Abstract
Background
Asymmetric dimethylarginine (ADMA) is an endogenous nitric oxide synthase inhibitor, which has been associated with total and cardiovascular mortality in various clinical settings. Studies on its structural isomer, symmetric dimethylarginine (SDMA), are scarce. This study aimed to determine the associations of both ADMA and SDMA levels with secondary cardiovascular disease events and all-cause mortality in patients with stable coronary heart disease (CHD).
Methods
In the observational prospective cohort study KAROLA, 1,148 CHD patients were followed for a median of 8.1 years. ADMA and SDMA were determined by liquid chromatography–tandem mass spectrometry. Baseline ADMA and SDMA levels were categorized in quartiles or standardized by their respective standard deviation, and appropriate hazard ratios and 95 % confidence intervals (HR [95 % CI]) were estimated in Cox proportional hazards models.
Results
150 patients experienced secondary cardiovascular disease events (CVD) and 121 patients died. After adjustment for confounders, ADMA was not associated with the risk of secondary CVD events (HR per standard deviation increase: 1.02 [95 %CI: 0.86–1.21]), whereas an association was suggested for SDMA (HR 1.17 [1.00–1.37]). Higher hazard ratios were observed in all-cause mortality models (ADMA: HR 1.15 [0.95–1.37]; SDMA: HR 1.29 [1.09–1.52]).
Conclusions
Our results suggest that especially SDMA might possibly have potential as a risk marker for all-cause mortality and to a lesser extent for secondary cardiovascular events. Future studies are needed to quantify these associations more precisely and should, in particular, further address the possibility of residual confounding by impaired kidney function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Posttranslational methylation of l-arginine residues is an almost ubiquitous process mediated by a family of protein arginine N-methyltransferases. During endogenous protein turnover, asymmetrically and symmetrically methylated l-arginine residues are released as asymmetric dimethylarginine (ADMA) and its structural isomer, symmetric dimethylarginine (SDMA) [1]. ADMA and SDMA can be cleared by the kidney directly or by enzymatic degradation [2]. However, elimination of SDMA is dominated by renal clearance, whereas ADMA is predominantly metabolized by dimethylarginine dimethylaminohydrolases [3].
ADMA and SDMA are structurally related to l-arginine, which is a key substrate of numerous metabolic and signaling pathways [4, 5]. Among other effects, ADMA can impair l-arginine-dependent nitric oxide synthases (NOS) which produce the key signaling molecule nitric oxide (NO) [6]. ADMA has been shown to be associated with several cardiovascular risk factors and markers of vascular disease such as endothelial dysfunction, decreased cerebral blood flow, and intima-media thickness [7–11]. ADMA has also been associated with cardiovascular disease and mortality in the general population, as well as in several clinical populations, including patients with coronary artery disease and chronic kidney disease [12–15]. Besides being a marker of kidney function, SDMA is thought to inhibit both cellular and renal uptake of l-arginine, thus also potentially creating a decrease in NO availability [16–18].
The association of ADMA with all-cause mortality has consistently been described in various clinical settings. In contrast, data on SDMA is less homogeneous and only few pertinent studies have been published so far; Zoccali et al. [15]. and Aucella et al. [19] found no association between SDMA and mortality in patients with terminal renal disease, whereas SDMA was a risk factor for cardiovascular morbidity and all-cause mortality in patients with a history of stroke[20] or subjects undergoing coronary angiography [21]. Another study in an angiography referral population found associations of both ADMA and SDMA with mortality, but suggested that further research was needed in particular with respect to the dose–response relationships [22].
Patients who suffer from stable coronary heart disease (CHD) have a high risk of secondary cardiovascular events, both fatal and non-fatal [23]. Knowledge of the risks associated with ADMA and SDMA, and of the specific underlying pathophysiologic mechanisms, could improve risk stratification and aid in the development of new treatments. Therefore, the present study aimed to determine the association and detailed dose–response relationships of both ADMA and SDMA levels with secondary cardiovascular events (non-fatal myocardial infarction and stroke, or cardiovascular disease as the main cause of death) and all-cause mortality in patients with stable CHD.
Methods
Study population
The KAROLA study (‘Langzeitfolge der KARdiOLogischen Anschlussheilbehandlung’) was set up to investigate the long-term effects of in-hospital rehabilitation for patients with stable coronary heart disease. In Germany, patients suffering from myocardial infarction/acute coronary syndrome, or undergoing cardiac surgery due to coronary heart disease, are entitled to such a specialized rehabilitation program by law. Details about study design, inclusion criteria and data collection have previously been described [24, 25]. In brief, patients were recruited to two specialized rehabilitation centers between January 1999 and May 2000. Patients admitted to the rehabilitation program within 3 months after the diagnosis of coronary heart disease (ICD-9 code 410–414) or administration of cardiac surgery were eligible to participate in this study.
The study was in accordance with the Declaration of Helsinki and approved by the ethics boards of the Universities of Ulm and Heidelberg as well as the physicians’ chambers of Baden-Württemberg and Hessen. All participants gave written informed consent.
Data collection
Patients filled in a standardized questionnaire both at the start and end of the rehabilitation program which covered topics such as medical history and socio-demographic factors. Additional information was obtained from hospital records.
A follow-up questionnaire was mailed 1, 3, 4.5, 6 and 8 years after the rehabilitation discharge to the patients and a separate one to their primary care physicians. Death certificates including the main cause of death were obtained from local public health authorities. The primary end point was defined as secondary cardiovascular disease (CVD) events (non-fatal myocardial infarction, non-fatal stroke or cardiovascular disease as the main cause of death [ICD-9 pos. 390–459, ICD-10 pos. I00–I99 and R57.0]).
Laboratory methods
Baseline blood samples were drawn at discharge in the participating rehabilitation centers according to a standardized sampling scheme in a fasting state and stored at −80 °C until ADMA/SDMA measurements. Other laboratory variables such as blood lipids, C-reactive protein and creatinine were determined as previously described [25].
ADMA, SDMA and l-arginine were measured by means of liquid chromatography–tandem mass spectrometry as previously validated and described in detail [26, 27]. All laboratory measurements were done in a blinded fashion.
Statistical methods
The study population was first described according to socio-demographic factors, cardiovascular risk factors, and ADMA, SDMA and l-arginine levels, which were available for 1,148 patients. In further analyses, ADMA and SDMA levels were divided into quartiles, balancing potential non-linearity of associations against category sizes. We also explored the ratios of l-arginine to ADMA and SDMA as exposures, as ratios might physiologically be more relevant than the amount of l-arginine per se.
Kaplan–Meier plots were used to show the survival during follow-up by quartiles of ADMA and SDMA. Differences across strata were assessed by log-rank test. Multivariate analyses of the relationship between ADMA and SDMA quartiles and the outcomes were performed by Cox proportional hazards regression estimating hazard ratios and corresponding 95 % confidence intervals (HR [95 % CI]). Log–log survival plots suggested no relevant violation of the proportional hazards assumption (not shown). In addition to unadjusted crude models, two models were fitted to address confounding by adjusting for potential confounding variables based on subject matter knowledge. The first model included age at baseline and sex. The second model additionally included body mass index (BMI), total cholesterol/high density lipoprotein cholesterol ratio, diastolic and systolic blood pressures, glomerular filtration rate estimated by the creatinine-based CKD-EPI formula (eGFR) [28], smoking status (current/former/never), history of myocardial infarction, history of diabetes mellitus, CRP levels (log10-transformed), and discharge prescription of diuretics or angiotensin-converting enzyme inhibitors. Twenty-six subjects with missing covariable values were excluded from the fully adjusted models. This fully adjusted model was also used in cubic spline analyses, which modeled the risk associated with the dimethylarginines on a continuous scale allowing for non-linearity of the dose–response relationship. The three quartile cutoffs were used as ‘knots’ of the spline functions in these models [29].
We further explored the associations in secondary analyses by including ADMA and SDMA together in the fully adjusted model to investigate their joint relationship with prognosis. Events were furthermore split into fatal cardiovascular events, fatal non-cardiovascular events and non-fatal cardiovascular events to further disentangle the associations between ADMA, SDMA and our end points. Finally, we explored the stability of our results when replacing the more commonly used creatinine-based eGFR by the cystatin C-based Arnal-Dade estimator of kidney function, which remains less established yet appears to be less influenced by body composition (eGFRcyst = 74.835/[cystatin C in mg/l]4/3) [30, 31].
Exact confidence intervals for event rates were obtained using the epitools package of R (version 2.10.0, R Foundation for Statistical Computing). All other analyses were performed with SAS (version 9.1.3, SAS-institute Inc.).
Results
The baseline characteristics of the study population of n = 1,148 subjects are displayed in Table 1. The average age was 59 years and patients were predominantly male. A substantial proportion (16 %) was obese. The cohort included many former smokers, with only 5 % reporting persistent smoking at baseline. Six hundred and eighty-one patients (59 %) had a history of myocardial infarction. The median (interquartile range) creatinine-based eGFR was 89.9 (76.0–98.2) ml/min/1.73 m2. The mean plasma concentration was 0.57 μmol/l for ADMA and 0.53 μmol/l for SDMA. ADMA and SDMA levels were correlated with a Pearson coefficient of 0.46 (p < 0.0001).
Complete follow-up including the reporting of non-fatal secondary cardiovascular events by the primary care physician was available for 1,054 (92 %) of the participants (94 [8 %] subjects with this information missing were excluded from this analysis). Over a median follow-up of 8.1 years, 150 (14 % of 1,054) secondary CVD events were observed during a total of 7,133 person-years (incidence rate [95 % confidence interval]: 21.0 [17.8–24.7] per 1,000 py). For the all-cause mortality analyses, outcome information was available for all subjects, and the 1,148 participants yielded a total of 8,971 person-years, during which 121 (11 %) subjects died (incidence rate: 13.5 [11.2–16.1] per 1,000 py). Of the 150 secondary CVD events, 59 were fatal, whereas 91 patients experienced a non-fatal event (6 of these subsequently died of cardiovascular disease). Of the 121 deaths, 56 (46 %) were not due to cardiovascular disease as a major cause.
Cardiovascular disease events
As displayed in Table 2, a one standard deviation (SD) increase of ADMA levels was associated with a 14 % higher risk of secondary cardiovascular events in crude analyses (hazard ratio [95 % confidence interval] of HR = 1.14 [0.97–1.33]). When adjusted for potential confounders, no increase in risk was observed (HR = 1.02 [0.86–1.21]). A similar pattern was observed for the quartile analyses: high levels of ADMA (4th quartile [Q4] vs. 1st quartile [Q1]) were associated with elevated risk in the crude model, but this was markedly reduced in the fully adjusted model (HR = 1.14 [0.70–1.87]).
As also shown in Table 2, a 1 SD increase of SDMA was associated with a 32 % higher risk of a secondary CVD event (HR = 1.32 [1.18–1.46]). The reduction of the estimate in the fully adjusted model (HR = 1.17 [1.00–1.37]) compared to the crude model was less pronounced than for ADMA. In crude analyses, patients in the fourth quartile had an 86 % higher risk of developing a secondary CVD event compared to patients in the first quartile. When adjusted for confounders, the effect estimate was reduced to HR = 1.31 [0.79–2.20].
When ADMA and SDMA were jointly included in the fully adjusted model, again no effect was observed for ADMA (+1 SD: HR = 0.93 [0.77–1.12]), but an increased risk still appeared for higher SDMA levels (+1 SD: HR = 1.21 [1.01–1.44]).
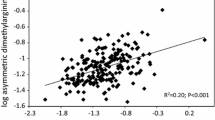
The results described above altogether resembled those of Kaplan–Meier analyses, in which patients with the highest levels of SDMA had the largest number of cardiovascular events (Fig. 1b). The spline estimate likewise suggested a somewhat higher risk with higher SDMA (Fig. 2b). In contrast, neither analysis revealed such an association for ADMA (Figs. 1a and 2a).
Restricted cubic spline estimates of the dose–response relationships between ADMA or SDMA and secondary cardiovascular events or all-cause mortality hazard ratios (HR) are confounder adjusted and given in reference to median marker concentrations (HR in red; 95 % confidence interval in black; red dots mark the quartile knots)
All-cause mortality
The risk of death during follow-up was increased with higher levels of ADMA (+1 SD: HR = 1.32 [1.12–1.55]; Table 3). Adjustment for confounders attenuated this association (HR = 1.15 [0.95–1.37]). Higher levels of ADMA were also associated with increased risk in the crude quartile analysis (Q4 vs. Q1: HR = 2.43 [1.42–4.17]), but this risk was also reduced after adjustment for potential confounders (HR = 1.52 [0.86–2.68]).
As also shown in Table 3, a 1 SD increase in SDMA was also associated with an increased risk of mortality (HR = 1.42 [1.27–1.58]), but in comparison to ADMA, adjustment for potential confounders attenuated this estimate slightly less (HR = 1.29 [1.09–1.52]). The Q4 versus Q1 hazard ratio was similarly affected (crude: HR = 2.46 [1.46–4.16]; fully adjusted: HR = 1.62 [0.91–2.89]).
When ADMA and SDMA were jointly included in the fully adjusted model, the association with ADMA disappeared (+1 SD: HR = 1.01 [0.82–1.24]), whereas the association with SDMA remained comparable (+1 SD: HR = 1.28 [1.06–1.55]).
The Kaplan–Meier and spline analyses were in accordance with these results: survival differed across quartiles of SDMA (Fig. 1d; P log-rank = 0.0012) and SDMA levels appeared to be log-linearly related to mortality (Fig. 2d). The differences in survival by ADMA quartiles were somewhat less pronounced (Fig. 1c; P log-rank = 0.0085). The spline results were suggestive of a decreased risk of mortality in subjects with the lowest levels of ADMA, and the dose–response curve leveled off around the median (Fig. 2c).
Fatal secondary CVD, non-fatal secondary CVD and non-CVD mortality
Table 4 displays the fully adjusted associations between ADMA or SDMA and fatal secondary CVD events, non-fatal secondary CVD events and non-CVD mortality. Higher levels of ADMA or SDMA were associated with fatal CVD, but neither with non-fatal CVD nor non-CVD mortality. When ADMA and SDMA were jointly included in the model for fatal CVD, the association with ADMA levels almost disappeared (+1 SD: HR = 1.07 [0.82–1.40]), whereas the hazard ratio for SDMA remained stable (+1 SD: HR = 1.40 [1.11–1.76]).
Sensitivity to varying adjustments for kidney function
The comparison of hazard ratios obtained in the fully adjusted models to similar models not adjusting for creatinine clearance did not suggest excessive confounding of our main results by kidney function (data not shown). However, especially the SDMA estimates were rather sensitive to adjustment for cystatin C-based instead of creatinine-based eGFR. More specifically, the hazard ratios were attenuated to 1.07 [0.91–1.26] per 1 SD increase (Q4 vs. Q1: HR = 1.05 [0.61–1.78]) for secondary CVD events, to 1.18 [1.00–1.39] per 1 SD increase (Q4 vs. Q1: HR = 1.35 [0.74–2.47]) for all-cause mortality, and to 1.18 [0.96–1.45] per 1 SD increase (Q4 vs. Q1: HR = 1.27 [0.53–3.01]) for fatal secondary CVD events.
Absolute and relative levels of l-arginine
Absolute levels of l-arginine were not associated with secondary cardiovascular events (+1 SD: HR = 1.03 [0.87–1.21]; Q4 vs. Q1: HR = 1.21 [0.75–1.94]) or mortality (+1 SD: HR = 1.15 [0.97–1.38]; Q4 vs. Q1: HR = 1.25 [0.76–2.07]) in our fully adjusted models (not shown). Likewise, l-arginine levels relative to ADMA (l-arginine/ADMA ratio) were associated with neither outcome (+1 SD: HR = 1.00 [0.85–1.18] for secondary events, HR = 1.00 [0.83–1.21] for all-cause mortality). When instead taken relative to SDMA (l-arginine/SDMA ratio), there also was no significant association (+1 SD: HR = 0.97 [0.80–1.17] for secondary events, HR = 1.00 [0.82–1.23] for all-cause mortality).
Discussion
The findings of this study suggest that SDMA might possibly constitute an independent risk factor for all-cause mortality in patients with stable coronary heart disease, as independent associations remained after covariable adjustment; the associations found for ADMA were less pronounced. Associations with secondary cardiovascular disease events (fatal and non-fatal) were weaker (SDMA) or even absent (ADMA). The dose–response analyses showed similar patterns and suggested that the association of ADMA with all-cause mortality might be non-linear, which could explain why the associations in corresponding quartile models were relatively modest.
Pathophysiological mechanisms of ADMA and SDMA
Adverse outcomes associated with ADMA are frequently attributed to inhibition of NO production, as ADMA is a competitive inhibitor of the NO-synthesizing enzymes (NOS). For SDMA, the link to NO synthesis is less evident, although it has been shown that SDMA can reduce cellular uptake of l-arginine, the key substrate for NO synthesis [16]. Therefore, if NO is the main mechanism through which ADMA and SDMA are associated with CVD morbidity and mortality, absolute and relative levels of l-arginine levels should also be associated with CVD morbidity and mortality. However, our results showed no clear associations for l-arginine levels with either outcome. Also, when assuming competitive inhibition of l-arginine-dependent signaling as a main pathophysiologic mechanism, one would also expect the ratios of l-arginine to SDMA or ADMA to be associated with cardiovascular disease. This likewise was not the case in our study, which suggests that the mechanisms through which dimethylarginines are associated with the risk of CVD mortality might be independent of l-arginine levels. This interpretation would be in concordance with observations that l-arginine administration, although beneficial with respect to intermediate cardiovascular outcomes, seems not to improve clinical prognosis after acute myocardial infarction [32]. One explanation generally could be that NOS rather than l-arginine availability is the rate-limiting factor in NO production. However, in our study, SDMA showed stronger associations with outcomes than ADMA, although SDMA does not directly inhibit NOS. Alternative mechanisms therefore should be considered.
Further complexities in the marker—outcome associations
High levels of both ADMA and SDMA were strong risk factors for fatal, but not for non-fatal, cardiovascular events, which actually is in line with recent data from the Framingham Heart Study Offspring Cohort [12]. This raises the somewhat counter-intuitive possibility that fatal and non-fatal cardiovascular events have different etiologies, but one certainly should be cautious not to over-interpret these sub-analyses with rather small numbers of events. Interestingly, recently published analyses in the LURIC cohort of patients referred for coronary angiography produced very similar adjusted estimates, especially for all-cause mortality in the fourth versus first quartile of ADMA or SDMA [22]. For SDMA, a J-shaped association with mortality was suggested in that study, which we could not confirm. Estimates referring to continuous marker variables were not reported. It is important to note that the LURIC study design on one hand allowed the inclusion of subjects without significant coronary artery disease; on the other hand, it assessed ADMA and SDMA at the time of coronary angiography for indications including “chest pain and/or noninvasive test results consistent with myocardial ischemia” [22]. It appears quite possible that such differences in participant characteristics and measurement timing could be responsible, e.g., for the discrepant results regarding SDMA and mortality.
The role of kidney function in the relationship between dimethylarginines and cardiovascular morbidity and mortality is complex, as impaired renal function may lead to the accumulation of SDMA and to a smaller extent of ADMA. The resulting higher dimethylarginine levels could then possibly increase cardiovascular risk, but so does certainly the impaired kidney function per se. Our main models thus were adjusted for the creatinine-based eGFR, although the impact of this adjustment was limited. Interestingly, the associations especially for SDMA were clearly attenuated when we instead used a cystatin C-based eGFR, which more recently has been suggested as a potentially superior estimator of kidney function [31, 33]. Taken together, we cannot rule out that residual confounding due to imperfect adjustment for kidney function—which is not fully avoidable due to the imprecision of any estimate of kidney function—was partially responsible for the remaining observed associations of SDMA with outcome events.
Limitations
While mortality follow-up was available for all patients, data on non-fatal secondary cardiovascular events were based on the reports of the primary care physicians and incomplete for a few participants, leading to a reduced sample size in the analyses pertaining to non-fatal cardiovascular events. We believe though that the refusal of the physicians or the inability to reach them was independent of ADMA or SDMA levels or the outcome of the patient and that this will not affect the conclusions of our study except for a reduction in statistical power. Reassuringly, there were no major differences in baseline characteristics including dimethylarginines between the participants with complete versus incomplete follow-up, the most notable ones being that subjects with incomplete follow-up were on average 2.5 years younger and had a CKD-EPI eGFR 5.3 ml/min/1.73 m2 higher. Since the participants of this study volunteered to participate, some selection bias might have occurred potentially affecting generalizability, whereas internal validity is not likely to be affected. Finally, observational studies usually have limited capacity to draw final conclusions on the causality of the associations observed. A clinical trial with specific ADMA and SDMA plasma concentration-lowering drugs could help to address causal inference, but such drugs are not available so far. Studies with genetically altered animals could also help: a recent published study on genetically modified animals with lower ADMA plasma and tissue levels indicates, for example, that a reduction of ADMA may indeed improve clinical outcome [34]. It should be noted that our results cannot be generalized to healthy populations. Furthermore, the patterns of association might crucially depend on the timing of the marker measurements in relation to the initial cardiovascular event leading to study inclusion. Future studies could address these issues by including repeat ADMA/SDMA assessments, ideally obtaining baseline measurements already well before the onset of underlying cardiovascular disease. Such studies preferably would also be based on a larger number of outcome events in order to achieve higher statistical power. Whereas the imprecision of our results was addressed by including confidence intervals around our estimates throughout the present work, it might well be that limited robustness is responsible for inconsistencies in this and previous reports.
Conclusions
The current findings seem to suggest that SDMA and to a lesser extent ADMA might be associated with all-cause and cardiovascular mortality. Our data indicate that it is unclear whether reduced NO bioavalability is the causal mechanism through which they act. Furthermore, the role of reduced kidney function in the relation between both ADMA and SDMA and the different cardiovascular outcomes needs to be further clarified.
References
Boger RH, Zoccali C (2003) ADMA: a novel risk factor that explains excess cardiovascular event rate in patients with end-stage renal disease. Atheroscler Suppl 4:23–28
Ogawa T, Kimoto M, Sasaoka K (1987) Occurrence of a new enzyme catalyzing the direct conversion of NG, NG-dimethyl-l-arginine to l-citrulline in rats. Biochem Biophys Res Commun 148:671–677
Vallance P, Leone A, Calver A, Collier J, Moncada S (1992) Accumulation of an endogenous inhibitor of nitric oxide synthesis in chronic renal failure. Lancet 339:572–575
Boger RH (2007) The pharmacodynamics of l-arginine. J Nutr 137:1650S–1655S
Morris SM Jr (2007) Arginine metabolism: boundaries of our knowledge. J Nutr 137:1602S–1609S
Vallance P, Leone A, Calver A, Collier J, Moncada S (1992) Endogenous dimethylarginine as an inhibitor of nitric oxide synthesis. J Cardiovasc Pharmacol 20(Suppl 12):S60–S62
Boger RH, Bode-Boger SM, Szuba A, Tsao PS, Chan JR, Tangphao O et al (1998) Asymmetric dimethylarginine (ADMA): a novel risk factor for endothelial dysfunction: its role in hypercholesterolemia. Circulation 98:1842–1847
Boger RH, Maas R, Schulze F, Schwedhelm E (2005) Elevated levels of asymmetric dimethylarginine (ADMA) as a marker of cardiovascular disease and mortality. Clin Chem Lab Med 43:1124–1129
Kielstein JT, Donnerstag F, Gasper S, Menne J, Kielstein A, Martens-Lobenhoffer J et al (2006) ADMA increases arterial stiffness and decreases cerebral blood flow in humans. Stroke 37:2024–2029
Maas R, Xanthakis V, Polak JF, Schwedhelm E, Sullivan LM, Benndorf R et al (2009) Association of the endogenous nitric oxide synthase inhibitor ADMA with carotid artery intimal media thickness in the Framingham Heart Study offspring cohort. Stroke 40:2715–2719
Zoccali C, Benedetto FA, Maas R, Mallamaci F, Tripepi G, Malatino LS et al (2002) Asymmetric dimethylarginine, C-reactive protein, and carotid intima-media thickness in end-stage renal disease. J Am Soc Nephrol 13:490–496
Boger RH, Sullivan LM, Schwedhelm E, Wang TJ, Maas R, Benjamin EJ et al (2009) Plasma asymmetric dimethylarginine and incidence of cardiovascular disease and death in the community. Circulation 119:1592–1600
Schnabel R, Blankenberg S, Lubos E, Lackner KJ, Rupprecht HJ, Espinola-Klein C et al (2005) Asymmetric dimethylarginine and the risk of cardiovascular events and death in patients with coronary artery disease: results from the AtheroGene Study. Circ Res 97:e53–e59
Schulze F, Lenzen H, Hanefeld C, Bartling A, Osterziel KJ, Goudeva L et al (2006) Asymmetric dimethylarginine is an independent risk factor for coronary heart disease: results from the multicenter Coronary Artery Risk Determination investigating the Influence of ADMA Concentration (CARDIAC) study. Am Heart J 152:493e1–493e8
Zoccali C, Bode-Boger S, Mallamaci F, Benedetto F, Tripepi G, Malatino L et al (2001) Plasma concentration of asymmetrical dimethylarginine and mortality in patients with end-stage renal disease: a prospective study. Lancet 358:2113–2117
Bode-Boger SM, Scalera F, Kielstein JT, Martens-Lobenhoffer J, Breithardt G, Fobker M et al (2006) Symmetrical dimethylarginine: a new combined parameter for renal function and extent of coronary artery disease. J Am Soc Nephrol 17:1128–1134
Closs EI, Basha FZ, Habermeier A, Forstermann U (1997) Interference of l-arginine analogues with l-arginine transport mediated by the y+ carrier hCAT-2B. Nitric Oxide 1:65–73
Kielstein JT, Fliser D, Veldink H (2009) Asymmetric dimethylarginine and symmetric dimethylarginine: axis of evil or useful alliance? Semin Dial 22:346–350
Aucella F, Maas R, Vigilante M, Tripepi G, Schwedhelm E, Margaglione M et al (2009) Methylarginines and mortality in patients with end stage renal disease: a prospective cohort study. Atherosclerosis 207:541–545
Schulze F, Carter AM, Schwedhelm E, Ajjan R, Maas R, von Holten RA et al (2010) Symmetric dimethylarginine predicts all-cause mortality following ischemic stroke. Atherosclerosis 208:518–523
Wang Z, Tang WH, Cho L, Brennan DM, Hazen SL (2009) Targeted metabolomic evaluation of arginine methylation and cardiovascular risks: potential mechanisms beyond nitric oxide synthase inhibition. Arterioscler Thromb Vasc Biol 29:1383–1391
Meinitzer A, Kielstein JT, Pilz S, Drechsler C, Ritz E, Boehm BO et al (2011) Symmetrical and asymmetrical dimethylarginine as predictors for mortality in patients referred for coronary angiography: the Ludwigshafen Risk and Cardiovascular Health study. Clin Chem 57:112–121
Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G et al (2010) Executive summary: heart disease and stroke statistics–2010 update: a report from the American Heart Association. Circulation 121:948–954
Koenig W, Twardella D, Brenner H, Rothenbacher D (2006) Lipoprotein-associated phospholipase A2 predicts future cardiovascular events in patients with coronary heart disease independently of traditional risk factors, markers of inflammation, renal function, and hemodynamic stress. Arterioscler Thromb Vasc Biol 26:1586–1593
Rothenbacher D, Koenig W, Brenner H (2006) Comparison of N-terminal pro-B-natriuretic peptide, C-reactive protein, and creatinine clearance for prognosis in patients with known coronary heart disease. Arch Intern Med 166:2455–2460
Schwedhelm E, Maas R, Tan-Andresen J, Schulze F, Riederer U, Boger RH (2007) High-throughput liquid chromatographic–tandem mass spectrometric determination of arginine and dimethylated arginine derivatives in human and mouse plasma. J Chromatogr B Analyt Technol Biomed Life Sci 851:211–219
Schwedhelm E, Tan-Andresen J, Maas R, Riederer U, Schulze F, Boger RH (2005) Liquid chromatography–tandem mass spectrometry method for the analysis of asymmetric dimethylarginine in human plasma. Clin Chem 51:1268–1271
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Desquilbet L, Mariotti F (2010) Dose–response analyses using restricted cubic spline functions in public health research. Stat Med 29:1037–1057
Beauvieux MC, Le Moigne F, Lasseur C, Raffaitin C, Perlemoine C, Barthe N et al (2007) New predictive equations improve monitoring of kidney function in patients with diabetes. Diabetes Care 30:1988–1994
Soares AA, Eyff TF, Campani RB, Ritter L, Camargo JL, Silveiro SP (2009) Glomerular filtration rate measurement and prediction equations. Clin Chem Lab Med 47:1023–1032
Sun T, Zhou WB, Luo XP, Tang YL, Shi HM (2009) Oral l-arginine supplementation in acute myocardial infarction therapy: a meta-analysis of randomized controlled trials. Clin Cardiol 32:649–652
Zhang QL, Brenner H, Koenig W, Rothenbacher D (2010) Prognostic value of chronic kidney disease in patients with coronary heart disease: role of estimating equations. Atherosclerosis 211:342–347
Jacobi J, Maas R, Cardounel AJ, Arend M, Pope AJ, Cordasic N et al (2010) Dimethylarginine dimethylaminohydrolase overexpression ameliorates atherosclerosis in apolipoprotein E-deficient mice by lowering asymmetric dimethylarginine. Am J Pathol 176:2559–2570
Acknowledgments
The authors wish to thank the participating patients and doctors. Our special thanks go out to Claudia El Idrissi-Lamghari, Data Manager of the KAROLA study, Mariola Kastner and Anna Steenpaß for the technical assistance with the ADMA measurements and Prof. Dr. F. M. Helmerhorst for the sparkling discussions on the subject. Funding: The work reflected in this article was in part funded by the German Ministry of Education and Research (Grant 01GD9820/0), the Association of German Pension Fund Agencies (Grant 02708), Willy-Robert-Pitzer Foundation, the Leducq Foundation, Paris, France for the development of Transatlantic Networks of Excellence in Cardiovascular Research (grant 04 CVD 02) and the Erasmus Life Learning Programme.
Conflict of interest
Renke Maas, Edzard Schwedhelm, and Rainer Böger are co-inventors of a method to determine methylarginines. All other authors have no conflicts to report.
Author information
Authors and Affiliations
Corresponding author
Additional information
Bob Siegerink and Renke Maas contributed equally to this manuscript.
Rights and permissions
About this article
Cite this article
Siegerink, B., Maas, R., Vossen, C.Y. et al. Asymmetric and symmetric dimethylarginine and risk of secondary cardiovascular disease events and mortality in patients with stable coronary heart disease: the KAROLA follow-up study. Clin Res Cardiol 102, 193–202 (2013). https://doi.org/10.1007/s00392-012-0515-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-012-0515-4