Abstract
Background
The patients’ misinterpretation of symptoms of an evolving acute myocardial infarction (AMI) is a major cause for prolonged pre-hospital delays. The objective of this study was to identify factors associated with an attribution of the symptoms to the heart and to investigate the association between symptom misinterpretation and time until first medical contact (delay time).
Methods
The study population comprised 1,684 men and 559 women, aged 25–74 years, hospitalized with a first-time AMI recruited from a population-based AMI Registry.
Results
A total of 50.3 % of the patients attributed their experienced symptoms to the heart. Logistic regression modeling revealed that symptoms like chest pain, pain in the left upper extremity, and fear of death facilitated a correct attribution to the heart, whereas symptoms like vomiting or pain in the right upper extremity made a correct labeling difficult. Female sex, low educational status, migration background, and current smoking were associated with a higher risk of misinterpretation of symptoms. A family history of AMI or a history of angina pectoris, hypertension, and hyperlipidemia were shown to facilitate a correct interpretation of symptoms. Variables associated with a misinterpretation of symptoms did not significantly differ between men and women. People with misinterpretation of symptoms had a 1.59-fold risk (95 % confidence interval 1.33–1.90) to have a delay time of at least 2 h, compared with persons who correctly attributed their symptoms.
Conclusions
Symptom misinterpretation is common among patients with AMI, significantly related to symptoms, sociodemographic characteristics and individual risk factors, and associated with a prolonged delay time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background/objectives
Early treatment is paramount to successful therapy of patients with acute myocardial infarction (AMI) [1, 2]. However, pre-hospital delays in seeking treatment for AMI have changed little in recent decades and remain unacceptably long, with median intervals averaging 2–4 h [3–5]. Three main barriers have been identified that contribute to a prolonged pre-hospital delay: misperception of symptoms, misinterpretation of symptoms, and delay in seeking medical attention [5]. A number of studies have almost consistently shown that the misinterpretation of symptoms is a major cause for deciding not to seek medical care [6–11]. Studies found that between one-half and three-quarters of the patients reported that their symptoms were different from what they expected [12, 13], and between 25 and 75 % did not label their symptoms to the heart [6, 8, 14]. The wide range of results could be attributable to the methodological diversity of the studies.
However, available studies substantially vary regarding a number of methodological characteristics, such as population, sample size, standardization of data collection, or adjustment for possible confounding variables.
Thus, the overall objective of the present study was to investigate the role of the interpretation of symptoms for the decision process to seek treatment for AMI in a well-defined, population-based sample of men and women with first-time AMI taking into account potential confounding variables. The specific aims were: firstly, to describe the magnitude of misinterpretation of symptoms; secondly, to identify factors that are associated with a misinterpretation; and thirdly, to investigate the association between symptom misinterpretation and delay time.
Materials and methods
As part of the World Health Organization MONICA (MONItoring trends and determinants in CArdiovascular disease) project, the population-based Augsburg Coronary Event Registry was initiated in 1984 [15]. After the termination of the MONICA project in 1995, the registry became part of the framework of KORA (Cooperative Health Research in the Region of Augsburg). Since 1985, all cases of coronary death and non-fatal AMI within the 25- to 74-year-old study population in the city of Augsburg and the two adjacent counties (about 600,000 inhabitants) have been registered. Data regarding hospitalized patients are obtained from eight hospitals within the study region and two in the adjacent areas. Approximately, 80 % of all AMI cases within the study region are treated in Augsburg’s major hospital, Klinikum Augsburg, a tertiary care center offering invasive and interventional cardiovascular procedures, as well as heart surgery facilities [15, 16]. Methods of case finding, diagnostic classification of events and data quality control have been described previously [15–17]. Informed consent was obtained from each patient and the study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in a priori approval by the ethics committee.
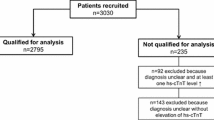
Sample
In the present analysis, all registered patients between 1 January 2001 and 31 December 2006 who survived longer than 24 h with an incident AMI were included. From 3,120 men and women with an incident AMI during the study period, all subjects who could not be interviewed (n = 711) or whose data on any of the covariables were incomplete (n = 166) were excluded. Reasons for missing interviews were: patient died (n = 162), patient declined interview (n = 210), insufficient German language skills (n = 60), early discharge (n = 38), delayed case identification (n = 125), or bad health status (e.g. impaired consciousness or orientation) (n = 116). Finally, the present analysis comprised 1,684 male and 559 female persons aged 25–74 years with an incident AMI.
Data collection
Patients were interviewed during their hospital stay after transfer from the intensive care unit using a standardized questionnaire. The interviews were performed by trained study nurses and included demographic data, data on cardiovascular risk factors, medical history, co-morbidities, and symptoms associated with the AMI event. The initial question on AMI symptoms was: “Did you have pain in the chest or a feeling of pressure or tightness?” Patients were then asked if they had experienced other symptoms and complaints. If they agreed, they were queried on the occurrence of 12 additional symptoms. In addition, the patients were asked which disease they thought of first when the symptoms came up. They could select “heart”, “lung”, “stomach”, “spine”, “other”, and “no attribution” as response options. Patients were classified into those who attributed their symptoms to the heart and those who did not.
Patients were asked for the time between symptom onset and first examination by a physician. Response options were: <5 min, 5 min to <1 h, 1 to <2 h, 2 to <4 h, 4 to <24 h, 1 day, and longer. For the statistical analysis, the cut points of <2 and ≥2 h were chosen to distinguish early from late responders to their symptoms of AMI. In addition, the time of symptom onset was used to define whether the event occurred in the daytime (after 6 a.m. to 10 p.m.) or at night (after 10 p.m. to 6 a.m.). Moreover, patients were asked for their nationality and whether both parents were Germans. In case the patient did not have German nationality or disagreed that both parents were German, a migration background was noted. Further, patients were asked whether father or mother ever had an AMI. If they agreed, a positive family history was documented. Education was requested using four different response options reflecting the national educational system. The highest educational level refers to more than 13 years of education, whereas the lowest level means 9 years of education.
Further data on co-morbidities, electrocardiogram, and in-hospital course were determined by chart review. If the information on co-morbidities from patient report and medical chart differed, the chart information was used.
Data analysis
Continuous data were expressed as median values and interquartile ranges (IQR), and categorical variables as percentages. The Chi-square test was used to determine the differences in frequencies. The Mann–Whitney U test or Kruskal–Wallis test were used to compare medians.
The relationship between the interpretation of symptoms (attribution to the heart or not) and the occurrence of the 13 symptoms and other clinical and demographic characteristics was examined by multiple logistic regression modeling. Significance at the 15 % level in the univariate analysis was used as the criterion for entry in the multivariable model. The variables which were considered as potential confounders are shown in Tables 1 and 2. Since men and women significantly differed regarding the magnitude of misinterpretation of symptoms, the logistic regression models were additionally calculated separately for women and men.
The association between delay time <2 versus ≥2 h and the attribution of symptoms to the heart was also examined by multiple logistic regression modeling taking into account variables that showed a significant association at the 15 % level in the univariate analysis. In all regression analyses, variables with a p value <0.05 were taken to be statistically significant.
Results
The sample consisted of 1,684 male and 559 female persons with a median age of 61 years. The study sample was characterized by 39.6 % who had an ST-segment elevation AMI, 54.9 % had a non-ST-segment elevation AMI and 5.5 % had a bundle branch block. The AMI location was posterior for 44.6 % of the sample, anterior for 40.9 % and not determined for 14.5 %. The median time between hospital admission and patient interview was 6 days (25th percentile: 4 days; 75th percentile: 9 days). Men were significantly more likely to attribute symptoms to the heart than women (51.7 vs. 46.0 %; p = 0.02). In the total sample, 48.7 % had a delay time <2 h. No significant sex or age effects were found in the univariate analysis. Persons who attributed their symptoms to the heart were significantly more likely to have a delay time <2 h compared with persons who misinterpreted their symptoms (see Table 1).
Of the total sample, 50.3 % attributed the experienced symptoms to the heart, 30.4 % reported to have no idea about the origin of the symptoms, and 19.3 % attributed the symptoms to other organs, for instance lung, stomach, or spine (see Table 2). Chest pain, pain in the throat/jaw, and fear of death were most often reported by people who attributed symptoms to the heart. Dyspnea was most common in persons who attributed symptoms to the lung, and pain in the upper abdomen, nausea and vomiting were most often reported by persons who attributed symptoms to the stomach. Pain in the left or right extremity, and between the shoulder blades nausea and diaphoresis were most common in persons who labeled their symptoms to the spine, and dizziness was most common in persons who attributed their symptoms to any other organs. Syncope was most often experienced by persons who reported to have no idea about the origin of their symptoms.
In the total sample, persons who attributed their symptoms to the heart were significantly more likely to be men, to have more than 13 years of education, and to have a family history of AMI compared with persons who failed to attribute their symptoms to the heart (see Table 3). Furthermore, a history of angina pectoris, hypertension, or hyperlipidemia could be shown to facilitate a correct attribution of symptoms to the heart, whereas migration background and current smoking significantly hindered a correct attribution of symptoms. Regarding the experienced symptoms, chest pain or feelings of pressure or tightness, pain in the left upper extremity and fear of death positively supported a correct interpretation, whereas persons who reported vomiting or pain in the right upper extremity significantly less often attributed their symptoms to the heart compared with persons who did not experience those symptoms.
Table 3 displays the results of logistic regression models calculated separately for men and women. A higher educational level, a history of hypertension, and the experience of chest pain seem to be more positively related to a correct interpretation of symptoms in women than in men. Moreover, a family history of AMI and a history of hyperlipidemia and diaphoresis were more positively related to an attribution of symptoms to the heart in men, whereas vomiting, syncope, and pain in upper abdomen were more often associated with a misinterpretation of symptoms in men than in women. However, differences between men and women regarding all variables were not statistically significant.
The results of the multivariable logistic regression analysis on the predictors of the delay time are summarized in Table 4. Persons who correctly attributed their symptoms to the heart had a 1.59-fold likelihood to have a delay time <2 h, compared with persons with symptom misinterpretation. In addition, the experience of syncope, diaphoresis, dizziness, or dyspnea significantly contributed to a shorter delay time. Persons living alone and those with a family history of AMI were significantly less likely to be examined by a physician in <2 h from symptom onset (see Table 4).
Discussion
Our study, based on self-reports from women and men with an incident AMI from the KORA Augsburg Myocardial Infarction Registry showed that only one-half of the persons with an AMI correctly attributed their symptoms to the heart. One-third had no initial idea about the possible origin of the symptoms. Since syncope was most common among this group of patients, it can be assumed that the loss of consciousness was one reason for not being able to perform any symptom attribution. However, most of these patients experienced typical AMI symptoms without being able to recognize that the symptoms may be related to a heart dysfunction. Persons who attributed their symptoms to specific organs, like lung or stomach, also experienced additional symptoms that were commonly associated with dysfunction of the corresponding organs, for instance dyspnea or abdominal pain. The logistic regression analysis confirmed that “typical” AMI symptoms like chest pain, pressure or tightness, or pain in the left extremity were most important for a correct attribution to the heart. Other studies have already confirmed that these symptoms are the most common ones expected by AMI patients [19] and most often known as the beginning of cardiac origin in the general population [20, 21]. The occurrence of unspecific symptoms like vomiting hindered an attribution to the heart in our study. These symptoms were expected by 34 % and, however, experienced by 48 % of the patients included in the study of Perry et al. [19]. To our knowledge, our study is the first to show that the experience of fear of death facilitates the correct symptom attribution, but is not significantly associated with delay time. Moser et al. [8] found that patients who felt anxious about their symptoms delayed less than patients who did not experience anxiety about them. Future studies should have a closer look at the different ways fears may interfere with or facilitate the decision to seek care for AMI symptoms.
Sociodemographic factors including sex, education and migration background were found to significantly influence symptom attribution. We demonstrated that woman more often failed to correctly attribute their symptoms to the heart. This is particularly interesting because a number of studies on the public awareness of AMI symptoms consistently reported that women had a better knowledge of AMI symptoms than men [20, 21]. In addition, women who were already affected by an ischemic heart disease showed better disease knowledge and a more precise perception of their individual risk for a future coronary event than men [22].
Thus, we may assume that the knowledge of AMI symptoms is not sufficient to correctly assign the symptoms to the heart, and the finding in our study might be explained by women who did not sufficiently perceive themselves as being at risk to experience an AMI.
Furthermore, we found in our study that low education and migration background was associated with a higher risk of misinterpretation of symptoms. Consequently, educational interventions for AMI should be targeted specifically at women, persons with low education or migration background.
A history of AMI risk factors including angina pectoris, hypertension, and hyperlipidemia was shown to facilitate the correct interpretation of symptoms. Contrary to our results, Greenlund et al. [20] showed that persons with high blood pressure or cholesterol were not more likely to recognize heart attack symptoms than were persons without these conditions. However, consistent with other findings from Greenlund et al. [20], in our study diabetes was not significantly related to a correct assignment of symptoms to the heart, which may indicate the need to increase educational efforts in this risk group.
In agreement with other studies, we demonstrated that the correct attribution of symptoms to the heart was significantly associated with a lower delay time [6–8, 19, 23, 24]. In addition, some single symptoms, such as syncope, dyspnea, dizziness, and diaphoresis, independently affected delay time positively. While in several studies, a delay in seeking treatment was observed among participants who did not experience diaphoresis [23, 25, 26], an association of syncope, dyspnea, or dizziness with delay time has not yet been reported and needs further investigation.
The most striking findings refer to the different roles that single variables play in two phases of the decision process to seek care, namely the symptom attribution and the decision to call for help. Living alone did not significantly affect the symptom attribution, but was significantly related to a longer delay in seeking treatment. Surprisingly, family history of AMI significantly facilitated the correct symptom attribution on the hand, but on the other hand it was associated with a significantly prolonged delay time. This finding is somehow comparable with other studies, which showed that the experience of a re-infarction does not necessarily have a positive influence on delay time [27] and sometimes is even associated with a longer delay [18]. In persons with re-infarction, previous experiences with cardiac emergency care may have induced fear and denial or even a post-traumatic stress disorder. Denial may influence any future actions delaying calls for help in the situation of the re-infarction. Similarly, the experience of a relatives’ death from an AMI or the care for a close relative affected with an AMI, including the experiences with the health-care system, can be associated with a broad range of emotions and distress that may lead to denial and hinder care seeking if AMI-like symptoms are recognized in the person. More research on patients’ previous experiences with AMI and their associated emotional and cognitive reactions is necessary to clarify its influence on the process of care seeking. It also seems worthwhile to explore how experiences with or beliefs about the health-care system and health-care providers are related to emotional and cognitive reactions. As reported by Pattenden et al. [28], many patients felt concerned about wasting time and resources of the health-care system when calling the ambulance. The identification of factors within the health-care system that contribute to emotions or beliefs which finally prevent people from seeking help could be helpful to develop new interventions targeting not merely the individual patient, but at the entire health-care system.
There are study limitations that are worth considering. First, only patients younger than 75 years were included. In addition, patients who died within 24 h after admission or before the interview could not be included. A high number of subjects were excluded from the analyses, because they could not be interviewed, or data on any of the covariables were incomplete. A limited number of covariables were included in the logistic regression models and it cannot be excluded that further relevant factors have not been sufficiently considered. The definition of family history of AMI was restricted to parents and did not include any age limits. Finally, the study was performed in Germany and the findings may not be generalizable to people from other countries.
In conclusion, our study confirmed that the decision to seek help for symptoms of myocardial infarction is a complex process influenced by various factors. Education on AMI in general and specifically on AMI symptoms should be intensified by public health campaigns in selected target groups such as women, persons with lower educational level, or individuals with migration background. Individual education of those groups should also be provided by clinicians involved in the care of persons with coronary heart disease. However, educational interventions to improve patient knowledge of AMI symptoms are important, but not sufficient to reduce delay time. Thus, more emphasis should be placed on the investigation of the cognitive and emotional processes of the individual that may influence the decision process. A more detailed knowledge of these processes could result in innovative interventions in order to reduce delay time.
References
Lambert L, Brown K, Segal E, Brophy J, Rodes-Cabau J, Bogaty P (2010) Association between timeliness of reperfusion therapy and clinical outcomes in ST-elevation myocardial infarction. JAMA 303:2148–2155
Müller UM, Eitel I, Eckrich K, Erbs S, Linke A, Möbius-Winkler S, Mende M, Schuler GC, Thiele H (2011) Impact of minimising door-to-balloon times in ST-elevation myocardial infarction to less than 30 min on outcome: an analysis over an 8-year period in a tertiary care centre. Clin Res Cardiol 100:297–309
McGinn AP, Rosamond WD, Goff DC Jr, Taylor HA, Miles JS, Chambless L (2005) Trends in prehospital delay time and use of emergency medical services for acute myocardial infarction: experience in 4 US communities from 1987–2000. Am Heart J 150:392–400
Ladwig KH, Meisinger C, Hymer H et al (2010) Sex and age specific time patterns and long term time trends of pre-hospital delay of patients presenting with acute ST-segment elevation myocardial infarction. Int J Cardiol [Epub ahead of print]
Gärtner C, Walz L, Bauernschmitt E, Ladwig KH (2008) The causes of prehospital delay in myocardial infarction. Dtsch Arztebl Int 105:286–291
Thuresson M, Jarlöv MB, Lindahl B, Svensson L, Zedigh C, Herlitz J (2007) Thoughts, actions, and factors associated with prehospital delay in patients with acute coronary syndrome. Heart Lung 36:398–409
Ottesen MM, Dixen U, Torp-Pedersen C, Kober L (2004) Prehospital delay in acute coronary syndrome—an analysis of the components of delay. Int J Cardiol 96:97–103
Moser DK, McKinley S, Dracup K, Chung ML (2005) Gender differences in reasons patients delay in seeking treatment for acute myocardial infarction symptoms. Patient Educ Couns 56:45–54
Kentsch M, Rodemerk U, Muller-Esch G et al (2002) Emotional attitudes toward symptoms and inadequate coping strategies are major determinants of patient delay in acute myocardial infarction. Z Kardiol 91:147–155
McKinley S, Moser DK, Dracup K (2000) Treatment-seeking behavior for acute myocardial infarction symptoms in North America and Australia. Heart Lung 29:237–247
Dracup K, Moser DK (1997) Beyond sociodemographics: factors influencing the decision to seek treatment for symptoms of acute myocardial infarction. Heart Lung 26:253–262
Horne R, James D, Petrie K, Weinman J, Vincent R (2000) Patients’ interpretation of symptoms as a cause of delay in reaching hospital during acute myocardial infarction. Heart 83:388–393
Johnson JA, King KB (1995) Influence of expectations about symptoms on delay in seeking treatment during myocardial infarction. Am J Crit Care 4:29–35
Perkins-Porras L, Whitehead DL, Strike PC, Steptoe A (2009) Pre-hospital delay in patients with acute coronary syndrome: factors associated with patient decision time and home-to-hospital delay. Eur J Cardiovasc Nurs 8:26–33
Meisinger C, Hörmann A, Heier M, Kuch B, Löwel H (2006) Admission blood glucose and adverse outcomes in non-diabetic patients with myocardial infarction in the reperfusion era. Int J Cardiol 113:229–235
Kuch B, Heier M, von Scheidt W, Kling B, Hoermann A, Meisinger C (2007) 20-Year-trends in clinical characteristics, therapy and short-term prognosis in acute myocardial infarction according to presenting electrocardiogram—results of the MONICA/KORA Augsburg Myocardial Infarction Registry (1985–2004). Am J Cardiol 100:1056–1060
Alpert JS, Thygesen K, Antman E, Bassand JP (2000) Myocardial infarction redefined—a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol 36:959–969
Saczynski JS, Yarzebski J, Lessard D et al (2008) Trends in prehospital delay in patients with acute myocardial infarction (from the Worcester Heart Attack Study). Am J Cardiol 15(102):1589–1594
Perry K, Petrie KJ, Ellis CJ, Horne R, Moss-Morris R (2001) Symptom expectations and delay in acute myocardial infarction patients. Heart 86:91–93
Greenlund KJ, Keenan NL, Giles WH et al (2004) Public recognition of major signs and symptoms of heart attack: seventeen states and the US Virgin Islands, 2001. Am Heart J 147:1010–1016
Centers for Disease Control and Prevention (CDC) (2008) Disparities in adult awareness of heart attack warning signs and symptoms–14 states, 2005. MMWR Morb Mortal Wkly Rep 2008(57):175–179
Dracup K, McKinley S, Doering LV et al (2008) Acute coronary syndrome: what do patients know? Arch Intern Med 168:1049–1054
Bunde J, Martin R (2006) Depression and prehospital delay in the context of myocardial infarction. Psychosom Med 68:51–57
Fox-Wasylyshyn SM, El-Masri M, Artinian NT (2010) Testing a model of delayed care-seeking for acute myocardial infarction. Clin Nurs Res 19:38–54
Goldberg RJ, Steg PG, Sadiq I et al (2002) Extent of, and factors associated with, delay to hospital presentation in patients with acute coronary disease (the GRACE registry). Am J Cardiol 89:791–796
Zerwic JJ, Ryan CJ, DeVon HA, Drell MJ (2003) Treatment seeking for acute myocardial infarction symptoms: differences in delay across sex and races. Nurs Res 52:159–167
Carney R, Fitzsimons D, Dempster M (2002) Why people experiencing acute myocardial infarction delay seeking medical assistance. Eur J Cardiovasc Nurs 1:237–242
Pattenden J, Watt I, Lewin RJ, Stanford N (2002) Decision making processes in people with symptoms of acute myocardial infarction: qualitative study. BMJ 324(7344):1006–1009
Acknowledgments
The KORA research platform and the MONICA Augsburg studies were initiated and financed by the Helmholtz Zentrum München, German Research Center for Environmental Health, which is funded by the German Federal Ministry of Education, Science, Research and Technology and by the State of Bavaria. Since the year 2000, the collection of AMI data has been co-financed by the German Federal Ministry of Health to provide population-based AMI morbidity data for the official German Health Report (see http://www.gbe-bund.de). Steering partners of the MONICA/KORA Infarction Registry, Augsburg, include the KORA research platform, Helmholtz Zentrum München and the Department of Internal Medicine I, Cardiology, Central Hospital of Augsburg. We thank all members of the Helmholtz Zentrum München, Institute of Epidemiology II and the field staff in Augsburg who were involved in the planning and conduct of the study. We wish to thank the local health departments, the office-based physicians, and the clinicians of the hospitals within the study area for their support. Finally, we express our appreciation to all study participants.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kirchberger, I., Heier, M., Wende, R. et al. The patient’s interpretation of myocardial infarction symptoms and its role in the decision process to seek treatment: the MONICA/KORA Myocardial Infarction Registry. Clin Res Cardiol 101, 909–916 (2012). https://doi.org/10.1007/s00392-012-0475-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-012-0475-8