Abstract
Background
Young women with acute coronary syndrome (ACS) may represent a high risk group, but little is known about specific age and sex differences in clinical characteristics, treatment, outcomes, and trends over time.
Methods
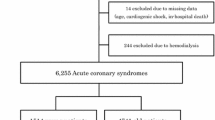
Data from 3237 men and women admitted with an ACS event from 1999 to 2006 were analyzed. Patients were grouped by sex and age less than 55 years. Demographics, presentation, treatment, and outcomes at 6 months were analyzed. Primary outcomes included mortality, recurrent myocardial infarction, rehospitalization, and stroke at 6 months. Secondary analyses assessed risk factors, management, and trends over time.
Results
Women under 55 years represented 8 % of the entire cohort, and 26 % of patients under age 55 years. Compared to older women, young women were more likely to be smokers (51 vs. 14 %, p < 0.001) and obese (44 vs. 34 %, p = 0.006). Young women had more diabetes and hypertension than young men. Mortality was lowest among young women and did not change over time. Young women received less treatment with aspirin, beta blockers, lipid-lowering agents, and ACE inhibitors, and underwent less coronary angiography and stenting than young men (44 vs. 59 %, p < 0.001). Rehospitalization was higher among young women than young men (37 vs. 27 %, p < 0.001), with no change over time.
Conclusions
Modifiable risk factors such as smoking, obesity, diabetes, and hypertension should be addressed in young women. Following ACS, young women received fewer evidence-based medications, were treated less invasively, and had higher readmission rates within 6 months compared to young men.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Despite increased awareness and interest in cardiovascular disease in women [1, 2], gaps in understanding the interaction of age and gender remain. Young women may represent a particularly high risk group with more short- and long-term mortality than men following (ACS) [3–6], but studies are inconsistent [7–10]. It remains unclear whether young women with ACS have more co-morbidities and worse adverse outcomes following ACS than young men and older women.
To study the net effect of both age and gender, we compared young women under age 55 years to two other groups: (1) women 55 years of age and older, and (2) men under age 55 years. Our aims were to identify cardiac risk factors among young women with ACS, describe differences in presentation and management, assess in-hospital and 6-month outcomes, and examine trends in outcomes over time.
Methods
Data from 3237 men and women admitted to the University of Michigan Health System with an ACS event were prospectively collected from January 1999 to December 2006. Patients were eligible for inclusion if they were 18 years or older and met criteria for ACS. Diagnosis of ACS was based on clinical presentation (ischemic symptoms) consistent with ACS and at least one of the following: ECG changes consistent with an ACS, serial increases in biochemical markers of cardiac necrosis (creatine kinase-MB, creatine phosphokinase, and/or troponin), or documented coronary artery disease. Patients were excluded if there was a non-cardiovascular cause of the ACS (e.g., trauma or surgery). The study was approved by the University of Michigan Institutional Review Board and written informed consent was obtained from all participants at inclusion.
Demographics, medical history, medications on admission, in-hospital management and outcomes at 6 months were included in the analysis. All cases were assigned to one of the following categories: ST-segment elevation MI (STEMI), non-ST-segment elevation (NSTEMI) or unstable angina. The primary outcomes of interest 6 months after ACS were all-cause mortality, recurrent myocardial infarction (MI), rehospitalization, and stroke, as verified by review of medical records and phone call follow-up. Standardized definitions of clinical diagnoses were used. The absence of any classic cardiovascular risk factor, defined as smoking, diabetes mellitus, hypertension, hyperlipidemia, and obesity (BMI > 30) was also evaluated. For comparisons, women and men were grouped by age into a younger group <55 years of age and those 55 years or older. The vast majority of women are postmenopausal by age 55 [11], thus providing a logical age cutoff for comparing differences between younger and older women. In secondary analysis, changes in outcomes over time were assessed by comparing patients enrolled in the database between 1999 and 2001 with a more recent cohort enrolled between 2004 and 2006.
Statistical analysis
Age was dichotomized at 55 years. Younger women were compared with older women and younger men. Differences between study groups for categorical variables were assessed by Pearson Chi square or Fisher’s exact test where appropriate. For normally distributed continuous variables, two-way analysis of variance was performed, followed by Student’s T tests with Bonferroni adjustment where appropriate. For continuous variables with skewed distributions, the Wilcoxon rank sum test was utilized. Univariate analysis as well as multivariable logistic regression was performed to determine predictors of poor outcomes. Trends over time were compared using the Cochran–Armitage Test. Statistical significance was determined at (alpha) ≤ 0.05. All statistical analyses were conducted with SAS version 9.2 (Cary, NC).
Results
Clinical profile
The age distribution of women and men younger than 55 years is shown in Fig. 1. Women younger than 55 years represented 7.8 % of all ACS patients, and 23.1 % of all women. Compared to older women, young women were more likely to be smokers and have a higher body mass index (BMI) (Table 1), but had lower 6-month GRACE risk scores (Table 2) and were less likely to have a prior history of heart failure, hypertension, hyperlipidemia, or stroke (Table 1). Among all patients younger than 55 years, women represented 26.1 %. Compared to young men, young women were more likely to have a prior history of heart failure, angina, diabetes mellitus, and hypertension, but no difference in smoking or obesity (Table 1).
Presentation and management
Compared to older women, young women were more likely to present with a diagnosis of unstable angina, but had equal rates of STEMI (Table 2). Younger women had significantly lower GRACE risk scores, but underwent more catheterization and PCI than older women. Upon discharge, among patients without contraindications, younger women were less likely to receive aspirin and beta blockers when compared to older women. In comparison to young men, young women were less likely to present with STEMI and more likely to present with unstable angina (Table 2). Young women received fewer percutaneous coronary interventions and lytics, but had similar rates of bypass surgery. Upon discharge, younger women were less often treated with aspirin, beta blockers, ACE inhibitors/ARBs, and lipid-lowering agents, as compared to young men (Table 2).
Outcomes
In-hospital and 6-month outcomes are shown in Table 3. During hospitalization for an ACS event, older women were more likely to develop acute renal failure. Compared to young men, young women had more than twice the rate of major bleeding events. At 6 months, young women had significantly higher rates of rehospitalization than young men. Young women had lower mortality than older women, but similar to young men. There were no significant differences in recurrent myocardial infarction rates. In multivariable logistic regression, only serum creatinine predicted rehospitalization rates among young women (OR 1.37, 95 % CI 1.06–1.76), while prior history of heart failure (p = 0.002), MI (p = 0.049), PCI (p = 0.004) and history of smoking (p = 0.008) were predictors of rehospitalization among older women. Key differences in treatment and outcomes between the three groups are highlighted in Fig. 2.
Trends over time
Differences in mortality and rehospitalization outcomes were compared over time, grouped by year of discharge. While there was a decrease in mortality among older women from 1999 (19.1 %) to 2006 (6.4 %), there was no significant improvement in mortality in young women over the study period (Fig. 3). Rehospitalization rates among older women appeared to increase over time, but there was no statistically significant change in any of the three groups over time (Fig. 4). Young women consistently had higher rates of rehospitalization than young men (Fig. 4).
Discussion
This study directly addressed the interaction of both age and gender in presentation, treatment, and outcomes after ACS. Young women have high rates of smoking, obesity, diabetes, and hypertension. Young women are less likely to receive goal-directed medical therapy following ACS and have a high rate of rehospitalization within 6 months.
The high prevalence of modifiable risk factors among young women is particularly concerning. Smoking is a well-recognized cardiovascular risk factor, particularly among young patients [12, 13]. In our study, 72 % of young people had smoked, with no difference between young men and young women. The majority of young women in our study were obese, with an average BMI of 31.2, higher than older women (BMI 28.8, p < 0.001). Although prior studies have indicated that obesity may affect young men more than young women [14, 15], our results point to obesity as a significant risk factor for heart disease in young women as well. Finally, diabetes and hypertension are thought to be more common among older patients [16, 17]. Our study revealed more hypertension among older women than younger women, but rates of diabetes among younger and older women were similar. Young women carried a higher burden of both diabetes and hypertension than young men, which is in agreement with prior studies [14].
Over time, improved medical management and adherence to secondary prevention guidelines has been reported for both women and men [18]. Unfortunately, young women in our study were significantly less likely than young men to receive goal-directed medical therapy following a diagnosis of ACS. Although we can only speculate, possible reasons include insufficient recognition and treatment of CAD in women, incomplete documentation of intolerances or contraindications, patient preference, or concern for treating women of childbearing age with certain medications. Young women were also less likely to have angiography and PCI than young men. Undertreatment of women has been reported previously [19, 20]; for example, women with ACS have been shown to undergo coronary angiography and stenting less often than men, even after adjusting for co-morbidities and number of significant stenoses [21]. Perhaps, women undergo less coronary angiography because of the differences in symptom presentation, less ST elevations, lower levels of risk by cardiac biomarkers, or patient preference. The lower rates of coronary intervention may be explained by less-frequent coronary angiography, as well as differences in coronary anatomy including less obstructive CAD or smaller coronary arteries, which can make PCI technically difficult.
Contrary to prior studies [3], young women in our study were not observed to have higher in-hospital or short-term mortality. Mortality has been shown to be higher in women than men especially under the age of 60 [3, 5, 14], but as overall mortality has been improving, any such gap in outcome has been reported to be narrowing [4]. Our study evaluated patients from 1999 to 2006, which may have reflected less difference among the genders than was observed in the early 1990s. Women who present with coronary disease at a younger age, at a time when they are protected by the effects of estrogen, may be predisposed to more aggressive disease or may have more risk factors [3]. Although it is possible that our cohort may have been healthier than those of other studies, the young women in our group had high rates of obesity, smoking, diabetes, and hypertension.
Our most notable finding was the high rate of rehospitalization within 6 months of diagnosis of ACS among young women, with no significant improvement over time (Fig. 4). Possible reasons for high rates of rehospitalization among young women may include persistent angina despite normal or non-obstructive coronary disease [22], inadequate medical treatment, insufficient reassurance, or other medical co-morbidities, but further investigation is needed. Female gender has also been associated with a 32 % increase in the risk of readmission within 30 days following PCI [23]. In our current era of using readmission rates as a cornerstone metric for reimbursement and quality control, additional research into reasons for readmission among young women is indicated.
Our study revealed no significant improvement in mortality among young women between 1999 and 2006 (Fig. 3). In contrast, large studies that have evaluated in-hospital mortality trends indicate there has been improvement among young women. Between 1994 and 2006, the National Registry of Myocardial Infarction revealed in-hospital mortality after acute MI decreased 3 times more in young women than young men (<55 years) (2.7 vs. 0.9 %), largely explained by changes in risk profiles [4]. More recently, a study using National Inpatient Sample data from 2001 to 2010 also showed that in-hospital mortality among young women has been improving [24]. Although these studies are encouraging, additional attention to long-term outcomes among young women is warranted as barriers to optimal medical care continue to exist, including delays in seeking care [25], delays in ambulance prioritization and transfer [26], and less aggressive medical therapy [9].
Strengths of this study include the observational design, which allowed for a more heterogeneous patient population than typically represented by randomized controlled trials. However, the observational nature of this study also has certain inherent limitations and potential biases. Additional limitations should be acknowledged. First, this was a single-center study and does not account for regional variations in demographics, risk factors, and management. Second, patients who died before hospital arrival were not included and only 6 months of follow-up data were collected. Longer duration of follow-up may have provided additional insight, particularly in young people for whom a long event-free survival period is expected. Additional data such as menopausal status, peripartum status, baseline medications, family history of coronary disease, and other less common causes of ACS such as vasospasm and coronary dissection may have been useful. Coronary angiography was not performed in all patients; although informative, this would not have been clinically indicated in many patients.
Conclusions
Young women have a high prevalence of potentially modifiable risk factors including: cigarette smoking, diabetes, hypertension, and obesity. Contrary to prior studies, young women did not have higher rates of mortality or recurrent MI; however, they did have high rates of rehospitalization within 6 months. Young women were less likely to receive goal-directed medications, were treated less invasively, and had higher readmission rates than young men. Further research is warranted to understand predictors of rehospitalization among younger women.
References
Mosca L, Benjamin EJ, Berra K, Bezanson JL, Dolor RJ, Lloyd-Jones DM, Newby LK, Pina IL, Roger VL, Shaw LJ, Zhao D, Beckie TM, Bushnell C, D’Armiento J, Kris-Etherton PM, Fang J, Ganiats TG, Gomes AS, Gracia CR, Haan CK, Jackson EA, Judelson DR, Kelepouris E, Lavie CJ, Moore A, Nussmeier NA, Ofili E, Oparil S, Ouyang P, Pinn VW, Sherif K, Smith SC Jr, Sopko G, Chandra-Strobos N, Urbina EM, Vaccarino V, Wenger NK (2011) Effectiveness-based guidelines for the prevention of cardiovascular disease in women–2011 update: a guideline from the American heart association. Circulation 123:1243–1262
Mosca L, Barrett-Connor E, Wenger NK (2011) Sex/gender differences in cardiovascular disease prevention: what a difference a decade makes. Circulation 124:2145–2154
Vaccarino V, Parsons L, Every NR, Barron HV, Krumholz HM (1999) Sex-based differences in early mortality after myocardial infarction. National registry of myocardial infarction 2 participants. N Engl J Med 341:217–225
Vaccarino V, Parsons L, Peterson ED, Rogers WJ, Kiefe CI, Canto J (2009) Sex differences in mortality after acute myocardial infarction: changes from 1994 to 2006. Arch Intern Med 169:1767–1774
Vaccarino V, Krumholz HM, Yarzebski J, Gore JM, Goldberg RJ (2001) Sex differences in 2-year mortality after hospital discharge for myocardial infarction. Ann Intern Med 134:173–181
Canto JG, Rogers WJ, Goldberg RJ, Peterson ED, Wenger NK, Vaccarino V, Kiefe CI, Frederick PD, Sopko G, Zheng ZJ (2012) Association of age and sex with myocardial infarction symptom presentation and in-hospital mortality. JAMA 307:813–822
Galatius-Jensen S, Launbjerg J, Mortensen LS, Hansen JF (1996) Sex related differences in short and long-term prognosis after acute myocardial infarction: 10 year follow up of 3073 patients in database of first Danish Verapamil Infarction Trial. BMJ 313:137–140
White AD, Rosamond WD, Chambless LE, Thomas N, Conwill D, Cooper LS, Folsom AR (1999) Sex and race differences in short-term prognosis after acute coronary heart disease events: the atherosclerosis risk in communities (ARIC) study. Am Heart J 138:540–548
Alfredsson J, Stenestrand U, Wallentin L, Swahn E (2007) Gender differences in management and outcome in non-ST-elevation acute coronary syndrome. Heart 93:1357–1362
Fengler K, Fuernau G, Desch S, Eitel I, Neumann FJ, Olbrich HG, de Waha A, de Waha S, Richardt G, Hennersdorf M, Empen K, Hambrecht R, Fuhrmann J, Bohm M, Poess J, Strasser R, Schneider S, Schuler G, Werdan K, Zeymer U, Thiele H (2014) Gender differences in patients with cardiogenic shock complicating myocardial infarction: a substudy of the IABP-SHOCK II-trial. Clin Res Cardiol 104:71–78
McKinlay SM (1996) The normal menopause transition: an overview. Maturitas 23:137–145
Cole JH, Miller JI 3rd, Sperling LS, Weintraub WS (2003) Long-term follow-up of coronary artery disease presenting in young adults. J Am Coll Cardiol 41:521–528
Panagiotakos DB, Rallidis LS, Pitsavos C, Stefanadis C, Kremastinos D (2007) Cigarette smoking and myocardial infarction in young men and women: a case–control study. Int J Cardiol 116:371–375
Egiziano G, Akhtari S, Pilote L, Daskalopoulou SS, Investigators G (2013) Sex differences in young patients with acute myocardial infarction. Diabet Med J Br Diabet Assoc 30:e108–e114
McGill HC Jr, McMahan CA, Herderick EE, Zieske AW, Malcom GT, Tracy RE, Strong JP (2002) Obesity accelerates the progression of coronary atherosclerosis in young men. Circulation 105:2712–2718
Chen TS, Incani A, Butler TC, Poon K, Fu J, Savage M, Dahl M, Callow DE, Colburn D, Hammett C, Walters DL (2014) The demographic profile of young patients (<45 years-old) with acute coronary syndromes in Queensland. Heart Lung Circ 23:49–55
Hoit BD, Gilpin EA, Henning H, Maisel AA, Dittrich H, Carlisle J, Ross J Jr (1986) Myocardial infarction in young patients: an analysis by age subsets. Circulation 74:712–721
Lewis WR, Ellrodt AG, Peterson E, Hernandez AF, LaBresh KA, Cannon CP, Pan W, Fonarow GC (2009) Trends in the use of evidence-based treatments for coronary artery disease among women and the elderly: findings from the get with the guidelines quality-improvement program. Circ Cardiovasc Qual Outcomes 2:633–641
Nohria A, Vaccarino V, Krumholz HM (1998) Gender differences in mortality after myocardial infarction. Why women fare worse than men. Cardiol Clin 16:45–57
Chandra NC, Ziegelstein RC, Rogers WJ, Tiefenbrunn AJ, Gore JM, French WJ, Rubison M (1998) Observations of the treatment of women in the United States with myocardial infarction: a report from the national registry of myocardial infarction-I. Arch Intern Med 158:981–988
Hvelplund A, Galatius S, Madsen M, Rasmussen JN, Rasmussen S, Madsen JK, Sand NP, Tilsted HH, Thayssen P, Sindby E, Hojbjerg S, Abildstrom SZ (2010) Women with acute coronary syndrome are less invasively examined and subsequently less treated than men. Eur Heart J 31:684–690
Jespersen L, Abildstrom SZ, Hvelplund A, Prescott E (2013) Persistent angina: highly prevalent and associated with long-term anxiety, depression, low physical functioning, and quality of life in stable angina pectoris. Clin Res Cardiol 102:571–581
Khawaja FJ, Shah ND, Lennon RJ, Slusser JP, Alkatib AA, Rihal CS, Gersh BJ, Montori VM, Holmes DR, Bell MR, Curtis JP, Krumholz HM, Ting HH (2012) Factors associated with 30-day readmission rates after percutaneous coronary intervention. Arch Intern Med 172:112–117
Gupta A, Wang Y, Spertus JA, Geda M, Lorenze N, Nkonde-Price C, D’Onofrio G, Lichtman JH, Krumholz HM (2014) Trends in acute myocardial infarction in young patients and differences by sex and race, 2001–2010. J Am Coll Cardiol 64:337–345
Nguyen HL, Gore JM, Saczynski JS, Yarzebski J, Reed G, Spencer FA, Goldberg RJ (2010) Age and sex differences and 20-year trends (1986–2005) in prehospital delay in patients hospitalized with acute myocardial infarction. Circ Cardiovasc Qual Outcomes 3:590–598
Melberg T, Kindervaag B, Rosland J (2013) Gender-specific ambulance priority and delays to primary percutaneous coronary intervention: a consequence of the patients’ presentation or the management at the emergency medical communications center? Am Heart J 166:839–845
Conflict of interest
The authors declare that they have no conflict of interest. This study was approved by the Institutional Review Board and conducted in accordance with the ethical standards in the 1964 Declaration of Helsinki.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Davis, M., Diamond, J., Montgomery, D. et al. Acute coronary syndrome in young women under 55 years of age: clinical characteristics, treatment, and outcomes. Clin Res Cardiol 104, 648–655 (2015). https://doi.org/10.1007/s00392-015-0827-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-015-0827-2