Abstract
Background
Systolic heart failure (SHF) and chronic obstructive pulmonary disease (COPD) are frequently associated. The purpose of our study was to explore the impact of COPD severity on symptoms and prognosis in patients with SHF.
Methods and results
Chronic obstructive pulmonary disease was systematically screened by spirometry in 348 patients admitted for SHF from April 2002 to December 2006. Severity of COPD was defined according to the GOLD classification. Prevalence of COPD was 37.9 %. Patients’ distribution according to GOLD stages I, II, II and IV were, respectively, 51.5, 37.9, 7.6 and 3.0 %. Severity of dyspnoea increases with GOLD stage. There was a significant correlation between NYHA stage and left ventricular ejection fraction in patients without COPD (R 2 = 0.03; P = 0.01) but not in patients with COPD. Mean follow-up was of 54.9 ± 27.4 months. Mortality was 46.6 % and was highest in the COPD group (53.8 vs. 42.3 %; P = 0.049). Kaplan–Meier survival curves showed that patients with GOLD stage I had the same prognosis than patients without COPD and mortality increased from GOLD stage II to stage IV. After multivariate analysis, GOLD stage and diuretics’ dose were independently associated with mortality.
Conclusions
Chronic obstructive pulmonary disease is frequent in patients with SHF and increases mortality. Since dyspnoea is poorly specific of COPD in chronic heart failure patients, COPD remains underdiagnosed thus leading to inappropriate increase of diuretics’ dose. COPD should be systematically screened in patients with SHF to adapt prescription of selective β1-blockers, and diuretics’ dose and reduce the exposition to risk factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systolic heart failure (SHF) and chronic obstructive pulmonary disease (COPD) share the same risk factors, which partly explains their frequent association [1]. They also share same symptoms explaining why COPD is often under-diagnosed in patients with SHF [2]. SHF and COPD have an important prognostic value independently of their association [3, 4]. Patients with COPD are more susceptible to develop SHF [5] that is an independent predictor of all-cause mortality in COPD patients [6]. In spite of the same risk factors and symptoms, SHF and COPD have different pathophysiology, which requires opposite treatments and represents new therapeutic challenges [7]. If recent studies suggest that COPD is common in patients with SHF [8] and increase mortality [8, 9], there is few data about the impact of COPD severity assessed by GOLD stage on symptoms and prognosis in SHF population.
The purpose of our study was to explore the impact of COPD severity assessed by GOLD stage on symptoms and prognosis in patients with SHF.
Methods
Study population
From April 2002 to December 2006, we identified 679 patients prospectively hospitalized for the management and the exploration of SHF in the heart failure Unit of Toulouse University Hospital. Patients living <100 km away from our hospital systematically underwent pulmonary testing by spirometry within a week after discharge. We thus retrospectively identified 371 chronic heart failure patients screened for a pulmonary test (Fig. 1). SHF was defined according to the European Society of Cardiology guidelines [10]. Left ventricular systolic dysfunction was defined by a left ventricular ejection fraction (LVEF) ≤45 % assessed by transthoracic echocardiography using the conventional apical two- and four-chamber views and the modified Simpson’s method. Exclusion criteria were acute myocardial infarction within the last 3 months. Decompensated SHF was defined by the exacerbation of typical symptoms of SHF within the last month. All patients were explored by coronary angiography within the last 2 years and the diagnosis of ischaemic cardiomyopathy was retained when there was >50 % stenosis of at least one principal coronary artery. Dyspnoea was quantified according to the New York Heart Association (NYHA) functional class [10]. Self-reported COPD was retained when patients reported the diagnosis or when the diagnosis was reported by a previous report. Current smoking was defined by a smoking habitus persisting during the last month. Systemic hypertension was defined as a systolic blood pressure ≥140 mmHg or a diastolic blood pressure ≥90 mmHg without treatment; hypercholesterolemia in patients without atherosclerotic cardiovascular disease as a total plasma cholesterol or LDL cholesterol above 5 and 3 mmol/L, respectively, or in patients with atherosclerotic cardiovascular disease or diabetes above 4 and 2.5 mmol/L, respectively; obesity as a body mass index ≥30 kg/m2 and chronic renal insufficiency as an estimated glomerular filtration rate by Cockcroft and Gault formula <60 mL/min/1.73 m2. Creatinin levels were collected with missing data for 14 (3.8 %) patients.
Pulmonary function test
Patients with stable SHF had systematic spirometry performed by practice nurses. All spirometry curves were reviewed retrospectively by the same trained investigator (BA). The following measures of lung function were collected at baseline and 15 min after bronchodilator test consisting in inhalation of 400 μg of salbutamol: forced expiratory volume in 1 s (FEV1), forced vital capacity (FVC) and FEV1/FVC ratio. COPD was defined by a post-bronchodilatator FEV1/FVC ratio <0.7. When FEV1/FVC ratio was between 0.68 and 0.72 spirometry was analysed by an expert pneumologist (RE) which categorized the patient as COPD or no COPD. The severity of COPD was based on the Global initiative for chronic Obstructive Lung Disease (GOLD) classification [11]. GOLD stage I (mild COPD) was defined as post-bronchodilator FEV1 >80 % of predicted. GOLD stage II (moderate COPD) was defined as post-bronchodilator 50 % ≤ FEV1 < 80 % of predicted. GOLD stage III (severe COPD) was defined as post-bronchodilator 30 % ≤ FEV1 < 50 % of predicted. GOLD stage IV (very severe COPD) was defined as post-bronchodilator FEV1 < 30 % of predicted, or FEV1 < 50 % of predicted in association with chronic respiratory failure defined by arterial partial pressure of oxygen (PaO2) < 60 mmHg with or without arterial partial pressure of CO2 (PaCO2) > 50 mmHg while breathing room air. During hospitalization, physicians were blinded for the results of spirometry and patients were treated independently of their pulmonary status.
Follow-up
Clinical follow-up was assessed in October 2010 by phone interview of patient’s general practitioner/cardiologist, patient himself, or his family. The outcome event examined was total mortality. Patients unable to be interviewed up to 6 months at the date of follow-up were considered as lost to follow-up. Only patients with available demographic data were used for survival analysis. This research investigation was approved by the ethical committee of the Institutional Review Board of our hospital.
Statistical analysis
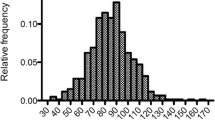
Continuous variables were tested for normal distribution using the Kolmogorov–Smirnov test and expressed as mean ± standard deviation. Nominal values were expressed as numbers and percentages. Association between the mean values of continuous normally distributed variables were compared using unpaired and paired Student’s t test and the Mann–Whitney rank sum test was used when the samples were not normally distributed or had unequal variances. Comparison between multiple groups was performed with analysis of variance (ANOVA), with post hoc analysis performed as appropriate. Nominal variables were investigated by the χ 2 test. Relationships between variables were assessed using linear regression analysis and expressed as R 2. Total mortality was summarized using Kaplan–Meier survival curves and log rank test was used for initial comparisons. Univariate and multivariate comparisons were made using a Cox proportional hazards regression model. Univariate variables with a P value of <0.20 were entered into the multivariate logistic models. Differences were considered statistically significant for P values of <0.05. All analyses were performed using Statview 5.0 (SAS Institute Inc., Cary, NC, USA).
Results
Baseline characteristics of patients with SHF according to the presence of COPD
Between April 2002 and December 2006, 371 patients were proposed for a screening by systematic pulmonary function test. Twenty-three patients were excluded because the spirometry was not feasible (14 patients; 3.8 %) or due to the low quality of the spirometry (9 patients; 2.4 %). Among the 348 others patients, 132 (37.9 %) had COPD proven by spirometry.
Baseline clinical characteristics and treatments of patients according to the presence of COPD are shown in Table 1. There were 68 (51.5 %), 50 (37.9 %), 10 (7.6 %) and 4 (3.0 %) patients with GOLD stage I, II, III and IV, respectively. History of COPD in patients GOLD stage II, III and IV was for 22.0, 60.0 and 50.0 %, respectively (P < 0.0001). No patient had theophylline at admission.
Baseline clinical characteristics and treatment of patients with COPD according to the GOLD stage are shown in Table 2. The NYHA stage increases with GOLD stage. β-2 agonist therapies increase and beta-blocker therapies decrease with GOLD stage.
Correlation between dyspnoea and LVEF according to the presence of COPD in patients with SHF
There is a low but significant correlation between the NYHA stage and the LVEF in patients without COPD (R 2 = 0.03; P = 0.01). This correlation was no longer significant in patients with COPD (P = 0.15).
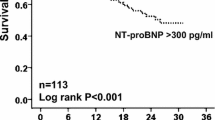
Prognosis of patients with SHF according to the presence of COPD
Thirty-three patients (9.4 %) were missing for follow-up: 20 (9.3 %) in the no COPD group and 13 (9.8 %; P = 0.86) in the COPD group. Among the 315 other patients, mean follow-up time was 54.9 ± 27.4 months. Mortality occurred in 147 patients (46.6 %) and was greatest in COPD group compared to no COPD group (n = 64; 53.8 % vs. n = 83; 42.3 % P = 0.049; Fig. 1). The Kaplan–Meier plot survival for patients with SHF according to the presence of COPD are shown in Fig. 2.
Figure 3 shows the Kaplan–Meier plot survival for patients with COPD according to the GOLD classification: patients with GOLD stage I had the same prognosis than patients without COPD and mortality increased from GOLD stage II to stage IV.
Univariate and multivariate Cox proportional hazards regression model analysis for predictors of all-cause mortality in patients with SHF
Table 3 summarizes the prognostic value for all-cause mortality of different clinical, and treatment characteristics. In univariate analyses, age, NYHA stage III and IV, decompensated SHF, LVEF, COPD, GOLD stage, FEV1, atrial fibrillation, renal insufficiency, history of COPD, exposure and diuretics’ dose, ACEI/ARB treatment, beta-blockers, β-2 agonists and implantable cardioverter defibrillator (ICD) with or without cardiac resynchronization therapy (CRT) had significant prognostic value. After multivariate analyse, only GOLD stage and dose of diuretics were independent predictors with an hazard ratio of 2.274 (95% CI 1.218–4.245; P = 0.01) for GOLD stage II, 2.813 (95% CI 1.029–7.687; P = 0.044) for GOLD stage III and IV and 1.012 (95% CI 1.002–1.022; P = 0.017) for a 10 mg per day increment in diuretics dose.
Discussion
Our study confirms association between SHF and COPD is frequent. In our study, COPD is found in more than one-third of patients with SHF and deteriorate the prognosis. This prevalence is concordant with recent studies that detected COPD by systematic spirometry [8, 12] but much more important than in studies based on self-reported COPD which reported a prevalence of 19.5–23.6 % [13, 14]. Previous studies with screening of COPD by systematic spirometry have selected patients with decompensated SHF [8, 12]. Intravascular overload increase airflow obstruction in patients with left ventricular dysfunction [15] and may explain the increased risk of mortality attributed to COPD previously reported in patients with SHF [8]. Our results show that prevalence of COPD detected by systematic spirometry is similar in decompensated and compensated SHF (Table 1). By multivariate analysis, COPD is an independent factor of mortality in patients with SHF but decompensated SHF is not. This increased risk begins from GOLD stage II and increase with the severity of the COPD: patients with GOLD stage I have the same prognosis than patients without COPD. After multivariate analysis GOLD stage II and GOLD stage III and IV are independent factors of mortality. The influence of the severity of the COPD on mortality in general population is well known [16]. We show in a population of SHF this correlation begins from the GOLD stage II. Nevertheless, COPD and particularly GOLD stage II are underestimate in patients with SHF. In our population, less than quarter of patients detected GOLD stage II reported an history of COPD versus more than half in patients detected GOLD stage III and IV.
The other independent factor of mortality is the diuretics’ dose. The influence of diuretics’ dose on mortality could suggest that higher doses of diuretics identify sicker patients who have a worse outcome. This explanation is highlighted by recent evidence about the association between higher diuretics’ dose and shorter survival in patients with decompensated SHF [17]. COPD is reported to participate to functional impairment in patients with SHF [18]. We do the hypothesis that part of dyspnoea attributable to COPD in patients with SHF is misrecognized by the physician and reattached to volume overload bringing to increase diuretics. This hypothesis could explain the increased rate of renal insufficiency in COPD population, which is a factor of mortality by univariate analysis but no longer after adjustment of diuretics’ doses. Our results show dyspnoea increases with GOLD stage: patients with GOLD stage III and IV are more symptomatic than patients with GOLD stage I and II but have the same LVEF (Table 2). In the whole population, patients with COPD have a better LVEF than patients without COPD but have the same NYHA stage (Table 1). We show in patients with SHF and without COPD there is a low but significant correlation between the LVEF and the NYHA stage. This correlation is no longer significant in patients with both SHF and COPD, showing the poor specificity of dyspnoea in this population. These results strengthen the hypothesis that part of dyspnoea due to the obstructive airway disease is under diagnosed and wrongly reattached to SHF. Others confounding factors can participate to the lack of specificity of dyspnoea. In our study, patients with COPD had highest age and body mass index than patient without COPD that can participate to exercise deconditioning and explain part of dyspnoea. But the absence of prognostic value of the NYHA stage after multivariate analysis confirms the lack of specificity of dyspnoea in this population. Finally, multivariate analysis shows association of ICD and CRT had tendency to increase mortality but not ICD alone. We can suppose patients indicated for both ICD and CRT are more symptomatic than patients indicated for ICD alone whom are selected only on LVEF levels. This last result highlight the hypothesis that dyspnoea due to COPD is incorrectly reattached to left ventricular dysfunction explaining the tendency to an increased risk of mortality in patients selected for both ICD and CRT but the absence of influence of ICD alone and LVEF.
Others characteristics that differentiate patients with than patients without COPD are usual parameters accompanying obstructive airways diseases: lowest FEV1, more β-2 agonists and inhaled corticosteroids and more history of smoking and COPD. Nevertheless, after multivariate analysis, none of these factors is predictor of mortality.
The main problem of a systematic screening of COPD in patients with SHF is the impact on therapeutic decision. Main therapeutic drugs used in SHF and COPD, represented by beta-blockers and β-2 agonists, respectively, have common biological target but opposite effects. Studies show beta-blockers are well tolerated in patients with COPD [19, 20]. Moreover, the use of beta-blockers in hospitalized patients with acute exacerbation of COPD is associated with reduced mortality [21]. In the other hand, use of β-2 agonist in patients with COPD are reattached to an increased cardiovascular risk [22] with increased SHF [23], acute coronary syndrome [24] and primary cardiac arrest [25]. If recent studies show that beta-blockers are beneficial in patients with both SHF and COPD [26], benefits and risks of use of β-2 agonists in this population is still debated [23, 27, 28]. In our study, univariate analysis show beta-blockers have a protective effect and β-2 agonist a noxious effect on mortality. After multivariate analysis and adjustment for confounding factors, neither beta-blockers nor β-2 agonists have prognostic value. Our results show patients with advanced COPD have more history of COPD, more β-2 agonists and more inhaled corticosteroids. These results suggest β-2 agonists and inhaled corticosteroids select sicker patients with more advanced COPD that is an independent factor of mortality.
Clinical implications
The high prevalence of COPD in patients with SHF, and the lack of specificity of dyspnoea incite to propose systematic screening of airflow obstruction to prefer β1-selective beta-blockers which decreased hospitalization [29] and mortality [23, 26] in patients with COPD. Recent study shows that if switch between β1-selective and non-selective beta-blockers is well tolerated in COPD with SHF, functional parameters are better with β1-selective beta-blockers [30]. Diagnosis of COPD in patients with SHF must alert the physician of the risk of misdiagnosed dyspnoea and over treat symptoms of volume overload with the risk of hypokaliemia and renal insufficiency. Furthermore, screening of COPD must incite to better risk factors control and particularly current smoking.
Limitations of the study
Main limit of this study is the lack of biological marker of SHF. It is nowadays proven that natriuretic peptides are discriminate markers to categorize dyspnoea [31]. Natriuretic peptide measurements in patients with chronic heart failure receiving optimal medical therapy can also predict cardiovascular prognosis [32]. However, there is few data of their utility in the specific population of patients with both SHF and COPD. Systematic testing of natriuretic peptides was introduced only since 2006 to our SHF Unit.
We have no information about treatment during the follow-up. We cannot exclude that part of mortality observed in patients with advanced COPD was attributable to default of adherence to treatment. Indeed, in our study, patients with more advanced COPD had higher NYHA functional class. Recent study shows that NYHA class III/IV is negatively associated with adherence to treatment in patients with SHF [33].
Another limit of this study is the lack of information concerning the death. We show that total mortality of patients with SHF increases with the stage of COPD, but we have no information concerning the influence of COPD on sudden cardiac death and rhythmic events. Nevertheless, sudden cardiac death and rhythmic events are classical major adverse cardiac events in patients with SHF that can be effectively treated by ICD. Studies show that COPD is associated with neurohumoral activation [34], left ventricular sympathetic nervous dysfunction [35] and increased cardiac sudden death in patients with history of myocardial infarction [36]. This pathophysiology of COPD by activation of the sympathetic nervous system could explain the benefit of beta-blockers previously reported in patients with COPD irrespective of GOLD stage [26].
Conclusion
More than one-third of patients with SHF have COPD, which increases mortality in patients with SHF from GOLD stage II to IV. Because part of dyspnoea attributable to COPD is wrongly attributed to left ventricular dysfunction and volume overload, most of COPD are underdiagnosed in this population, leading to inappropriate increase of diuretics’ dose. COPD should be systematically detected in patients with SHF to enhance selective β1-blockers prescription, adapt diuretics’ dose and reduce the exposition to risk factors for COPD known to increase mortality.
References
Rutten FH, Cramer MJ, Lammers JW, Grobbee DE, Hoes AW (2006) Heart failure and chronic obstructive pulmonary disease: an ignored combination? Eur J Heart Fail 8(7):706–711
Hawkins NM, Petrie MC, Jhund PS, Chalmers GW, Dunn FG, McMurray JJ (2009) Heart failure and chronic obstructive pulmonary disease: diagnostic pitfalls and epidemiology. Eur J Heart Fail 11(2):130–139
Mannino DM, Brown C, Giovino GA (1997) Obstructive lung disease deaths in the United States from 1979 through 1993. An analysis using multiple-cause mortality data. Am J Respir Crit Care Med 156(3 Pt 1):814–818
Levy D, Kenchaiah S, Larson MG, Benjamin EJ, Kupka MJ, Ho KK, Murabito JM, Vasan RS (2002) Long-term trends in the incidence of and survival with heart failure. N Engl J Med 347(18):1397–1402
Finkelstein J, Cha E, Scharf SM (2009) Chronic obstructive pulmonary disease as an independent risk factor for cardiovascular morbidity. Int J Chron Obstruct Pulmon Dis 4:337–349
Boudestein LC, Rutten FH, Cramer MJ, Lammers JW, Hoes AW (2009) The impact of concurrent heart failure on prognosis in patients with chronic obstructive pulmonary disease. Eur J Heart Fail 11(12):1182–1188
Hawkins NM, Petrie MC, Macdonald MR, Jhund PS, Fabbri LM, Wikstrand J, McMurray JJ (2011) Heart failure and chronic obstructive pulmonary disease the quandary of Beta-blockers and Beta-agonists. J Am Coll Cardiol 57(21):2127–2138
Iversen KK, Kjaergaard J, Akkan D, Kober L, Torp-Pedersen C, Hassager C, Vestbo J, Kjoller E (2010) The prognostic importance of lung function in patients admitted with heart failure. Eur J Heart Fail 12(7):685–691
Kwon BJ, Kim DB, Jang SW, Yoo KD, Moon KW, Shim BJ, Ahn SH, Cho EJ, Rho TH, Kim JH (2010) Prognosis of heart failure patients with reduced and preserved ejection fraction and coexistent chronic obstructive pulmonary disease. Eur J Heart Fail 12(12):1339–1344
Dickstein K, Cohen-Solal A, Filippatos G, McMurray JJ, Ponikowski P, Poole-Wilson PA, Stromberg A, van Veldhuisen DJ, Atar D, Hoes AW, Keren A, Mebazaa A, Nieminen M, Priori SG, Swedberg K, Vahanian A, Camm J, De Caterina R, Dean V, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL (2008) ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur Heart J 29(19):2388–2442
Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, Fukuchi Y, Jenkins C, Rodriguez-Roisin R, van Weel C, Zielinski J (2007) Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 176(6):532–555
Iversen KK, Kjaergaard J, Akkan D, Kober L, Torp-Pedersen C, Hassager C, Vestbo J, Kjoller E (2008) Chronic obstructive pulmonary disease in patients admitted with heart failure. J Intern Med 264(4):361–369
Rusinaru D, Saaidi I, Godard S, Mahjoub H, Battle C, Tribouilloy C (2008) Impact of chronic obstructive pulmonary disease on long-term outcome of patients hospitalized for heart failure. Am J Cardiol 101(3):353–358
Macchia A, Monte S, Romero M, D’Ettorre A, Tognoni G (2007) The prognostic influence of chronic obstructive pulmonary disease in patients hospitalised for chronic heart failure. Eur J Heart Fail 9(9):942–948
Puri S, Dutka DP, Baker BL, Hughes JM, Cleland JG (1999) Acute saline infusion reduces alveolar-capillary membrane conductance and increases airflow obstruction in patients with left ventricular dysfunction. Circulation 99(9):1190–1196
Celli BR, Cote CG, Marin JM, Casanova C, Montes de Oca M, Mendez RA, Pinto Plata V, Cabral HJ (2004) The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med 350(10):1005–1012
Gorelik O, Almoznino-Sarafian D, Shteinshnaider M, Alon I, Tzur I, Sokolsky I, Efrati S, Babakin Z, Modai D, Cohen N (2009) Clinical variables affecting survival in patients with decompensated diastolic versus systolic heart failure. Clin Res Cardiol 98(4):224–232. doi:10.1007/s00392-009-0746-1
Edelmann F, Stahrenberg R, Gelbrich G, Durstewitz K, Angermann CE, Dungen HD, Scheffold T, Zugck C, Maisch B, Regitz-Zagrosek V, Hasenfuss G, Pieske BM, Wachter R (2011) Contribution of comorbidities to functional impairment is higher in heart failure with preserved than with reduced ejection fraction. Clin Res Cardiol 100(9):755–764. doi:10.1007/s00392-011-0305-4
Mascarenhas J, Lourenco P, Lopes R, Azevedo A, Bettencourt P (2008) Chronic obstructive pulmonary disease in heart failure. Prevalence, therapeutic and prognostic implications. Am Heart J 155(3):521–525
Salpeter S, Ormiston T, Salpeter E (2005) Cardioselective beta-blockers for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 19(4):CD003566
Dransfield MT, Rowe SM, Johnson JE, Bailey WC, Gerald LB (2008) Use of beta blockers and the risk of death in hospitalised patients with acute exacerbations of COPD. Thorax 63(4):301–305
Macie C, Wooldrage K, Manfreda J, Anthonisen N (2008) Cardiovascular morbidity and the use of inhaled bronchodilators. Int J Chron Obstruct Pulmon Dis 3(1):163–169
Au DH, Udris EM, Curtis JR, McDonell MB, Fihn SD (2004) Association between chronic heart failure and inhaled β-2-adrenoceptor agonists. Am Heart J 148(5):915–920
Au DH, Curtis JR, Every NR, McDonell MB, Fihn SD (2002) Association between inhaled beta-agonists and the risk of unstable angina and myocardial infarction. Chest 121(3):846–851
Lemaitre RN, Siscovick DS, Psaty BM, Pearce RM, Raghunathan TE, Whitsel EA, Weinmann SA, Anderson GD, Lin D (2002) Inhaled β-2 adrenergic receptor agonists and primary cardiac arrest. Am J Med 113(9):711–716
Hawkins NM, MacDonald MR, Petrie MC, Chalmers GW, Carter R, Dunn FG, McMurray JJ (2009) Bisoprolol in patients with heart failure and moderate to severe chronic obstructive pulmonary disease: a randomized controlled trial. Eur J Heart Fail 11(7):684–690
Au DH, Udris EM, Fan VS, Curtis JR, McDonell MB, Fihn SD (2003) Risk of mortality and heart failure exacerbations associated with inhaled beta-adrenoceptor agonists among patients with known left ventricular systolic dysfunction. Chest 123(6):1964–1969
Bermingham M, O’Callaghan E, Dawkins I, Miwa S, Samsudin S, McDonald K, Ledwidge M (2011) Are β-2-agonists responsible for increased mortality in heart failure? Eur J Heart Fail 13(8):885–891
Brooks TW, Creekmore FM, Young DC, Asche CV, Oberg B, Samuelson WM (2007) Rates of hospitalizations and emergency department visits in patients with asthma and chronic obstructive pulmonary disease taking beta-blockers. Pharmacotherapy 27(5):684–690
Jabbour A, Macdonald PS, Keogh AM, Kotlyar E, Mellemkjaer S, Coleman CF, Elsik M, Krum H, Hayward CS (2010) Differences between beta-blockers in patients with chronic heart failure and chronic obstructive pulmonary disease: a randomized crossover trial. J Am Coll Cardiol 55(17):1780–1787
Mogelvang R, Goetze JP, Schnohr P, Lange P, Sogaard P, Rehfeld JF, Jensen JS (2007) Discriminating between cardiac and pulmonary dysfunction in the general population with dyspnea by plasma pro-B-type natriuretic peptide. J Am Coll Cardiol 50(17):1694–1701
Franke J, Frankenstein L, Schellberg D, Bajrovic A, Wolter JS, Ehlermann P, Doesch AO, Nelles M, Katus HA, Zugck C (2011) Is there an additional benefit of serial NT-proBNP measurements in patients with stable chronic heart failure receiving individually optimized therapy? Clin Res Cardiol 100(12):1059–1067. doi:10.1007/s00392-011-0340-1
Zugck C, Franke J, Gelbrich G, Frankenstein L, Scheffold T, Pankuweit S, Duengen HD, Regitz-Zagrosek V, Pieske B, Neumann T, Rauchhaus M, Angermann CE, Katus HA, Ertl GE, Stork S (2011) Implementation of pharmacotherapy guidelines in heart failure: experience from the German Competence Network Heart Failure. Clin Res Cardiol. doi:10.1007/s00392-011-0388-y
Andreas S, Anker SD, Scanlon PD, Somers VK (2005) Neurohumoral activation as a link to systemic manifestations of chronic lung disease. Chest 128(5):3618–3624
Sakamaki F, Satoh T, Nagaya N, Kyotani S, Nakanishi N, Ishida Y (1999) Abnormality of left ventricular sympathetic nervous function assessed by (123)I-metaiodobenzylguanidine imaging in patients with COPD. Chest 116(6):1575–1581
Hawkins NM, Huang Z, Pieper KS, Solomon SD, Kober L, Velazquez EJ, Swedberg K, Pfeffer MA, McMurray JJ, Maggioni AP (2009) Chronic obstructive pulmonary disease is an independent predictor of death but not atherosclerotic events in patients with myocardial infarction: analysis of the Valsartan in Acute Myocardial Infarction Trial (VALIANT). Eur J Heart Fail 11(3):292–298
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Arnaudis, B., Lairez, O., Escamilla, R. et al. Impact of chronic obstructive pulmonary disease severity on symptoms and prognosis in patients with systolic heart failure. Clin Res Cardiol 101, 717–726 (2012). https://doi.org/10.1007/s00392-012-0450-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-012-0450-4