Abstract
Purpose
Stress exposure elicits neuroinflammation and oxidative damage in brain, and stress-related neurological and neuropsychiatric diseases have been associated with cell damage and death. Mangiferin (MAG) is a polyphenolic compound abundant in the stem bark of Mangifera indica L. with antioxidant and anti-inflammatory properties in different experimental settings. In this study, the capacity of MAG to prevent neuroinflammation and brain oxidative damage induced by stress exposure was investigated.
Methods
Young–adult male Wistar rats immobilized during 6 h were administered by oral gavage with increasing doses of MAG (15, 30, and 60 mg/Kg), respectively, 7 days before stress.
Results
Prior treatment with MAG prevented all of the following stress-induced effects: (1) increase in glucocorticoids (GCs) and interleukin-1β (IL-1β) plasma levels, (2) loss of redox balance and reduction in catalase brain levels, (3) increase in pro-inflammatory mediators, such as tumor necrosis factor alpha TNF-α and its receptor TNF-R1, nuclear factor-kappa B (NF-κB) and synthesis enzymes, such as inducible nitric oxide synthase (iNOS) and cyclooxygenase-2 (COX-2), (4) increase in lipid peroxidation.
Conclusions
These multifaceted protective effects suggest that MAG administration could be a new therapeutic strategy in neurological/neuropsychiatric pathologies in which hypothalamic/pituitary/adrenal (HPA) stress axis dysregulation, neuroinflammation, and oxidative damage take place in their pathophysiology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stress exposure elicits a wide range of physiological and psychopathological processes. Most of the evidence about harmful consequences of stress indicates that chronic persistence of the stressor is required, however, before non-reversible or partially reversible changes take place, acute exposure to stress produces some cellular changes very similar to those observed after repeated stressful stimulus [1]. In the brain, most of the deleterious consequences after stress exposure are attributed to supraphysiological effects of glucocorticoids, which lead to imbalance in energy systems and an increased vulnerability to excitotoxicity [2].
In addition to these deleterious effects of stress on energy production and excitotoxic processes, an increasing number of studies continue paying attention to the oxidative/nitrosative damage and the inflammatory processes involved in the response to stress in the central nervous system (CNS) [3]. In fact, numerous neurological and neuropsychiatric diseases related with stress exposure (neurodegenerative diseases, depression, and schizophrenia) have been associated with inflammatory/oxidative phenomena [4–7]. In this context, it has been demonstrated that pro-inflammatory cytokines interleukin 1β and tumor necrosis factor α (IL-1β and TNFα) released after stress stimulus initiate an inflammatory response characterized by the activation of the pro-inflammatory nuclear transcription factor-kappa B (NF-κB) pathway [8, 9]. NF-κB activation elicits the expression and activity of pro-inflammatory mediator’s synthesis enzymes, such as inducible nitric oxide (NO) synthase (iNOS) and cyclooxygenase-2 (COX-2), among others [10, 11]. It is demonstrated that iNOS stimulation leads to the over-production of NO, and consequently, generation of peroxynitrite anion (ONOO−), which damages target molecules including proteins, glutathione (GSH), and DNA [12] and disrupts membrane phospholipids integrity, causing cell damage in a process known as lipid peroxidation [13].
The specific molecular and cellular events induced by stress that are responsible for the brain damage found in these conditions are still a matter of debate, and the search for mechanisms of prevention or treatment against the negative consequences of stress has increased [3, 14].
Polyphenolic compounds, specifically found in fruit, vegetables, plant extracts, wine, tea, and dry fruits, are natural antioxidants that have been recently proposed to be useful prophylactics for the treatment for oxidative neuronal damage [15, 16]. An aqueous stem bark extract from Mangifera indica L. (Mango, Anacardiaceace family) has been traditionally used as a nutritional supplement. The composition is a defined mixture of polyphenols, flavonoids, triterpenoids, steroids, phytosterols, fatty acids, and microelements (mainly zinc, copper, and selenium) [17]. The extract has been described as an antioxidant with anti-inflammatory and immunomodulatory activities in several experimental settings [18–21]. In general, the neuroprotective effects of the extract have been demonstrated in in vitro experimental settings [19] and a reduced number of studies show anti-inflammatory and anti-excitotoxic properties in specific in vivo models, such as experimental brain ischemia [22].
Mangiferin (2-beta-D-glucopyranosyl-1,3,6,7-tetrahydroxyxanthone; MAG) is a xanthone, which is abundantly found in fruit and in the cortex of the stalk of Mangifera indica L. The mechanisms of action of MAG need to be fully investigated but recent studies demonstrate an improvement in memory and learning deficits afforded by the treatment with MAG in rodents [23, 24]. Given the promising biological actions of the extract and the aforementioned nootropic effects of MAG, the aim of the present study was to evaluate the in vivo effects of increasing doses of MAG in a model of oxidative and inflammatory damage in brain caused by acute restraint stress in rats and to elucidate some of the possible neuroprotective mechanisms of action involved.
Methods
Animals
Male outbred Wistar Hannover rats (HsdRccHan:Wist, from Harlan, Spain), initially weighing 200–225 g, were housed five per cage and maintained in an animal holding room controlled at a constant temperature of 24 ± 2 °C with a relative humidity of 70% ± 5% and a 12 h light–dark cycle. Animals were fed on a standard pellet chow (standard rat chow A04 SAFE, Scientific Animal Food and Engineering, Augy, France) with free access to fresh tap water. All experimental protocols followed the guidelines of the Animal Welfare Committee of the Universidad Complutense according to European legislation (2003//65/EC). Chemicals were from Sigma (Spain) or as indicated.
Preparation of mangiferin
MAG was supplied by the Laboratory of Analytical Chemistry, Center of Pharmaceutical Chemistry (Havana, Cuba). It was isolated from a standardized extract of Mangifera indica L. stem bark by extraction with methanol. At the end of the process, a yellow powder with 90% purity was obtained [17]. MAG was suspended in distilled water (DW) to obtain doses of 15, 30, and 60 mg/Kg, respectively. MAG plasma concentration in rats following intragastric administration of free MAG at a dose of 70 mg/kg decreases in time (1–8 h after administration) from 200 to 50 ng/mL [25]. MAG can pass the blood–retina barrier after a single administration; tissue concentrations reached 5.7 μg/mL 0.5 h after iv administration (50 mg/kg) and then dropped gradually to 0.30 μg/mL 5.0 h later [26]. Trace amount of MAG were found in the brain after the oral administration of an extract of the herb Rhizoma Anemarrhenae (0.75 g/mL, whose major active component is MAG), which indicated that mangiferin could pass through the blood–brain barrier [27]. The doses of MAG here used are not toxic in base of previous studies showing an EC50 for intra-peritoneal MAG of 365 mg/Kg [28].
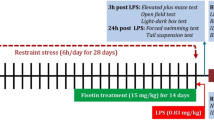
Experimental design
The rats were randomly divided into six groups. Three groups (n = 7) received MAG at doses of 15, 30, and 60 mg/Kg p.o. once a day, during 7 days (MAG15, MAG30, MAG60, respectively). Other group (n = 7) received vehicle (DW) 7 days p.o. (S); Ctr, n = 4. At day 8, animals were exposed to 6-h stress between 09:00 and 15:00 in the animal homeroom. Two other groups were carried out: a control group (Ctr) receiving vehicle p.o. 7 days but not subjected to stress on day 8th and a group (Ctr + MAG60) receiving the higher dose of MAG (60 mg/Kg p.o.) 7 days and not subjected to stress on day 8th.
The restraint was performed using a plastic rodent restrainer that allowed for a close fit to rats [29]. One hour before the onset of stress, each treated group received MAG or DW at the corresponding doses. The two non-stressed groups (Ctr and Ctr + MAG60) were not subjected to stress, but were handled at 09:00 for a few seconds. Animals were killed immediately after restraint (still in the restrainer) using sodium pentobarbital. Blood for plasma determinations was collected by cardiac puncture and anticoagulated in the presence of trisodium citrate (3.15% (wt/vol), 1 vol citrate per 9 vol blood). After decapitation, the brain was removed from the skull, and after careful removal of the meninges and blood vessels, the prefrontal cortical areas from both brain hemispheres were excised and frozen at −80 °C until assayed. Rat brain prefrontal cortex was chosen because of its high levels of pro-inflammatory mediators (TNF-α, NF-κB, iNOS, COX-2) after stress or inflammatory challenge, its susceptibility to neuroinflammatory/oxidative process elicited by inflammatory/immune stimulus [30], and finally because this brain area is an important neural substrate for the regulation of the hypothalamic/pituitary/adrenal (HPA) axis response to stress [31].
Plasma corticosterone
Plasma was obtained from blood samples by centrifuging the samples at 1,000g for 15 min immediately after stress. All plasma samples were stored at −20 °C before assay by using a commercially available kit by RIA of 125I-labeled rat corticosterone (DPC, Los Angeles, CA, USA). A gamma counter was used to measure radioactivity of the samples. The values obtained in control animal match with the kit manufacturer’s expected values in adult male Wistar rats at the time of blood extraction (≈15:00 h).
Detection of plasma lL-1β levels
To determine brain levels of IL-1β, brain cortices were removed and homogenized by sonication for 10 s at 4 °C in 4 volumes of homogenization buffer containing 320 mmol/L sucrose, 1 mmol/L dl-dithiothreitol, 10 μg/mL leupeptin, 10 μg/mL soybean trypsin inhibitor, 2 μg/mL aprotinin, 0.2% Nonidet® P40, and 50 mmol/L Tris brought to pH 7.0 with HCl. The homogenates were centrifuged (13,000g for 10 min at 4 °C), and supernatants were used for determinations with a commercially available rat enzyme-linked immunosorbent assay kit (Quantikine®, R&D Systems, Abingdon, UK) according to the manufacturer’s instructions.
Total antioxidant activity
To determine total antioxidant activity in brain cortex, samples were homogenized by sonication for 10 s at 4 °C in 4 vol of phosphate buffer, pH 7.4. The homogenates were then centrifuged for 20 min at 12,000g, and the supernatant was utilized for determinations using a commercially available Total Antioxidant Status Assay kit (Calbiochem, Germany) following the manufacturer’s instructions.
Lipid peroxidation
Lipid peroxidation was measured by the thiobarbituric acid test for malondialdehyde (MDA) following a method previously described [32] with some modifications. Brain cortices were homogenized by sonication for 10 s at 4 °C in 10 vol 50 mM phosphate buffer and deproteinized with 40% trichloroacetic acid and 5 M HCL, followed by the addition of 2% (w/v) thiobarbituric acid in 0.5 M NaOH. The reaction mixture was heated in a water bath at 90 °C for 15 min and centrifuged at 12,000g for 20 min. The pink chromogen was measured at 532 nm in a Beckman DU-7500 spectrophotometer. The results were expressed as nanomol per milligram of protein.
Catalase determination
Catalase (CAT) activity was determined in frozen brain cortices that were homogenized by sonication for 10 s at 4 °C in cold 50 mM Tris buffer pH 7.4 by means of commercially available colorimetric assay (Bioxytech, Catalase 520, Oxis Research, Portland, OR, USA). The method is based on a two-stage reaction.
The rate of dismutation of hydrogen peroxide (H2O2) to water and molecular oxygen is proportional to the concentration of CAT. A known amount of H2O2 was added to the sample with CAT and incubated exactly 1 min. The reaction was stopped with sodium azide. The amount of H2O2 remaining in the reaction mixture was then determined by the oxidative coupling reaction of 4-aminophenazone (AAP) and 3,5-dichloro-2-hydroxybenzenesulfonic acid (DHBS) and catalyzed by horseradish peroxidase. The resulting quinoneimine dye was measured at 520 nm (microplate reader, Molecular Devices, Thermo Max®).
Western blot analysis
Cortical samples were homogenized at 4 °C in 5 vol of buffer containing 320 mmol/L sucrose, 1 mmol/L, DL-dithiothreitol, 10 μg/mL leupeptin, 10 μg/mL soybean trypsin inhibitor, 2 μg/mL aprotinin, and 50 nmol/L Tris brought to pH 7.0, and centrifuged at 12,000g for 20 min. After determining and adjusting protein levels, supernatants were mixed with Laemmli sample buffer (Bio Rad, Hercules, CA, USA; SDS 10%, distilled H2O, glycerol 50%, Tris–HCl 1 M, pH 6,8, dithiotreitol and blue bromophenol) and beta mercapthoethanol (50 μL per mL of Laemmli). After heating at 90° for 10 min, the proteins present in the supernatants were loaded (20 μg) and size was separated in 10 or 14% (for TNF-α analysis) SDS–PAGE (90–100 mV). The proteins were electroblotted onto nitrocellulose membranes (Millipore, Bedford, MA). Afterward, the membranes were blocked in 10 mM Tris-buffered saline containing 0.1% Tween 20 (TBST) and 5% skim milk and then incubated with the following specific antibodies: (a) for inducible cyclooxygenase COX-2, a goat polyclonal antibody 1:1,000 in TBS-Tween; (b) for inducible nitric oxide synthase, NOS-2, a rabbit polyclonal antibody 1:1,000 in TBS-Tween; (c) for IkB in citosolic fraction, a rabbit polyclonal antibody 1:1,000 in TBS-Tween; (d) for p65, in nuclear fraction, rabbit polyclonal antibody 1:1,000 in TBS-Tween; (e) for TNFR-1, a rabbit polyclonal antibody 1:750 in 2.5% skimmed milk in TBS-Tween; (f) for TNFR-2, a rabbit polyclonal antibody 1:750 in 2.5% skimmed milk in TBS-Tween; and (g) for TNF-α, a rabbit polyclonal antibody from Peprotech Inc, 1:750 in 2.5% skimmed milk in TBS-Tween. All antibodies were provided by Santa Cruz Biotechnology or as it indicating. After washing the membranes with 10 mM Tris-buffered saline containing 0.1% Tween 20, the membranes were incubated with the respective horseradish peroxidase-conjugated secondary antibodies for 90 min at room temperature. Proteins recognized by the antibody were visualized on X-ray film by chemiluminescence following the manufacturer’s instructions (Amersham, lbérica, Spain). Autoradiographs were quantified by densitometry (Image J), and several exposition times were analyzed to ensure the linearity of the band intensities. All densitometries are expressed in arbitrary units (AU). The house keeping gene β-actin was used as loading control and the nuclear receptor sp-1 for nuclear extracts (blots shown in the respective figures).
Preparation of nuclear extracts
A modified procedure based on the method of Schreiber et al. [33] was used. Tissues (brain cortex) were homogenized with 300 mL of buffer A (10 mm HEPES, pH 7.9, 1 mm EDTA, 1 mm EGTA, 10 mm KCl, 1 mm DTT, 0.5 mm PMSF, 0.1 mg/mL aprotinin, 1 mg/mL leupeptin, 1 mg/mL TLCK, 5 mm NaF, 1 mm NaVO 4, and 10 mm Na2 MoO4). After 15 min, Nonidet P-40 was added to reach a 0.5% concentration. The tubes were gently vortexed for 15 s, and cytosolic fraction was collected by centrifugation at 13,000×g for 1 min. The pellets were resuspended in 70 μL of buffer C (20 mm HEPES, pH 8, 1 mm EDTA, 1 mm EGTA, 0.4 M NaCl, 1 mm DTT, 0.5 mm PMSF, 0.1 mg/mL aprotinin, 1 mg/mL leupeptin, 1 mg/mL TLCK, 5 mm NaF, 1 mm NaVO 4, and 10 mm Na2 MoO4) and gently shaken for 30 min at 4 °C.
Nuclear protein extracts were obtained by centrifugation at 13,000×g for 5 min, and aliquots of the supernatant were stored at −80 °C. All steps of the fractionation were carried out at 4 °C. Cytosolic proteins were used for IkBα determination and nuclear extracts for the identification of the NF-κB subunit p65.
Chemicals and statistical analysis
Unless otherwise stated, the chemicals were from Sigma Spain, Madrid. Data in text and figures are expressed as mean ± SEM. For multiple comparisons, a one-way ANOVA followed by the Newman-Keuls post hoc test to compare all pairs of means between groups was made. A p value <0.05 was considered statistically significant.
Results
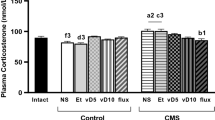
Effect of mangiferin on corticosterone and IL-1β plasma levels
Acute stress induced a significant increase in corticosterone plasma levels compared to control group as shown in Fig. 1a (S = 509.2 ± 32.7 ng/mL vs. Ctr = 265.0 ± 62.2 ng/mL). The respective treatments with MAG blocked this increase at all doses assayed (MAG15 = 199.7 ± 32.4 ng/mL, MAG30 = 201.3 ± 81.3 ng/mL, MAG60 = 177.6 ± 66.1 ng/mL). Similarly, stress exposure also increased IL-1β plasma levels (S = 146 ± 27.2 ρg/mL, Ctr = 48.8 ± 3.8 ρg/mL). Previous administration of MAG resulted in a significant decrease in IL-1β levels only at the doses of 30 and 60 mg/Kg (MAG15 = 111.0 ± 15.2 ρg/mL, MAG30 = 71.5 ± 18.8 ρg/mL, MAG60 = 62.9 ± 16.0 ρg/mL; Fig. 1b).
Effect of MAG on corticosterone and IL-1β plasma levels. Corticosterone (ng/mL) (a) and IL-1β (pg/mL) (b) plasma levels at the time of blood extraction (15:00 h) of control (Ctr), stressed during 6 h (S), and stressed + Mangiferin at increasing doses of 15, 30 and 60 mg/Kg, respectively (MAG15, MAG30, MAG60) Wistar rats. Data represent the mean ± SEM of six rats. *p < 0.05 versus Ctr; # p < 0.05 versus S (One-way ANOVA following Newman-Keuls posttest)
The group of animals receiving MAG 60 mg/Kg p.o. 8 days and not subjected to stress (Ctr + MAG60) did not show differences versus Ctr group in any plasma or brain determinations made (corticosterone levels: 243.5 ± 43 ng/mL; IL-1β levels: 43 ± 7.2 ρg/mL). For clarity, this group is not shown in text of figures.
Mangiferin improves antioxidant status
Restraint stress was also characterized by a decrease in total antioxidants levels in brain prefrontal cortex (S = 0.057.01 ± 0.006 μg/mg of protein) compared with control group (Ctr = 0.097 ± 0.017 μg/mg of protein; Fig. 2a). Prior administration of MAG partially reverted this stress-induced depletion in antioxidants levels at doses of 30 years 60 mg/Kg, respectively (MAG30 = 0.077 ± 0.004 μg/mg of protein, MAG60 = 0.087 ± 0.005 μg/mg of protein).
MAG antioxidant effects on brain. Total antioxidant status (a), catalase levels (b), and lipid peroxidation (MDA levels) (c) in prefrontal cortex homogenates of control (Ctr), stressed during 6 h (S) and stressed + Mangiferin at increasing doses of 15, 30 and 60 mg/Kg, respectively (MAG15, MAG30, MAG60) Wistar rats. Values represent the mean ± SEM of six rats. *p < 0.05 versus Ctr; # p < 0.05 versus S; (One-way ANOVA following Newman–Keuls post-test)
Effect of mangiferin on catalase levels
Catalase is one of the most important antioxidant enzymes. Figure 2b shows a decrease in catalase activity in stressed animals (S) (1.07 ± 0.2 Units/mg of protein) compared to the control group (2.26 ± 0.16 Units/mg of protein). In this case, MAG at 15 mg/Kg did not show differences compared with SS group (MAG15 = 2.21 ± 0.3 Units/mg of protein; MAG30 = 4.54 ± 0.45 μg/mg of protein). However, the higher doses of MAG significantly restored catalase activity to control levels (MAG30 = 2.84 ± 0.66; MAG 60 = 2.93 ± 0.14 Units/mg of protein).
Effect of mangiferin on lipid peroxidation
The effect of MAG on lipid peroxidation—an indicator of cellular membrane damage as a result of oxidative/nitrosative toxicity caused by acute immobilization stress in rats’ brain cortex is represented in Fig. 2c. In the stressed rats (S), the levels of MDA were significantly increased (0.50 ± 0.07 nmol/mg) when compared with control group (0.31 ± 0.05 nmol/mg). Previous administration of MAG resulted in a significant reduction in MDA values at all doses tested (MAG15 = 0.29 ± 0.05 nmol/mg, MAG 30 = 0.23 ± 0.01 nmol/mg; MAG60 = 0.26 ± 0.02 nmol/mg), compared to the stress group.
Effect of mangiferin on expression of iNOS and COX-2
When rats were exposed to 6 h of acute stress, the levels of the pro-inflammatory enzymes iNOS and COX-2 in brain prefrontal cortex samples were significantly increased (Fig. 3a, b: lanes 3, 4). Pre-treatment with MAG at higher doses (30 years 60 mg/Kg) resulted in a significant decrease in iNOS expression. Regarding COX-2 expression, attenuation of band intensities was also observed at the lower dose (Fig. 3a, b; lanes 5–10). The significant differences between groups were quantified by densitometry analysis.
MAG anti-inflammatory effects on brain I. Pro-inflammatory enzymes. Western blots and densitometric analysis of iNOS (a) and COX-2 (b) in prefrontal cortex homogenates of control (Ctr), stressed during 6 h (S), and stressed + Mangiferin at increasing doses of 15, 30 and 60 mg/Kg, respectively (MAG15, MAG30, MAG60) Wistar rats. Data are normalized by β-actin (lower band) and are representative of 3 experiments. *p < 0.05 versus Ctr; # p < 0.05 versus S (One-way ANOVA following Newman-Keuls posttest). AU: arbitrary units
Effect of mangiferin on expression of TNF-α and TNF receptors
As shown in Fig. 4a, exposure to acute stress produced a significant increase in TNF-α expression (lanes 3, 4) compared to Ctr group (lanes 1, 2). In relation with this effect, an increase in TNFR-1 expression was also found (Fig. 4b). Administration of Mangiferin reduced TNF-α and TNFR-1 up-regulation only at the higher dose of 60 mg/Kg (Fig. 4a, b: lanes 9, 10). Values of relative band intensities of increased TNF-α and TNFR-1 expression caused by stress were reduced by prior treatment with Mangiferin (60 mg/Kg) in 19.5 and 10.3%, respectively. Expression of TNFR-2 was not significantly affected by stress exposure or MAG pre-treatments (Fig. 4c).
MAG anti-inflammatory effects on brain II. TNF-α pathway. Western blots and densitometric analysis of the pro-inflammatory cytokine TNF-α (a) and its receptors TNFR-1 (b) and TNFR-2 (c) in prefrontal cortex homogenates of control (Ctr), stressed during 6 h (S) and stressed + Mangiferin at increasing doses of 15, 30 and 60 mg/Kg, respectively (MAG15, MAG30, MAG60) Wistar rats. Data are normalized by β-actin (lower band) and are representative of 3 experiments. *p < 0.05 versus Ctr; # p < 0.05 versus S (One-way ANOVA following Newman-Keuls posttest). AU arbitrary units
Effect of mangiferin on expression of p65 and IκBα
Stress exposure led to a decrease in IκBα subunit expression in cytosolic extracts of brain prefrontal cortex samples. Conversely, an enhancement of the NF-κB pro-inflammatory unit p65 expression was observed in nuclear extracts (Fig. 5a: lanes 3, 4). Prior treatment with MAG at doses of 15 and 30 mg/Kg did not show differences compared to S group (Fig. 5a: lanes 5–8). However, administration of MAG at dose of 60 mg/Kg produced an increase in the values of relative intensity bands for IκBα (14.1%) and a corresponding reduction in the values of relative intensity bands for p65 (34.8%; Fig. 5a, b: lanes 9, 10).
MAG anti-inflammatory effects on brain III. NF-κB activation. Western blots and densitometric analysis of the NF-κB pro-inflammatory subunit p65 in nuclear extracts (a) and the NF-κB inhibitory protein IκBα in cytosolic extracts (b) of prefrontal cortex samples of control (Ctr), stressed during 6 h (S), and stressed + Mangiferin at increasing doses of 15, 30, and 60 mg/Kg, respectively (MAG15, MAG30, MAG60) Wistar rats. Data are normalized by SP-1 (lower band) and are representative of three experiments. *p < 0.05 versus Ctr; # p < 0.05 versus S (One-way ANOVA following Newman-Keuls posttest). AU arbitrary units
Discussion
The present series of experiments demonstrate that administration of MAG prevents the over-accumulation of some pro-inflammatory mediators and the resultant oxidative damage produced by acute exposure to restraint stress in rat prefrontal cortex. Previous studies have demonstrated the molecular neuroprotective effects for the Mangifera indica L. extract (Vimang) but most of them are limited to in vitro models and it is not possible to determine whether the effects reported are attributable to MAG. From this point of view, our study constitutes a novel and relevant approach, taking into account the experimental design and the variables studied and the use of pure MAG.
Our first findings suggest relevant and possibility-related effects of MAG on glucocorticoids (GCs) and IL-1β plasma levels. Remarkably, in the case of GCs, this inhibitory effect was already produced by the low dose, showing a dose-independent response. GCs are classically considered anti-inflammatory, immunosuppressive and immunomodulatory under standard conditions [34, 35]. However, in recent years, the classic view that glucocorticoids are universally anti-inflammatory has been challenged at a variety of levels, mainly in the CNS. Thus, in the brain, GCs are not uniformly anti-inflammatory, and can even be pro-inflammatory at the level of cell extravasation and migration as well as inflammatory messenger, and transcription factor levels [36]. In the CNS, prior exposure to GCs can result in a “priming” of the immune response to a subsequent inflammatory challenge. It has been proven that high stress concentrations of corticosterone exacerbate excitotoxin-induced increases in IL-1β and TNF-α mRNA and protein levels both in vivo and in vitro [37, 38]. Consequently, stress-secreted glucocorticoids act as pro-inflammatory mediators in the CNS. In addition, GCs induce the expression of enzymes related to prostaglandin and leukotriene synthesis, molecules that are closely related to the generation of the inflammatory process [39]. Taking into account all these evidences, a reduction in GCs plasma levels by the administration of MAG could be contributing to moderate the central effects of GCs in relation with the neuroinflammatory response and the accumulation of oxidative/nitrosative parameters. To our knowledge, this is the first report showing this negative modulation of MAG on the stress response. Further studies are necessary to elucidate the mechanisms implicated although its capacity to inhibit IL-1β plasma levels needs to be further explored, taking into account the stimulating effects of IL-1β on HPA axis glucocorticoids secretion [40, 41].
It is worth noting the necessity to elucidate if MAG effects on these and others peripheral mediators could be contributing to its anti-inflammatory/antioxidant effects in prefrontal brain, in fact as animals have not been perfused in our study, residual blood in brain could be a potential confounder. Similarly, the possibility that MAG could be affecting other areas of the brain that might signal to the prefrontal cortex and be responsible for the observed protective effects, needs to be further investigated.
Higher doses of MAG also modulated plasma IL-1β levels. It has been demonstrated that the CNS is able to respond to peripheral inflammatory stimuli mounting a local inflammatory response called neuroinflammation: circulating or endothelial-derived cytokines can transduce a signal to neurons via substances such as NO or prostanoids; these are synthesized by iNOS and COX-2, whose transcription is induced by IL-1β among other cytokines [42]. Indeed, circulating IL-1 β can activate the endothelium to synthesize additional IL-1β, leading to signal amplification [43]. Thus, an IL-1β-mediated inflammatory signal can be transduced from the blood stream into neurons [44] and these, together with astrocytes, microglia and oligodendrocytes, can themselves produce inflammatory mediators [45]. In this sense, the inhibition by MAG of IL-1β systemic levels constitutes another added effect that could be improving the potential neuropathological events produced during acute stress exposure.
Interestingly, both GCs and IL-1β over-activation have been related to memory and learning deficits [46]. It remains to be demonstrated whether the recently demonstrated MAG nootropic effects [23, 24] are dependent of its inhibitory role on GCs and IL-1β synthesis here reported.
Moreover, we determined the action of MAG on some variables involved in brain redox balance. Our results show that acute stress induces a decrease in total antioxidant activity (TAOS), as well as a depletion of catalase levels and an increase in lipid peroxidation. These findings coincide with previous reports obtained in this experimental model [3], and they have been directly related to the augment of oxidative/nitrosative species also demonstrated after acute stress exposure. The higher doses of MAG revert the unbalanced redox state, increasing TAOS and catalase levels, and decreasing lipid peroxidation. The antioxidant activity of MAG has been widely demonstrated in in vitro systems, such as rat cortical neurons in culture and peritoneal rat macrophages [47, 48]. Besides, MAG presents a low redox potential related to its ROS scavenger ability [49]. This way, the protective effect of the polyphenol on redox variables in brain cortex could be a consequence not only of a peripheral stabilization of glucocorticoids and IL-1β levels but also of a central scavenger activity of MAG on stress-derived oxidative/nitrosative species over-accumulation.
Closely related with its antioxidant properties, MAG is able to inhibit iNOS and COX-2 expression in the prefrontal cortex of stressed rats. Both enzymes are considered important sources of oxidative and nitrosative metabolites and pro-inflammatory prostanoids (PGE2), respectively, and their induction is related to the previous release of cytokines (TNF-α) and NF-κB activation [11, 50]. Our results demonstrated that MAG administration decreased iNOS expression, and in the case of COX-2, the reduction was even more evident because it occurred from the low dose. Previous studies have demonstrated the in vitro inhibition of iNOS and COX-2 expression for Vimang, as well as the in vitro (microglial cells) and in vivo inhibition of NO· [51, 52]. Likewise, it has been reported that various polyphenols (notably those present in green tea) are capable of inhibiting COX-2 expression in diverse cell types [53, 54]. In this sense, although the results here reported regarding iNOS and COX-2 expression, could be tightly linked to systemic reduction in GCs and IL-1β levels, we cannot discard a possible direct effect of MAG on both enzymes, more, if we take into account the different MAG’s effectiveness to inhibit each one.
The MAG neuroprotective activity described in this stress model could be attributable to its ability to modulate calcium influx in neuronal cells [22] taking into account that acute restraint exposure increases extracellular glutamate levels that bind to its ionotropic NMDA receptor, whose over-activation causes a dramatic increase in intracellular Ca2+ levels, which then activates Ca2+-dependent enzymes (e.g., proteases, lipases, peroxidases) and eventually leads to neuronal death [55].
On the other hand, one of the most important mediators involved in stress pathological pathways that is directly associated with iNOS and COX-2 expression is TNF-α. In the CNS, resident macrophages, astrocytes, and microglia are able to synthesize and release TNF-α, which seems to be pro-inflammatory during the acute phase of CNS inflammatory responses [56]. TNF-signaling pathways are mediated by two receptors, TNF-R1 and TNF-R2. Both isoforms are expressed in the CNS, and it is assumed that TNF-R1 activation initiates signals leading to neuronal apoptosis [57]. Furthermore, TNF-Rs share some signaling pathways with IL-1RI, the primary IL-1 receptor. These signaling pathways include NF-κB. Previous studies, using a model of acute immobilization stress, have shown increased levels of soluble TNF-α levels in brain cortex after 1-h stress [58] and changes in TNF-R1 and TNF-R2 protein expression after subacute immobilization stress in rats, correlating these findings with other pro-inflammatory events elicited by stress exposure in rat prefrontal cortex [59]. Similarly, our results exhibited an increase in TNF-α and TNF-R1 expression in brain cortex after acute immobilization stress (6 h). Preceding studies in inflammation-related models, such as septic shock and LPS-stimulated microglial cell lines, demonstrated the inhibitory effect of MAG on TNF-α in serum levels and down-regulation of TNF-α mRNA expression [52]. In our work, previous treatment with MAG produced a parallel reduction in TNF-α and TNF-R1 expression in brain cortex, but only at the higher dose. As mentioned previously, glucocorticoids released by stress induce pro-inflammatory cytokines and cytokine receptors expression. Interestingly, for these targets, the stronger inhibition of GCs plasma levels observed for MAG at lowest doses is not translated into a protective effect on rat brain cortex.
Finally, we analyzed the expression of NF-κB and its possible modulation by MAG. Activation of brain NF-κB is one of the earliest events in the stress-induced neuroinflammatory response in animal models [58]. Consequently, NF-κB is considered the central regulator of the stress response since it regulates the transcription of many acute-phase proteins and inflammatory genes, such as iNOS or COX-2 [55]. Later studies have shown the induction of NF-κB in humans too, after the exposure to psychological stress (free speech and a mental arithmetic task) [8]. This activation appears to be included in the complex mechanisms that constitute the general stress response, and it is regulated by pro-inflammatory cytokines (IL-1β and TNF-α) released after stress [9]. Our results show an activation of NF-κB pathway, expressed as an increase of its p65 subunit in nucleus and a decrease of its inhibitory protein IκB in cytosol. MAG modulation of TNF-α could be related to its inhibitory effects on NF-κB pathway, taking into account that NF-κB activation by stress is dependent on TNF-α [9]. In agreement with our results, MAG negatively regulates NF-κB activation in mouse neuronal populations, both in vivo and in vitro [23, 47, 60].
In summary, MAG exerts a protective action in brain after acute immobilization stress. These effects may be related on the one hand, with the strong inhibition exhibited by the compound on the systemic levels of glucocorticoids and IL-1β and on the other, with a possible modulation of redox parameters and inflammation-related mediators in SNC. MAG emerges as an attractive multifaceted neuroprotective strategy for the treatment for diverse neuropsychiatric pathologies with HPA axis dysregulation and an oxidative/neuroinflammatory component in their pathophysiology.
References
Madrigal JLM, Caso J, Hurtado O et al (2004) Brain oxidative markers in stress. Possible new drug targets against neuroinflammation. Curr Neuropharmacol 2:183–189
García-Bueno B, Caso J, Pérez-Nievas BG et al (2006) Effects of peroxisome proliferator-activated receptor gamma agonists on brain glucose and glutamate transporters after stress in rats. Neuropsychopharmacology 32:1251–1261
García-Bueno B, Caso JR, Leza JC (2008) Stress as a neuroinflammatory condition in brain: damaging and protective mechanisms. Neurosci Biobehav Rev 32:1136–1151
Shelton RC, Claibome J, Sidoryk-Wegrzynowicz M et al (2010) Altered expression of genes involved in inflammation and apoptosis in frontal cortex in major depression. Mol Psychiatry (Epublication ahead of print version)
Galasko D, Montine TJ (2010) Biomarkers of oxidative damage and inflammation in Alzheimer’s disease. Biomark Med 4:27–36
Zunszain PA, Anacker C, Cattaneo A et al (2010) Glucocorticoids, cytokines and brain abnormalities in depression. Prog Neuropsychopharmacol Biol Psychiatry (Epublication ahead of print version)
Potvin S, Stip E, Sepehry AA, Gendron A et al (2008) Inflammatory cytokine alterations in schizophrenia: a systematic quantitative review. Biol Psychiatry 63:801–808
Bierhaus A, Wolf J, Andrassy M et al (2003) A mechanism converting psychosocial stress into mononuclear cell activation. Proc Natl Acad Sci USA 100:1920–1925
Madrigal JL, Hurtado O, Moro MA et al (2002) The increase in TNF-alpha levels is implicated in NF-kappaB activation and inducible nitric oxide synthase expression in brain cortex after immobilization stress. Neuropsychopharmacology 26:155–163
Madrigal JL, Olivenza R, Moro MA et al (2001) Glutathione depletion, lipid peroxidation and mitochondrial dysfunction are induced by chronic stress in rat brain. Neuropsychopharmacology 24:420–429
Olivenza R, Moro MA, Lizasoain I et al (2000) Chronic stress induces the expression of inducible nitric oxide synthase in rat brain cortex. J Neurochem 74:785–791
Pacher P, Beckman JS, Liaudet L (2007) Nitric oxide and peroxynitrite in health and disease. Physiol Rev 87:315–324
Keller JN, Mattson MP (1998) Roles of lipid peroxidation in modulation of cellular signaling pathways, cell dysfunction, and death in the nervous system. Rev Neurosci 9:105–116
McEwen BS (2008) Central effects of stress hormones in health and disease: understanding the protective and damaging effects of stress and stress mediators. Eur J Pharmacol 583(2–3):174–185
Chi CW, Wang CN, Lin YL et al (2005) Tournefolic acid B methyl ester attenuates glutamate-induced toxicity by blockade of ROS accumulation and abrogating the activation of caspase and JNK in rat cortical neurons. J Neurochem 92:692–700
Kanada A, Nishimura Y, Yamaguchi JY et al (2005) Extract of Ginkgo biloba Leaves attenuates kainate-induced increase in intracellular Ca2+ concentration of rat cerebellar granule neurons. Biol Pharm Bull 28:934–936
Núñez Selles AJ, Velez H, Aguero J et al (2002) Isolation and quantitative analysis of phenolic antioxidants, free sugars, and polyols from mango (Mangifera indica L.) stem bark aqueous decoction used in Cuba as nutritional supplement. J Agric Food Chem 50:762–766
Nuñez AJ, Durruthy MD, Rodríguez E et al (2007) Comparison of major and trace element concentration in sixteen varieties of Cuban mango stem bark (Mangifera indica L.). J Agric Food Chem 55:2176–21781
Martínez G, Delgado R, Perez G et al (2000) Evaluations of the in vitro antioxidant activity of Mangifera indica L. extract (Vimang). Phytother Res 14:424–427
Garrido G, González D, Delporte C et al (2001) Analgesic and anti-inflammatory effects of Mangifera indica L. extract (Vimang). Phytother Res 15:18–21
Márquez L, Pérez-Nievas BG, Gárate I et al (2010) Anti-inflammatory effects of Mangifera indica L. extract in a model of colitis. World J Gastroenterol 16:4922–4931
Gottlieb M, Leal-Campanario R, Campos-Esparza MR et al (2006) Neuroprotection by two polyphenols following excitotoxicity and experimental ischemia. Neurobiol Dis 23:374–386
Jung K, Lee B, Han SJ et al (2009) Mangiferin ameliorates scopolamine-induced learning deficits in mice. Biol Pharm Bull 32:242–246
Pardo Andreu GL, Maurmann N et al (2010) Mangiferin, a naturally occurring glucoxilxanthone improves long-term object recognition memory in rats. Eur J Pharmacol 635:124–128
Liu Y, Xu F, Zeng X et al (2010) Application of a liquid chromatography/tandem mass spectrometry method to pharmacokinetic study of mangiferin in rats. J Chromatogr B Anal Technol Biomed Life Sci 878:3345–3350
Hou Y, Fan S, Zhang H et al (2010) Pharmacokinetic study of mangiferin in rat plasma and retina using high-performance liquid chromatography. Mol Vis 16:1659–1668
Yu-Juan L, Ying-Jie S, Yue-Han D, Yu-Lin DLC (2008) Determination and pharmacokinetics study of mangiferin in rat plasma and tissues. Chromatographia 67(11–12):957–960
Bhattacharya SK, Ghosal S, Chaudhuri RK, Sanyal AK (1972) Canscora decussata (Gentianaceae) xanthones. 3. Pharmacological studies. Pharm Sci 61(11):1838–1840
Leza JC, Salas E, Sawicki G et al (1998) The effects of stress on homeostasis in JCR-LA-cp rats: the role of nitric oxide. J Pharmacol Exp Ther 286:1397–1403
de Pablos RM, Villarán RF, Argüelles S et al (2006) Stress increases vulnerability to inflammation in the rat prefrontal cortex. J Neurosci 26:709–719
Radley JJ, Williams B, Sawchenko PE (2008) Noradrenergic innervation of the dorsal medial prefrontal cortex modulates hypothalamo-pituitary-adrenal responses to acute emotional stress. J Neurosci 2:5806–5816
Das NP, Ratty AK (1987) Studies on the effects of the narcotic alkaloids, cocaine, morphine, and codeine on nonenzymatic lipid peroxidation in rat brain mitochondria. Biochem Med Metabol Biol 37:258–264
Schreiber E, Matthias P, Müller MM et al (1989) Rapid detection of octamer binding proteins with ‘mini-extracts’, prepared from a small number of cells. Nucleic Acid Res 17:6419
Li M, Wang Y, Guo R et al (2007) Glucocorticoids impair microglia ability to induce T cell proliferation and Th1 polarization. Immunol Lett 109:129–137
Nair A, Hunzeker J, Bonneau RH (2007) Modulation of microglia and CD8(+) T cell activation during the development of stress-induced herpes simplex virus type-1 encephalitis. Brain Behav Immun 21:791–806
Sorrells SF, Sapolsky RM (2007) An inflammatory review of glucocorticoid actions in the CNS. Brain Behav Immun 21:259–272
Dinkel K, MacPherson A, Sapolsky RM (2003) Novel glucocorticoid effects on acute inflammation in the CNS. J Neurochem 84:705–716
MacPherson A, Dinkel K, Sapolsky R (2005) Glucocorticoids worsen excitotoxin- induced expression of pro-inflammatory cytokines in hippocampal cultures. Exp Neurol 194:376–383
Garcia-Fernandez LF, Iniguez MA, Eguchi N et al (2000) Dexamethasone induces lipocalin-type prostaglandin D synthase gene expression in mouse neuronal cells. J Neurochem 75:460–470
Besedovsky H, del Rey A, Sorkin E et al (1986) Immunoregulatory feedback between interleukin-1 and glucocorticoid hormones. Science 233:652–654
Sapolsky R, Rivier C, Yamamoto G et al (1987) Interleukin-1 stimulates the secretion of hypothalamic corticotropin-releasing factor. Science 238:522–524
Bartfai T, Sánchez-Alavez M, Andell-Jonsson S et al (2007) Interleukin-1 system in CNS stress: seizures, fever, and neurotrauma. Ann N Y Acad Sci 1113:173–177
Skinner RA, Gibson RM, Rothwell NJ et al (2009) Transport of interleukin-1 across cerebromicrovascular endothelial cells. Br J Pharmacol 156:1115–1123
Licinio J, Wong ML (1997) Pathways and mechanisms for cytokine signaling of the central nervous system. J Clin Invest 100:2941–2947
Lucas SM, Rothwell NJ, Gibson RM (2006) The role of inflammation in CNS injury and disease. Br J Pharmacol 147:S232–S240
Song C, Phillips AG, Leonard B (2003) Interleukin 1 beta enhances conditioned fear memory in rats: possible involvement of glucocorticoids. Eur J Neurosci 18:1739–1743
Campos-Esparza MR, Sánchez-Gómez MV, Matute C (2009) Molecular mechanisms of neuroprotection by two natural polyphenols. Cell Calcium 45:358–368
García D, Delgado R, Ubeira FM et al (2002) Modulation of rat macrophages function by the Mangifera indica L. extracts Vimang and mangiferin. Int Immunophar 2:797–806
Mishra B, Indira K, Sudheerkumar M et al (2006) Pulse radiolysis study of mangiferin: a C-glycosyl xanthone isolated from Mangifera indica. Rad Phys Chem 75:70–77
Madrigal JL, Moro MA, Lizasoain I et al (2003) Induction of cyclooxygenase-2 accounts for restraint stress-induced oxidative status in rat brain. Neuropsychopharmacology 28:1579–1588
Leiro J, García D, Arranza JA et al (2004) An Anacardiaceae preparation reduces the expression of inflammation-related genes in murine macrophages. Int Immunophar 4:991–1003
Garrido G, Delgado R, Lemus Y et al (2004) Protection against septic shock and suppression of tumor necrosis factor alpha and nitric oxide production on macrophages and microglia by a standard aqueous extract of Mangifera indica L. (VIMANG®). Role of mangiferin isolated from the extract. Pharmacol Res 50:165–172
Ahmed S, Rahman A, Hasnain A et al (2002) Green tea polyphenol epigallocatechin-3-gallate inhibits the IL-1 beta-induced activity and expression of cyclooxygenase-2 and nitric oxide synthase-2 in human chondrocytes. Free Radic Biol Med 33:1097–1105
Hong J, Smith TJ, Ho CT et al (2001) Effects of purified green and black tea polyphenols on cyclooxygenase and lipoxygenase dependent metabolism of arachidonic acid in human colon mucosa and colon tumor tissues. Biochem Pharmacol 62:1175–1183
Madrigal JL, García-Bueno B, Caso JR et al (2006) Stress-induced oxidative changes in brain. CNS Neurol Disord Drug Targets 5:561–568
Allan SM, Rothwell NJ (2003) Inflammation in central nervous system injury. Phil Trans R Soc Lond B Biol Sci 358:1669–1677
Hallenbeck JM (2002) The many faces of tumor necrosis factor in stroke. Nat Med 8:1363–1368
Madrigal JL, Moro MA, Lizasoain I et al (2001) Inducible nitric oxide synthase expression in brain cortex after acute restraint stress is regulated by nuclear factor kappaB-mediated mechanisms. J Neurochem 76:532–538
Caso JR, Lizasoain I, Lorenzo P et al (2006) The role of TNF α in stress-induced worsening of cerebral ischaemia in rats. Neuroscience 142:59–69
Leiro J, Arranz JA, Yáñez M et al (2004) Expression profiles of genes involved in the mouse nuclear factor-kappa B signal transduction pathway are modulated by mangiferin. Int Immunopharmacol 4:763–778
Acknowledgments
Supported by Spanish Ministry of Education (MEC, SAF07-63138), the Instituto de Salud Carlos III, Centro de Investigación en Red de Salud Mental, CIBERSAM, and Foundation Santander-UCM (GR 58/08). Lucía Márquez is recipient of a fellowship from Programme Alßan, European Commission.
Conflict of interest
The authors declare that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Márquez, L., García-Bueno, B., Madrigal, J.L.M. et al. Mangiferin decreases inflammation and oxidative damage in rat brain after stress. Eur J Nutr 51, 729–739 (2012). https://doi.org/10.1007/s00394-011-0252-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-011-0252-x