Abstract
Aims
Heart failure is known to profoundly affect health-related quality of life (HRQoL). We aimed to describe both generic and disease-specific HRQoL in a large community-based sample of patients with systolic heart failure (SHF) and to identify important somatic and psychosocial correlates.
Methods and results
Seven hundred and two patients, 67 ± 12 years old, 71 % men, with distributions of New York Heart Association (NYHA) functional classes I/II/III/IV of 2/55/39/4 % were included in this cross-sectional analysis. Generic HRQoL was measured with the SF-36 health survey, disease-specific HRQoL with the Kansas City Cardiomyopathy Questionnaire, and depression with the self-reported Patient Health Questionnaire (PHQ-9). Both generic- and disease-specific HRQoL measurements indicated moderate to poor HRQoL. The KCCQ scores demonstrated higher sensitivity to the varying levels of heart failure severity as compared to the SF-36 scores. Patients with either a minor (15 %) or a major depression (24 %) reported significantly and substantially lower HRQoL (p < .001) than patients without depression did. In multivariable regression analyses, depression accounted for the largest part of the variance of both generic and specific HRQoL (12 and 36 %, respectively), whereas most biomedical variables had no or only a marginal influence.
Conclusion
Patients with SHF suffer from severe limitations of HRQoL. Depression was the most important correlate of both generic and disease-specific HRQoL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systolic heart failure (SHF) is recognized as an increasing public health concern among the aging populations of industrialized countries [1]. Patients with heart failure have a high mortality risk [2, 3] and a serious impairment in all generic and disease-specific domains of health-related quality of life (HRQoL) [4–8]. Comorbid depression and panic disorders occur in these patients at a three- to five-times higher rate than in the general population [2, 9–11]. Many studies have shown an additional negative influence of depression on prognosis [11–13].
In our previous research, we discovered that comorbid major depression was closely related to disease severity and clinical features of SHF [11]. Studies analyzing correlates of low HRQoL indicate an association with New York Heart Association (NYHA) functional class and various socio-demographic variables, including younger age, social support and female sex [2, 14, 15]. In most studies, objective measures of SHF severity, such as indicators of left ventricular function, were not associated with self-reported HRQoL [16, 17]. However, when psychosocial factors were considered, they contributed substantially to the explained variance [18, 19].
To clarify the significance of individual variables associated with HRQoL, detailed analyses of the various facets of the heart failure syndrome are needed, including objective measures of SHF severity, somatic comorbidities, socio-demographic and psychosocial variables, and patient mood parameters. Only a few previous studies investigating the significance of HRQoL in patients with SHF were performed with large samples and systematically explored disease-specific HRQoL in addition to generic HRQoL, which may allow for a more profound understanding of the HRQoL construct [4, 7, 18, 19]. Moreover most studies failed to recruit a community-based sample, which represent the ‘real world’ heart failure population.
In this paper, we extend our previous research, in which we explored and focussed on the somatic correlates of depression, including blood parameters, such as leucocyte count and hemoglobin level, and certain diseases, such as chronic obstructive pulmonary disease (COPD), diabetes, and hyperuricemia [11]. In contrast, the present study analyses the correlates of HRQoL by including depression as a potential predictor. Furthermore, we provide a detailed description of the generic and disease-specific HRQoL in a large community-based sample of patients suffering from SHF. Further, we aim to clarify important correlates of HRQoL, especially depression.
Methods
The investigation conforms with the principles outlined in the Declaration of Helsinki. The study protocol was approved by the institutional Ethics Committees. Written informed consent was obtained from all patients.
Subjects
The interdisciplinary network for heart failure (INH) at the University of Würzburg Cardiovascular Centre promotes patient-oriented research in community-based heart failure populations. Within this frame, adult patients hospitalized for SHF [echocardiographic left ventricular ejection fraction (LVEF) <40 %] were recruited consecutively in nine hospitals of the Würzburg area to take part in the randomized control INH study [11]. The aim was to obtain a large representative sample of the ‘real world’ heart failure population. Therefore, exclusion criteria were kept to a minimum and comprised only acutely decompensated SHF following new-onset structural heart disease (e.g., acute coronary syndrome), linguistic problems likely to preclude patient evaluation, and patient refusal to complete the psychometric questionnaires. All patients had been hospitalized for aggravated heart failure conditions. However, NYHA functional class as reported in the current manuscript was assessed at randomization, which occurred after best possible recompensation. As such, the symptoms experienced by many patients had improved considerably while in the hospital. LVEF was measured shortly before or after randomization.
Complete reversal of (pulmonary and/or peripheral) edema, i.e., complete recompensation, could not be achieved in all patients. When sufficient dosages of diuretic and concomitant cardiac treatment were documented, but complete stabilization had not yet been achieved, a status of “best possible cardiac recompensation” was accepted.
Procedure
All study participants underwent psychometric evaluation prior to discharge and after best possible cardiac recompensation. The Short Form (SF)-36 Health Survey was used to assess generic HRQoL [20]. The SF-36 is a common international standardized tool with proven reliability and validity [21]. It contains eight subscales, physical function, role-physical, bodily pain, general health, vitality, role-emotional, social function, and mental health, and two summary scales: the physical health (subscales 1–4) and mental health (subscales 5–8) component scores. The mental health component score includes items related to depression so that a high correlation with depression scales (e.g., Patient Health Questionnaire depression module PHQ-9) may be found. The scores range from 0 to 100, with higher scores indicating a better HRQoL.
The patients’ disease-specific HRQoL was measured using the self-reported Kansas City Cardiomyopathy Questionnaire (KCCQ). This recently developed tool was specifically designed for SHF patients, and both the original US [22] and German [23] versions have demonstrated very good reliability and validity. The following areas are covered by the KCCQ: physical function, symptoms (frequency, severity), self-efficacy, quality of life (psychological well-being), and social limitations. The scores range from 0 to 100, with higher scores again indicating a better health status. The functional status summary scale, which indicates the patient’s physical state, is composed of the physical function and symptoms subscales. A clinical summary scale that incorporates all subscales except for self-efficacy is also available.
Depression was assessed using the German version of the Patient Health Questionnaire depression module PHQ-9 [24–26], a self-report screening tool consisting of nine items. It may be used to identify a probable current major or minor depressive episode (no depression: PHQ-Score <9, minor depression: PHQ-Score 9–11, major depression: PHQ-score >11). Compared to other screening tools, the PHQ-9 compared well when evaluated against the structured clinical interview for DSM-IV as a reference standard [26].
A thorough standardized check-up including physical examination, laboratory assessment, 12-lead-electrocardiogram, pulmonary function testing and two-dimensional echocardiography was performed for every patient, as detailed elsewhere [27]. Physicians performing the clinical tests were blinded to the psychometric results.
Data analysis
All statistical analyses were performed using SPSS 14.0 for Windows (SPSS Inc. Chicago, III., USA). For the test of group differences, analyses of variance were used. Inter-collinearity was checked. Block-wise linear regression analyses were applied to identify independent predictors of quality of life outcomes (SF-36 physical and mental health summary scales and the KCCQ clinical summary and functional status scales). Four different blocks of variables, basic socio-demographic variables, medications and indicators of SHF severity, comorbidities and risk factors, and depression, were used. Rationale behind this strategy was to identify the contribution of each block for the prediction of outcomes in a step-by-step manner.
The first block of independent variables consisted of the following socio-demographic variables: age, sex, family status (living alone, living together with a partner) and educational level. A low educational level was assigned to patients who had undergone basic education (8 years) or less, with and without occupational training. The second block added medications, such as diuretics and statins (3-hydroxy-3-methylglutaryl-coenzyme-A-reductase inhibitors), and indicators of SHF severity, such as leukocyte count >8,000 mm−3, NYHA functional class, and LVEF, to the model. The third block additionally included comorbidities and risk factors: hypercholesterolemia (total cholesterol >200 mg/dl or on lipid-lowering drugs), hyperuricemia (uric acid >6.5 mg/dl), diabetes, hypertension (blood pressure >140/90 mmHg or on antihypertensive drugs), renal dysfunction (GFR <60 mL/min/1.73 m2), anemia [hemoglobin (g/dl) <13 (male), <12 (female)], COPD, cerebrovascular disease (transient ischemic attack, apoplexy), coronary heart disease (CHD), obesity (body mass index >30 kg/m2) and current smoking habit. The PHQ-9 summary score was used as a continuous variable in the fourth block. The amount of variance (R 2) explained by the four blocks of variables was determined.
Values are given as means (SD) or percentages, statin; hypercholesterolemia: total cholesterol >200 mg/dl or on lipid-lowering drugs; hyperuricemia: uric acid >6.5 mg/dl; hypertension: blood pressure >140/90 mmHg or on antihypertensive drugs; renal dysfunction: GFR <60 mL/min/1.73 m2; anemia: hemoglobin (g/dl) <13 (male), <12 (female); COPD: chronic obstructive pulmonary disease; obesity: body mass index >30 kg/m2; dpw: drinks per week, 1 drink: 0.25 l of beer or 0.1 l of wine or 0.02 l of hard liquor; major/minor depression: suspected according to PHQ sum: greater than 11 (major depression), between 9 and 11 (minor depression).
Results
Descriptive statistics
Out of 834 eligible patients, 702 patients provided informed consent (rejection rate: 15.8 %) and had complete psychometric, clinical and laboratory data available. Demographic and clinical characteristics, important laboratory parameters, comorbidities, risk factors and information on depression are given in Table 1. The main causes of SHF were CHD in 58 %, cardiomyopathy in 27 %, hypertension in 7 % and other diseases in 9 %.
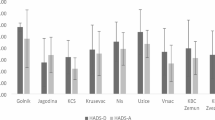
The mean scores of HRQoL according to severity of depression subgroups are summarized in Table 2. As shown, all scales of the SF-36 and the KCCQ indicate moderate to poor HRQoL and correspond to the sum scores of other patients with chronic diseases. Patients with either minor or major depression reported significantly and substantially worse HRQoL than patients without depression did. Figure 1 displays the summary scores of both the SF-36 (physical and mental health component scores) and the KCCQ (functional status, clinical summary scale) by NYHA class. A decrease in HRQoL concurs with increasing severity of SHF according to the NYHA classification. The figure shows that the KCCQ summary scores seems to discriminate patients at different NYHA classes better than the SF-36 summary scores do, particularly in advanced SHF stages. For example, in comparing NYHA classes 1 and 4, the effect sizes of the KCCQ summary scores are much larger than the respective effect sizes of the SF-36 summary scores are, with the KCCQ effects not being included in the 95 % confidence intervals of the SF-36 effects.
Quality of life scores (mean values and standard deviations) by New York Heart Association (NYHA) functional classes. All differences between NYHA classes are significant at p < .001 (ANOVA). SF-36 PCS Short Form-36 Physical Health Component Score; SF-36 MCS Short Form-36 Mental Health Component Score; KCCQ-CS Kansas City Cardiomyopathy Questionnaire Clinical Summary Score; KCCQ-FS Kansas City Cardiomyopathy Questionnaire Functional Status Score
Predictors of health-related quality of life
Tables 3 and 4 detail the results of the block-wise regression analyses of the SF-36 physical and mental health component scores and the KCCQ clinical summary and functional status scales. For each of these variables, the results of the block-wise regression analysis were similar: demographics, as well as clinical predictors and comorbidities, explained only a marginal degree of HRQoL variance (models 1–3), whereas the final model, by adding the PHQ summary score, explained between 31 and 53 % of the variance. The increase of explained variance (∆R 2) from model 3 (without PHQ) to model 4 (including PHQ) was substantial and ranged from 12 to 37 %, respectively. Besides the PHQ sum score, age, NYHA functional class, hyperuricemia, and COPD were significant predictors for the SF-36 scores in the final model. Regarding the KCCQ scales, demographic variables, i.e., gender, family status and education, also contributed significantly to the model. In addition, NYHA functional class, diuretics, hyperuricemia, and coronary artery disease had predictive power.
The final model (model 4) demonstrated that the PHQ sum score had the strongest association with HRQoL: higher PHQ sum scores were associated with lower scores on all four HRQoL summary scales. A lower SF-36 physical health component score was seen in patients with increased depressive symptoms, those with NYHA functional classes III/IV, those of increasing age, and those with hyperuricemia, anemia and COPD. The SF-36 mental health component score was not associated with any other variables in addition to the PHQ sum score. Lower scores in KCCQ functional status were found in depressed patients, females, those who lived alone, patients with a lower educational level, those with NYHA functional classes III/IV, those with hyperuricemia, those with coronary artery disease and those who used diuretics. Lower scores in the KCCQ clinical summary scale were linked with depression, female sex, living alone, NYHA functional classes III/IV, use of diuretics, and hyperuricemia.
Discussion
We have performed a study using a large community-based sample to evaluate the influence of objective measures of SHF severity, somatic comorbidities, socio-demographic variables, and depressive symptoms on both generic and disease-specific HRQoL in patients suffering from SHF.
The findings confirm the large influence of depression on HRQoL summary scores, whereas biomedical predictors showed only marginal effects. This finding holds true for both generic HRQoL as well as disease-specific HRQoL. Most interestingly, factors that were previously identified as correlates of depression, such as increased leukocytes as an indicator of inflammatory activity and somatic comorbidities [11], were not or only marginally predictive for HRQoL. In congruence with previous research, LVEF did not influence HRQoL when depression was included.
The remarkable association between depression and HRQoL in SHF, which corresponds to previous studies [18, 19], cannot be interpreted as a result of confounding of the measurement tools, i.e., similar contents of the questionnaire items [28]. The fact that HRQoL items other than those reflecting psychosocial burden were sensitive to the effect of depression suggests a need for alternative explanations. Although the causal pathways between depression and HRQoL in chronic diseases such as SHF cannot be determined by a cross-sectional study, several possible associations may be considered. A lower HRQoL may reflect more severe physical and mental limitations. Bodily pain and functional impairment, both characteristics of a chronic disease, may complicate or inhibit positive social activities and relationships, which may lead to the development or aggravation of depression. On the other hand, depression may cause a biased perception and reporting of the actual health status. Depressed patients experience the burden of the disease more profoundly and over-report subjective symptoms, such as fatigue, which may well be a symptom of heart failure, thus yielding worse reports of HRQoL [29]. The enormous influence of the PHQ-depression score on HRQoL may be explained by both of these bidirectional associations, i.e., the loss of reinforcement because of the activity limitations and the negative perception of the quality of life. On a more global methodical level, shared method variance due to common self-report assessment methods of PHQ, KCCQ and SF-36 may contribute to the associations found. Further research is needed to clarify the causal direction of the association between HRQoL and depression as well as the mechanisms by which it is mediated. The reason as to why some patients with SHF develop a depression and others do not also remains unclear. Presumably positive resources, such as social networks, supportive family relationships, religious involvement and positive activities, e.g., hobbies, may be protective factors enhancing the potential for effective coping with the psychosocial burdens of chronic diseases [30, 31]. In contrast to other studies, our results showed a lower number of patients with symptoms of minor depression compared to major depression. We do not have any explanation for this result. It may limit the generalizability of the results.
Apart from depression, socio-demographic variables, such as age, sex, family status, and educational level, somatic risk factors or comorbidities, such as hyperuricemia, CHD and COPD, as well as use of diuretics and NYHA classification accounted for only marginal amounts of HRQoL variance.
Although some studies identified age as a significant predictor of HRQoL [15, 19], the direction of the association between age and HRQoL was inconsistent. In this study, higher age was shown to be associated with lower HRQoL, which can be explained by a higher rate of comorbidities accompanied by impaired physical functioning among older individuals. Gender differences have also been studied previously. In correspondence with other studies, our study showed poorer HRQoL for female than for male patients [32]. Reasons for this gender difference are still unclear, but higher depression rates among women and different symptom perceptions are being discussed as possible explanations [33]. However, in this study, female sex was still associated with lower HRQoL even after adjustment for depression had been made. Moreover, stress and depression are more prevalent in patients with lower socio-economical status [34]. Among demographics, partnership status also emerged as a correlate of HRQoL. The previously reported positive impact of social support on HRQoL [18] may explain the lower HRQoL in patients living without a partner.
Somatic comorbidities are frequent in patients with SHF and create further burdens associated with the disease. This raises the question whether patients with SHF who suffer from additional comorbidities have a low HRQoL because of the associated restrictions (e.g., pain, limited physical functioning) or because of the development of depressive symptoms that decrease HRQoL, or both. Those results that were not controlled for depression (see Tables 3, 4, Model 3) show that patients with additional comorbidities do indeed have a lower HRQoL—especially patients who have comorbidities with clearly noticeable restrictive symptoms (e.g., COPD). From a psychological perspective, limited physical functioning may result in a decrease of positive activities and therefore an increase in depression. This corresponds to the behavioral model of depression postulated by Lewinsohn et al. [35], which states that depression can result from a stressor that disrupts normal behavior patterns, thus causing a loss of positive reinforcement.
After controlling for depression (see Tables 3, 4, Model 4), the effect of additional comorbidities remained virtually unchanged, but depression still played the most important role. This suggests that HRQoL is influenced by both additional comorbidities as well as depression.
The use of diuretics can be regarded as a marker for heart failure severity, which influences the disease-specific aspect of HRQoL (KCCQ scales). Other measures of heart failure severity, such as NYHA and LVEF, only have a marginal or no influence on the predictive ability of HRQoL. Although LVEF is an important factor in determining heart failure severity, it does not seem to play a role in the patients’ subjective evaluation of restrictions due to their disease. While a decrease in HRQoL was seen with increasing severity of SHF, as indicated by NYHA classification, NYHA class independently explained only a small proportion of variance of HRQoL. This finding is in accordance with previous research [19]. The association between depression and physician-reported NYHA functional class may also be considered to be bidirectional. A higher functional class may reflect more severe disease limitations, which may in turn account for the development of depression. Conversely, physicians may classify their depressed patients to be in higher NYHA functional classes because the patients are likely to report more pronounced functional impairments.
Our data also support the finding that SHF is associated both with a severe reduction of generic and disease-specific HRQoL [7], as well as with an increased prevalence of minor or major depression [2].
In contrast to the generic SF-36 component scores, the disease-specific KCCQ summary scores were more widely distributed across the possible ranges of the scales, so that in patients with varying levels of heart failure severity, as measured by NYHA classification, clearly different KCCQ scores were observed. Thus, as compared to the generic SF-36 component scores, the disease-specific KCCQ summary scores were more sensitive for heart failure severity because they showed better differentiation between subgroups according to NYHA classification. Moreover, the KCCQ scales showed effects of socio-demographic variables, such as sex, family status, and educational level, which were not significant within the SF-36 component scores. Consequently, whereas the KCCQ appears to be more sensitive for the impact of the disorder in question, i.e., heart failure, demographic variables may also be risk factors for impaired HRQoL. Taken together, both assessment tools may provide the most complete picture of HRQoL in chronic heart failure patients.
The following limitations should be considered in the interpretation of this study. One limitation is the use of self-reports of depression with resulting diagnoses that were not confirmed by a structured interview. To confirm a diagnosis of depression, a structured interview performed by a professional would be necessary. The employed PHQ-9 has an excellent sensitivity and specificity, particularly regarding major depression, for general medical patients [26]. However, the sensitivity of the PHQ-9 is lower among cardiac patients [36]. In spite of this, it has been recommended by the American Heart Association for the screening of depression and was therefore used in this study [37].
Another limitation is that we examined a sample of hospitalized patients. Some studies have indicated that hospitalization may decrease quality of life. Furthermore, the direction of causality could not be examined due to the cross-sectional study design. To confirm possible causal directions, experimental studies are necessary. Our sample of patients with SHF was also heterogeneous according to NYHA classes. However, our sample represents a typical ‘real world’ sample of patients with SHF.
To conclude, our results indicate that both generic and disease-specific HRQoL are considerably impaired in SHF. Moreover, our results show that depression plays a major role in explaining variance of both types of HRQoL, whereas other variables only have a marginal or no impact. This finding strongly indicates that comorbid depression is relevant for the HRQoL of patients with SHF. From a clinical perspective, we recommend to include the assessment of depression in the routine medical evaluation of patients with SHF to optimize the treatment of patients with comorbid depressive disorders. Our findings indicate that the non-cardiac factor depression is more important than cardiac functioning itself in determining the HRQoL of patients suffering from SHF. Therefore, HRQoL should only be used as a valid measure of health status in patients with SHF if depression is considered as well. Our study outcomes indicate that depression is more important than cardiac functioning in determining the HRQoL of patients suffering from SHF. Furthermore, taking into consideration that depression is not only frequent among patients with SHF but also increases their mortality risk [38] and has a negative impact on compliance with treatment [39], improved diagnosis and treatment of this comorbidity are warranted.
References
Fonarow GC (2008) Epidemiology and risk stratification in acute heart failure. Am Heart J 155:200–207
Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ (2006) Depression in heart failure. A meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol 48:1527–1537
Franke J, Zugck C, Wolter JS, Frankenstein L, Hochadel M, Ehlermann P, Winkler R, Nelles M, Zahn R, Katus HA, Senges J (2012) A decade of developments in chronic heart failure treatment: a comparison of therapy and outcome in a secondary and tertiary hospital setting. Clin Res Cardiol 101:1–10
Iqbal J, Francis L, Reid J, Murray S, Denvir M (2010) Quality of life in patients with chronic heart failure and their carers: a 3-year follow-up study assessing hospitalization and mortality. Eur J Heart Fail 12:901–902
Karapolat H, Demir E, Bozkaya YT, Eyigor S, Nalbantgil S, Durmaz B, Zoghi M (2009) Comparison of hospital-based versus home-based exercise training in patients with heart failure: effects on functional capacity, quality of life, psychological symptoms, and hemodynamic parameters. Clin Res Cardiol 98(10):635–642
Meinertz T, Kirch W, Rosin L, Pittrow D, Willich SN, Kirchhof P, ATRIUM investigators (2011) Management of atrial fibrillation by primary care physicians in Germany: baseline results of the ATRIUM registry. Clin Res Cardiol 100:897–905
Zuluaga MC, Guallar-Castillón P, López-García E, Banegas JR, Conde-Herrera M, Olcoz-Chiva M, Rodríguez-Pascual C, Rodriguez-Artalejo F (2010) Generic and disease-specific quality of life as a predictor of long-term mortality in heart failure. Eur J Heart Fail 12:1372–1378
Calvert MJ, Freemantle N, Cleland JG (2005) The impact of chronic heart failure on health-related quality of life data acquired in the baseline phase of the CARE-HF study. Eur J Heart Fail 7:243–251
Müller-Tasch T, Frankenstein L, Holzapfel N, Schellberg D, Löwe B, Nelles M, Zugck C, Katus H, Rauch B, Haass M, Jünger J, Remppis A, Herzog W (2008) Panic disorder in patients with chronic heart failure. J Psychosom Res 64:299–303
Freedland KE, Rich MW, Skala JA, Carney RM, Dávila-Román VG, Jaffe AS (2003) Prevalence of depression in hospitalized patients with congestive heart failure. Psychosom Med 65:119–128
Angermann CE, Gelbrich G, Störk S, Schowalter M, Deckert J, Ertl G, Faller H, on Behalf of the Competence Network Heart Failure (2011) Somatic correlates of comorbid major depression in patients with systolic heart failure. Int J Card 147:66–73
Faller H, Störk S, Schowalter M, Steinbüchel T, Wollner V, Ertl G, Angermann CE (2007) Depression and survival in chronic heart failure: does gender play a role? Eur J Heart Fail 9:1018–1023
Jiang W, Kuchibhatla M, Clary GL, Cuffe MS, Christopher EJ, Alexander JD, Califf RM, Krishnan RR, O’Connor CM (2007) Relationship between depressive symptoms and long-term mortality in patients with heart failure. Am Heart J 154:102–108
Bennet SJ, Oldridge NB, Eckert GJ, Embree JL, Browning S, Hou N, Deer M, Murray MD (2002) Discriminant properties of commonly used quality of life measures in heart failure. Qual Life Res 11:349–359
Masoudi FA, Rumsfeld JS, Havranek EP, House JA, Peterson ED, Krumholz HM, Spertus JA, Cardiovascular Outcomes Research Consortium (2004) Age, functional capacity, and health-related quality of life in patients with heart failure. J Card Fail 10:368–373
Smith RF, Johnson G, Ziesche S, Bhat G, Blankenship K, Cohn JN (1993) Functional capacity in heart failure. Comparison of methods for assessment and their relation to other indexes of heart failure. The V-HeFT VA Cooperative Studies Group. Circulation 87(6 Suppl):VI88–VI93
Rector TS, Johnson G, Dunkman WB, Daniels G, Farrell L, Henrick A, Smith B, Cohn JN (1993) Evaluation by patients with heart failure of the effects of enalapril compared with hydralazine plus isosorbide dinitrate on quality of life. V-HeFT II. The V-HeFT VA Cooperative Studies Group. Circulation 87(6 Suppl):VI71–VI77
Mendes CF, Grady KL, Eaton C, Rucker-Whitacker C, Janssen I, Calvin J, Powell LH (2009) Quality of life in a diverse population of heart failure patients. Baseline findings from the Heart Failure Adherence and Retention Trial (Hart). J Cardiopulm Rehabil Prev 29:171–178
Müller-Tasch T, Peters-Klimm F, Schellberg D, Holzapfel N, Barth A, Jünger J, Szecsenyi J, Herzog W (2007) Depression is a major determinant of quality of life in patients with chronic systolic heart failure in general practice. J Card Fail 13:818–8124
Ware JE (1996) The SF-36 Health Survey. In: Spilker B (ed) Quality of life and pharmacoeconomics in clinical trials. Raven, Philadelphia, pp 337–346
Bullinger M, Morfeld M, Kohlmann T, Nantke J, van den Bussche H, Dodt B, Dunkelberg S, Kirchberger I, Krüger-Bödecker A, Lachmann A, Lang K, Mathis C, Mittag O, Peters A, Raspe HH, Schulz H (2003) SF-36 Health Survey in Rehabilitation Research. Findings from the North German Network for Rehabilitation Research, NVRF, within the rehabilitation research funding program. Rehabilitation 42:218–225
Green PC, Porter CB, Bresnahan DR, Spertus JA (2000) Development and evaluation of the Kansas City Cardiomyopathy Questionnaire: a new health status measure for heart failure. J Am Coll Cardiol 55:1245–1255
Faller H, Steinbüchel S, Schowalter M, Störk S, Angermann C (2005) The Kansas City Cardiomyopathy Questionnaire (KCCQ)—a new disease-specific quality of life measure for patients with chronic heart failure. Psychother Psych Med 55:200–208
Kroenke K, Spitzer RL, Williams JBW (2001) The PHQ-9. Validity of a brief depression severity measure. J Gen Intern Med 16:606–613
Löwe B, Gräfe K, Zipfel S, Witte S, Loerch B, Herzog W (2004) Diagnosing ICD-10 depressive episodes: superior criterion validity of the Patient Health Questionnaire. Psychother Psychosom 73:386–390
Löwe B, Spitzer RL, Gräfe K, Kroenke K, Quenter A, Zipfel S, Buchholz C, Witte S, Herzog W (2004) Comparative validity of three screening questionnaires for DSM-IV depressive disorders and physicians′ diagnoses. J Affect Disord 87:131–140
Angermann CE, Störk S, Gelbrich G, Faller H, Jahns R, Frantz S, Loeffler M, Ertl G (2011) Mode of action and effects of standardized collaborative disease management on mortality and morbidity in patients with systolic heart failure: The Interdisciplinary Network for Heart Failure (INH) study. Circ Heart Fail 5(1):25–35. doi:10.1161/CIRCHEARTFAILURE.111.962969
Callahan CM, Kroenke K, Counsell SR, Hendrie HC, Perkins AJ, Katon W et al (2005) Treatment of depression improves physical functioning in older adults. J Am Geriatr Soc 53:367–373
Sullivan MD, LaCroix AZ, Russo JE, Walker EA (2001) Depression and self-reported physical health in patients with coronary disease: mediating and moderating factors. Psychosom Med 63:248–256
Bean MK, Gibson D, Flattery M, Duncan A, Hess M (2009) Psychosocial factors, quality of life, and psychological distress: ethnic differences in patients with heart failure. Prog Cardiovasc Nurs 24:131–140
Koenig HG (2007) Religion and depression in older medical inpatients. Am J Geriatr Psychiatry 15:282–291
Luttik ML, Lesman-Leegte I, Jaarsma T (2009) Quality of life and depressive symptoms in heart failure patients and their partners: the impact of role and gender. J Card Fail 15:580–585
Stromberg A, Martenson J (2003) Gender differences in patients with heart failure. Eur J Cardiocasc Nurs 2:7–18
Akhtar-Danesh N, Landeen J (2007) Relation between depression and socio-demographic factors. Int J Ment Health Syst 4:4
Lewinsohn PM, Youngren MA, Grosscup SJ (1979) Reinforcement and depression. In: Dupue RA (ed) The psychobiology of depressive disorders: implications for the effects of stress). Academic Press, New York, pp 291–316
McManus D, Pipkin SS, Whooley MA (2005) Screening for depression in patients with coronary heart disease (data from the heart and soul study). Am J Cardiol 96(8):1076–1081
Lichtman JH, Bigger JT Jr, Blumenthal JA et al (2008) Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research. Circulation 118:1768–1775
Faris R, Purcell H, Henein MY, Coats AJS (2002) Clinical depression is common and significantly associated with reduced survival in patients with non-ischaemic heart failure. Eur J Heart Fail 4:541–551
Joynt KE, Whellan DJ, O’connor CM (2004) Why is depression bad for the failing heart? A review of the mechanistic relationship between depression and heart failure. J Card Fail 10:258–271
Acknowledgments
The authors of this manuscript have certified that they comply with the Principles of Ethical Publishing in the International Journal of Cardiology. We are indebted to the patients who participated in the study. Further, we thank the heart failure specialist nurses S. Muck, M. Kirsch, E. Pfänder and E. Schupfner for support of patient acquisition and study logistics. We also thank Dr. C. Prettin and M. Hanke for excellent data and query management Funded by the German Ministry of Education and Research (BMBF, Berlin, project number 01GL0304) and by the German Competence Network Heart Failure (Berlin, BMBF project number 01GI0205).
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schowalter, M., Gelbrich, G., Störk, S. et al. Generic and disease-specific health-related quality of life in patients with chronic systolic heart failure: impact of depression. Clin Res Cardiol 102, 269–278 (2013). https://doi.org/10.1007/s00392-012-0531-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-012-0531-4