Abstract
Purpose
This study proposes to examine the accuracy of four anthropometric indexes of obesity to identify the presence of hypertension and assess differences in the estimation and strength of effect measures of the association between each anthropometric measure and hypertension in Brazilian adults.
Methods
A population-based cross-sectional study was carried out with a sample of 1,720 adults from Florianópolis, Brazil. Receiver operating characteristic (ROC) curves were performed to identify the sensitivity and specificity of the best cutoff values for anthropometric indexes (body mass index—BMI, waist circumference—WC, waist-to height ratio—WHtR and conicity index—C-index) for prediction of hypertension. The associations between anthropometric indexes and hypertension were analyzed by Poisson regression expressed as Prevalence Ratios (95% CI) adjusted for socio-demographic variables, health behavior, height, and anthropometric indexes.
Results
Of the four anthropometric indexes studied, BMI, WC, and WHtR were found to have the largest areas under the ROC curve relative to hypertension in both sexes. The cutoff values in women and men associated with presence of hypertension were BMI of 24.9 and 24.6 kg/m², WC of 86.2 and 89.5 cm, WHtR of 0.49 and 0.50, and C-index of 1.15 and 1.18, respectively. WC and BMI had greater magnitude of association with presence of hypertension, adjusting for socio-demographic variables, health behavior, height, and anthropometric indexes in women and men, respectively.
Conclusions
Anthropometric indexes provide an effective, simple, inexpensive, and non-invasive means for a first-level screening for hypertension.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The incidence of obesity and obesity-related diseases, particularly hypertension, is increasing worldwide [1]. Between 1980 and 2008, the mean global body mass index (BMI) increased by 0.4–0.5 kg/m² per decade in men and women, reflecting an increase in total body adiposity [2]. During this period, hypertension became a public health problem worldwide. It is associated with chronic diseases such as cardiovascular disease (CVD) and stroke, and it has been widespread in both developing and developed countries [1].
In 1998, the National Heart, Lung, and Blood Institute of the National Institutes of Health (NIH) published evidence-based clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults [3]. These guidelines include a classification system for assessing health risk based on BMI (calculated as weight in kilograms divided by the square of height in meters) and waist circumference (WC). However, some researches have found that BMI and WC were not so accurate for the identification of health risks in certain populations, being affected by height and racial/ethnicity characteristics [4, 5].
Other anthropometric indexes of adiposity have been developed, such as waist-to-height ratio (WHtR), which is able to predict the need of weight management, intra-abdominal fat, cardiovascular risk, and mortality [6, 7]. In a population-based study conducted in the Chinese adult population, WHtR was the best anthropometric index predicting cardiovascular risk factors [8]. Another anthropometric index of obesity with evidence of high accuracy for cardiovascular risk factors is the conicity index (C-index) [9]. In a population-based study conducted in a Brazilian city with a high prevalence of African descent, it was found that the C-index was the anthropometric index that best discriminated high coronary risk [9].
A recent meta-analysis was aimed to determine which simple index of obesity would be the best discriminator of cardiovascular risk factors in adults (hypertension, diabetes, dyslipidemia) [4]. The reported BMI was the poorest discriminator for hypertension. On the other hand, WHtR was the best discriminator for hypertension, diabetes, and dyslipidemia in both sexes. However, criteria of eligibility studies excluded investigations from South America. In addition, it is well known that racial and ethnic characteristics influence the magnitude of the association between obesity index and hypertension, precluding generalization of results of particular studies in Brazil.
The aim of this study was therefore to examine the accuracy of four anthropometric indexes of obesity to identify the presence of hypertension among adults. In addition, the differences in the estimation and strength of effect measures of the association between each anthropometric measure and the presence of hypertension were assessed.
Methods
Study population
A population-based, cross-sectional study was carried out in Florianópolis, Southern Brazil, from September 2009 to January 2010. The city is the capital of the Brazilian State of Santa Catarina; its population is nearly 400,000 inhabitants, with one of Brazil’s highest health and social indicators [10].
This study was part of a comprehensive population survey called EpiFloripa Adults, whose target population included all adults aged 20–59 years who were living in the urban area of the city, accounting for nearly 240,000 inhabitants.
The project was approved by the Ethics Research Committee on Human Beings at the Federal University of Santa Catarina (protocol number 351/08). All participants signed the Free and Cleared Consent Forms giving their consent for participation in the study.
Sampling procedures
The sample size was calculated to estimate the prevalence of each of the several outcomes investigated in the survey considering the following parameters: unknown prevalence (50%), 95% confidence level, sample error of 3.5% points, design effect of 2 due to the cluster sample design, and the addition of 10% to compensate eventual refusals. An oversample of 15% was included to allow controlling for confounders in the study of associations. The final sample size was 2,016 adults.
The sampling selection was performed in two stages. Firstly, 60 of the 420 urban census tracts of the city were selected. All 420 urban census tracts of the city were ordered according to the average monthly income of the head of the family. A systematic sample of 60 census tracts were used (60/420 or 1/7), which meant 6 census tracts in each income decile. Secondly, all selected census tracts were visited by the fieldwork team and all occupied houses were checked and counted to update the number of residents in the selected clusters. Three census tracts were split into two and six were merged into three, reducing the variability among the number of households in each of them. Sixty-three census tracts resulted from this process, totaling 16,755 eligible households; among these, 1,134 were systematically selected for this study. On average, 32 adults in each census tract were selected.
Eligibility and exclusion criteria
All adults aged between 20 and 59 who were residents of the selected houses were eligible to participate. Exclusion criteria included amputees, bedridden individuals, those with an arm cast, individuals who could not remain in the proper position for the required measurements, and those who were considered unable to answer the questionnaire. Anthropometric and blood pressure measurements were not applied to pregnant women, and those who were within 6 months from delivery were not included.
Data collection
The home visits included the administration of a face-to-face questionnaire applied with the use of a personal digital assistant (PDA), two blood pressure measurements, and weight, height and waist circumference measurements. Thirty-five interviewers were intensively trained prior to field work; the questionnaire pre-test was applied to 35 adults. The pilot study included almost 100 adults living close to the research headquarters and in two census tracts not included in the sample.
Outcome
The dependent variable was hypertension (yes/no). Hypertension was defined as Systolic Blood Pressure (SBP) ≥140 mmHg, or Diastolic Blood Pressure (DBP) ≥90 mmHg, or those taking anti-hypertensive medication [11]. Blood pressure levels (SBP and DBP) were measured twice during the questionnaire application, and the average between the two measurements was considered for the study. The resting time before and between measurements was approximately 10 min. Blood pressure measurements were taken with the interviewee in the sitting position, with feet planted on the floor, left arm relaxed and supported on a table at heart level and with the palm facing upward [12]. Electronic sphygmomanometers with a digital reading system (Techiline®) were used, which had been previously and adequately calibrated to measure blood pressure levels.
Anthropometric variables
Anthropometrics variables were measured twice according to recommendations of Lohman et al. [13], and the average between two measurements was considered for this study.
Body weight (kg) was measured with the individuals in light clothing and barefoot to the nearest 100 g with a scale (GAMA Italy Professional, HCM 5110 M®). Height (cm) was measured maintaining the Frankfort plane, to the nearest 0.1 cm, using a stadiometer with an inelastic measuring tape of 1 mm resolution. BMI was calculated by weight (kg)/height (m)2.
WC was measured with a flexible inelastic plastic-fiber tape measure placed on the midpoint between the lower rib margin and the iliac crest in a perpendicular plane to the long axis of the body, while the subject stood balanced on both feet, nearly 20 cm apart, and with both arms hanging freely.
WHtR was calculated by the ratio between waist circumference (cm) and height (cm). According to Valdez [14], C-index is an indicator of abdominal adiposity and of health risks associated with this type of obesity. Its advantages over other waist ratios are that it is based on a likely model, and its denominator is amenable to tabulation within the normal ranges of human height and weight. The C-index mathematical equation is as following:
Observer reliability measures were calculated as recommended by Gore et al. [15] by using a technical measurement error in percentage points both for intra- and inter-observer errors. The highest value was 1.86% for inter-observer waist circumference.
Control variables
The control variables included socioeconomic-demographic and health behaviors. Age was expressed in years; education was assessed by years in full-time education. Monthly per capita income was calculated as the sum of all earnings in the last month before the interview of all members of the family divided by the number of residents in the house expressed in Reais (R$; Brazilian currency; 1.7 R$ was U$ 1 during data collection). Self-reported skin color was classified as white, dark-skinned black, and light-skinned black (Asiatic—1.0% and Amerindians—1.2% were excluded from the study).
Smoking status was assessed using the categories of never smoking, former smoking, light current smoking (less than 10 cigarettes daily), moderate current smoking (10–20 cigarettes daily), and heavy current smoking (more than 20 cigarettes daily). The latter two categories were merged into one for the current analysis. The Alcohol Use Disorders Identification Test (AUDIT) was used to identify persons with hazardous and harmful patterns of alcohol consumption [16]. Physical activity and fruit and vegetable consumption were assessed through a questionnaire used in the Telephone-based Surveillance of Risk and Protective Factors of Chronic Diseases (VIGITEL) in Brazil [17, 18]. The practice of physical activity was assessed according to the leisure-time domain, with inactive individuals defined as those who did not practice any physical activity in leisure time or practiced less than once a week in the 3 months preceding the interview [17]. The fruit and vegetable consumption was assessed according to regular consumption (≥5 day/week) [18].
Statistical analysis
Descriptive statistics of the outcome and all anthropometric measures are expressed as mean, standard deviation, or as percentage, whenever appropriate. To compare the mean values of continuous variables according to sex, the t test for independent samples was used. To compare the distribution of categorical variables according to sex, the chi-square test was used.
BMI, WC, WHtR, and C-index were used to predict the presence of hypertension. Receiver operating characteristic (ROC) were calculated to compare their predictive validity and to find out their optimal cutoff values [19]. ROC curves were plotted using sensitivity and specificity measures based on various anthropometric cutoff values. The ROC curves demonstrated the overall discriminatory power of a diagnostic test over the whole range of testing values. A better test shows its curve skewed closer to the upper left corner [20]. The area under the curve (AUC) is a measure of the diagnostic power of a test. A diagnostic test with an AUC value of 1 is perfectly accurate, and one with 0.5 has no discrimination power. The differences between AUC of the anthropometric indexes were compared using a nonparametric test [21]. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio (LR+), negative likelihood ratio (LR−) of the anthropometric measurements have been calculated at all possible cutoff points to find the optimal cutoff value. The optimal sensitivity and specificity were the values yielding maximum sums from the ROC curves.
Associations between anthropometric indexes of obesity and hypertension were analyzed by Poisson regression expressed as prevalence ratios (PR) and 95% confidence interval. In addition to the crude Poisson regression analysis, three models of adjusted analysis were developed to verify the association between obesity and hypertension. Model 1 was adjusted by sociodemographic variables (age, skin color, number of school years, and per capita family income). Model 2 was adjusted by sociodemographic variables and health behaviors (smoking status, alcohol abuse, practice of physical activity, and fruit and vegetable consumption). Model 3 was adjusted by sociodemographic variables, health behaviors, BMI (for anthropometric indicators of central obesity) or WC (for BMI), and height.
All analyses were used a significance level of 5%, performed separately for men and women, and adjusted for the complex sample (weighted sample and design effect), considering the whole sample and also stratified by sex, being performed using the MedCalc 12.1.4 and Stata 9.0 software.
Results
Among the 2,016 sampled adults, 1,720 were investigated, which is a response rate of 85.3%. Table 1 shows the main characteristics of the studied sample. For each variable, there were ignored responses as can be seen by the different number of subjects in each variable. The variable with the largest number of responses with no information was the C-index, which is calculated based on the WC, body weight, and height values (women: n = 44; men: n = 14).
Mean values for age, schooling years, BMI, WHtR, and distribution in relation to skin color were similar between men and women (p > 0.05). However, men had higher values for per capita family income, weight, height, WC, C-index, SBP, and DBP (p < 0.05).
The prevalence of hypertension among men who reported smoking more than 10 cigarettes per day, who showed abused use of alcohol, improper diet, BMI between 25 and 29.9 kg/m², and inadequate WHtR, was higher than that of women. In contrast, women were more physically inactive than men and with increased health risk when analyzing the WC values (Table 1).
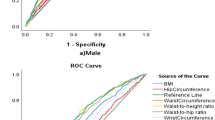
In both sexes, all anthropometric markers of obesity had satisfactory predictive capacity to detect the presence of hypertension (i.e., AUC > 0.5). Moreover, it was found that in both sexes, BMI, WC, and WHtR showed a larger area under the ROC curve than the C-index (p < 0.01) and therefore greater discriminatory power for hypertension (Table 2; Fig. 1).
Table 2 shows the best cutoff points for anthropometric markers of adiposity as discriminators of hypertension in adults and their sensitivity, specificity, PPV, NPV, and likelihood ratios. Concerning women, the cutoff points of BMI and WHtR were those showing the highest sensitivity, that is, they were able to detect more cases of hypertension. On the other hand, the marker with the highest specificity value was the WC, indicating that more than five-sixths (85.7%) of the sample with values below the cutoff points for WC showed no hypertension. The cutoff point of the anthropometric indicator with the highest proportion of true positives was WC (PPV = 59.8%), and the cutoff with the highest proportion of truly negative women was BMI (NPV = 82.4%). Moreover, the cutoff point of WC was the one that best expressed (LR+ = 3.3) how much it would be more probable or the likelihood ratio of a positive test (WC values above the cutoff points) of individuals actually with hypertension when compared with those without hypertension.
In relation to men (Table 2), the cutoff points of BMI and C-index were those showing the highest sensitivity (72.2 and 70.0%, respectively). On the other hand, the marker with the highest specificity was the WC. The cutoff point of WC showed the highest proportion of true positives (PPV = 71.1%), and the indicator with the highest proportion of true negatives was BMI (NPV = 66.2%). Moreover, the cutoff point of WC was the one that best expressed (LR+ = 2.3) how much it would be more probable for a positive test (WC values above the cutoff points) of individuals actually with hypertension when compared with those without hypertension.
Table 3 shows that men and women with abnormal anthropometric indexes were approximately two times more likely to have hypertension than those with normal cutoffs (in crude analyses and adjusted analyses for socio-demographic variables and health behaviors). Model 3, after adjustment by height and BMI (for WC, WHtR, and C-index) or WC (for BMI), showed that the association between obesity and hypertension decreased in both sexes. Moreover, in men, the C-index was not associated with hypertension. In women, the best independent predictor of hypertension was the WC. For men, the best independent predictor of hypertension was the BMI.
Discussion
In this study, all anthropometric indexes analyzed were adequate to identify the presence of hypertension because they had AUC > 0.5. This indicates that both anthropometric indicators of overall obesity (BMI), as indicators of central obesity (WC, WHtR, and C-index), can be used in Brazilian adults as tools for screening of hypertension. Population-based studies conducted with adults in other countries are consistent in showing these associations [4, 6–9], which show the impact of obesity on blood pressure levels.
A recent meta-analysis has reported that BMI was the poorest discriminator for cardiovascular risk factors such as hypertension. On the other hand, WHtR was the best discriminator for both sexes [4]. In this study, the results were not consistent with data reported in the meta-analysis, because the BMI had AUC similar to WHtR and WC. A possible explanation for this finding is that no study conducted in South America was included in the meta-analysis, and ethnic and racial characteristics also affect the magnitude with which anthropometric indicators of obesity are associated with hypertension [22].
By comparing the data from this study with the few population-based surveys conducted in cities from South America, different results were observed. Investigations in cities where most population is Afro-descendant have found that the C-index was the best discriminator of coronary risk factors in adults compared to other indicators such as BMI, WC, and waist-to-hip ratio (WHR) [9, 23]. In exploratory analysis of data from this study, it was found that in black women, the C-index was the best discriminator of hypertension, since it showed larger AUC than the other indicators; however, in black men, none of the indicators analyzed were good discriminators of hypertension.
The best cutoff points for the BMI to detect hypertension in this study were 24.9 kg/m² for women and 24.6 kg/m² for men. These cutoff points are virtually identical to those proposed by the World Health Organization—WHO, which is 25.0 kg/m² for both sexes [24]. Results of cutoff points for BMI for predicting hypertension similar to those of the WHO have been reported in Iran [7] and Mexico [25]. However, in Eastern countries, the cutoff point for BMI for both sexes is 23.0 kg/m², which reflects the differences between western and eastern populations [26].
With respect to the cutoff points for WC identified in this study, the results are different from those of literature. The proposal widespread by the NIH and used in most western countries uses WC values >102 cm (men) and 88 cm (women) as the best cutoff points to identify obesity and health risks. These cutoff points are based on population surveys conducted in the North American population [3]. In the present study, the use of these values would imply many people being incorrectly classified (20.4%, CI 95%: 17.1, 23.6 of women and 11.2%, CI 95%: 8.8, 13.6 of men), generating many false negatives, since the cutoff points identified in the study participants were 86.2 cm for women and 89.5 cm for men. Other surveys conducted in different countries also found cutoff points lower than those suggested by the NIH of WC [7–9, 23, 25], which highlights the necessity of using local cutoff points of WC.
In the present study, the best cutoff points of WHtR to detect the presence of hypertension were 0.49 for women and 0.50 for men. In a study conducted in Mexico City, the best cutoff points of WHtR as a discriminator of diabetes, hypertension and dyslipidemia ranged from 0.53 to 0.54 [25]. In China, it was observed that the most suitable cutoff point of WHtR to detect coronary risk was 0.48 for both sexes [8]. In a South American city, the best cutoffs for detecting health risks were 0.52 and 0.53 for men and women, respectively [27]. Due to these similarities in the cutoff points for different locations, Pitanga and Lessa [27] stressed that the public health message could be that the WC of a particular person should not be greater than half of his height.
As in the present study, other investigations have found association of C-index with health risks [9, 23]. The major limitation for the use of the C-index is that there are few proposals for cutoff points that can discriminate non-communicable diseases. One of these studies suggested a cutoff point of 1.25 for men and 1.18 for women [9]. Another study investigated only men and proposed a cutoff point of 1.26 [28]. In the present study, the cutoff points proposed were 1.18 for men and 1.15 for women. One of the main differences of this study from other studies is that in the former [9], the cutoff points were proposed for coronary risk, not differentiating hypertension from diabetes, hypercholesterolemia and smoking habit, and the latter, the cutoff point was proposed based on a percentile distribution (percentile 75) [28], rather than on criteria as in this study. Moreover, none of the studies previously mentioned showed predictive values and likelihood ratios, which prevent larger comparisons.
For each cutoff point of anthropometric indicators set out in this study, sensitivity, specificity, PPV, NPV, LR+, and LR− values were presented. Most studies that investigated the accuracy of anthropometric indicators of obesity to detect coronary risk factors such as hypertension, diabetes, and dyslipidemia reported only sensitivity and specificity values of each cutoff point [9, 23, 27, 29]. Although the sensitivity and specificity measures are important to evaluate a diagnostic test, they do not provide detailed information for choosing the most appropriate anthropometric indicator. Thus, it is recommended to investigate other accuracy measures such as PPV and NPV, which depend essentially on the sensitivity, specificity, and prevalence of the disease at the location where the study was developed.
The likelihood ratio (LR+ and LR−) is another recommended measure in accuracy studies and describes the practical usefulness of the anthropometric indicator, expressing how many times would be most probable or likely a positive outcome to anthropometric indicators in individuals actually with hypertension when compared with those without this condition. The higher the LR+ of the anthropometric indicator, the greater the ability to diagnose hypertension, while a low LR− value reveals a low probability of the disease to occur in individuals with negative test. Few researchers that have investigated the accuracy of anthropometric indicators for predicting hypertension showed LR+ and LR− values for cutoff points [30]. In a population-based study developed in Iraq [30], the indicator with the highest LR+ value for both women and men was, respectively, WHtR and BMI, unlike in the present study, which was WC for both sexes.
The Poisson regression was run separately for each index in men and women, and all anthropometric indexes were independently associated with hypertension (crude analyzes, model 1 and model 2). These results have confirmed that abnormal cutoff values of BMI, WC, WHtR, and C-index increased the risk of having hypertension, in comparison with normal cutoffs [29–31]. However, differently from other studies conducted in general populations [29–31], our findings were obtained adjusted by age, number of schooling years, per capita family income, skin color, smoking status, alcohol abuse, physical activity and diet, factors that affect blood pressure independently. A study conducted in the adult population of Mexico found that of the four indicators examined (BMI, WC, WHR, and WHtR), only BMI and WHR have been associated with hypertension after adjusting for age [25]. Lee et al. [4] reported that in adults in Taiwan, BMI and WC were the best predictors of hypertension and as the values of indicators increased, their chances to show hypertension were higher (odds ratio >1.0); however, the authors did not adjust for any other variable.
By comparing the crude analysis with the analysis adjusted by sociodemographic variables and health behaviors (model 1 and model 2), it was found that the association between obesity and hypertension in men almost remained unchanged. On the other hand, in women, the magnitude of the association in adjusted analysis compared to the crude analysis decreased. These findings indicate that in men of the present study, the confounding variables almost did not influence the association between obesity and hypertension. In women, these variables attenuated this association, indicating that there may be possible interactions between sociodemographic aspects and/or health behaviors and obesity. By adjusting the analysis model by BMI or WC and height, it was found that the magnitude of association between obesity and hypertension decreased in both sexes, which was also observed in other studies [32, 33]. This decrease may be due, at least in part, to the strong correlation between anthropometric indicators [33].
For the four anthropometric indicators analyzed, the magnitude of association (odds ratio) between obesity and hypertension was higher in women than in men, even after adjusting for potential confounding variables. This increased strength of association between obesity and hypertension in women compared to men was also observed by other researchers [4–34]. One possible explanation for these findings could be the use of oral contraceptives that once used by obese women above 35 years of age increases the risk of hypertension [12]. The present study did not collect information on the use of contraceptives; therefore, inferences must be analyzed with caution.
This study has some limitations such as: the analyses are based on cross-sectional data; therefore, a cause and effect relationship between anthropometric indexes and hypertension cannot be drawn; therefore, reverse causality cannot be ruled out. In addition, chronic diseases such as hypertension are heterogeneous and multifactorial and besides anthropometric measurements, other factors such as hereditary factors must be considered in future researches.
In conclusion, our findings showed that in Brazilian adults, BMI, WC, and WHtR were the best anthropometric indexes of obesity to identify the presence of hypertension. Moreover, among all cutoff points set out, WC was the one the best expressed how much would be more likely a positive result to the test for individuals with hypertension. WC and BMI had greater magnitude of association with hypertension in women and men, respectively.
This study is the first study in Brazil to estimate the prevalence ratios with the cutoffs in their own population. This increases the possible inferences regarding anthropometric indexes of obesity to identify the presence of hypertension in the adult population. These results have a vital public health implication for developing countries. Anthropometric indexes provide the prospect of an extremely effective, simple, inexpensive, and non-invasive means for a first-level screening for hypertension.
References
Tuck ML, Corry DB (2010) Prevalence of obesity, hypertension, diabetes, and metabolic syndrome and its cardiovascular complications. Curr Hypertens Rev 6:73–82
Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, Singh GM, Gutierrez HR, Lu Y, Bahalim AN, Farzadfar F, Riley LM, Ezzati M, Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Body Mass Index) (2011) National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet 377:557–567
National Institutes of Health, National Heart, Lung, and Blood Institute, (1998) Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. Obes Res 6:S51–S210
Lee CM, Huxley RR, Wildman RP, Woodward M (2008) Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: a meta-analysis. J Clin Epidemiol 61:646–653
Wang TD, Goto S, Bhatt DL, Steg PG, Chan JC, Richard AJ, Liau CS, REACH Registry Investigators (2010) Ethnic differences in the relationships of anthropometric measures to metabolic risk factors in Asian patients at risk of atherothrombosis: results from the REduction of Atherothrombosis for Continued Health (REACH) Registry. Metabolism 59:400–408
Cox BD, Whichelow M (1996) Ratio of waist circumference to height is better predictor of death than body mass index. BMJ 313:1487
Mirmiran P, Esmaillzadeh A, Azizi F (2004) Detection of cardiovascular risk factors by anthropometric measures in Tehranian adults: receiver operating characteristic (ROC) curve analysis. Eur J Clin Nutr 58:1110–1118
Ho SY, Lam TH, Janus ED (2003) Waist to stature ratio is more strongly associated with cardiovascular risk factors than other simple anthropometric indices. Ann Epidemiol 13:683–691
Pitanga FJG, Lessa I (2005) Anthropometric indexes of obesity as an instrument of screening for high coronary risk in adults in the city of Salvador—Bahia. Arq Bras Cardiol 85:26–31
Brazilian Institute of Geography and Statistics (2009) Estimates of the resident population on 1 July 2009, according to cities. http://www.ibge.gov.br/home/estatistica/populacao/estimativa2009/POP2009_DOU.pdf. Accessed March 2010
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ, National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee (2011) The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA 289:2560–2572
Sociedade Brasileira de Hipertensão, Sociedade Brasileira de Cardiologia e Sociedade Brasileira de Nefrologia (2007) V Diretrizes Brasileiras de Hipertensão Arterial. Sociedade Brasileira de Hipertensão, Sociedade Brasileira de Cardiologia e Sociedade Brasileira de Nefrologia. Arq Bras Cardiol 89:e24–e79
Lohman TG, Roche AF, Martorell R (1998) Anthropometric standardization reference manual. Human Kinetics Books, USA, Champaign
Valdez R (1991) A simple model-based index of abdominal adiposity. J Clin Epidemiol 44:955–956
Gore C, Norton K, Olds T, Whittingham N, Birchall K, Clough M, Dickerson B, Downie L (1996) Accreditation in anthropometry: an Australian model. In: Norton K, Olds T (eds) Anthropometrica. University of New South Wales Press, Sydney, pp 395–411
Babor TF, Higgins-Bible JC, Saunders JB, Monteiro MG (2001) The alcohol use disorders identification test: guidelines for use in primary care, 2nd edn. World Health Organization, Geneve
Florindo AA, Hallal PC, Moura EC, Malta DC (2009) Practice of physical activities and associated factors in adults, Brazil, 2006. Rev Saúde Pública 43:65–73
Jaime PC, Figueiredo IC, Moura EC, Malta DC (2009) Factors associated with fruit and vegetable consumption in Brazil, 2006. Rev Saúde Pública 43:S57–S64
Swets JA (1973) The relative operating characteristics in psychology. Science 182:990–1000
Hanley JA, McNeil BJ (1982) The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 143:29–36
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845
Danaei G, Finucane MM, Lin JK, Singh GM, Paciorek CJ, Cowan MJ, Farzadfar F, Stevens GA, Lim SS, Riley LM, Ezzati M, Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Blood Pressure) (2011) National, regional, and global trends in systolic blood pressure since 1980: systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5.4 million participants. Lancet 377:568–577
Almeida RT, Almeida MM, Araújo TM (2009) Abdominal obesity and cardiovascular risk: performance of anthropometric indexes in women. Arq Bras Cardiol 92:345–350
World Health Organization (2000) Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 894:i–xii, 1–253
Berber A, Gómez-Santos R, Fanghänel G, Sánchez-Reyes L (2001) Anthropometric indexes in the prediction of type 2 diabetes mellitus, hypertension and dyslipidaemia in a Mexican population. Int J Obes Relat Metab Disord 25:1794–1799
World Health Organization (2000) The Asia-Pacific perspective: redefining obesity and its treatment. WHO, Geneva
Pitanga FJ, Lessa I (2006) Waist-to-height ratio as a coronary risk predictor among adults. Rev Assoc Med Bras 52:157–161
Coniglio RI, Colombo O, Vasquez L, Salgueiro AM, Otero JC, Malaspina MM (1997) Central obesity: relationship between conicity index and lipoproteic parameters as a risk factors for coronary atherosclerosis. Medicina (B.Aires) 57:21–28
Lin WY, Lee LT, Chen CY, Lo H, Hsia HH, Liu IL, Lin RS, Shau WY, Huang KC (2002) Optimal cut-off values for obesity: using simple anthropometric indices to predict cardiovascular risk factors in Taiwan. Int J Obes Relat Metab Disord 26:1232–1238
Mansour AA, Al-Jazairi MI (2007) Cut-off values for anthropometric variables that confer increased risk of type 2 diabetes mellitus and hypertension in Iraq. Arch Med Res 38:253–258
Schneider HJ, Glaesmer H, Klotsche J, Böhler S, Lehnert H, Zeiher AM, März W, Pittrow D, Stalla GK, Wittchen HU, DETECT Study Group (2007) Accuracy of anthropometric indicators of obesity to predict cardiovascular risk. J Clin Endocrinol Metab 92:589–594
Wang TD, Goto S, Bhatt DL, Steg PG, Chan JC, Richard AJ, Liau CS, REACH Registry Investigators (2010) Ethnic differences in the relationships between anthropometric measures and metabolic risk factors in Asian patients at risk of atherothrombosis: results from the REduction of Atherothrombosis for Continued Health (REACH) Registry. Metabolism 59:400–408
Barbosa LS, Scala LCN, Ferreira MG (2009) Association between anthropometric markers of body adiposity and hypertension in an adult population of Cuiabá, Mato Grosso. Rev Bras Epidemiol 12:237–247
Yusuf S, Hawken S, Ounpuu S, Bautista L, Franzosi MG, Commerford P, Lang CC, Rumboldt Z, Onen CL, Lisheng L, Tanomsup S, Wangai P Jr, Razak F, Sharma AM, Sharma AM, Anand SS, INTERHEART Study Investigators (2005) Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control study. Lancet 366:1640–1649
Acknowledgments
We would like to thank Dr. Nilza Nunes da Silva, School of Public Health of the University of São Paulo, São Paulo, Brazil, for her advice on sample procedures and to the Brazilian Institute of Geography and Statistics (IBGE) and the Florianópolis Health Authority staff for their useful help with the practical aspects of the study.
Conflict of interest
The authors declare no conflict of interest. The Project was sponsored by the Brazilian National Council for Scientific and Technological Development (CNPq), grant number 485327/2007-4. ELP, and MAP received grants for research productivity (CNPq).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Silva, D.A.S., Petroski, E.L. & Peres, M.A. Accuracy and measures of association of anthropometric indexes of obesity to identify the presence of hypertension in adults: a population-based study in Southern Brazil. Eur J Nutr 52, 237–246 (2013). https://doi.org/10.1007/s00394-012-0314-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-012-0314-8