Abstract
Background
Myocarditis might be associated with increased markers of myocardial injury. However, data on novel biomarkers, such as high-sensitive Troponin T (hs-TnT) or Copeptin, are lacking. This study aimed to determine the diagnostic and prognostic utility of biomarkers in patients with suspected myocarditis.
Methods
Seventy patients with clinically suspected myocarditis (age 43.4 ± 14 years, 76 % male, ejection fraction 36.9 ± 17.8) underwent endomyocardial biopsy (EMB) and were followed for 7.5 (2–21) months. At the time of EMB, blood samples to evaluate concentrations of hs-TnT, Copeptin, NT-proBNP and mid-regional pro-adrenomedullin (MR-proADM) were collected.
Results
According to EMB, 6 patients were diagnosed with acute myocarditis (AM) and 36 patients with chronic myocarditis (CM). In 28 patients, EMB revealed no myocardial inflammation (NM). Acute myocarditis was associated with the highest concentrations of hs-TnT compared to other groups (AM 262.9 pg/ml (61.4–884.2); CM 20.4 pg/ml (15.6–20.4); NM 19.5 pg/ml (13.8–50.7); p < 0.0001). No significant differences existed in the Copeptin, NT-proBNP, and MR-proADM concentrations between the groups. The concentration of hs-TnT was significantly higher in myocarditis when myocardial viral genome was detected (37.4 pg/ml (21.9–163.6) vs. 20 pg/ml (14–44.4); p = 0.042). During follow-up, only NT-proBNP in the highest quartile (>4,225 ng/ml) was predictive for cardiac death or heart transplantation (hazard ratio 9.2; 95 % confidence interval 1.7–50; p = 0.011).
Conclusions
Biopsy-proven acute and viral myocarditis is associated with elevated concentrations of hs-TnT. Elevated hs-TnT is highly suggestive of acute myocarditis, if other causes of increased myocardial necrosis markers such as myocardial infarction have been systematically excluded.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The clinical manifestation of myocarditis is highly variable and may range from oligosymptomatic courses with palpitations over acute coronary syndrome-like presentations to devastating illness with cardiogenic shock [1]. Cardiac arrhythmias, chest pain, and acute or chronic heart failure may all occur during the course of the disease [2]. Hence, the diagnosis of myocarditis based on clinical symptoms alone is unreliable and usually needs confirmation by laboratory testing, ECG, cardiac imaging and heart catheterization [2]. The gold standard to diagnose myocarditis remains endomyocardial biopsy (EMB) with histological and immunohistochemical analyses, as well as molecular biological detection of microbial gene signatures in the myocardium [3, 4].
Contemporary cardiac biomarkers which are able to detect myocyte injury (cardiac troponins) [5], volume overload (natriuretic peptides) [6], acute endogenous stress (Copeptin) [7], and acute heart failure with microcirculatory dysfunction (MR-proADM) [8] have improved diagnosis and risk stratification in acute coronary syndromes and chronic heart failure. The objective of this study was to validate the diagnostic performance of these biomarkers in patients with suspected myocarditis undergoing EMB.
Methods
Study subjects and design
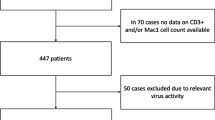
The study included 70 consecutive patients who underwent EMB as part of an evaluation for clinically suspected myocarditis in our hospital and were followed until July 2011. Enrolled patients were suspected to be affected by myocarditis if they experienced an episode of febrile infection of the (upper) respiratory tract, the gut, or the urinary tract within the last 6 months and if they presented at least one of the following features not related to myocardial ischemia: impaired global or regional left ventricular systolic function, pericardial effusion, or sustained or non-sustained ventricular tachycardia or ventricular fibrillation of unknown origin. Patients with overt cardiogenic shock at initial presentation were not included in the study. All patients gave a written informed consent to EMB and for further analyses of their data for scientific reasons. The study was approved by the local ethics committee.
Cardiac catheterization and endomyocardial biopsy
In each patient, left heart catheterization with coronary angiography was performed before EMB to exclude significant coronary artery disease as cause of heart failure. The mean time between hospital admission and biopsy was 2.9 ± 1.9 days. The biopsy sample sites [right (n = 8) vs. left ventricle (n = 62), wall segment] were chosen according to the findings of echocardiography or magnetic resonance imaging (MRI) of the heart, if available (33 patients with MRI before EMB). EMB were analyzed by immunohistochemistry, and by molecular biological detection of viral genomes as previously described [9]. According to the World Health Organization/International Society and Federation of Cardiology Task Force on the Definition an Classification of Cardiomyopathies [3], endomyocardial biopsies were considered to be inflamed after immunohistochemical detection of mononuclear infiltrates with >14 leukocytes per 1 mm2 (CD3+ T lymphocytes and/or CD68+ macrophages) in the myocardium, in addition to enhanced expression of HLA class II molecules. The diagnosis of acute myocarditis required the presence of myocyte necrosis in addition to inflammation, whereas chronic myocarditis was diagnosed if inflammation was detected without myocyte necrosis [3]. Viral genomes investigated by PCR/RT-PCR were enterovirus species (comprising coxsackieviruses and echoviruses), parvovirus B19, adenovirus, Epstein-Barr virus, and human herpesvirus type 6. Additionally, echocardiography was performed to determine left ventricular function and to exclude significant valvular disease.
Laboratory exams
Investigated biomarkers were high-sensitive troponin T (hs-TnT), N-terminal pro-B type natriuretic peptide (NT-proBNP), Copeptin as an indirect marker for arginine-vasopressin, and mid-regional pro-adrenomedullin (MR-proADM). Blood samples for determination of biomarkers were collected on the day of EMB. This time point was chosen, rather than “admission to hospital”, as the patients were in a stable clinical condition and levels of biomarkers may in this situation more likely represent myocardial inflammation than exacerbation of acute heart failure. High-sensitive troponin T (hs-TnT) was analyzed using the Modular Analytics E170 assay (Roche Diagnostics, Mannheim, Germany). The lower limit of detection of this hs-cTnT assay is 5 pg/mL. The upper reference limit, which corresponds to the 99 percentile in a healthy population, is 14 pg/mL. NT-proBNP was analyzed using ECLIA. After centrifugation, samples (n = 62) were frozen at −80 °C in plastic tubes containing ethylenediaminetetraacetic acid until analyzed. Copeptin and MR-proADM were measured with an automated sandwich chemiluminescence immunoassay on the KRYPTOR System (BRAHMS AG, Hennigsdorf/Berlin, Germany) as described elsewhere [10]. The lower limits of detection of Copeptin and MR-proADM were 5 pmol/l and 0.05 nmol/l, respectively. In case of non-detectable concentrations, values were set to the lower limit of detection. All blood samples were processed by personnel blinded from any patient data.
Follow-ups
Patients with suspected myocarditis who underwent EMB are scheduled for follow-up at 3–6-month intervals in our heart failure outpatient clinic. The total follow-up time of all subjects was 10,524 months. The mean follow-up time for each patient was 55.1 ± 105.1 months. All patients with signs or symptoms of heart failure received evidence-based medical treatment (Table 1). For investigation of the prognostic role of the biomarker, time to cardiac death or heart transplantation within 12 months after EMB was assessed.
Statistical analysis
Comparisons between groups were performed using the Wilcoxon rank sum test for continuous variables and the Pearson Chi Square Test for categorical variables. Survival curves of patients grouped by prespecified variables were calculated by the Kaplan–Meier method and compared with the log-rank test. The receiver operating characteristic (ROC) curves for prediction of acute myocardial inflammation were calculated. Continuous variables were redefined as categorical (above and below the 4th quartile of each biomarker) and dichotomized to allow presentation in a Kaplan–Meier plot. Cox proportional-hazards regression analysis was performed to assess the association of biomarkers with the occurrence of cardiac death or heart transplantation. Variables tested in the univariate analysis were age, gender, kidney function, ejection fraction, NYHA class, and variables with p < 0.1 were entered in the multivariable analysis. All analyses were performed with SPSS statistical software (version 20.0, SPSS Inc, Chicago, IL).
Results
Description of the study group
Baseline characteristics of the 70 patients are depicted in Table 1. Patients (mean age 44.2 ± 15.1 years) had a severely depressed left ventricular function (EF 36.9 ± 17.8 %). 53 patients (76 %) were in NYHA functional class III or IV. Immunohistochemical analyses of the EMB revealed acute myocarditis (AM) in 6, chronic myocarditis (CM) in 36 and no myocardial inflammation (NM) in 28 patients. Patients with AM tended to have a better left ventricular ejection fraction (LVEF) compared to other groups (p = 0.068). In 16 patients with a LVEF > 45 %, additional biopsy indications as signs of myocardial inflammation in MRI (n = 11), ventricular tachyarrhythmias (n = 3), complete atrioventricular block (n = 1), and pericardial effusion (n = 1) were present.
Concentration of biomarkers according to the different groups is listed in Table 2. Hs-TnT was markedly increased in AM compared to those without myocardial inflammation (Fig. 1). Additionally, concentration of creatinine kinase (CK) tended to be higher in AM (p = 0.057). Concentration of NT-proBNP, MR-proADM, Copeptin, or Cystatin C glomerular filtration rate did not significantly differ between groups. Figure 2 depicts the ROC curves of the investigated biomarkers in regard to identify AM. Only hs-TnT was significantly associated with AM (area under curve 0.878; p = 0.002) leading to a sensitivity of 83 % and specificity of 80 % for predicting AM in patients with a hs-TnT concentration ≥50 pg/ml.
Receiver operating characteristic (ROC) curves of biomarkers regarding their ability to predict acute myocardial inflammation (AM). Only hs-TnT was significantly associated with AM (area under curve 0.878; p = 0.002) leading to a sensitivity of 83 % and specificity of 80 % for predicting AM in patients with a hs-TnT concentration ≥50 pg/ml
Presence of viral genome in the myocardium
In the group of patients with acute or chronic myocardial inflammation, viral genome was detected in 12 (29 %) patients (parvovirus B19 n = 9; parvovirus B19 and HHV-6 n = 1; Epstein-Barr virus n = 1; Epstein-Barr virus and HHV-6 n = 1). In patients with myocarditis and viral genome detection in the myocardium, hs-TnT [37.4 (21.9–163.6) pg/ml] was increased compared to those with myocarditis without evidence of viral genome [20.0 (14–44.4) pg/ml; p = 0.042] or those without myocardial inflammation [19.5 (13.8–50.7) pg/ml; p = 0.021]. Concentrations of the other investigated biomarkers were not significantly different with respect to the prevalence of inflammation and/or viral genome detection in the myocardium. In patients without myocardial inflammation, viral genome was detected in 5 subjects (18 %). These patients with viral persistence did not differ from those without detection of viral genome concerning baseline characteristics or biomarkers concentrations.
Duration of symptoms
The time since onset of symptoms was 0–13 days in 14 (20 %) patients, 14–27 days in 15 (21 %) patients, 28–60 days in 22 (31 %) patients, and >60 days in 19 (28 %) patients. Three (50 %) patients with AM had a history of symptoms <14 days compared to 7 (19 %) with CM and 4 (14 %) with NM. Patients with a longer period symptoms (≥14 days) had a worse EF (34.4 ± 17.1 % vs. 47.3 ± 17.3 %; p = 0.014) and a lower systolic blood pressure (112.1 ± 21.7 vs. 126.8 ± 28.4 mmHg; p = 0.047) compared to those with shorter onset of symptoms (<14 days). Accordingly, the concentration of biomarkers was different in relation to onset of symptoms (Fig. 3). Patients with a shorter history of symptoms had higher concentrations of hs-TnT, whereas those with longer standing symptoms had higher concentrations of MR-proADM and NT-proBNP.
Outcome
During the first 12 months after EMB, 8 primary endpoints occurred: 6 patients died from cardiac cause and 2 patients underwent cardiac transplantation. The composite end point of cardiac death and heart transplantation occurred in 3 (8 %) patients with CM and 5 (18 %) patients with NM, whereas no event was documented in the group of AM (p = 0.323). In all patients with suspected myocarditis, the predictive value of the biomarkers for outcome was investigated (Fig. 4). Patients were categorized according to the 4th quartile of each biomarker. Only NT-proBNP concentration above the 4th quartile (≥4,245 pg/ml) proved to be of prognostic relevance for the occurrence of cardiac death or heart transplantation (p = 0.002). This was confirmed by multivariable analysis, where a NT-proBNP concentration ≥4,245 pg/ml was an independent predictor (odds ratio 7.91; 95 % confidence interval 1.29–48.58; p = 0.026) after adjusting for covariates (Table 3).
Kaplan–Meier analysis for cardiac death or heart transplantation according to the biomarkers categorized by the 4th quartile of each marker. a hs-TnT b NT-proBNP c MR-proADM d Copeptin. Only NT-proBNP concentration above the 4th quartile (≥4,245 pg/ml) proved to be of prognostic relevance for the occurrence of cardiac death or heart transplantation (p = 0.002). Q4 4th quartile, No number
Discussion
For the first time, this study evaluated a panel of novel biomarkers to diagnose and stratify patients with clinically suspected myocarditis. The key findings of the study can be summarized as follows:
-
1.
In patients with biopsy-proven acute myocarditis, hs-TnT concentrations are higher by at least one order of magnitude as compared to both, subjects with biopsy-proven chronic myocarditis, and patients in whom myocarditis has been excluded by biopsy.
-
2.
In patients who present a case history suggestive of inflammatory heart disease, a hs-TnT concentration >50 pg/ml is highly predictive for acute myocarditis, provided that acute myocardial infarction is definitely excluded by angiography and other common causes of troponin elevations like tachyarrhythmia, hypertensive crisis or decompensation of longstanding chronic heart failure.
-
3.
None of the other biomarkers measured in the study showed any predictive value for the diagnosis of myocarditis, but NT-proBNP concentrations allowed for cardiac mortality prognostication.
Non-specific serum markers of inflammation including leukocytes and C-reactive protein can be elevated in case of acute myocarditis [11], but normal values do not rule out an acute myocardial inflammatory process [12]. Virus serology is expensive and has no acceptable sensitivity in patients with clinically suspected myocarditis [12]. Additionally, serological methods lack specificity due to cross reactions, reactivations, reinfections and a high seroprevalence of antibodies against most of the viruses involved in the pathogenesis of myocarditis [2]. Electrocardiography and echocardiography are widely used as diagnostic tools [13–17]. However, there is no specific electrocardiographic or echocardiographic feature typical for myocarditis, and patterns consistent with hypertrophy, dilated cardiomyopathy, and ischemic heart disease can also be observed in myocarditis patients. Cardiac magnetic resonance (CMR) imaging has evolved as a non-invasive and valuable clinical tool for the diagnosis of myocarditis [18]. However, CMR is expensive, not available in all hospitals and still has limited sensitivity and specificity as compared to EMB, which remains the gold standard for diagnosing inflammatory heart disease [2]. Even when applying the state-of-the-art Lake Louise consensus criteria, CMR will not exceed a sensitivity of 63–67 % in comparison with EMB [18]. The lack of sensitivity of CMR is even more relevant in chronic compared to acute myocarditis, since two of the Lake Louise criteria, T1-weighted late gadolinium enhancement and T2-weighted oedema are less frequent in the chronic phase of myocarditis [19]. Although EMB is regarded as a safe procedure with low complication rates [4], non-invasive diagnostic tools may be preferable.
In contrast to hs-TnT which exhibited significantly higher plasma concentrations in patients with a very short history of symptoms (<14 days), NT-proBNP and MR-proADM concentrations were higher in patients with a longer history (≥28 days). Since acute myocyte necrosis with release of intracellular antigens into the blood stream is confined to the first few days of myocarditis [2], it becomes obvious that increased blood concentrations of myocyte necrosis markers (e.g. troponins) can only be detected in patients presenting during the very acute phase of this inflammatory heart disease. In most patients with myocarditis, immune response declines with virus elimination, and left ventricular function recovers without sequelae. The pathogenetic significance of persistence of viral genome in the myocardium is not completely understood and warrants further investigations [20–23]. However, in some patients autoimmune processes persist that lead to chronic myocarditis, characterized by myocardial remodeling and development of heart failure [2]. Thus, increased NT-proBNP and MR-proADM concentrations in our patients with a longer history of cardiac symptoms may be explained by the development of left ventricular dysfunction and volume overload. This assumption is substantiated by a significantly lower left ventricular ejection fraction in patients with a long symptom history as compared to subjects with a short history (34.4 ± 17.1 vs. 47.3 ± 17.3 %; p = 0.014).
As MR-proADM just as little as NT-proBNP could differentiate between the patient groups in the current study, MR-proADM in comparison with NT-proBNP does not seem to provide any additional information beyond hemodynamic burden. The finding that MR-proADM in contrast to NT-proBNP was not suitable to stratify outcome in our patient cohort is different to published studies in heart failure patients where the prognostic value of MR-proADM was comparable to natriuretic peptides [8]. It could be speculated that the small study size or the low number of cardiac events may account for this unexpected result.
Hitherto, there are no studies concerning the role of Copeptin in the diagnosis of myocarditis. In suspected acute coronary syndrome (ACS) the detection of elevated Copeptin levels improves the early diagnosis of acute myocardial infarction [24, 25]. The current study does not support the assumption that—in contrast to the ACS scenario—measurement of Copeptin concentrations provides any diagnostic or prognostic benefit in the setting of suspected myocarditis. Even in patients with acute myocarditis, there does not seem to be an exaggerated arginine-vasopressin release as derived from Copeptin concentrations. This finding does not exclude that Copeptin levels may be increased in patients with a fulminant course of acute myocarditis, as patients needing pharmacologic or mechanical hemodynamic support were excluded from the current study.
The present study might have some limitations. First, it is a rather small, single-centre study. In particular concerning the prognostic value, our study may be underpowered. The limited study size and the low number of events may—in part—account for the lack of prognostic utility of the novel biomarker MR-proADM. Another limitation is the rather low number of subjects with acute myocarditis compared to chronic myocarditis cases which hampers the generalizability of our results and requires further large scale studies. Additionally, measurements of biomarkers during follow-up period were lacking. The time course of those concentrations might be helpful in identifying patients with ongoing myocardial inflammation.
Conclusions
After exclusion of other common causes of troponin elevations (e.g. coronary artery disease, tachyarrhythmia, hypertensive crisis, cardiac decompensation) an elevated hs-Troponin T (>50 pg/ml) is highly predictive for the diagnosis of acute myocarditis. As in other cardiac dysfunction states NT-proBNP is a valuable prognostic marker in patients with clinically suspected myocarditis. Newer cardiac biomarkers like MR-proADM or Copeptin do not confer additional diagnostic or prognostic information in this setting.
Abbreviations
- AM:
-
Acute myocarditis
- CK:
-
Creatinine kinase
- CM:
-
Chronic myocarditis
- EMB:
-
Endomyocardial biopsy
- HF:
-
Heart failure
- Hs-TnT:
-
High-sensitive troponin T
- LVEF:
-
Left ventricular ejection fraction
- MRI:
-
Magnetic resonance imaging
- MR-proADM:
-
Mid-regional pro-adrenomedullin
- NM:
-
No myocardial inflammation
- NT-proBNP:
-
N-terminal pro-B-type natriuretic peptide
- ROC:
-
Receiver operating characteristic
References
Cooper LT Jr (2009) Myocarditis. N Engl J Med 360:1526–1538
Kindermann I, Barth C, Mahfoud F et al (2012) Update on myocarditis. J Am Coll Cardiol 59:779–792
Richardson P, McKenna W, Bristow M et al (1996) Report of the 1995 World Health Organization/International Society and Federation of Cardiology Task Force on the Definition and Classification of cardiomyopathies. Circulation 93:841–842
Yilmaz A, Kindermann I, Kindermann M et al (2010) Comparative evaluation of left and right ventricular endomyocardial biopsy: differences in complication rate and diagnostic performance. Circulation 122:900–909
Lauer B, Niederau C, Kuhl U et al (1997) Cardiac troponin T in patients with clinically suspected myocarditis. J Am Coll Cardiol 30:1354–1359
Takemura G, Fujiwara H, Takatsu Y et al (1995) Venticular expression of atrial and brain natriuretic peptides in patients with myocarditis. Int J Cardiol 52:213–222
Meissner J, Nef H, Darga J et al (2011) Endogenous stress response in Tako-Tsubo cardiomyopathy and acute myocardial infarction. Eur J Clin Invest 41:964–970
Maisel A, Mueller C, Nowak R et al (2010) Mid-region pro-hormone markers for diagnosis and prognosis in acute dyspnea: results from the BACH (biomarkers in acute heart failure) trial. J Am Coll Cardiol 55:2062–2076
Kindermann I, Kindermann M, Kandolf R et al (2008) Predictors of outcome in patients with suspected myocarditis. Circulation 118:639–648
Morgenthaler NG, Struck J, Alonso C et al (2006) Assay for the measurement of copeptin, a stable peptide derived from the precursor of vasopressin. Clin Chem 52:112–119
Smith SC, Ladenson JH, Mason JW et al (1997) Elevations of cardiac troponin I associated with myocarditis. Experimental and clinical correlates. Circulation 95:163–168
Mahfoud F, Gartner B, Kindermann M et al (2011) Virus serology in patients with suspected myocarditis: utility or futility? Eur Heart J 32:897–903
Morgera T, Di Lenarda A, Dreas L et al (1992) Electrocardiography of myocarditis revisited: clinical and prognostic significance of electrocardiographic changes. Am Heart J 124:455–467
Di Bella G, Florian A, Oreto L et al (2012) Electrocardiographic findings and myocardial damage in acute myocarditis detected by cardiac magnetic resonance. Clin Res Cardiol 101:617–624
Ukena C, Mahfoud F, Kindermann I et al (2011) Prognostic electrocardiographic parameters in patients with suspected myocarditis. Eur J Heart Fail 13:398–405
Blauwet LA, Cooper LT (2010) Myocarditis. Prog Cardiovasc Dis 52:274–288
Pauschinger M, Noutsias M, Lassner D et al (2006) Inflammation, ECG changes and pericardial effusion: whom to biopsy in suspected myocarditis? Clin Res Cardiol 95:569–583
Friedrich MG, Sechtem U, Schulz-Menger J et al (2009) Cardiovascular magnetic resonance in myocarditis: a JACC white paper. J Am Coll Cardiol 53:1475–1487
De Cobelli F, Pieroni M, Esposito A et al (2006) Delayed gadolinium-enhanced cardiac magnetic resonance in patients with chronic myocarditis presenting with heart failure or recurrent arrhythmias. J Am Coll Cardiol 47:1649–1654
Kuhl U, Pauschinger M, Seeberg B et al (2005) Viral persistence in the myocardium is associated with progressive cardiac dysfunction. Circulation 112:1965–1970
Kuhl U, Lassner D, Pauschinger M et al (2008) Prevalence of erythrovirus genotypes in the myocardium of patients with dilated cardiomyopathy. J Med Virol 80:1243–1251
Corcioli F, Zakrzewska K, Rinieri A et al (2008) Tissue persistence of parvovirus B19 genotypes in asymptomatic persons. J Med Virol 80:2005–2011
Stewart GC, Lopez-Molina J, Gottumukkala RV et al (2011) Myocardial parvovirus B19 persistence: lack of association with clinicopathologic phenotype in adults with heart failure. Circ Heart Fail 4:71–78
Keller T, Tzikas S, Zeller T et al (2010) Copeptin improves early diagnosis of acute myocardial infarction. J Am Coll Cardiol 55:2096–2106
Afzali D, Erren M, Pavenstadt HJ et al (2013) Impact of copeptin on diagnosis, risk stratification, and intermediate-term prognosis of acute coronary syndromes. Clin Res Cardiol 102:755–763
Acknowledgments
CU, FM, IK, and MB are supported by the Ministry of Science and Economy of the Saarland. CU, FM, and MB are supported by the Deutsche Forschungsgemeinschaft (KFO 196). FM is supported by Deutsche Gesellschaft für Kardiologie und Deutsche Hochdruckliga. RK is supported by the Deutsche Forschungsgemeinschaft (SFB/TR19 “Inflammatory Cardiomypathy”, B5).
Conflict of interest
CU has received speakers’ honoraria by BRAHMS/ThermoFisher, Germany.
Author information
Authors and Affiliations
Corresponding author
Additional information
The two authors contributed equally to the study.
Rights and permissions
About this article
Cite this article
Ukena, C., Kindermann, M., Mahfoud, F. et al. Diagnostic and prognostic validity of different biomarkers in patients with suspected myocarditis. Clin Res Cardiol 103, 743–751 (2014). https://doi.org/10.1007/s00392-014-0709-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-014-0709-z