Abstract
Objectives
Poor sleep quality is common in patients with chronic heart failure (CHF). This study tested the hypothesis that adaptive servo-ventilation (ASV) therapy in CHF patients whose central sleep apnoea (CSA) was not suppressed by continuous positive airway pressure (CPAP) (CPAP-non-responders) would improve sleep quality compared to CPAP-responders receiving ongoing CPAP therapy.
Methods
Eighty-two patients with CHF (65 ± 9 years, left ventricular ejection fraction 35 ± 16 %) and CSA [apnoea–hypopnoea index (AHI) ≥15/h] were retrospectively studied. Within an average of 47 days, patients were reevaluated on CPAP therapy and stratified according to their suppression of CSA: 34 were CPAP-non-responders switched to ASV therapy the following day and 48 were CPAP-responders who continued on CPAP therapy. Polysomnographic parameters were assessed in the diagnostic night and on the last night of PAP therapy (CPAP or ASV) before the patient was discharged with the final pressure settings.
Results
Compared with the CPAP group, the ASV group had significantly greater reductions from baseline in AHI (−37 ± 15/h vs −28 ± 18/h, p = 0.02), arousal index (−12.7 ± 13.6/h vs −6.8 ± 12.5/h, p = 0.04) and sleep stage N1 (−9 ± 14 % vs −2 ± 12 %, p = 0.03). In addition, the ASV group gained significantly more rapid eye movement (REM) sleep compared with the CPAP group (+5 ± 9 % vs +1 ± 9 %, p = 0.02).
Conclusions
CPAP therapy is effective in reducing AHI in a significant proportion of CHF patients with reduced ejection fraction and CSA. Treatment of CSA with ASV in CHF patients reduces sleep fragmentation and improves sleep structure to a significantly greater extent than changes seen in responders to CPAP therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Central sleep apnoea (CSA) is highly prevalent in patients with chronic heart failure (CHF) [1, 2] and increases mortality risk in such patients, independent of heart failure (HF) severity [3]. These patients have fragmented sleep due to multiple factors such as sleep apnoea, periodic limb movements, severity of HF and depression. Standardized scoring of the electroencephalogram (EEG) as part of in-lab polysomnography allows to quantify sleep (e.g. total sleep time and sleep efficiency), sleep stages [stage N1, stage N2, stage N3 and rapid eye movement (REM) sleep] as well as the degree of sleep fragmentation (arousals from sleep). Poor sleep efficiency is associated with mortality in patients with CHF and CSA [4]. Therefore, sleep quality may be an important treatment target to improve quality of life and prognosis in these patients. Evaluation of response to therapy often includes assessment of the extent to which sleep fragmentation and structure improve, as measured by a reduction in the arousal index (ArI) or the relative time in stage N1 sleep or by an increase in the time in stage N3 or REM sleep.
It is well documented that treatment with continuous positive airway pressure (CPAP) effectively suppresses obstructive sleep apnoea, reduces sleep fragmentation and restores normal sleep structure in patients without cardiac disease [5, 6]. In contrast, the effects of CPAP and adaptive servo-ventilation (ASV) on sleep fragmentation and sleep structure in CHF patients with CSA are not completely understood. In a randomized clinical trial of CPAP in patients with HF and CSA, the Canadian Continuous Positive Airway Pressure for Patients with Central Sleep Apnea and Heart Failure (CANPAP) trial, the primary outcome transplant-free survival was similar in the CPAP compared to the control group [7]. One potential reason for the neutral result was that CPAP suppressed the apnoea–hypopnoea index (AHI) to <15/h of sleep in only 57 % of patients [7, 8]. Even in a subgroup of patients, in whom AHI was effectively suppressed by CPAP (CPAP-responders), there were no significant changes in arousal frequency, sleep efficiency or sleep structure [9]. Authors concluded that arousals were not mainly a consequence of CSA, and may not have been acting as a defense mechanism to terminate apnoeas in the same way they do in obstructive sleep apnoea [9].
On the one hand, ASV is regarded as the most effective therapy for suppressing CSA in CHF patients [10–12]. Therefore, ASV was usually used in CHF patients who had persistent CSA despite CPAP therapy. Small studies of CHF patients with CSA suggest that suppression of CSA by ASV is paralleled by a reduction in arousals and an improvement in sleep structure [13].
On the other hand, there is evidence that automatically titrating CPAP devices do not reduce blood pressure as effective as the application of fixed CPAP [14]. The mechanism could be that variations of PAP during the night as applied by automatically titrating CPAP devices may trigger arousals from sleep [15]. Whether the variable inspiratory pressure support of ASV devices may promote arousals from sleep has not been studied before.
Therefore, we tested the hypothesis that ASV therapy would improve sleep quality in CHF patients whose CSA was not suppressed by CPAP (CPAP-non-responders) compared to CPAP-responders receiving ongoing CPAP therapy.
Methods
Patients
To test this hypothesis, sleep fragmentation and sleep structure, assessed by polysomnography (PSG), were retrospectively compared in patients with CHF and CSA who responded to CPAP and were receiving ongoing therapy or who did not respond to CPAP and were switched to ASV. Consecutive CHF patients referred to University Hospital Regensburg for PSG between January 2002 and October 2011 were eligible for inclusion. Inclusion criteria were: CHF secondary to ischaemic or non-ischaemic cardiomyopathy with objective evidence of systolic dysfunction (LVEF ≤ 50 %) measured by echocardiography within 3 months prior to the sleep study; stable clinical status and stable optimal medical therapy for ≥4 weeks; CSA, defined as AHI ≥15/h with >50 % of all apnoeas being of a central nature; and patient consent to be treated with positive airway pressure (PAP) therapy. Exclusion criteria were: CHF due to valvular heart disease, listing for heart transplantation, known concurrent terminal illness (e.g. severe pulmonary disease, cancer), and oxygen therapy or current treatment with PAP. This retrospective analysis was approved by the ethics committee of the University of Regensburg (approval no. 12-101-0144), and was conducted in accordance with Good Clinical Practice and the principles of the Declaration of Helsinki.
Polysomnography
PSG was performed in all subjects using standard techniques [3]. During PSG, body position, eye and leg movements, cardiotachography, nasobuccal airflow, chest and abdominal effort, electroencephalogram (EEG) monitoring, and arterial oxyhaemoglobin saturation (SaO2) assessed by pulse oximetry were recorded (Alice 3.5, Respironics, Pittsburgh, USA). Sleep stages were determined according to the American Academy of Sleep Medicine (AASM) Manual 2007 [16]. Apnoea was defined as a cessation of inspiratory airflow of ≥10 s. Hypopnoea was defined as a ≥30 % reduction in nasal air flow lasting ≥10 s resulting in a ≥4 % drop in oxygen saturation for ≥90 % of the event duration [16]. AHI was defined as the number of apnoeas or hypopnoeas per hour of sleep. The oxygen desaturation index (ODI) was defined as the number of ≥4 % oxygen desaturations per hour of sleep. Time in bed (TIB) was defined as the timespan between lights off and lights on recorded by PSG laboratory staff, and total sleep time (TST) was defined as the total time subjects spent in sleep stages N1–N3 and REM sleep recorded by EEG monitoring. Sleep efficiency is the proportion of sleep in the recorded period and was calculated by dividing TST by TIB, and expressed as a percentage.
Arousals were defined as an abrupt shift of EEG frequency including alpha, theta and/or frequencies >16 Hz (but no spindles) that lasted ≥3 s, with ≥10 s of stable sleep preceding the change. Scoring of arousals during REM sleep required a concurrent increase in submental electromyography lasting ≥1 s. Frequency of arousals per hour of sleep was defined as the arousal index (ArI).
Initiation of therapy
After the diagnostic PSG, standard clinical procedure was CPAP initiation using PSG monitoring. CPAP was initially set to 4 cmH2O and then titrated upwards in 1 cmH2O increments until any sign of flow limitation was eliminated, or maximum patient tolerance was reached (≤10 cmH2O).
Within an average of 47 days, patients were reevaluated on CPAP therapy and stratified according to their suppression of CSA: before the CANPAP study results were published, patients whose AHI could not be suppressed to <10/h during CPAP therapy were switched to ASV [8, 13]; after publication of the CANPAP trial [8], patients whose AHI was suppressed to <15/h and reduced by ≥50 % during CPAP therapy were defined as responders, and continued with CPAP therapy. In this study, patients whose AHI could not be suppressed below thresholds described above were defined as CPAP-non-responders, and switched to ASV the following day after CPAP reevaluation [7, 8, 13]. The expiratory PAP of the ASV device was set to the level determined to suppress upper airway obstruction and flow limitation during CPAP titration. The minimum inspiratory PAP was set to the expiratory PAP level, and the maximum inspiratory PAP to a maximum of 10 cmH2O above the expiratory PAP. The default automatic back-up rate of the device was used.
Outcome
PSG parameters were assessed in the diagnostic night and on the last night of PAP therapy (CPAP or ASV) before the patient was discharged with the final pressure settings for long-term PAP therapy.
Statistical analysis
Continuous data are expressed as mean ± standard deviation (SD), unless otherwise stated. Baseline patient characteristics in the two groups were compared using two-sided t tests for continuous variables, and by Chi square tests for nominal variables. If the expected counts were <5, Fisher exact test was used. Change in outcome variable values within the baseline and the final treatment groups was tested with paired samples t test. p values of between-group differences were tested with analysis of covariance. A two-sided p value of <0.05 was considered statistically significant. All analyses were performed using SPSS Statistic software version 20.0 (IBM, Corp., New York).
Results
Patients
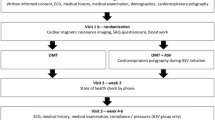
Four-hundred and seventy-seven consecutive patients with CHF underwent diagnostic PSG in the sleep laboratory and were tested for eligibility (Fig. 1). The most common causes for exclusion from the analysis were preserved LVEF (≥50 %; n = 89) and no SDB (AHI ≤ 15/h; n = 93). The reminder reasons for exclusion are listed in Fig. 1. The final analysis included 82 patients with CHF and CSA. Of these, 48 patients were treated with CPAP and 34 with ASV. Groups were generally similar at baseline, but patients in the ASV group were significantly older and were somewhat more likely to be receiving β-blockers than those in the CPAP group (Table 1).
Sleep and apnoea characteristics at baseline
Overall, baseline apnoea and sleep characteristics were similar in CPAP-responder and ASV patients, apart from a higher proportion of N2 sleep and a lower proportion of N3 sleep in ASV vs CPAP recipients (Table 2).
Breathing and sleep parameters
AHI, cAI and ArI values decreased significantly from baseline during CPAP or ASV therapy (Table 3). However, reductions in AHI, cAI and ArI were significantly greater in ASV recipients compared with the CPAP-responder group (Table 3; Fig. 2a).
Between-group differences in the effects of treatment on breathing (a) and sleep (b) parameters. CPAP-responders were treated with CPAP (white bars) and CPAP-non-responders received adaptive servo-ventilation (ASV; black bars). AHI apnoea–hypopnoea index, ArI arousal index, ASV adaptive servo-ventilation, cAI central apnoea index, CPAP continuous positive airway pressure, N1 sleep stage N1, N2 sleep stage N2, N3 sleep stage N3, REM rapid eye movement sleep, ∆ change from diagnostic PSG to the last PSG on treatment prior to discharge on long-term therapy. Error bars represent ± standard error
With respect to sleep structure, patients treated with ASV had a significant reduction in N1 sleep and a significant increase in REM sleep, while these parameters remained stable in the CPAP-responder group. ASV reduced stage N1 sleep (Fig. 2b) and increased REM sleep (Fig. 2b) to a significantly greater extent than CPAP. Time spent in N3 sleep significantly increased only in the CPAP-responder group (Table 3).
Discussion
This analysis of CHF patients with predominant CSA has identified several novel findings. ASV treatment decreased the number of arousals from sleep in patients who had not responded to CPAP therapy, and this decrease was significantly greater than that seen in CPAP recipients who responded to therapy. In addition, ASV treatment in CHF patients with CSA reduced the time spent in sleep stage N1 and increased time spent in REM sleep to a significantly greater extent than CPAP treatment. Findings suggest that ASV is better than CPAP at reducing sleep fragmentation and restoring a normal sleep structure.
Importantly, findings of this study have to be interpreted in the light of the recently released preliminary results from the SERVE-HF trial [17] (ISRCTN19572887), which is a multinational, multi-center, randomized controlled trial designed to assess whether treatment of predominantly CSA with ASV therapy reduces mortality and morbidity in patients with CHF). Findings indicate that study participants who received ASV therapy as treatment for moderate to severe predominant CSA had an increased risk of cardiovascular mortality compared to the control group [18, 19]. Mechanism that explains this unexpected result remains unclear [20]. Malhotra et al. remark in their comment that the new results should not be seen as a disappointment but rather as a call for intensifying the research efforts in this area [20].
In the present analysis, ASV treatment of CSA in CHF patients who did not respond to CPAP reduced arousal frequency by approximately 32 %, while CPAP treatment in the CPAP-responder group only reduced arousal frequency by 14 %. Published data on the effects of CPAP and ASV therapy on the number of arousals from sleep are heterogeneous. Randerath et al. showed similar effects of CPAP and ASV therapy on the arousal index (ArI) [21], which might be due to the fact that, in contrast to our study, both groups had a high proportion of obstructive apnoeas and hypopnoeas. Teschler et al., who studied CHF patients with severe CSA and Cheyne Stokes respiration (CSR), found a 23 % higher reduction in the number of arousals with ASV therapy compared to CPAP [10]. Similar effects were observed in non-randomised trials comparing the effects of CPAP and ASV in patients with CHF and CSA, showing 23–26 % greater decreases in the ArI during ASV therapy [13, 22]. None of the above studies, nor the present study, reported respiratory vs movement arousals [10, 13, 22]. To date, no studies have compared CPAP-responders treated with CPAP and CPAP-non-responder treated with ASV. Therefore, the findings of this study extend existing knowledge and highlight the superiority of ASV therapy in CPAP-non-responder compared to CPAP in CPAP-responders with respect to sleep fragmentation. Our findings do not support the concept that the variable inspiratory pressure support applied by ASV may trigger arousals from sleep.
In addition, patients treated with ASV had a significant reduction in sleep stage N1 and a significant increase in REM sleep compared to the CPAP group. Similar to these results, previous studies showed that CPAP therapy did not significantly influence the distribution of sleep stages [9, 10, 13]. Only Randerath et al. found a significant decrease in N1 sleep and a significant increase in N3 sleep, while there was no change in the proportion of REM sleep [21].
The observed reorganization of sleep stages on ASV therapy is consistent with other studies. Most of them also showed a decrease in sleep stage N1 and N2 and a shift to N3 and REM sleep [10, 13, 21–24]. This restoration of normal distribution of sleep stages favours improved sleep quality in CHF patients treated with ASV compared with CPAP.
The results of this study need to be interpreted in the context of several limitations. The retrospective design meant that data on daily usage of CPAP and ASV, and differentiation between movement and respiratory arousals were not available for analysis. Without usage of the data, the possibility that differences between the ASV and CPAP groups observed in this study were due to different treatment adherence cannot be excluded. Furthermore, there were no individuals with CHF but without CSA in our study, meaning that the effects of CPAP and ASV therapy in CHF patients can only be compared with previous studies. However, clear predictors for CPAP-response could not be identified. Similar to the previous subanalysis of the CANPAP trial [8], CHF patients without sufficient response to CPAP therapy tended to be older and having more severe CSA. One possible predictor for the failure of CPAP to suppress CSA could be increased LV filling pressure, which was not assessed in the CANPAP subanalysis or in the present study.
By design, this study cannot prove a causal relationship between sleep quality and cardiovascular outcome. E.g. sleep quality could be impaired by neurohumeral activation in patients with CHF and CSA [25, 26].
Conclusions
CPAP therapy is effective in reducing AHI in a significant proportion of CHF patients with reduced ejection fraction and CSA, indicating that a trial of CPAP may be a treatment option for some patients with CHF and CSA. This study showed that treatment of CSA with ASV in CHF patients reduces sleep fragmentation and improves sleep structure to a significantly greater extent than changes seen in responders to CPAP therapy. Data do not support that the variable inspiratory pressure support applied by the ASV device may trigger arousals from sleep.
References
Ferrier K, Campbell A, Yee B, Richards M, O’Meeghan T, Weatherall M, Neill A (2005) Sleep-disordered breathing occurs frequently in stable outpatients with congestive heart failure. Chest 128:2116–2122
Sin DD, Fitzgerald F, Parker JD, Newton G, Floras JS, Bradley TD (1999) Risk factors for central and obstructive sleep apnea in 450 men and women with congestive heart failure. Am J Respir Crit Care Med 160:1101–1106
Jilek C, Krenn M, Sebah D, Obermeier R, Braune A, Kehl V, Schroll S, Montalvan S, Riegger GA, Pfeifer M, Arzt M (2011) Prognostic impact of sleep disordered breathing and its treatment in heart failure: an observational study. Eur J Heart Fail 13:68–75
Reinhard W, Plappert N, Hengstenberg C, Riegger GA, Novack V, Maimon N, Pfeifer M, Arzt M (2013) Prognostic impact of sleep duration and sleep efficiency on mortality in patients with chronic heart failure. Sleep Med 14:502–509
Loredo JS, Ancoli-Israel S, Kim E, Lim WJ, Dimsdale JE (2006) Effect of continuous positive airway pressure versus supplemental oxygen on sleep quality in obstructive sleep apnea: a placebo-CPAP-controlled study. Sleep 29:564–571
McArdle N, Douglas NJ (2001) Effect of continuous positive airway pressure on sleep architecture in the sleep apnea–hypopnea syndrome: a randomized controlled trial. Am J Respir Crit Care Med 164:1459–1463
Bradley TD, Logan AG, Kimoff RJ, Series F, Morrison D, Ferguson K, Belenkie I, Pfeifer M, Fleetham J, Hanly P, Smilovitch M, Tomlinson G, Floras JS (2005) Continuous positive airway pressure for central sleep apnea and heart failure. N Engl J Med 353:2025–2033
Arzt M, Floras JS, Logan AG, Kimoff RJ, Series F, Morrison D, Ferguson K, Belenkie I, Pfeifer M, Fleetham J, Hanly P, Smilovitch M, Ryan C, Tomlinson G, Bradley TD (2007) Suppression of central sleep apnea by continuous positive airway pressure and transplant-free survival in heart failure: a post hoc analysis of the Canadian Continuous Positive Airway Pressure for Patients with Central Sleep Apnea and Heart Failure Trial (CANPAP). Circulation 115:3173–3180
Ruttanaumpawan P, Logan AG, Floras JS, Bradley TD (2009) Effect of continuous positive airway pressure on sleep structure in heart failure patients with central sleep apnea. Sleep 32:91–98
Teschler H, Döhring J, Wang YM, Berthon-Jones M (2001) Adaptive pressure support servo-ventilation: a novel treatment for Cheyne-Stokes respiration in heart failure. Am J Respir Crit Care Med 164:614–619
Arzt M, Schroll S, Series F, Lewis K, Benjamin A, Escourrou P, Luigart R, Kehl V, Pfeifer M (2013) Auto-servo ventilation in heart failure with sleep apnea—a randomized controlled trial. Eur Respir J 42:1244–1254
Aurora RN, Chowdhuri S, Ramar K, Bista SR, Casey KR, Lamm CI, Kristo DA, Mallea JM, Rowley JA, Zak RS, Tracy SL (2012) The treatment of central sleep apnea syndromes in adults: practice parameters with an evidence-based literature review and meta-analyses. Sleep 35:17–40
Arzt M, Wensel R, Montalvan S, Schichtl T, Schroll S, Budweiser S, Blumberg FC, Riegger GA, Pfeifer M (2008) Effects of dynamic bilevel positive airway pressure support on central sleep apnea in men with heart failure. Chest 134:61–66
Patruno V, Aiolfi S, Costantino G, Murgia R, Selmi C, Malliani A, Montano N (2007) Fixed and autoadjusting continuous positive airway pressure treatments are not similar in reducing cardio-vascular risk factors in patients with obstructive sleep apnea. Chest 131:1395–1399
Marrone O, Insalaco G, Bonsignore MR, Romano S, Salvaggio A, Bonsignore G (2002) Sleep structure correlates of CPAP variations during application of an autotitration CPAP machine in obstructive sleep apnea syndrome. Chest 121:759–767
Iber C, Ancoli-Israel S, Chesson A, Quan SF; for the American Academy of Sleep Medicine (2007) The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications, 1st edn. American Academy of Sleep Medicine, Westchester, IL
Cowie MR, Woehrle H, Wegscheider K, Angermann C, d’Ortho MP, Erdmann E, Levy P, Simonds A, Somers VK, Zannad F, Teschler H (2013) Rationale and design of the SERVE-HF study: treatment of sleep-disordered breathing with predominant central sleep apnoea with adaptive servo-ventilation in patients with chronic heart failure. Eur J Heart Fail 15(8):937–943. doi:10.1093/eurjhf/hft051
American College of Cardiology (2015) Preliminary results of SERVE-HF Trial reveal increased CV mortality from ASV therapy. http://www.acc.org/latest-in-cardiology/articles/2015/05/15/11/38/preliminary-results-of-serve-hf-trial-reveal-increased-cv-mortality-from-asv-therapy. Accessed 15 May 2015
Federal Institute for Drugs and Medical Devices (BfArM). Urgent field safety notification/increased risk of cardiovascular death with adaptive servo-ventilation (ASV) therapy for patients with symptomatic chronic heart failure with reduced ejection fraction, ResMed Ltd. http://www.bfarm.de/SharedDocs/Kundeninfos/EN/12/2015/2968-15_Kundeninfo_en.pdf?__blob=publicationFile&v=2. Accessed 15 May 2015
Malhotra A, Patil S, Sands S, Ayas N (2015) Central sleep apnoea in congestive heart failure. Lancet Respir Med. doi:10.1016/S2213-2600(15)00235-0
Randerath WJ, Nothofer G, Priegnitz C, Anduleit N, Treml M, Kehl V, Galetke W (2012) Long-term auto servo-ventilation or constant positive pressure in heart failure and co-existing central with obstructive sleep apnea. Chest 142:440–447
Allam JS, Olson EJ, Gay PC, Morgenthaler TI (2007) Efficacy of adaptive servoventilation in treatment of complex and central sleep apnea syndromes. Chest 132:1839–1846
Campbell AJ, Ferrier K, Neill AM (2012) Effect of oxygen versus adaptive pressure support servo-ventilation in patients with central sleep apnoea-Cheyne Stokes respiration and congestive heart failure. Intern Med J 42:1130–1136
Zhang X, Yin K, Li X, Jia E, Su M (2006) Efficacy of adaptive servoventilation in patients with congestive heart failure and Cheyne-Stokes respiration. Chin Med J 119:622–627
Koyama T, Watanabe H, Tamura Y, Oguma Y, Kosaka T, Ito H (2013) Adaptive servo-ventilation therapy improves cardiac sympathetic nerve activity in patients with heart failure. Eur J Heart Fail 15(8):902–909
Calvin AD, Somers VK, van der Walt C, Scott CG, Olson LJ (2011) Relation of natriuretic peptide concentrations to central sleep apnea in patients with heart failure. Chest 140(6):1517–1523
Acknowledgments
Medical editing assistance was provided by Nicola Ryan, independent medical writer, funded by ResMed.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Michael Arzt has received unrestricted grant support from Philips Home Healthcare Solutions (Murrysville, PA, USA), ResMed (Martinsried, Germany) and the German Foundation for Cardiac Research (Deutsche Stiftung für Herzforschung). Michael Arzt is the holder of an endowed professorship from the Free State of Bavaria at the University of Regensburg that was donated by Philips Home Healthcare Solutions (Murrysville, PA, USA) and ResMed (Martinsried, Germany). Tatjana Roth, Andrea Hetzenecker, Christoph Birner, Lars S. Maier and Michael Pfeifer have reported that they have no potential conflicts of interest with any companies/organizations whose products or services may be discussed in this article. The content is entirely the responsibility of the authors, and sponsors had no role in the design or conduct of the study.
Additional information
A. Hetzenecker and T. Roth were contributed equally to this work.
Rights and permissions
About this article
Cite this article
Hetzenecker, A., Roth, T., Birner, C. et al. Adaptive servo-ventilation therapy of central sleep apnoea and its effect on sleep quality. Clin Res Cardiol 105, 189–195 (2016). https://doi.org/10.1007/s00392-015-0904-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-015-0904-6