila A, Permpongpaiboon T, Tantrarongroj S, Porapakkham P, Chinwattana K, Deakin S, Porntadavity S (2009) Effect of atorvastatin on paraoxonase 1 (PON1) and oxidative status. Pharmacol Rep 61:892–898
Meagher EA, Barry OP, Lawson JA, Rokach J, Fitzgerald GA (2001) Effects of vitamin E on lipid peroxidation in healthy persons. JAMA 285:1178–1182
Acknowledgments
We would like to thank Marion Nowicki and Romain Bott for their expert technical assistance. This work was financed by Laboratoire Lescuyer.
Conflict of interest
Nicolas Ogier, Sébastien L. Peltier and Nicolas Cardinault are employees of the company Laboratoire Lescuyer. Jean-François Lescuyer is the general director of the company. Other authors have no conflicting interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
Trial registration: ClinicalTrials.gov, http://www.clinicaltrials.gov, NCT01354327.
Rights and permissions
About this article
Cite this article
Ogier, N., Amiot, MJ., Georgé, S. et al. LDL-cholesterol-lowering effect of a dietary supplement with plant extracts in subjects with moderate hypercholesterolemia. Eur J Nutr 52, 547–557 (2013). https://doi.org/10.1007/s00394-012-0357-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-012-0357-x