Abstract
Background
Cardiac disease management programmes (CHD-DMPs) and secondary cardiovascular prevention guidelines aim to improve complex care of post-myocardial infarction (MI) patients. In Germany, CHD-DMPs, in addition to incorporating medical care according to guidelines (guideline-care), also ensure regular quarterly follow-up. Thus, our aim was to examine whether CHD-DMPs increase the frequency of guideline-care and whether CHD-DMPs and guideline-care improve survival over 4 years.
Methods
The study included 975 post-MI patients, registered by the KORA-MI Registry (Augsburg, Germany), who completed a questionnaire in 2006. CHD-DMP enrolment was reported by physicians. Guideline-care was based on patient reports regarding medical advice (smoking, diet, or exercise) and prescribed medications (statins and platelet aggregation inhibitors plus beta-blockers or renin-angiotensin inhibitors). All-cause mortality until December 31, 2010 was based on municipal registration data. Cox regression analyses were adjusted for age, sex, education, years since last MI, and smoking and diabetes.
Results
Physicians reported that 495 patients were CHD-DMP participants. CHD-DMP participation increased the likelihood of receiving guideline-care (odds ratio 1.55, 95 % CI 1.20; 2.02) but did not significantly improve survival (hazard rate 0.90, 95 % CI 0.64–1.27). Guideline-care significantly improved survival (HR 0.41, 95 % CI 0.28; 0.59). Individual guideline-care components, which significantly improved survival, were beta-blockers, statins and platelet aggregation inhibitors. However, these improved survival less than guideline-care.
Conclusions
This study shows that CHD-DMPs increase the likelihood of guideline care and that guideline care is the important component of CHD-DMPs for increasing survival. A relatively high percentage of usual care patients receiving guideline-care indicate high quality of care of post-MI patients. Reasons for not implementing guideline-care should be investigated.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary heart disease (CHD) remains one of the leading causes of mortality and morbidity in industrial countries. In 2010, ischaemic heart disease accounted for 16 % of all deaths in Germany [1]. Reported age-standardized death rates for CHD in 2008 showed that the rate in Germany at 75 per 100,000 was similar to rates in the UK (69/100,000) and the USA (81/100,000), but higher than in France (29/100,000) and Italy (52/100,000) [2]. National and international prevention guidelines address the treatment of risk factors such as hypertension, smoking, diabetes and hypercholesterolemia [3]. Disease management programmes (DMPs) use such evidence-based guidelines to define appropriate investigations, treatment and follow-up for CHD patients. In Germany, DMPs for CHD (CHD-DMPs) were introduced in 2003 for patients with statutory health insurance (SHI) which insured about 85 % of the population in 2012. Participation in CHD-DMP is voluntary, but patients must provide consent to be enrolled and they are excluded from the programme if follow-up requirements are not fulfilled [4, 5]. CHD-DMP guidelines regarding medical care are similar to European and American guidelines regarding the importance of medical advice about diet, exercise and smoking and the appropriate medications [3, 6]. Although guidelines provide numerous references for individual recommendations, only few studies have evaluated the effect on endpoints if most or all guideline recommendations are fulfilled [7].
In 2012, 1.7 million patients were enrolled in CHD-DMP in Germany [4]. This corresponds to about 30 % of cardiovascular patients (own calculations based on federal statistics office data) [8, 9]. While enrolment in DMPs for type 2 diabetes has been shown to be associated with improved survival based on health insurance data, similar studies for CHD-DMP have not been performed [10, 11]. However, CHD-DMP participation of post-myocardial infarction (MI) patients has been shown to increase the frequency of medical advice regarding diet, exercise and smoking and treatment with statins and platelet aggregation inhibitors (PAI) [12].
Because of the improved care of patients enrolled in CHD-DMP and its aim to fulfil guidelines, based on a cohort of post-MI patients, it was our objective to evaluate:
-
1.
Whether enrolment in CHD-DMP improves survival?
-
2.
Whether medical care which is mostly adherent to published guidelines (guideline care) is provided more frequently in CHD-DMP and whether this improves survival?
-
3.
Which individual components of CHD-DMP and secondary prevention guidelines (if any) lead to increased survival?
Methods
Patients
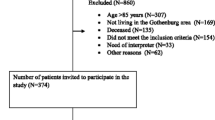
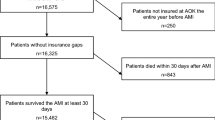
Patients included in our study had previously had an MI and were registered in the KORA (Cooperative Health Research in the Augsburg Region) Myocardial Infarction Registry [13, 14]. As described elsewhere, included patients had filled in a postal questionnaire regarding their medical care in 2006 [12]. Physicians were then asked to report CHD-DMP enrolment status (yes/no) for all patients reporting DMP enrolment (n = 665) and 1/3 of patients denying enrolment (n = 583). Physicians reported CHD-DMP status for 1,128 patients, a response rate of 90 %. Of these, 153 patients were excluded from further analyses for various reasons as shown in Fig. 1. A total of 975 patients was included in the follow-up study. All patients provided informed consent. Data collection and follow-up questionnaires of the KORA MI Registry have been approved by the Bavarian State Ethics Committee.
Study design and patient selection. * “Patients not eligible for DMP” is based on physician’s comment and they were excluded because of heart transplant (n = 1), dementia (n = 1), nursing home admission (n = 1), metastatic rectal cancer (n = 1), non-compliance (n = 3), living outside the country (n = 1)
Based on patient reports in the 2006 survey, the presence of the following aspects of secondary prevention guidelines (guideline care) which are included in CHD-DMP were evaluated for all patients: whether the physician had provided advice regarding diet, exercise or smoking (or patient is non-smoker) within the last year and whether the patient had taken beta-blockers, statins, agents acting on the renin-angiotensin system (ACE-inhibitors or angiotensin II antagonists labelled as RAI) or PAIs within the last week. Medications were identified on the basis of their Anatomical Therapeutic Chemical (ATC) code. Other aspects of CHD-DMP, such as coordination of care, referrals and psychological support, could not be evaluated based on our data [5]. Guideline-care was defined as being present when the patient reported receiving medical advice for at least two of three topics covering diet, exercise, or smoking and reported the intake of a PAI and a statin and either a beta-blocker or an RAI. Lack of a beta-blocker or RAI could indicate a contraindication or hypotension precluding the intake of both antihypertensives [15].
The study start of the survival analysis was defined as the date on which patients completed their survey questionnaire in 2006. CHD-DMP participation was present if the physician documented an enrolment date before or on the study start. For nine patients, the physician verified DMP enrolment but did not document the DMP start date, thus the DMP start date documented by the patient was used. Patients not enrolled in a CHD-DMP at study start were designated as controls. However, controls that were later enrolled in CHD-DMP were censored at the time point of CHD-DMP enrolment. Patients were defined as having diabetes if this was documented in the KORA MI Registry, in the patient survey, if the patient documented the intake of diabetes medications or if the patient was enrolled in a diabetes-DMP.
The survival analysis examined all-cause-mortality until December 31, 2010. In order to determine whether patients were living or deceased at follow-up, the responsible municipal registration office according to the last reported address was contacted. If the patient was deceased, date and place of death were provided by the registration office, otherwise the address was either confirmed or a new address was provided and the next registration office was contacted until a definite status (living versus deceased) was determined.
Confounders used in the analysis originated either from information from the KORA MI Registry (age, sex, education, date of last MI, history of peripheral artery disease (PAD), history of revascularization such as thrombolysis, angioplasty or a coronary bypass operation) or from patient reports in the 2006 survey (smoking status, height and weight to calculate BMI). The Visual Analogue Scale of the Euroqol-5D was examined as an indicator of health-related quality of life (HRQoL) [16].
Statistics
There were no missing values for mortality status, CHD-DMP status, age, sex, education, time since last MI and diabetes. Missing data for other independent variables (see Table 1) were imputed, assuming data were missing at random. Single imputation was performed using Markov-chain Monte-Carlo method, accounting for all variables required for the analyses and for HRQoL [17]. Reported results show imputed values unless stipulated otherwise. Baseline comparisons are two-tailed and use the Wilcoxon test for continuous variables and Chi-squared test for class variables.
The regression analyses were adjusted for the confounders: age, sex, education, smoking status in 2006, and time since last MI, diabetes diagnosis, PAD and history of revascularization. The association of guideline-care with CHD-DMP participation was evaluated using logistic regression. Survival analyses were performed using Cox proportional hazards regression. As mentioned above, patients who were enrolled in CHD-DMP after the starting point of the study (completion of the questionnaire) were censored to the time point of CHD-DMP enrolment in the Cox proportional hazards regression. All analyses were performed using SAS 9.2, and variables with a p value <0.05 were considered significant.
Results
Baseline characteristics
Of 1,128 patients whose CHD-DMP participation was verified, 153 patients were excluded for reasons shown in Fig. 1, leaving 975 patients included in this study. These subjects had an average age of 67.8 (range 34.4–87.9), 78 % were male and 33 % had diabetes. Physicians reported that 495 patients were participating in CHD-DMP at study start in 2006, while 480 were not enrolled at that time and thus were designated as controls. However, 94 controls were enrolled in CHD-DMP after study start until the end of 2007. CHD-DMP participants had been enrolled in the programme for a median of 0.9 years (range 0–2.8 years). Baseline patient characteristics according to CHD-DMP enrolment are shown in Table 1. Demographic variables were similar between the groups, but the last MI of CHD-DMP participants was more recent than that of controls. According to physician reports, 19 % of controls and 24 % of CHD-DMP participants were enrolled in the DMP for type 2 diabetes at start of study. Comparison of CHD-DMP participants and controls regarding their self-reported medical care in 2006 (Table 1) revealed that CHD-DMP participants more frequently reported receiving medical advice regarding diet and exercise. They also reported the intake of statins, RAI and PAIs more frequently. Guideline-care was more frequently reported by CHD-DMP participants. Overall 55 % of patients in our sample received guideline-care. As also shown in Table 1, patients receiving guideline-care were younger (66.7 versus 69.1 years), their last MI was more recent (7.7 versus 9.6 years), a higher proportion had a re-infarction (14.1 versus 9.3 %), they had a higher BMI (28.6 versus 27.7), and more frequently had diabetes (36.3 versus 29.6 %) and more frequently had a revascularization.
Multivariate analysis of factors associated with receiving guideline-care showed that enrolment in CHD-DMP (odds ratio (OR) 1.54, 95 % CI 1.19–2.01), having diabetes (OR 1.48, 95 % CI 1.12–1.97), fewer years since the last MI (OR 0.94, 95 % CI 0.92–0.97) and revascularization (OR 1.45, 95 % CI 1.06–1.99) increased the likelihood of receiving guideline-care.
Evaluation of survival revealed that 141 patients had died until the end of 2010 (see Fig. 1). Comparison of mortality between CHD-DMP participants and controls is shown in Fig. 2 and indicates some difference between the groups. The unadjusted survival analysis showed that CHD-DMP participation reduced mortality risk by about 25 % (hazard ratio (HR) 0.73, 95 % CI 0.52–1.03). Adjusting for confounders showed an HR of 0.90 (see Table 2). The unadjusted survival analysis of patients receiving guideline-care showed that all-cause-mortality was reduced by 66 % (HR 0.34, 95 % CI 0.24–0.49). Adjusting for confounders resulted in an HR of 0.41 (see Table 2). Further adjustment for BMI (which was significantly different between the groups) and HRQoL resulted in a HR of 0.44 (95 % CI 0.30–0.64) (Fig. 3).
Survival analysis of the individual components of the CHD-DMP shows that the intake of beta-blockers, statins and PAIs were the components of the CHD-DMP programme and of guideline-care, which were independently associated with increased survival (see Table 2). However, the risk reduction of the individual medications was less than the combined therapy of guideline-care.
Discussion
CHD-DMPs were introduced to improve medical care of patients with coronary heart disease. Our study examined a sample of patients with a previous MI. We found that CHD-DMP participants more frequently reported appropriate medical care and were more likely to receive guideline-care. However, CHD-DMP participation did not significantly improve survival. We found that 60 % of CHD-DMP participants and almost 50 % of controls were receiving guideline-care and guideline-care significantly improved survival. Examination of the individual CHD-DMP components showed that beta-blockers, statins and platelet aggregation inhibitors significantly improved survival but the individual effect was lower than the combination in guideline-care.
In CHD-DMP, regulations define appropriate therapies, follow-up and clinical parameters which are documented by physicians and submitted for evaluation. The submitted data is used to provide individual feedback to physicians regarding their performance and to evaluate intermediate outcomes of CHD-DMP participants. Improvements in individual healthcare processes associated with DMPs have been shown for CHD and diabetes [12, 18, 19]. However, changes in complex care, such as guideline-care, have not been previously evaluated. Some trials of secondary prevention of CHD have evaluated the achievement of single treatment goals, but not the use of combined treatments [20, 21]. Our analyses show that post-MI patients who are enrolled in CHD-DMP or who are perceived to have an increased risk, patients with diabetes or a recent MI, are more likely to receive guideline-care. However, cardiovascular mortality risk for post-MI patients persists at 5 % per year after the first MI and at 10 % per year after the second MI for many years (independent of age and sex) if patients do not receive effective preventative treatment [22].
CHD-DMP enrolment did not significantly improve survival in our study. This may have been due to an inadequate sample size, especially considering that we only observed a 10 % difference in hazard ratio. However, no previous studies of a similar CHD-DMP intervention were available on which to base a sample size calculation. Furthermore, revascularization has improved prognosis after an acute myocardial infarction in the last years [23]. Examining the effect of CHD-DMP enrolment in the subgroup of patients who had a revascularization in the past and whose last myocardial infarction was at most 8 years prior to study start (n = 451), shows that CHD-DMP does have a significant effect on mortality (HR 0.50, 95 % CI 0.27–0.93) when adjusting for age, sex, education, smoking and PAD. This effect becomes not significant but indicates a trend (HR 0.58, 95 % CI 0.31–1.10) if further adjustment for guideline-care is made. Studies using SHI data have shown an association between increased survival and diabetes-DMP for Germany [10, 11]. These studies found significant differences in survival ranging from 3.1 to 6.6 %. They had a large number of patients available for analysis but also lacked randomisation and were not population-based. The observed improvement in survival associated with guideline-care has not been previously shown. Since our study was not randomised, selection bias must be considered. A review of ten studies of secondary prevention programmes for CHD (randomised clinical trials) published until the year 2000, found no survival advantage (summary risk ratio 0.91, 95 % CI 0.79–1.04) but did show a risk reduction for hospitalisations of 0.84 (95 % CI 0.79–0.94) [24]. However, the reviewed studies only assessed diet and exercise interventions. Newer secondary prevention programmes in CHD patients have shown improved blood pressure and cholesterol control and a reduction in patients requiring hospitalisation but have not reported survival [21, 25]. Trials evaluating outcomes with respect to whether therapy is consistent with guidelines often evaluate whether guidelines are fulfilled on discharge from hospital [7, 26, 27]. One of these studies showed a 1-year survival advantage for patients after an acute MI treated with aspirin, an ACE-inhibitor and a statin added to beta-blockers, but the patients were not randomised [7].
The individual components of the CHD-DMP and guideline-care which were associated with improved survival only correspond to a subset of guideline-care. We found improved survival associated with statins, beta-blockers and antiplatelet agents. Statins have been shown to improve survival even for patients with a low risk of vascular disease [28]. Also blood pressure-reducing drugs (including beta-blockers and RAIs) have been shown to proportionally reduce cardiovascular disease regardless of pre-treatment blood pressure [29]. The use of aspirin is also recommended in secondary prevention, reducing the incidence of serious vascular events [30]. Although medical advice for diet and exercise were individually not associated with survival, this may indicate that their effect is not independent of drug treatment in secondary prevention or may reflect the difficulty of translating medical advice into changes in patient behaviour. Special patient education programmes regarding diet or exercise are not part of the CHD-DMP. However, given an exact protocol, the importance and independent effect of diet in cardiovascular mortality has been recently shown [31]. Thus numerous studies show the importance of the individual components of guideline-care, but guideline-care shows the importance of the combination of the individual components—the additive effect of these components—since this leads to a higher risk reduction than associated with any single component.
Our study has several methodological limitations. Since patients are not randomised regarding either DMP participation or guideline-care, treatment choices may reflect selection bias [32]. Although a randomised trial protocol was available, DMPs were politically legislated before these studies were performed [33]. CHD-DMP enrolment was also not consistent during the study since 20 % of controls were enrolled in CHD-DMP shortly after the study start date. However, censoring controls who enrolled in CHD-DMP after study start to the time point of CHD-DMP enrolment attempted to control for their change in status in the survival analysis. This also illustrates the difficulty of excluding treatment spill-over effects in medical practices with both types of patients, especially since physicians in DMP must participate in additional medical education. Of the 97 controls enrolled in CHD-DMP after the study start date, 65 % already reported receiving guideline-care in 2006. Furthermore, both CHD-DMP enrolment, guideline-care and its components (diet, exercise and medications) were not evaluated during the follow-up period. Thus patients may have changed their status, but this is not accounted for in the analysis which would be compatible with an intention to treat analysis. Selection bias may also determine which patients receive guideline-care since the care of patients with other severe comorbidities (e.g. cancer), will not focus on secondary prevention of CHD. The failure to receive guideline-care may also indicate a poor health status. For example, patients may not receive PAIs if they are receiving oral anticoagulants such as for atrial fibrillation. Overall cardiovascular risk of patients in 2006 cannot be established from our data, however the risk of patients in CHD-DMP may be higher since their last MI was more recent. Adjustments for HRQoL attempted to account for unknown differences in health status. Lack of recent laboratory and clinical measurements (e.g. blood pressure, LDL-cholesterol) and patient-reported medication intake are further study limitations. Thus, it is unknown whether factors such as lipid levels or hypertension are being adequately controlled or if all medications were reported by patients. Also important confounders such as heart failure, left ventricular ejection fraction, heart rate and renal failure were not available for analysis, which also limits the explanatory power of the results [34, 35].
The advantage of our study is that individual processes and complex aspects of CHD care could be evaluated in a population-based study. The association of this care with survival was analysed adjusting for socio-demographic variables not available in health insurance data. The control group and the starting point of the study were exactly defined. Furthermore, we evaluated how well the therapy of these high risk post-MI patients complied with German CHD-DMP and international guidelines and showed that guideline-care improved survival, a result which is not restricted only to Germany. Since enrolment in CHD-DMP was significantly associated with receiving guideline-care, it is possible that the DMP has increased awareness of the guidelines and adherence to them and has also improved the care of patients not enrolled in CHD-DMP.
Conclusions
This is the first population-based study to show that CHD-DMP increases the likelihood of receiving guideline-care in post-MI patients. Although CHD-DMP improved survival only insignificantly, adherence to guideline-care significantly improved survival. Our results indicate that larger studies are required to evaluate the effect of CHD-DMP on survival but that randomised controlled trials are actually required to evaluate the effect of CHD-DMPs and guideline-care on survival.
References:
Federal Ministry of Health Mortality statistics. Available from URL: www.gbe-bund.de/gbe10/F?F=14187D. Accessed on 01.08.2012
WHO (2012) Global atlas on cardiovascular disease prevention and control available on http://www.who.int/cardiovascular_diseases/publications/atlas_cvd/en/index.html. Accessed 08.07.2013
Smith SC Jr, Allen J, Blair SN, Bonow RO, Brass LM, Fonarow GC, Grundy SM, Hiratzka L, Jones D, Krumholz HM, Mosca L, Pasternak RC, Pearson T, Pfeffer MA, Taubert KA (2006) AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update: endorsed by the National Heart, Lung, and Blood Institute. Circulation 113(19):2363–2372. doi:10.1161/CIRCULATIONAHA.106.174516
Federal Insurance Agency Basic facts of disease management programs in Germany, http://www.bundesversicherungsamt.de/cln_115/nn_1046154/DE/DMP/dmp__inhalt.html. Accessed 2 Aug 2012
Federal Joint Committee Directives regarding disease management programs in Germany, http://www.g-ba.de/downloads/62-492-353/2009-07-01-RSAV20.pdf (see page 1552 regarding CHD-DMP). Accessed November 6, 2012 2012
Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren M, Albus C, Benlian P, Boysen G, Cifkova R, Deaton C, Ebrahim S, Fisher M, Germano G, Hobbs R, Hoes A, Karadeniz S, Mezzani A, Prescott E, Ryden L, Scherer M, Syvanne M, Scholte op Reimer WJ, Vrints C, Wood D, Zamorano JL, Zannad F, European Association for Cardiovascular P, Rehabilitation, Guidelines ESCCfP (2012) European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth joint task force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Eur Heart J 33(13):1635–1701. doi:10.1093/eurheartj/ehs092
Zeymer U, Junger C, Zahn R, Bauer T, Bestehorn K, Senges J, Gitt A (2011) Effects of a secondary prevention combination therapy with an aspirin, an ACE inhibitor and a statin on 1-year mortality of patients with acute myocardial infarction treated with a beta-blocker. Support for a polypill approach. Curr Med Res Opin 27(8):1563–1570. doi:10.1185/03007995.2011.590969
Federal Statistics Office Annual German Population on December 31st of each year, www.gbe-bund.de/gbe10/F?F=262D. Accessed 2 Aug 2012
Federal Statistics Office Prevalence of coronary heart disease diagnosed by a physician based on patient reports, www.gbe-bund.de/gbe10/F?F=204D Accessed 2 Aug 2012
Miksch A, Laux G, Ose D, Joos S, Campbell S, Riens B, Szecsenyi J (2010) Is there a survival benefit within a German primary care-based disease management program? Am J Manag Care 16(1):49–54. doi:12562
Drabik A, Buscher G, Thomas K, Graf C, Muller D, Stock S (2012) Patients with type 2 diabetes benefit from primary care-based disease management: a propensity score matched survival time analysis. Popul Health Manag 15(4):241–247. doi:10.1089/pop.2011.0063
Gapp O, Schweikert B, Meisinger C, Holle R (2008) Disease management programmes for patients with coronary heart disease—an empirical study of German programmes. Health Policy 88(2–3):176–185. doi:10.1016/j.healthpol.2008.03.009
Holle R, Happich M, Lowel H, Wichmann HE, Group MKS (2005) KORA—a research platform for population based health research. Gesundheitswesen 67(Suppl 1):S19–S25. doi:10.1055/s-2005-858235
Kirchberger I, Heier M, Kuch B, Wende R, Meisinger C (2011) Sex differences in patient-reported symptoms associated with myocardial infarction (from the population-based MONICA/KORA Myocardial Infarction Registry). Am J Cardiol 107(11):1585–1589. doi:10.1016/j.amjcard.2011.01.040
Hostetter JC, Ghaffari S (2003) Should everyone with a recent myocardial infarction receive a beta-blocker and an ACE inhibitor? Clevel Clin J Med 70(1):46–48
Leidl R, Reitmeir P (2011) A value set for the EQ-5D based on experienced health states: development and testing for the German population. Pharmacoeconomics 29(6):521–534. doi:10.2165/11538380-000000000-00000
Horton NJ, Lipsitz SR (2001) Multiple imputation in practice: comparison of software packages for regression models with missing variables. Am Stat 55(3):244–254
Schunk M, Stark R, Reitmeir P, Rathmann W, Meisinger C, Holle R (2011) Improvements in type 2 diabetes care? Pooled analysis of survey data in southern Germany (KORA) from 1999-2008. Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz 54(11):1187–1196. doi:10.1007/s00103-011-1364-4
Stark RG, Schunk MV, Meisinger C, Rathmann W, Leidl R, Holle R, Grp KS (2011) Medical care of type 2 diabetes in German disease management programmes: a population-based evaluation. Diabetes Metab Res 27(4):383–391
Jolly K, Bradley F, Sharp S, Smith H, Thompson S, Kinmonth AL, Mant D (1999) Randomised controlled trial of follow up care in general practice of patients with myocardial infarction and angina: final results of the Southampton heart integrated care project (SHIP). The SHIP Collaborative Group. BMJ 318(7185):706–711
Khunti K, Stone M, Paul S, Baines J, Gisborne L, Farooqi A, Luan X, Squire I (2007) Disease management programme for secondary prevention of coronary heart disease and heart failure in primary care: a cluster randomised controlled trial. Heart 93(11):1398–1405. doi:10.1136/hrt.2006.106955
Law MR, Watt HC, Wald NJ (2002) The underlying risk of death after myocardial infarction in the absence of treatment. Arch Intern Med 162(21):2405–2410
Kuch B, Heier M, von Scheidt W, Kling B, Hoermann A, Meisinger C (2008) 20-year trends in clinical characteristics, therapy and short-term prognosis in acute myocardial infarction according to presenting electrocardiogram: the MONICA/KORA AMI Registry (1985-2004). J Intern Med 264(3):254–264. doi:10.1111/j.1365-2796.2008.01956.x
McAlister FA, Lawson FM, Teo KK, Armstrong PW (2001) Randomised trials of secondary prevention programmes in coronary heart disease: systematic review. BMJ 323(7319):957–962
Murphy AW, Cupples ME, Smith SM, Byrne M, Byrne MC, Newell J (2009) Effect of tailored practice and patient care plans on secondary prevention of heart disease in general practice: cluster randomised controlled trial. BMJ 339:b4220. doi:10.1136/bmj.b4220
Bailey TC, Noirot LA, Gage BF, Li X, Shannon WD, Waterman B, Sinha S, Bouselli DA, Reichley RM, Goldberg AC, Dunagan WC (2006) Improving adherence to coronary heart disease secondary prevention medication guidelines at a community hospital. AMIA Annual Symposium proceedings/AMIA Symposium AMIA Symposium:850
Tickoo S, Fonarow GC, Hernandez AF, Liang L, Cannon CP (2008) Weekend/holiday versus weekday hospital discharge and guideline adherence (from the American Heart Association’s get with the guidelines—coronary artery disease database). Am J Cardiol 102(6):663–667. doi:10.1016/j.amjcard.2008.04.053
Ctt C Cholesterol Treatment Trialists’ (2012) The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. doi:10.1016/S0140-6736(12)60367-5
Law MR, Morris JK, Wald NJ (2009) Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ 338:b1665. doi:10.1136/bmj.b1665
Antithrombotic Trialists C, Baigent C, Blackwell L, Collins R, Emberson J, Godwin J, Peto R, Buring J, Hennekens C, Kearney P, Meade T, Patrono C, Roncaglioni MC, Zanchetti A (2009) Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet 373(9678):1849–1860. doi:10.1016/S0140-6736(09)60503-1
Estruch R, Ros E, Salas-Salvado J, Covas MI, Corella D, Aros F, Gomez-Gracia E, Ruiz-Gutierrez V, Fiol M, Lapetra J, Lamuela-Raventos RM, Serra-Majem L, Pinto X, Basora J, Munoz MA, Sorli JV, Martinez JA, Martinez-Gonzalez MA, Investigators PS (2013) Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med 368(14):1279–1290. doi:10.1056/NEJMoa1200303
Danaei G, Tavakkoli M, Hernan MA (2012) Bias in observational studies of prevalent users: lessons for comparative effectiveness research from a meta-analysis of statins. Am J Epidemiol 175(4):250–262. doi:10.1093/aje/kwr301
Joos S, Rosemann T, Heiderhoff M, Wensing M, Ludt S, Gensichen J, Kaufmann-Kolle P, Szecsenyi J (2005) ELSID-Diabetes study-evaluation of a large scale implementation of disease management programmes for patients with type 2 diabetes. Rationale, design and conduct—a study protocol [ISRCTN08471887]. BMC Public Health 5:99. doi:10.1186/1471-2458-5-99
Azaouagh A, Churzidse S, Konorza T, Erbel R (2011) Arrhythmogenic right ventricular cardiomyopathy/dysplasia: a review and update. Clinical Res Cardiol Off J Ger Cardiac Soc 100(5):383–394. doi:10.1007/s00392-011-0295-2
Dabiri Abkenari L, Theuns DA, Valk SD, Van Belle Y, de Groot NM, Haitsma D, Muskens-Heemskerk A, Szili-Torok T, Jordaens L (2011) Clinical experience with a novel subcutaneous implantable defibrillator system in a single center. Clin Res Cardiol Off J Ger Cardiac Soc 100(9):737–744. doi:10.1007/s00392-011-0303-6
Acknowledgments
The KORA research platform (KORA, Cooperative Research in the Region of Augsburg) was initiated and financed by the Helmholtz Zentrum München—German Research Center for Environmental Health, which is funded by the German Federal Ministry of Education and Research and by the State of Bavaria. The survival analysis was part of the project “Medium term effects of Disease Management Programs for Coronary Heart Disease” funded by the Federal Association of Statutory Regional Health Funds (AOK Bundesverband). We thank all members of the Helmholtz Zentrum München who are involved in the conduct of the study. Furthermore, we wish to thank the field staff in Augsburg, especially Claudia Greschik, Dorothea Lukitsch, and Gisela Sietas.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stark, R., Kirchberger, I., Hunger, M. et al. Improving care of post-infarct patients: effects of disease management programmes and care according to international guidelines. Clin Res Cardiol 103, 237–245 (2014). https://doi.org/10.1007/s00392-013-0643-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-013-0643-5