Abstract
Background
It is assumed that patients with non-ST-elevation myocardial infarctions (NSTEMI) showing an infero- or posterolateral occluded culprit artery (OCA) during diagnostic angiography frequently elude standard 12-lead electrocardiogram diagnosis. In addition, coronary collaterals may have beneficial effects in patients with OCA.
Methods
We examined 448 consecutive NSTEMI patients within 72 h of symptom onset. All patients underwent early invasive angiography plus optimal medical therapy. We compared clinical characteristics and 30-days/6-month major adverse cardiovascular events (MACE) between patients with OCA and non-OCA. The secondary objective was to investigate the effect of angiographically visible coronary collaterals on 6-month MACE in patients with OCA.
Results
The angiograms revealed OCA in 130 (29%) of 448 patients. Patients with OCA showed more often infero- or posterolateral lesions (75 vs. 53%, p < 0.001) and more collaterals (57 vs. 8%, p < 0.001) compared with those with non-OCA. Patients with OCA had larger infarcts (peak CK-MB 2.1 ± 2.3 vs. 1.2 ± 1.1 μmol/L/s, p < 0.001), lower left ventricular ejection fraction (42 ± 21 vs. 48 ± 20%, p = 0.01), were more often revascularized (89 vs. 78%, p = 0.005), and had higher risk-adjusted 6-month MACE largely driven by its association with non-fatal reinfarctions (HR 2.16, 95% CI 1.04–4.50, p = 0.04). Patients with OCA and angiographically absent collaterals had significantly higher risk-adjusted 6-month MACE than those with OCA and angiographically visible collaterals (HR 1.96, 95% CI 1.02–3.76, p = 0.04).
Conclusions
Approximately one-fourth of patients with NSTEMI revealed OCA that was more frequently found in coronary arteries supplying the infero- or posterolateral myocardium. Patients with OCA had larger infarcts and more non-fatal reinfarctions than patients with non-OCA. Well-developed collaterals may limit the myocardial damage in these patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The electrocardiogram (ECG) plays a central role in the early assessment of patients with suspected acute coronary syndrome (ACS). According to the European Society of Cardiology guidelines an immediate revascularization is recommended in patients with persistent ST-segment elevation and assumed acute coronary occlusion from prognostic point of view [1]. In patients without ST-segment elevation the further management is variable and guided by risk stratification. In high-risk patients coronary angiography and subsequent revascularization—when indicated—is recommended within 72 h [2, 3].
However, ST-segment elevation on the standard 12-lead ECG, although specific as a surrogate marker, is insensitive to acute posterolateral circulation coronary artery occlusion. This false diagnosis especially occurs in cases, where the left circumflex artery represents the culprit lesion [4]. In a recently published study, more than one quarter of patients given the diagnosis of acute non-ST-segment myocardial infarction (NSTEMI) had an occluded culprit artery (OCA) on diagnostic angiography, with a predilection for infero- or posterolateral localization of these occluded arteries. Patients with OCA had larger infarcts and worse long-term outcomes, and might represent ST-segment myocardial infarction (STEMI) equivalents not identified by the standard 12-lead ECG-based risk stratification approach [5].
It has been shown that the presence of well-developed collaterals has beneficial effects on infarct size, coronary microcirculation, viability, ventricular function, and ventricular aneurysm formation after acute coronary occlusion in patients with STEMI [6–11]. The effect of coronary collaterals on long-term outcome in patients with acute coronary occlusion treated as STEMI by immediate revascularization is ambiguous [12–15]. Moreover, the effect of coronary collaterals among patients with NSTEMI undergoing an early invasive management of OCA is yet not sufficiently known.
Therefore, the aim of this prospective study in patients with NSTEMI was to compare clinical characteristics and 30-days/6-month major adverse cardiovascular events (MACE) between patients with OCA and non-OCA. The secondary objective was to investigate the effect of angiographically visible coronary collaterals on 6-month MACE in patients with OCA in NSTEMI.
Methods
Study population
The prospective study included 602 consecutive patients (age 68 ± 12 years; 399 males, 203 females) admitted to our tertiary care center with acute NSTEMI.
Inclusion criteria were (1) age between 18 and 90 years, (2) onset of angina pectoris at rest <24 h or crescendo angina in recent weeks with symptoms under minimal exertion or at rest lasting <24 h, and (3) elevated troponin T ≥0.03 ng/mL. Exclusion criteria were (1) persistent angina, (2) STEMI, (3) hemodynamic instability including cardiogenic shock, (4) oral anticoagulation therapy, (5) contraindications for glycoprotein IIb/IIIa inhibitors, (6) other disease with life expectancy <6 months, (7) known coagulopathy, (8) pregnancy, (9) other suspected causes of troponin elevation as myocarditis, secondary to hypertensive crisis, or cardiac decompensation, (10) no ability to consent, and (11) participation in another study.
The Institutional Ethics Committee of the University of Leipzig approved the study protocol. All patients gave written informed consent prior to study inclusion. The study conformed to the principles outlined in the Declaration of Helsinki.
Procedural protocol
Early invasive angiography was performed according to standard clinical practice within 72 h. Left ventricular ejection fraction was assessed by contrast ventriculography unless contraindicated. Patients were assigned to percutaneous coronary intervention (PCI) with stent placement, coronary artery bypass graft (CABG) surgery or optimal medical therapy at the discretion of the attending cardiologist. In case of PCI angiographic success was defined as a final angiographic residual stenosis of <20% diameter by visual estimation. Angiographic projections used were those that allowed optimal evaluation of the Thrombolysis in Myocardial Infarction (TIMI) flow of the infarct-related artery. Angiographic analysis included initial and final flows of the culprit vessel, as defined previously [16]. Angiographically visible collateral arteries of the infarct-related artery were graded according to the modified Rentrop classification (grade 0, no visible filling of any collateral channel; grade 1, filling of the side branches of the infarct-related artery; grade 2, partial filling of the epicardial vessel of the infarct-related artery; grade 3, complete collateral filling of the epicardial vessel) [17]. Visual assessments were performed off-line by two experienced interventional cardiologists blinded to clinical parameters, with any disagreements resolved by consensus.
All patients received 500 mg acetylsalicylic acid and unfractionated heparin (60 IU/kg body weight) intravenously immediately after NSTEMI diagnosis with continuous heparin infusion with the target aPTT 50–70 s. Clopidogrel medication was administered as early as possible before invasive angiography at a dose of 600 mg. In addition, a tirofiban high-dose bolus of 25 μg/kg bodyweight and an infusion of 0.15 μg/kg/min intravenously for a period of 24 h were administered to all patients. All patients received 100 mg acetylsalicylic acid per os indefinitely and 75 mg clopidogrel per os once daily for 12 months. All other medication was given at the discretion of the attending physician.
After invasive angiography and in case of PCI the sheath was removed and the puncture site was closed by a closure device or by 12 h gradual compression with a compression system.
Definitions
The physician treating the patient in the catheterization laboratory determined the culprit lesion and reported the segment-level stenosis of the culprit lesion. An occluded lesion was defined as a lesion with 100% stenosis or TIMI-flow grade 0 or 1. An infero- or posterolateral culprit was defined as a lesion in either the circumflex or right coronary artery. An anterior culprit was defined as a lesion in the left anterior descending coronary artery. Angiographically absent collateral arteries were defined as modified Rentrop grades 0 and 1 while angiographically visible collateral arteries were defined as modified Rentrop grades 2 and 3.
Biochemistry
Venous blood samples were taken at admission (baseline), and every 6 h subsequently for a period of 48 h. Creatine kinase (CK) and creatine kinase-MB fraction (CK-MB) were analyzed in these samples. Troponin T (cTNT) was only measured at admission and after 6 h if no elevated Troponin was detected in the baseline blood sample. CK (upper limit of normal 2.78 μmol/L/s for women and 3.17 μmol/L/s for men) and CK-MB (upper limit of normal 0.41 μmol/L/s) were determined enzymatically at 37°C (Access Test Menu®, Beckman Coulter, Brea, USA). Troponin T (threshold 0.03 ng/mL) was measured by an electrochemiluminescence immunoassay (Elecsys Troponin T Assay®, Roche Diagnostics, Grenzach-Wyhlen, Germany).
End points
The clinical primary end point MACE was a composite of death, reinfarctions, and readmission for unstable angina within 30 days or 6 months after inclusion. The diagnosis of death included death from any cause. The diagnosis of reinfarctions was defined as documented myocardial necrosis either in the setting of myocardial ischemia (spontaneous MI) or in the setting of PCI (procedure-related MI) following the recommendations of the Consensus Committee for the definition of MI [18]. The diagnosis of unstable angina pectoris included all hospital admissions due to unstable angina.
Statistical analysis
Data are expressed as mean ± standard deviation and categorical data as number and percent. In order to analyze differences between groups, we used the Pearson Chi-Square test for data in categories. The independent samples t test was used to compare means of parameters between two groups. Analysis of normality was performed by analyzing histograms and QQ plots integrating skewness and kurtosis values, and by Kolmogorov–Smirnov test.
Multivariate logistic regression modeling was used to examine variables associated with an OCA. Only variables showing significant correlation coefficients using Kendall’s rank test were included in the analysis. Variables examined included left ventricular ejection fraction, collateral supply, number of stents, multiple stenting, stent length, TIMI-flow grade after PCI, CK, and CK-MB level at admission, peak CK, and CK-MB level. All variables were entered into the model simultaneously. Validity of the model was assessed with the Hosmer and Lemeshow test. The Nagelkerke R 2 was used to quantify the amount of variation in the outcome variable explained by the model.
Hazard ratios (HR) with 95% confidence intervals (CI) were obtained with Cox proportional hazards models at 30 days and 6 months, including age, sex, diabetes, prior infarction, prior PCI, systolic blood pressure, heart rate, Killip class, presence of multivessel disease, left ventricular dysfunction, type of dominance, and collateral supply as covariates.
For the clinical end point MACE, the Kaplan–Meier method was applied for assessing time to event. Differences were assessed by log-rank test. All probability values were two-sided and a probability level of p < 0.05 was considered significant. All calculations were done with SPSS for Windows® (Version 17.0, SPSS, Chicago, USA).
Results
Patient characteristics
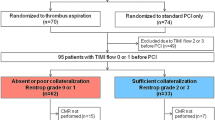
We excluded those patients who had missing data for the variables under consideration (n = 122), or did not receive cardiac catheterization during the same hospital stay (n = 32); 448 of 602 patients remained in the analysis. Comparisons of those included with those excluded showed no marked difference in age (67 vs. 69 years) or sex (67 vs. 63% men). Table 1 summarizes the baseline clinical characteristics of the included patients. There were no significant differences in age, sex, coronary risk factors, clinical comorbidities, number of narrowed coronary arteries and medications between the two groups at baseline. However, metformin was significantly more often taken by patients with OCA. The usage of aspirin and clopidogrel was not significantly different in both groups. But in contrast to clopidogrel patients with OCA tended to take less often aspirin upon presentation.
Incidence and distribution of culprit lesions
The angiograms revealed OCA in 130 (29%) of 448 patients. Culprit lesions were seen in the left anterior descending coronary artery, left circumflex coronary artery, and right coronary artery in 28, 31, and 41% of patients with OCA and in 52, 25, and 23% of patients with non-OCA.
The type of dominance in patients with an OCA was most often right-dominant with no significant difference in comparison with patients with non-occluded culprit (74 vs. 70%, p = 0.73). The culprit artery supplied the infero- or posterolateral territory in 242 patients (54%). Patients with OCA showed more often infero- or posterolateral culprit than patients with non-OCA (75 vs. 53%, p < 0.001). But in patients with infero- or posterolateral occluded culprit the frequency of the right-dominant type was similar to that of patients with anterior occluded culprit (73 vs. 76%, p = 0.76).
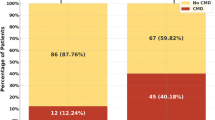
Comparison of occluded versus non-OCA
Procedural characteristics are shown in Table 2. There were no significant differences in hemodynamics or signs of heart failure between the two groups. Besides similar periods of symptom onset to study enrollment in both groups’ patients with OCA had significantly higher levels of CK and CK-MB on hospital admission in comparison with patients with non-OCA. During hospitalization, patients with OCA developed significantly higher peak levels of CK and CK-MB and showed lower left ventricular ejection fractions. Levels of CK-MB in both groups were highest at 6 h after admission and steadily declined thereafter. Time from study enrollment to revascularization was similar in both groups. Well-developed collaterals were significantly more frequent in patients with OCA. Patients with angiographically visible collateral arteries and OCA had significantly smaller infarcts than patients with angiographically absent collateral arteries and OCA (peak CK 9.4 ± 8.9 vs. 25.4 ± 26.8 μmol/L/s; peak CK-MB 1.5 ± 1.5 vs. 2.9 ± 2.4 μmol/L/s, p < 0.001).
More patients with an OCA were revascularized than patients with non-OCA during hospitalization (89 vs. 78%, p = 0.01). Patients with OCA were more often revascularized by PCI whereas the rate of CABG was similar in both groups (12 vs. 11%, p = 0.62). The number and length of stents were significantly higher in patients with OCA. These patients showed a non-significant trend for a higher drug-eluting stent usage possibly caused by more complex interventions. TIMI-flow after PCI was lower in patients with OCA than non-OCA (Table 2). Nevertheless, the rate of reinterventions in the group with OCA was similar to that in the group with non-OCA during the following 6 months (10 vs. 9%, p = 0.63).
In multivariate logistic regression, baseline variables associated with an OCA included collateral supply (OR 6.14, 95% CI 3.48–10.82, p < 0.001), and TIMI flow grade after PCI (OR 0.30, 95% CI 0.12–0.72, p = 0.01).
Comparison of occluded infero- or posterolateral versus anterior culprit lesion
Within the occluded group, there were no significant differences in baseline characteristics and presenting features between patients with an occluded infero- or posterolateral versus anterior culprit lesion. Both groups presented with similar CK, CK-MB, and cTNT levels, but patients with occluded infero- or posterolateral culprit lesion had significantly higher peak CK and CK-MB levels during hospitalization (Table 3).
Procedural characteristics showed similar time periods from hospital arrival to angiography and extent of coronary artery disease. Percentages of revascularization during index hospitalization were equivalent in both groups. However, patients with occluded infero- or posterolateral culprit lesions underwent bypass surgery more often while patients with occluded anterior culprit lesions received more stents, especially drug-eluting stents. Stents had larger diameter and were longer in this group. Extent of angiographically visible collateral arteries and TIMI-flow grade post PCI were similar in both groups. Although patients with anterior OCA displayed smaller infarcts, left ventricular ejection fraction during angiography tended to be lower (Table 3).
Clinical outcome
Clinical outcomes at 30-days and 6-months are summarized in Table 4. After multivariate adjustment, MACE at 6 months were significantly higher in patients with an OCA. The rate of MACE was largely driven by its association with non-fatal reinfarctions at 6 months. These non-fatal reinfarctions consisted mainly of procedure-related MIs in both groups. But significantly more procedure-related MIs were seen in patients with OCA than non-OCA (29 vs. 10%, p < 0.001). The unadjusted Kaplan–Meier curves for 6 month MACE for each group are shown in Fig. 1.
Patients with OCA were further stratified into two groups by angiographically visible versus absent collateral arteries. After multivariate adjustment, MACE at 6 months were significantly higher in patients with angiographically absent collateral arteries (HR 1.96, 95% CI 1.02–3.76, p = 0.04). The unadjusted Kaplan–Meier curves for 6 month MACE for these groups are shown in Fig. 2.
Kaplan–Meier curve for unadjusted 6-month MACE in patients with OCA stratified by angiographically visible versus absent collateral arteries. Angiographically visible collateral arteries of the infarct-related artery were graded according to the modified Rentrop classification. p value for overall comparison between groups
Patients with angiographically visible collateral arteries were further stratified into two groups by occluded versus non-occluded culprit arteries. The unadjusted Kaplan–Meier curves for 6-month MACE for these groups are shown in Fig. 3.
Kaplan–Meier curve for unadjusted 6-month MACE in patients with angiographically visible collateral arteries stratified by occluded versus non-occluded culprit arteries. Angiographically visible collateral arteries of the infarct-related artery were graded according to the modified Rentrop classification. p value for overall comparison between groups
Discussion
In the present study approximately one quarter of patients with NSTEMI presented with an OCA. In these patients the occluded culprits were more frequently found in coronary arteries supplying the infero- or posterolateral myocardium than in patients with non-OCA. This study confirmed the results of previous investigators and included several new observations providing a more complete understanding of OCA in patients with NSTEMI [5, 19]. One observation was that the type of dominance in these patients did not have an effect on the incidence and anatomical distribution of OCA.
A second observation was that NSTEMI with OCA treated by an early invasive strategy had a higher 6-month rate of MACE than NSTEMI with non-OCA because more non-fatal reinfarctions, especially procedure-related MIs, occurred in these patients. It is well documented that in patients with ACS, whether STEMI or NSTEMI, early recanalization of the culprit artery soon after the onset of myocardial ischemia is associated with a better immediate and long-term prognosis [20]. A recent overall meta-analysis of studies investigating an early invasive versus a selective invasive approach at 5-year follow-up showed a sustained reduction in the rate of death using an early invasive strategy in patients with NSTEMI. The largest absolute benefit was observed in patients with higher baseline risk [21]. Despite performing an early invasive strategy in our study, the 6-month outcome of NSTEMI associated with a selective invasive strategy of OCA in a study by Wang et al. [5] was better than that found in our study. Potential explanations were the older age and the higher rates of diabetes of our patients indicating a higher risk of future events [22, 23]. The ICTUS (Invasive vs. Conservative Treatment in Unstable Coronary Syndromes) trial showed that outcome associated with an early invasive strategy in NSTEMI was primarily driven by an early increase in procedure-related MIs as seen in our study [24]. A similar long-term outcome to that of our study was seen in both arms of the TIMACS (Timing of Intervention in Acute Coronary Syndrome) study, which also included NSTEMI with moderate-to-high risk and performed an early versus deferred invasive strategy [25].
Notably, a recent study demonstrated that in patients with moderate- to high-risk NSTEMI, a strategy of immediate intervention compared with a strategy of intervention deferred to the next working day (mean, 21 h) did not result in a difference in infarct size as defined by peak troponin level [26]. Contrary to these results, our data underline that infarcts were larger in patients with NSTEMI and OCA as compared with non-OCA despite a similar delay from hospital arrival to angiography. We did not follow-up infarct size and left ventricular ejection fraction at 6 months, but Grenne et al. [27] showed that patients with NSTEMI due to acute OCA suffered larger infarct size and impaired long-term left ventricular function compared with NSTEMI patients with non-OCA. Previous studies reported that the presence of coronary collateral vessels at the onset of infarction is associated with a limitation of infarct size [7, 11]. Of note, our observation that among patients with OCA those with well-developed collaterals displayed smaller infarcts than those with angiographically absent collateral arteries further substantiates the influence of angiographically visible collateral arteries on infarct size.
The final observation was that patients with OCA and angiographically visible collateral arteries have better long-term outcomes than patients with OCA and angiographically absent collateral arteries. The outcomes in patients with OCA and angiographically visible collateral arteries were even similar to those with non-OCA. A protective effect of coronary collateral arteries on myocardial tissue in patients with recent myocardial infarction or with stable coronary artery disease has also been previously demonstrated [28, 29]. In patients with NSTEMI and early invasive treatment strategy the higher incidence of non-fatal reinfarctions after recanalization in the group with OCA may be influenced by collateral blood flow at baseline angiography. Our data showed that angiographically visible collateral arteries at baseline angiography were associated with a lower rate of MACE and non-fatal reinfarctions in patients with NSTEMI and acute OCA. It has been shown that recanalization of a chronically occluded artery is associated with a rapid regression of the functional collateral vessels during follow-up angiography and collaterals are not readily recruitable in the case of acute reocclusion [30]. We assume that the same applied to an artery recanalized after an acute occlusion. In patients with angiographically absent collateral arteries at baseline angiography abrupt reocclusions after recanalization may cause more extensive infarction, because only a minority of patients will have sufficient and immediately recruitable collaterals in such cases. Several studies showed that the reocclusion of the recanalized occluded infarct-related artery by PCI is not infrequent [31, 32]. Furthermore, the extent of microvascular obstruction in the infarct territory of an acute OCA may be smaller in patients with significant collaterals. We recently demonstrated that well-developed collaterals before reperfusion by PCI in patients with STEMI were associated with a protective effect on coronary microcirculation. A strong trend toward a lower rate of death and non-fatal reinfarctions could be seen in these patients [11]. The investigators of the Occluded Artery Trial recently reported in patients with subacute STEMI and persistent OCA that the higher the extent of collateral blood flow, the lower the rate of death and severe heart failure; but no effect was observed on the incidence of reinfarctions. However, after multivariate adjustment for various baseline characteristics, collateral flow was not an independent predictor of clinical outcome [14].
Confoundings could also have arisen from limitations of this study. One limitation of our study was that culprit lesion locations were determined by the treating cardiologist in the catheter laboratory. Independent adjustment was not performed and therefore confounding bias may result especially among patients with multivessel disease. Another limitation of the study was that the present study examined collateral vessels detected by angiography, which is typically limited to arteries >100 μm in diameter. Newer and more quantifiable methods of collateral assessment, such as pressure- and Doppler-derived collateral flow index, may be more sensitive for detection of recruitable blood flow during arterial occlusion [33–35]. Of note, the original Rentrop score is only applicable in case of total coronary occlusions and contrast injection into the contralateral artery, which has not been performed in the present study. This may have led to an underestimation of collateralization in the group without OCA. However, a recent study showed that the collateral pressure and flow in infarctions with total coronary occlusion correlated with angiographic collateral grade. The Rentrop classification was valid in MI patients with OCA [36]. A third limitation of our study was that ECG leads V7-9 were not routinely collected at admission. STEMI may have been misclassified as NSTEMI in some patients and the incidence of OCA among NSTEMI may have been overestimated.
In conclusion, this study showed that patients with OCA had larger infarcts and worse long-term outcome, compared with patients with non-OCA largely driven by a higher rate of non-fatal reinfarctions. Well-developed collaterals were associated with improvement of outcome in patients with OCA. These findings imply that significant collaterals in patients with NSTEMI and OCA may limit immediate myocardial damage.
Abbreviations
- ACE:
-
Angiotensin-converting enzyme
- ACS:
-
Acute coronary syndrome
- CABG:
-
Coronary arteries bypass graft
- CI:
-
Confidence interval
- CK:
-
Creatine kinase
- CK-MB:
-
Creatine kinase-myocardial band fraction
- cTNT:
-
Troponin T
- ECG:
-
Electrocardiogram
- HR:
-
Hazard ratio
- MACE:
-
Major adverse cardiovascular events
- MI:
-
Myocardial infarction
- NSTEMI:
-
Non-ST-segment elevation myocardial infarction
- OCA:
-
Occluded culprit artery
- PCI:
-
Percutaneous coronary intervention
- STEMI:
-
ST-segment elevation myocardial infarction
- TIMI:
-
Thrombolysis in myocardial infarction
References
Van de Werf F, Bax J, Betriu A, Blomstrom-Lundqvist C, Crea F, Falk V, Filippatos G, Fox K, Huber K, Kastrati A, Rosengren A, Steg PG, Tubaro M, Verheugt F, Weidinger F, Weis M, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Aguirre FV, Al-Attar N, Alegria E, Andreotti F, Benzer W, Breithardt O, Danchin N, Mario CD, Dudek D, Gulba D, Halvorsen S, Kaufmann P, Kornowski R, Lip GYH, Rutten F (2008) Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation. Eur Heart J 29(23):2909–2945
Bassand J-P, Hamm CW, Ardissino D, Boersma E, Budaj A, Fernández-Avilés F, Fox KAA, Hasdai D, Ohman EM, Wallentin L, Wijns W, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Filippatos G, Kristensen SD, Widimsky P, McGregor K, Sechtem U, Tendera M, Hellemans I, Gomez JLZ, Silber S, Funck-Brentano C, Andreotti F, Benzer W, Bertrand M, Betriu A, DeSutter J, Falk V, Ortiz AF, Gitt A, Hasin Y, Huber K, Kornowski R, Lopez-Sendon J, Morais J, Nordrehaug JE, Steg PG, Thygesen K, Tubaro M, Turpie AGG, Verheugt F, Windecker S (2007) Guidelines for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes. Eur Heart J 28(13):1598–1660
Bonzel T, Erbel R, Hamm CW, Levenson B, Neumann F-J, Rupprecht H-J, Zahn R (2008) Percutaneous coronary intervention (PCI). Clin Res Cardiol 97(8):513–547
Krishnaswamy A, Lincoff AM, Menon V (2009) Magnitude and consequences of missing the acute infarct-related circumflex artery. Am Heart J 158(5):706–712
Wang TY, Zhang M, Fu Y, Armstrong PW, Newby LK, Gibson CM, Moliterno DJ, FVd Werf, White HD, Harrington RA, Roe MT (2009) Incidence, distribution, and prognostic impact of occluded culprit arteries among patients with non-ST-elevation acute coronary syndromes undergoing diagnostic angiography. Am Heart J 157(4):716–723
Hirai T, Fujita M, Nakajima H, Asanoi H, Yamanishi K, Ohno A, Sasayama S (1989) Importance of collateral circulation for prevention of left ventricular aneurysm formation in acute myocardial infarction. Circulation 79(4):791–796
Habib G, Heibig J, Forman S, Brown B, Roberts R, Terrin M, Bolli R (1991) Influence of coronary collateral vessels on myocardial infarct size in humans. Results of phase I thrombolysis in myocardial infarction (TIMI) trial. The TIMI Investigators. Circulation 83(3):739–746
Kodama K, Kusuoka H, Sakai A, Adachi T, Hasegawa S, Ueda Y, Mishima M, Hori M, Kamada T, Inoue M, Hirayama A (1996) Collateral channels that develop after an acute myocardial infarction prevent subsequent left ventricular dilation. J Am Coll Cardiol 27(5):1133–1139
Elsman P, van `t Hof AWJ, de Boer MJ, Hoorntje JCA, Suryapranata H, Dambrink JHE, Zijlstra F (2004) Role of collateral circulation in the acute phase of ST-segment-elevation myocardial infarction treated with primary coronary intervention. Eur Heart J 25(10):854–858
Ishihara M, Inoue I, Kawagoe T, Shimatani Y, Kurisu S, Hata T, Mitsuba N, Kisaka T, Nakama H, Kijima Y (2005) Comparison of the cardioprotective effect of prodromal angina pectoris and collateral circulation in patients with a first anterior wall acute myocardial infarction. Am J Cardiol 95(5):622–625
Desch S, Eitel I, Schmitt J, Sareban M, Fuernau G, Schuler GC, Thiele H (2009) Effect of coronary collaterals on microvascular obstruction as assessed by magnetic resonance imaging in patients with acute ST-elevation myocardial infarction treated by primary coronary intervention. Am J Cardiol 104(9):1204–1209
Perez-Castellano N, Garcia E, Abeytua M, Soriano J, Serrano J, Elizaga J, Botas J, Lopez-Sendon J, Delcan J (1998) Influence of collateral circulation on in-hospital death from anterior acute myocardial infarction. J Am Coll Cardiol 31(3):512–518
Antoniucci D, Valenti R, Moschi G, Migliorini A, Trapani M, Santoro GM, Bolognese L, Cerisano G, Buonamici P, Dovellini EV (2002) Relation between preintervention angiographic evidence of coronary collateral circulation and clinical and angiographic outcomes after primary angioplasty or stenting for acute myocardial infarction. Am J Cardiol 89(2):121–125
Steg PG, Kerner A, Mancini GBJ, Reynolds HR, Carvalho AC, Fridrich V, White HD, Forman SA, Lamas GA, Hochman JS, Buller CE, for the OAT Investigators (2010) Impact of collateral flow to the occluded infarct-related artery on clinical outcomes in patients with recent myocardial infarction: a report from the randomized occluded artery trial. Circulation 121(25):2724–2730
Desch S, de Waha S, Eitel I, Koch A, Gutberlet M, Schuler GC, Thiele H (2010) Effect of coronary collaterals on long-term prognosis in patients undergoing primary angioplasty for acute ST-elevation myocardial infarction. Am J Cardiol 106(5):605–611
Study Group TIMI (1985) The thrombolysis in myocardial infarction (TIMI) trial. Phase I findings. N Engl J Med 312(14):932–936
Rentrop K, Cohen M, Blanke H, Phillips R (1985) Changes in collateral channel filling immediately after controlled coronary artery occlusion by an angioplasty balloon in human subjects. J Am Coll Cardiol 5(3):587–592
Thygesen K, Alpert JS, White HD, on behalf of the Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction (2007) Universal definition of myocardial infarction. Circulation 116(22):2634–2653
Abbott JD, Ahmed HN, Vlachos HA, Selzer F, Williams DO (2007) Comparison of outcome in patients with ST-elevation versus non-ST-elevation acute myocardial infarction treated with percutaneous coronary intervention (from the National Heart, Lung, and Blood Institute Dynamic Registry). Am J Cardiol 100(2):190–195
Müller UM, Eitel I, Eckrich K, Erbs S, Linke A, Möbius-Winkler S, Mende M, Schuler GC, Thiele H (2010) Impact of minimising door-to-balloon times in ST-elevation myocardial infarction to less than 30 min on outcome: an analysis over an 8-year period in a tertiary care centre. Clin Res Cardiol. doi:10.1007/s00392-010-0242-7
Fox KAA, Clayton TC, Damman P, Pocock SJ, de Winter RJ, Tijssen JGP, Lagerqvist B, Wallentin L, for the FIR Collaboration (2010) Long-term outcome of a routine versus selective invasive strategy in patients with non-ST-segment elevation acute coronary syndrome: a meta-analysis of individual patient data. J Am Coll Cardiol 55(22):2435–2445
van Miltenburg-van Zijl A, Simoons M, Veerhoek R, Bossuyt P (1995) Incidence and follow-up of Braunwald subgroups in unstable angina pectoris. J Am Coll Cardiol 25(6):1286–1292
Calvin JE, Klein LW, VandenBerg BJ, Meyer P, Condon JV, Snell RJ, Ramirez-Morgen LM, Parrillo JE (1995) Risk stratification in unstable angina: prospective validation of the Braunwald Classification. JAMA 273(2):136–141
Damman P, Hirsch A, Windhausen F, Tijssen JGP, de Winter RJ, for the ICTUS Investigators (2010) 5-year clinical outcomes in the ICTUS (invasive versus conservative treatment in unstable coronary syndromes) trial: a randomized comparison of an early invasive versus selective invasive management in patients with non-ST-segment elevation acute coronary syndrome. J Am Coll Cardiol 55(9):858–864
Mehta SR, Granger CB, Boden WE, Steg PG, Bassand J-P, Faxon DP, Afzal R, Chrolavicius S, Jolly SS, Widimsky P, Avezum A, Rupprecht H-J, Zhu J, Col J, Natarajan MK, Horsman C, Fox KAA, Yusuf S, the TIMACS Investigators (2009) Early versus delayed invasive intervention in acute coronary syndromes. N Engl J Med 360(21):2165–2175
Montalescot G, Cayla G, Collet J-P, Elhadad S, Beygui F, Le Breton H, Choussat R, Leclercq F, Silvain J, Duclos F, Aout M, Dubois-Rande J-L, Barthelemy O, Ducrocq G, Bellemain-Appaix A, Payot L, Steg P-G, Henry P, Spaulding C, Vicaut E, for the ABOARD Investigators (2009) Immediate vs delayed intervention for acute coronary syndromes: a randomized clinical trial. JAMA 302(9):947–954
Grenne Br, Eek C, Sjoli B, Dahlslett T, Uchto M, Hol PK, Skulstad H, Smiseth OA, Edvardsen T, Brunvand H (2010) Acute coronary occlusion in non-ST-elevation acute coronary syndrome: outcome and early identification by strain echocardiography. Heart 96(19):1550–1556
Sabia PJ, Powers ER, Ragosta M, Sarembock IJ, Burwell LR, Kaul S (1992) An association between collateral blood flow and myocardial viability in patients with recent myocardial infarction. N Engl J Med 327(26):1825–1831
Meier P, Gloekler S, Zbinden R, Beckh S, de Marchi SF, Zbinden S, Wustmann K, Billinger M, Vogel R, Cook S, Wenaweser P, Togni M, Windecker S, Meier B, Seiler C (2007) Beneficial effect of recruitable collaterals: a 10-year follow-up study in patients with stable coronary artery disease undergoing quantitative collateral measurements. Circulation 116(9):975–983
Werner GS, Emig U, Mutschke O, Schwarz G, Bahrmann P, Figulla HR (2003) Regression of collateral function after recanalization of chronic total coronary occlusions: a serial assessment by intracoronary pressure and doppler recordings. Circulation 108(23):2877–2882
Dzavik V, Buller CE, Lamas GA, Rankin JM, Mancini GBJ, Cantor WJ, Carere RJ, Ross JR, Atchison D, Forman S, Thomas B, Buszman P, Vozzi C, Glanz A, Cohen EA, Meciar P, Devlin G, Mascette A, Sopko G, Knatterud GL, Hochman JS, for the TOSCA-2 Investigators (2006) Randomized trial of percutaneous coronary intervention for subacute infarct-related coronary artery occlusion to achieve long-term patency and improve ventricular function: the Total Occlusion Study of Canada (TOSCA)-2 Trial. Circulation 114(23):2449–2457
Steg PG, Thuaire C, Himbert D, Carrié D, Champagne S, Coisne D, Khalifé K, Cazaux P, Logeart D, Slama M, Spaulding C, Cohen A, Tirouvanziam A, Montély J-M, Rodriguez R-M, Garbarz E, Wijns W, Durand-Zaleski I, Porcher R, Brucker L, Chevret S, Chastang C (2004) DECOPI (DEsobstruction COronaire en Post-Infarctus): a randomized multi-centre trial of occluded artery angioplasty after acute myocardial infarction. Eur Heart J 25(24):2187–2194
Pijls N, Bech G, el Gamal M, Bonnier H, De Bruyne B, Van Gelder B, Michels H, Koolen J (1995) Quantification of recruitable coronary collateral blood flow in conscious humans and its potential to predict future ischemic events. J Am Coll Cardiol 25(7):1522–1528
Wahl A, Billinger M, Fleisch M, Meier B, Seiler C (2000) Quantitatively assessed coronary collateral circulation and restenosis following percutaneous revascularization. Eur Heart J 21(21):1776–1784
Billinger M, Kloos P, Eberli FR, Windecker S, Meier B, Seiler C (2002) Physiologically assessed coronary collateral flow and adverse cardiac ischemic events: a follow-up study in 403 patients with coronary artery disease. J Am Coll Cardiol 40(9):1545–1550
Meisel SR, Shochat M, Frimerman A, Asif A, Blondheim DS, Shani J, Rozenman Y, Shotan A (2010) Collateral pressure and flow in acute myocardial infarction with total coronary occlusion correlate with angiographic collateral grade and creatine kinase levels. Am Heart J 159(5):764–771
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bahrmann, P., Rach, J., Desch, S. et al. Incidence and distribution of occluded culprit arteries and impact of coronary collaterals on outcome in patients with non-ST-segment elevation myocardial infarction and early invasive treatment strategy. Clin Res Cardiol 100, 457–467 (2011). https://doi.org/10.1007/s00392-010-0269-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-010-0269-9