Abstract
Background
AV nodal reentrant tachycardia (AVNRT) is commonly encountered in pediatric patients. Definite treatment can be achieved by catheter ablation. The purpose of the study was to evaluate the efficacy and safety of AVNRT ablation focusing on children with a body weight ≤25 kg.
Patients and results
Catheter ablation of AVNRT was attempted in 253 patients. Median age was 12.5 years; median body weight was 48.7 kg. 25 (9.9 %) children had a body weight ≤25 kg. Congenital heart disease was present in 6 patients (2.4 %). Procedural success was achieved in 98 % using radiofrequency, in 100 % using cryoenergy alone, and in 94 % using both energy sources. In patients with a body weight ≤25 kg, success was achieved in 96 %. In patients ≤25 kg, fluoroscopy and procedure duration did not differ from those >25 kg. The rate of major complications was significantly higher in the patients ≤25 kg (12 vs. 2.2 %, p = 0.04). Permanent AV block after RF ablation occurred in 2 patients with congenital heart disease and one infant with a body weight of 8.7 kg.
Conclusions
Catheter ablation of AVNRT in children and adolescents was safe and effective. Infants and small children with a body weight ≤25 kg had a higher prevalence of serious complications. This should alert physicians in decision making toward catheter ablation in these patients. In patients with congenital heart disease and different anatomy of the cardiac conduction system, operators must be aware of an increased risk for AV block.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Dual AV nodal pathways are the substrate for AV nodal reentrant tachycardia (AVNRT), a common type of supraventricular tachycardia (SVT) in children and adolescents. Catheter-based ablation of the tachycardia substrate by either radiofrequency (RF) or cryoenergy has been evolved as the treatment of choice in pediatric patients with an immediate success rate of up to 99 % [1–3]. Occurrence of major complications, in particular complete AV block requiring pacemaker implantation after RF ablation, however, has been reported in 1–3 % of children [1–6].
Up to now, data with respect to success and complications of AVNRT ablation in small children have not been published in a large series. Incidence of AVNRT in small children is lower than SVT mediated by accessory atrioventricular connections, as age-dependent incidence of AVNRT in pediatric patients ranges from 0 to 32 % [7]. There is, however, a substantial group of young patients with low body weight who suffer from recurrent drug-refractory AVNRT and who are therefore referred for catheter ablation. Besides the use of RF, the use of cryoenergy for ablation of various types of SVT substrates in small children has been reported recently. Cryoenergy was safe in ablation of SVT substrates in small children, but recurrence rate was significant [8].
Catheter ablation of AVNRT in small patients can be challenging and it may be hypothesized that the risk of AV block and other major complications increases with lower body weight due to smaller intracardiac dimensions. In patients with congenital heart disease, a different anatomy of the cardiac conduction system may increase the risk of inadvertent damage to those structures resulting in complete heart block requiring permanent pacemaker implantation. The aim of the present study was therefore to present data on catheter ablation of AVNRT in children and adolescents with a special focus on small children and patients with congenital heart disease.
Patients and methods
Patients
A total of 253 children and adolescents <20 years of age with AVNRT were referred to our tertiary center for electrophysiological study (EPS) and catheter ablation from October 2002 to May 2014. Data were collected from patients’ hospital records as well as the EPS protocols. The study was approved by the local ethics committee and fully complies with the Declaration of Helsinki.
Median age at the time of the procedure was 12.5 (3.7–19.3) years; median body weight was 49.1 (8.7–161) kg. In order to analyze the impact of body weight on efficacy and safety of the ablation procedure, patients were divided into subgroups either ≤25 or >25 kg. At catheter ablation, 25 (9.9 %) patients had a body weight of ≤25 kg, the remaining 228 patients had a body weight of >25 kg. Detailed biometrical and procedural data are provided in Table 1.
Significant congenital heart disease (CHD) was present in 6 patients (2.4 %; complex congenital heart disease n = 4, Ebstein’s anomaly of the tricuspid valve n = 2). Patients with repaired CHD and normal intracardiac anatomy (i.e., patients after surgical or catheter-guided closure of atrial or ventricular septal defects, closed PDA, s/p relief of aortic/pulmonic stenosis) were not considered to have CHD relevant to this study.
EPS and ablation protocol
Written informed consent was obtained prior to the procedure from the parents and/or patients. All antiarrhythmic medication was withdrawn at least 5 half-lives prior to the procedure. EPS was performed either under general anesthesia or under conscious sedation with propofol and ketamine, depending on body weight and co-morbidity, while patients with a body weight of <15 kg invariably were scheduled for general anesthesia. Vascular access was gained via the femoral vessels and/or the left antecubital vein or the right internal jugular vein.
In order to reduce fluoroscopy time and facilitate catheter guidance, a nonfluoroscopic catheter navigation system (LocaLisa®, Medtronic Inc., Minneapolis, USA, Ensite NavX®, St. Jude Medical, St. Paul, USA) was used in all cases. A decapolar electrode catheter was placed within the coronary sinus, a quadripolar electrode catheter at the His-bundle and either a quadripolar electrode catheter at the right ventricular apex (when using the Ensite NavX® system) or a bipolar electrode catheter screwed into the right ventricular septum (when using the LocaLisa® system).
In all patients, selective coronary angiography was performed prior to electrophysiological study and catheter ablation as a standard practice of care at our institution since RF ablation in the right posteroseptal space rarely may affect the right coronary artery after ablation of accessory pathways or AVNRT [9, 10]. Despite this complication occurring only on rare occasion, its possibility was taken seriously as AVNRT usually is not a life-threatening arrhythmia and indication for ablation is most often patients’/parents’ choice. Programed atrial and ventricular stimulation was performed to induce SVT and prove the presence of dual AV node physiology as described before [11, 12]. Isoproterenol provocation with a dosage of 0.01 µg/kg/min was used when necessary.
Dual AV node physiology was defined according to standard criteria [11]. For RF ablation, 5F (body weight ≤25 kg) or 7F (body weight >25 kg) deflectable quadripolar, nonirrigated RF ablation catheters with a 4-mm tip were used. RF ablation was performed in a temperature-controlled mode with a generator setting of 30–50 W at a target temperature of 65 °C. In patients with a body weight ≤25 kg, generator power setting was 30 W. For patients with a body weight >25 kg, primary power setting was 50 W. RF energy was applied for a maximum of 30 s. For cryoablation, a standard 7F quadripolar cryoenergy ablation catheter with either a 4-mm or a 6-mm tip was used. Cryomapping was performed as described before [3]. Cryoablation was performed at −70 °C for 4 min and was used since June 2003 at our institution.
Selection of the primary energy source was at the discretion of the individual operator (n = 4). In addition, cryoenergy was used in patients when RF application was deemed to be associated with a high risk of AV block. Vice versa, RF was used as the second energy source, when slow pathway ablation/modulation was unsuccessful after cryoenergy application.
RF and cryoablation of the slow pathway were performed with a combined anatomical/electrophysiological approach as described earlier [3, 12]. Aim of the procedure was modulation or ablation of the slow conducting pathway. Slow pathway modulation was defined as persistent anterograde conduction via the slow pathway after RF application allowing for a maximum of 1 atrial echo beat, whereas slow pathway ablation was defined as complete anterograde and retrograde loss of conductivity via the slow pathway [13]. As the rate of AVNRT recurrence does not correlate with residual slow pathway conduction [14, 15], either slow pathway ablation or slow pathway modulation as defined above was accepted as endpoint of ablation in any patient. Repeat stimulation protocol included isoproterenol provocation if needed before ablation. After a waiting period of 30 min, selective angiography of the coronary arteries was repeated to rule out coronary affection from RF or cryoenergy application in the right posteroseptal space.
Before discharge from the hospital, a standard EKG and a 24-h Holter monitor were obtained in all patients. Transthoracic echocardiography was performed to rule out pericardial effusion. All patients had regular follow-up visits with their referring pediatric cardiologist.
Complications
Major complications were defined as situations requiring additional diagnostic procedures or any specific therapy beyond standard procedural care. Any other observations like bruises or small local hematomas that did not prevent the patient being discharged as planned were considered to be insignificant.
Statistics
Data were analyzed using SPSS (version 21.0, IBM, Somers, NY, USA). Continuous data are displayed as median and interquartile range (IQR). Differences in categorical variables were calculated by χ 2 or Fischer’s exact test where appropriate. Differences in parametric data were calculated by Mann–Whitney U test. Bivariate correlation was tested using the Pearson correlation test. A p value <0.05 was considered significant.
Results
Indication for catheter ablation and procedural data
In a total of 253 patients, catheter ablation of AVNRT was performed between October 2002 and May 2014. Indication for EPS and consecutive catheter ablation was patients’ or parents’ preference in 73 % (n = 185) or drug-refractory SVT in 27 % (n = 68) of the patients. SVT had been documented in ECG in 71 % (n = 180) of the patients prior to ablation.
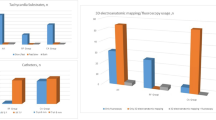
Basic biometrical and detailed procedural data are given in Table 1. Overall procedure duration was 177 (142–223) min (n = 253), and overall fluoroscopy time including coronary angiographies was 10.1 (7.2–14.7) min. Overall fluoroscopy dose including coronary angiographies was 3482 (2011–5861) cGy/m2.
Immediate procedural success (whole group)
Immediate success was achieved in 248 out of 253 patients (98 %). Slow pathway modulation was achieved in 140 patients (57 %), whereas slow pathway ablation was documented in 108 patients (43 %).
In 151 patients (60 %), RF was used as sole energy source for slow pathway modulation/ablation. Immediate ablation success was achieved in 147/151 (98 %) patients. Median lesion number in patients treated with RF only was 11 (5–21). Cryoenergy was solely used in 70 patients (28 %) with a median lesion number of 2 (1–5). Immediate success rate using cryoenergy alone was 100 %. In 32 patients (12 %), after failure to reach the primary endpoint (i.e., slow pathway modulation/ablation) using either cryoenergy or RF as primary energy source, switch to the alternative energy source was performed at the discretion of the operator. Immediate success rate in those patients was slightly lower (94 %, n = 30). This difference, however, did not reach statistical significance. The median number of cryolesions and RF lesions was 5 (3–10, n = 32) and 10 (4–17, n = 32), respectively, in patients who were treated with both energy forms. There was no significant difference with respect to the lesion number when RF was used as the sole energy source, i.e., in patients treated with both energy sources, the number of RF applications did not significantly differ from patients treated with RF only. There was, however, a significant difference in the number of cryoenergy lesions between patients treated with cryoenergy alone and those patients treated with both energy forms (p = 0.002, Table 1).
Complications
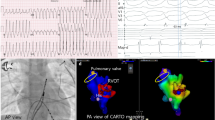
In 8 out of 253 patients, major complications occurred, resulting in a cumulative adverse event rate of 3.2 %. 3 patients had persistent high-degree AV block requiring pacemaker implantation after RF application. Two of those patients had the history of complex CHD, specifically tricuspid atresia (13-year-old female, body weight 44 kg) and d-transposition of the great arteries (16-year-old female, body weight 54 kg), and the remaining patient had the history of tuberous sclerosis (15-month-old female, body weight 8.7 kg). The former patients had palliative surgery for their CHD in the past (Fontan circulation for tricuspid atresia and Mustard atrial switch repair for d-transposition of the great arteries). The latter infant had had RF ablation of a left lateral accessory pathway 4 weeks prior to AVNRT ablation.
Pericardial tamponade requiring pericardial drainage occurred in 2 patients (two boys, 6 and 9 years old with a body weight of 24 and 38 kg, respectively) with structurally normal hearts. In the 6-year-old boy (body weight 24 kg), drainage of pericardial tamponade was necessary after cryoablation, and the 9-year-old patient (38 kg) had pericardial tamponade after RF ablation. Finally, surgical thrombectomy of the femoral artery used for the arterial sheath was required in 3 patients because of thrombotic occlusion. Table 2 summarizes all patients suffering from major complications. Selective coronary angiography did not show any evidence for affection of the coronary arteries.
Impact of body weight
In order to analyze the impact of body weight on procedural outcome of AVNRT ablation, our patients were subdivided into groups with either a body weight ≤25 or >25 kg. Table 1 provides detailed data on patient and procedural data of both patient groups. In 25 patients, body weight of the patient was ≤25 kg with the lowest body weight being 8.7 kg in a 15-month-old girl with tuberous sclerosis and recurrent AVNRT despite multiple antiarrhythmic medications. CHD was present in 8 % of the patients ≤25 kg (n = 2), whereas in patients >25 kg, CHD was found in only 1.8 % (n = 4, p = 0.001). Indication for ablation in patients ≤25 kg was drug-refractory SVT in 56 % of the patients, whereas patients’/parents’ preference was the most prevalent indication for ablation in patients >25 kg (79 %, p = 0.001). Vice versa, patients’/parents’ preference was the indication in 44 % of patients ≤25 kg, whereas drug-refractory SVT was the indication in 21 % of patients >25 kg. ECG documentation of SVT was significantly more prevalent in patients with a body weight ≤25 kg (p = 0.04).
No differences were found regarding procedure duration as well as fluoroscopy time. However, exposure to ionizing radiation as expressed by dose area product was less in the smaller patients (2396; IQR 2166–3140 cGy/m2 in patients ≤25 kg vs. 3612, IQR 2056–6339 cGy/m2 in patients >25 kg, p = 0.002). Primary success of catheter ablation could be achieved in 96 % (n = 24) of the patients ≤25 kg which was not significantly different from overall success (98 %, n = 248) and success in patients >25 kg (98 %, n = 224). Slow pathway ablation compared with slow pathway modulation was more prevalent in patients with a body weight of ≤25 kg (Table 1). Overall incidence of major complications was significantly higher in patients ≤25 kg with a complication rate of 12 % compared to a complication rate of 2.2 % in patients >25 kg (p = 0.04, see also Tables 1, 2).
Since AVNRT ablation was performed using RF energy as well as cryoenergy, we were interested in whether body weight influenced the decision to use either of both energy sources preferentially. Cryoenergy was more frequently used in patients ≤25 kg (40 % of patients ≤25 kg, n = 10 vs. 27 % of patients >25 kg, n = 60; p = 0.04, Table 1). There was, however, no difference in the percentage of patients treated with both energy sources consecutively.
Repeat procedures
In 18 patients, 20 repeat procedures were performed because of AVNRT recurrence. All but one patient had a body weight of >25 kg and a structurally normal heart at the time of re-ablation. Median age was 13.5 years (11.1–16.5 years), median body weight was 61.6 kg (35.6–64.5 kg), and median body height was 167 cm (144–175 cm) at the time of the procedure. A 4-year-old boy with repaired double-outlet right ventricle presented with a body weight of 18.1 kg at the first repeat procedure and 20 kg at the second repeat procedure. This particular boy was the only patient with a second repeat procedure because of AVNRT recurrence after the first repeat procedure. Procedure duration (median 194 min, IQR 151–274 min), fluoroscopy time (median 8.9 min, IQR 6.5–12.4 min), and fluoroscopy dose (median 3744 cGy/m2, IQR 2422–5080 cGy/m2) were in the range as in the primary procedures. Procedural success was achieved in 95 % (n = 19) with SP modulation and SP ablation being distributed slightly in favor of SP modulation (58 and 42 %, respectively, n = 19). RF was the energy source used in most of the repeat procedures (86 %, n = 17). No major complications were observed in patients after re-ablation of AVNRT.
Discussion
Catheter ablation of SVT in children and adolescents has evolved as the therapy of choice for definite treatment in the last 20 years [1, 2, 5, 6, 16, 17]. In a recently published consensus document of the EHRA/AEPC, catheter ablation of SVT in children >5 years of age has been recommended with a class II A indication regardless of prior antiarrhythmic treatment. In children <5 years of age, catheter ablation has been recommended with a class II A indication in drug-refractory SVT [18]. AVNRT is less prevalent in infants and smaller children below the age of 5 years compared with SVT due to accessory pathways. Accordingly, data are sparse for these small children. However, nowadays, a considerable number of patients are scheduled for catheter ablation because of either drug-refractory SVT or parents’ preference [7, 19].
In accordance with results from previous registries and studies [1–6, 12, 20], we found a high immediate success rate in a pediatric patient population undergoing either RF or cryoenergy ablation of AVNRT. Success was not related to body weight, indicating a high efficacy of catheter ablation of AVNRT even in infants and small children. With respect to either modulation or ablation of the slow pathway, the proportion of patients in whom ablation of the slow pathway was achieved was higher in the group ≤25 kg. It may be speculated that in these patients, because of smaller anatomical structures, RF energy and cryoenergy lesions are more effective than in older patients. This fact may also explain the higher rate of AV block and pericardial effusion in the smaller patients as the close proximity of AVNRT substrate and the cardiac conduction system and the low wall thickness of the atria might predispose small patients for such complications. Additional factors are unlikely to be of significant influence as the lesion number for RF energy as well as for cryoenergy did not differ among both groups of patients.
The use of cryoenergy for ablation of SVT substrates has been described as safe, but a recent retrospective multicenter trial demonstrated a lower efficacy in terms of immediate ablation success in small children and infants <5 years of age and/or <15 kg body weight [8]. In our patients, we found cryoenergy as effective as RF energy. These different results may be interpreted in two ways. First, in our center, a high number of patients were treated with cryoenergy and thus the operator’s experience with this technique was high. Second, in the present study, analysis was restricted to AVNRT ablation with an expected high primary success rate. A primary success rate of 100 % in ablation of AVNRT using cryoenergy in babies and small children has been reported recently [8].
For the whole group, fluoroscopy time was definitely shorter than that reported in the registries from the 1990s and early 2000s, where mean fluoroscopy times of 28 min and longer were reported [1, 2, 5, 6]. This promising result is due to the fact that in all our procedures a nonfluoroscopic catheter navigation system was used as previously described [1, 21, 22]. It is of note that we did not find a significant difference in fluoroscopy time between patients ≤25 kg and >25 kg. This indicates that nonfluoroscopic catheter navigation systems are of value also in catheter ablation of AVNRT in small children. The lower fluoroscopy dose in patients ≤25 kg has to be attributed to the lower body mass of the patients.
We found a higher percentage of patients with congenital heart disease among the patients with a body weight ≤25 kg. This is probably due to the fact that SVT was poorly tolerated by this group of patients, resulting in an indication for catheter ablation.
Complications
RF ablation of SVT substrates has been shown to be safe and effective in children and adolescents with a complication rate of 3–4 %. High-degree AV block requiring pacemaker implantation is the most common major complication with an incidence of 2 % after AVNRT ablation using RF energy [1, 2, 23]. Cryoenergy seems to be even safer when targeting SVT substrates with no major complications when cryoenergy was used exclusively for the ablation of SVT substrates in children and adolescents [3, 8]. To date, to the best of our knowledge, no pacemaker implantation due to complete AV block has been reported after cryoenergy ablation.
Besides operator experience and substrate localization, it seems to be reasonable to assume that body weight has an impact on the incidence of complications after catheter ablation in pediatric patients with the smaller patients being at higher risk. Our data show a significantly higher incidence of major complications in children with a body weight ≤25 kg. We observed complete AV block in one child, hemodynamically relevant pericardial effusion requiring drainage in one patient, and groin vessel damage requiring surgical revascularization in one child among 25 patients ≤25 kg (Table 2). This accounts for a major complication rate of 12 % in patients ≤25 kg in the present study. Comparing complication rate of the present study with data from other studies, however, is difficult, since none of these studies were restricted to patients with AVNRT but included patients with other SVT substrates as well [24]. One patient with a body weight ≤25 kg had right atrial perforation resulting in significant pericardial effusion requiring drainage after cryoablation (Table 2). This complication might be attributed to the stiffness of the 7F cryoenergy ablation catheter and has to be taken into consideration, when using cryoenergy for ablation of SVT substrates in small children.
Two adolescents with complex congenital heart disease required permanent pacemaker implantation because of persistent high-degree AV block after RF ablation. This emphasizes the need for the operator to keep the different anatomical situation of the conduction system in selected patients with congenital heart disease in mind when going for AVNRT ablation. Although being aware of the increased risk, we have to admit that the risk of AV block cannot be completely eliminated. It therefore seems to be worthwhile to start with cryoenergy as the first-line energy source during AVNRT ablation in patients with unknown or abnormal anatomy of the cardiac conduction system. In the group ≤25 kg, an infant with a body weight of 8.7 kg suffered from complete AV block requiring pacemaker implantation after RF ablation. Due to the close proximity of anatomical structures in smaller patients and the comparatively larger lesion size, the risk of damage to the cardiac conduction system is probably higher than in older patients and has to be taken into consideration when targeting the slow pathway. Therefore, cryoenergy might be the preferable source of energy in AVNRT ablation in small infants and children [3]. On the other hand, however, the higher stiffness of the commercially available 7F cryoenergy ablation catheter may contribute to other serious complications as mentioned above. This drawback might be overcome with the availability of smaller and more flexible cryoablation catheters.
Coronary artery stenosis has been described after RF application in the right posteroseptal space for accessory pathway as well as for AVNRT ablation [9, 10]. We did not observe any coronary artery affection in our patients neither after RF ablation nor after cryoenergy ablation. Given the fact that in three patients thrombotic occlusion of the femoral arteries required surgical thrombectomy and no coronary artery affection was observed in any patient, omitting insertion of an arterial sheath for routine coronary angiography at least in school-aged children and adolescents should be taken into consideration. In infants and small children, however, continuous blood pressure monitoring via an arterial sheath seems to be advisable because of possible hemodynamic compromise due to tachycardia.
Data from redo-procedures were not compared with data from primary AVNRT ablations to avoid bias. However, all but one patient scheduled for a redo-procedure had a body weight of >25 kg at the time of the primary ablation. Therefore, low body weight at the time of primary AVNRT ablation was not a predictor for SVT recurrence. The equal success rate of redo-procedures and the fact that we did not observe major complications in the context of redo-procedures lead us to the conclusion that redo-catheter ablation of AVNRT in children and adolescents >25 kg can be performed as efficacious and as safe as primary procedures are performed.
Limitations
The present study is limited by its retrospective nature and its limited follow-up as long-term follow-up data were not available at the time of data analysis. Number of patients, however, is significant to allow more insight into the ablation of AVNRT in young patients.
Conclusions
Efficacy of catheter ablation of AVNRT was not different between patients with a body weight of ≤25 and >25 kg. Major complications, including vascular occlusion and AV block, were more prevalent in patients ≤25 kg. High efficacy in the smaller patients may have been achieved at the expense of a higher complication rate.
Therefore, indication for AVNRT ablation in infants and small children should be discussed on an individual basis. Omitting insertion of an arterial sheath for routine coronary angiography and blood pressure monitoring should be taken into consideration at least in school-aged children and adolescents in order to avoid vessel complications. In patients with complex CHD and atypical localization of the cardiac conduction system, operators must be aware of an increased risk for AV block. It may be speculated that the primary use of cryoenergy in these patients will help avoid serious complications.
References
Kugler JD, Danford DA, Houston KA, Felix G, Pediatric Radiofrequency Ablation Registry of the Pediatric Radiofrequency Ablation Registry of the Pediatric Electrophysiology S (2002) Pediatric radiofrequency catheter ablation registry success, fluoroscopy time, and complication rate for supraventricular tachycardia: comparison of early and recent eras. J Cardiovasc Electrophysiol 13:336–341
Van Hare GF, Javitz H, Carmelli D, Saul JP, Tanel RE, Fischbach PS, Kanter RJ, Schaffer M, Dunnigan A, Colan S, Serwer G (2004) Prospective assessment after pediatric cardiac ablation: demographics, medical profiles, and initial outcomes. J Cardiovasc Electrophysiol 15:759–770
Kriebel T, Broistedt C, Kroll M, Sigler M, Paul T (2005) Efficacy and safety of cryoenergy in the ablation of atrioventricular reentrant tachycardia substrates in children and adolescents. J Cardiovasc Electrophysiol 16:960–966
Kubus P, Vit P, Gebauer RA, Zaoral L, Peichl P, Fiala M, Janousek J (2014) Long-term results of paediatric radiofrequency catheter ablation: a population-based study. Europace 16:1808–1813
Kugler JD, Danford DA, Houston K, Felix G (1997) Radiofrequency catheter ablation for paroxysmal supraventricular tachycardia in children and adolescents without structural heart disease. Pediatric EP Society, Radiofrequency Catheter Ablation Registry. Am J Cardiol 80:1438–1443
Kugler JD, Danford DA, Deal BJ, Gillette PC, Perry JC, Silka MJ, Van Hare GF, Walsh EP (1994) Radiofrequency catheter ablation for tachyarrhythmias in children and adolescents. The Pediatric Electrophysiology Society. N Engl J Med 330:1481–1487
Ko JK, Deal BJ, Strasburger JF, Benson DW Jr (1992) Supraventricular tachycardia mechanisms and their age distribution in pediatric patients. Am J Cardiol 69:1028–1032
LaPage MJ, Reed JH, Collins KK, Law IH, Pilcher TA, Tanel RE, Anderson CC, Young ML, Emmel M, Paul T, Blaufox AD, Arora G, Saul JP (2011) Safety and results of cryoablation in patients <5 years old and/or <15 kilograms. Am J Cardiol 108:565–571
Blaufox AD, Saul JP (2004) Acute coronary artery stenosis during slow pathway ablation for atrioventricular nodal reentrant tachycardia in a child. J Cardiovasc Electrophysiol 15:97–100
Schneider HE, Kriebel T, Gravenhorst VD, Paul T (2009) Incidence of coronary artery injury immediately after catheter ablation for supraventricular tachycardias in infants and children. Heart Rhythm 6:461–467
Denes P, Wu D, Dhingra R, Amat-y-Leon F, Wyndham C, Rosen KM (1975) Dual atrioventricular nodal pathways. A common electrophysiological response. Brit Heart J 37:1069–1076
Bertram H, Windhagen-Mahnert B, Bokenkamp R, Kriebel T, Peuster M, Hausdorf G, Paul T (2001) Abbreviated combined anatomical/electrophysiological approach for catheter ablation of atrioventricular nodal reentrant tachycardia in children. Cardiol Young 11:182–187
Jackman WM, Beckman KJ, McClelland JH, Wang X, Friday KJ, Roman CA, Moulton KP, Twidale N, Hazlitt HA, Prior MI et al (1992) Treatment of supraventricular tachycardia due to atrioventricular nodal reentry, by radiofrequency catheter ablation of slow-pathway conduction. N Engl J Med 327:313–318
Manolis AS, Wang PJ, Estes NA 3rd (1994) Radiofrequency ablation of slow pathway in patients with atrioventricular nodal reentrant tachycardia. do arrhythmia recurrences correlate with persistent slow pathway conduction or site of successful ablation? Circulation 90:2815–2819
Feldman A, Voskoboinik A, Kumar S, Spence S, Morton JB, Kistler PM, Sparks PB, Vohra JK, Kalman JM (2011) Predictors of acute and long-term success of slow pathway ablation for atrioventricular nodal reentrant tachycardia: a single center series of 1,419 consecutive patients. Pacing Clin Electrophysiol 34:927–933
Lee PC, Hwang B, Chen SA, Tai CG, Chen YJ, Chiang CE, Meng CC (2007) The results of radiofrequency catheter ablation of supraventricular tachycardia in children. Pacing Clin Electrophysiol 30:655–661
Joung B, Lee M, Sung JH, Kim JY, Ahn S, Kim S (2006) Pediatric radiofrequency catheter ablation: sedation methods and success, complication and recurrence rates. Circ J 70:278–284
Brugada J, Blom N, Sarquella-Brugada G, Blomstrom-Lundqvist C, Deanfield J, Janousek J, Abrams D, Bauersfeld U, Brugada R, Drago F, de Groot N, Happonen JM, Hebe J, Yen Ho S, Marijon E, Paul T, Pfammatter JP, Rosenthal E, European Heart Rhythm A, Association for European P, Congenital C (2013) Pharmacological and non-pharmacological therapy for arrhythmias in the pediatric population: EHRA and AEPC-Arrhythmia Working Group joint consensus statement. Europace 15:1337–1382
Crosson JE, Hesslein PS, Thilenius OG, Dunnigan A (1995) Av node reentry tachycardia in infants. Pacing Clin Electrophysiol 18:2144–2149
Kriebel T, Bertram H, Windhagen-Mahnert B, Bokenkamp R, Kaulitz R, Rohloff A, Peuster M, Hausdorf G, Paul T (2000) atrioventricular nodal reentry tachycardia in children: curative treatment by high frequency catheter ablation. Z Kardiol 89:538–545
Miyake CY, Mah DY, Atallah J, Oikle HP, Melgar ML, Alexander ME, Berul CI, Cecchin F, Walsh EP, Triedman JK (2011) Nonfluoroscopic imaging systems reduce radiation exposure in children undergoing ablation of supraventricular tachycardia. Heart Rhythm 8:519–525
Mah DY, Miyake CY, Sherwin ED, Walsh A, Anderson MJ, Western K, Abrams DJ, Alexander ME, Cecchin F, Walsh EP, Triedman JK (2014) The use of an integrated electroanatomic mapping system and intracardiac echocardiography to reduce radiation exposure in children and young adults undergoing ablation of supraventricular tachycardia. Europace 16:277–283
Reithmann C, Fiek M (2014) Fast pathway ablation for atrioventricular nodal reentrant tachycardia with a marked pr interval prolongation during sinus rhythm following transcatheter aortic valve implantation. Clin Res Cardiol 103:495–498
Aiyagari R, Saarel EV, Etheridge SP, Bradley DJ, Dick M 2nd, Fischbach PS (2005) Radiofrequency Ablation for Supraventricular Tachycardia in Children < or = 15 Kg Is Safe and Effective. Pediatr Cardiol 26:622–626
Conflict of interest
The authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
U. Krause and D. Backhoff contributed equally to this work.
Rights and permissions
About this article
Cite this article
Krause, U., Backhoff, D., Klehs, S. et al. Catheter ablation of pediatric AV nodal reentrant tachycardia: results in small children. Clin Res Cardiol 104, 990–997 (2015). https://doi.org/10.1007/s00392-015-0868-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-015-0868-6