Abstract
Aim
To evaluate changes of right ventricular (RV) parameters in follow-up examinations after corrected tetralogy of Fallot (TOF) by cardiac magnetic resonance (CMR).
Methods
CMR was performed twice within 4 years in 45 patients using a 1.5 T scanner. RV-volumes and pulmonary-regurgitant-fractions (PRF) were calculated from standard cine-sequences and flow-sensitive gradient-echo images, respectively. Patients were divided into two groups depending on the post-operative (po) interval (group 1 ≤5 years po; group 2 >5 years po) and subgroups depending on type of surgery (transannular vs. non-transannular). Patient groups were compared among each other and differences between 1st and 2nd CMR were assessed. Furthermore, patients were compared with 25 healthy volunteers.
Results
Compared with controls RV-size was increased (group 1: p = 0.007; group 2: p < 0.001) and RV function decreased (group 1: p = 0.02; group 2: p < 0.001) in po TOF-patients. PRF was higher in group 2 compared with group 1 (p = 0.04) and significant changes of PRF between 1st and 2nd CMR were found in group 2 (p < 0.01), but not in group 1 (p = 0.29). Compared with the non-transannular subgroup, PRF (p < 0.001) and RV end-diastolic-volume index (RV-EDVI) (p = 0.03) were significantly higher in patients with a transannular patch, EDVI increased between 1st and 2nd CMR. After correction, no significant changes of RV myocardial mass index (RV-MMI) were found.
Conclusion
After correction of TOF, RV-size, RV-muscle mass (RV-MM) was increased and ejection fraction decreased in “early” follow-up already. Whereas these parameters can remain stable over a long time period, the PRF significantly increased in “late” follow-up dependent on the po interval. Overall, transannular patching went along with higher PRF and bigger RV-size as well as a greater dynamic of these parameters in the time course, which makes this subgroup highly in need of regular follow-up examinations for the optimal timing of re-interventions. In contrast, the increased RV-MM demonstrated no regression po.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prognosis after surgical repair of tetralogy of Fallot (TOF) has improved significantly due to advances in cardiovascular diagnosis and surgical therapy in the recent decades resulting in a large number of patients reaching adulthood [1, 2]. Nevertheless, complete repair, particularly in the right ventricular outflow tract, may not be achieved in all patients leading to an increased incidence of long-term cardiac morbidities. Residual pulmonary regurgitation (PR), especially in transannular patching, leads to RV volume overload and ventricular dilatation as well as QRS-prolongation, which puts these patients on increased risk for right-sided heart failure, ventricular arrhythmia and sudden cardiac death [3, 4].
Long-lasting volume overload of the RV caused by PR does not only affect right ventricular function, but also the interventricular interaction and left ventricular performance [5–8].
Acquisition of volumetric and functional parameters is therefore crucial in routine follow-up examinations and early detection of changes can avoid major clinical complications. As cardiac magnetic resonance (CMR) is an excellent method to obtain these data with high accuracy, low variability and without radiation exposure [9–15]; it is performed routinely since the mid-1990s for this indication.
In the present study, our aim was
-
1.
to describe the development of RV dilatation and RV dysfunction in a longitudinal section
-
2.
to analyze whether there are important changes of volumes and function even early after correction and
-
3.
to compare data of TOF patients with a group of age-matched controls
Methods
Patient population
Forty-five patients (27 males, 18 females) after surgical repair of TOF undergoing quantitative assessment of right heart function and degree of regurgitation over the right ventricular outflow tract were included in this study. All patients came for regular outpatient visits to our tertiary care center. Evaluation of ventricular volume and function as well as the degree of pulmonary regurgitation was performed using a 1.5 T MR scanner (Gyroscan, Philips).
In this cohort each patient was examined twice within a period of follow-up time of 4 years. Patients with common contraindications for MR like a permanent pacemaker/ICD or intracranial metallic implants were excluded. Furthermore patients with a relevant pulmonary stenosis of >2.5 m/s flow velocity in the RVOT/pulmonary trunk were excluded from the study to avoid bias of the obstructive component.
Patients were divided into two groups depending on time between surgical repair and first CMR examination:
-
Group 1: ≤5 years after surgery = “early” follow-up group; mean po interval 4.5 ± 0.13 years
-
Group 2: >5 years after surgery = “late” follow-up group; mean po interval 16.5 ± 1.1 years
Changes in cardiac parameters between first and second CMR were compared in each group (within-group comparison) and groups were compared among each other (between-group comparison). We created subgroups in regard to the used surgical method, i.e., transannular versus non-transannular repair.
Furthermore, the CMR data of patients after TOF repair were compared with an age-matched group of 25 healthy volunteers.
This study complies with the declaration of Helsinki and was approved by the local ethics committee. All patients or parents had given their informed consent before the examination.
Measurement of cardiac volumes and masses
All CMR examinations were performed on a 1.5 T scanner (Gyroscan ACS-NT, Philips Medical Systems, Best, The Netherlands) with a five-channel phased-array surface coil in supine position.
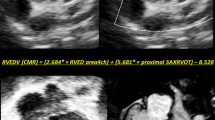
For the assessment of right ventricular volumes and masses, a breath hold or respiratory gated cine-SSFP sequence with retrospective ECG-gating in a short axis orientation perpendicular to the interventricular septum was performed. Thirty phases were acquired per heart cycle. TE was 1.8 ms, TR 3.6 ms, flip angle 50°, matrix size 256 × 128, slice thickness 6 mm, inter-slice gap 0 mm. Typical in plane spatial resolution was 1.2 × 1 mm. Endocardial and epicardial borders were manually traced in end-systole and end-diastole in each slice (Fig. 1).
Short axis view of the heart of a 4-year-old boy after transannular correction of TOF in a end-systole and b end-diastole. By manually tracing the endocardial and epicardial borders of each slice the ventricular volumes and the myocardial mass can be calculated. Determination of RV myocardial mass was performed in end-diastole for a better visualization of the compact myocardial layer. Trabeculations were excluded. Note the aneurysm of the right ventricular outflow tract that shows a dyskinesia in systole (white arrows) due to the creation of a transannular patch. Also note the straightening of the interventricular septum, which is a sign of volume overload of the right ventricle (black arrows). Ellipse right ventricular outflow tract, star right ventricle, triangle left ventricle
Volumes were obtained by Simpson’s rule [16] according to the protocol of the German Competence Network of Congenital heart disease [17]. All parameters were related to body surface and shown as indices. We determined right ventricular end-diastolic volume index (RV-EDVI), end-systolic volume index (RV-ESVI), stroke-volume index (RV-SVI) as well as right ventricular myocardial mass index (RV-MMI). Furthermore, we calculated right ventricular ejection fraction (RV-EF).
CMR-flow measurement
CMR phase contrast flow measurement to measure pulmonary regurgitant fraction (PRF) was performed with a flow-sensitive gradient echo sequence in a perpendicular orientation (“through plane”) cranial to the pulmonary valve and below the pulmonary bifurcation. Flow velocity and flow volumes were quantified. Encoded velocity (Venc) was 200 cm/s. In case of aliasing, we increased Venc in steps of 25 cm/s. The acquisition was performed during free breathing using a sequence with retrospective gating to cover the whole heart cycle (TE 6.1–6.4 ms, TR 20 ms, flip angle 20°, matrix size 96 × 256).
Statistical analysis
A Kolmogorov–Smirnov test was used to test for normality. Data were given as means ± SD when distribution was Gaussian and medians and ranges when not normally distributed. For comparison between groups an unpaired t test or a Mann–Whitney Test was performed depending on distribution. For comparison between first and second CMR within one group (within-group comparison) a paired t test or Wilcoxon test was performed. A probability value less than 0.05 was considered statistically significant. All data were analyzed with SPSS version 12 (SPSS Inc.).
Results
Distribution of patient and control group parameters is summarized in Table 1.
Patient and control group demographics
Patient characteristics are presented in Table 2. The control group consisted of 13 female and 12 male volunteers with a mean age of 18.5 ± 6.9 SD years and matched to the age of our patient group.
In ten patients, the first CMR examination was performed ≤5 years po (group 1 = “early” follow-up), in 35 patients >5 years after correction (group 2 = “late” follow-up). Reliable information on the used surgical technique for reconstruction of the right ventricular outflow tract was available in 38 patients; in group 1 a transannular patch was used in 8 (80%), a non-transannular approach in one patient. In group 2, 21 patients (60%) received a transannular and 8 a non-transannular repair. All patients in group 1 underwent surgical correction in the 1990s. Dates of correction in group 2 ranged from 1974 to 1995. Two patients demonstrated with NYHA grade III and all other patients with NYHA grade I or II.
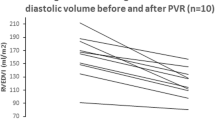
Time course of right ventricular volumetric and functional parameters
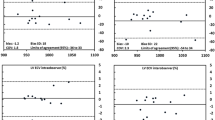
In 1st CMR, RV end-diastolic volume index (RV-EDVI) was significantly higher in both patient groups compared with controls (p = 0.007 for group 1; p < 0.001 for group 2, means ± SD, see Table 1). Furthermore, group 2 (mean 105.4 ± 27.2 SD ml/m²) showed a tendency of higher RV-EDVI compared with group 1 (mean 93.8 ± 26.9 SD ml/m²) without reaching significance (p = 0.25, Fig. 2). There was an increase of RV-EDVI between 1st and 2nd CMR only in the subgroup with transannular patching (1st CMR: mean 108.9 ± 22.1 SD ml/m², 2nd CMR: mean 123.0 ± 25.7 SD ml/m²; p = 0.001, Fig. 3), but not in the non-transannular subgroup (1st CMR: mean 89.5 ± 31.7 ml/m², 2nd CMR: mean 103.2 ± 27.5 ml/m²; p = 0.29). Three patients, all group 2, exceeded an RV-EDVI of >150 ml/m². Two of these patients demonstrated impaired right ventricular ejection fraction <40%, only one though with clinical symptoms of heart failure grade NYHA III. In four patients CMR results and clinical evaluation resulted in pulmonary valve replacement.
RV end-systolic volume index (RV-ESVI) demonstrated a significant increase in group 1 (mean 48.3 ± 19.3 SD ml/m²; p < 0.001) and group 2 (mean 53.4 ± 19.2 SD ml/m²; p < 0.001) compared with the control group (mean 31.1 ± 5.9 SD ml/m²).
RV stroke volume index (RV-SVI) showed no differences between patient groups (group 1: mean 45.5 ± 17.1 SD ml/m², group 2: mean 49.5 ± 14.6 SD ml/m²; p = 0.46). As a consequence, although significantly decreased compared with controls (medians ± IQR, see Table 1; p for group 1 = 0.017, p for group 2 < 0.001) also right ventricular EF did not change, neither between patient groups (medians ± IQR, see Table 1; p = 0.58, Fig. 4) nor between 1st and 2nd CMR in both groups (medians ± IQR, see Table 1; p = 0.88 for group 1, p = 0.42 for group 2).
Pulmonary regurgitant fraction was higher in group 2 compared with group 1 (median 27.5 ± 22.0 IQR ml/m² vs. median 18.5 ± 11.7 IQR ml/m²; p = 0.04). While there was no difference between 1st and 2nd CMR within group 1 (medians and IQR, see Table 1; p = 0.29), we found an increase of PRF between 1st and 2nd CMR within group 2 (medians and IQR, see Table 1; p < 0.001). There was also a significant increase between 1st and 2nd CMR within the transannular subgroup independent of the affiliation of patients to group 1 or group 2 (1st CMR: median 31.5 ± 12.2 IQR%, 2nd CMR: median 39.5 ± 12.8 IQR%; p < 0.001). No changes were found in the non-transannular subgroup (Fig. 5).
Compared with controls both patient groups showed a significantly higher RV myocardial mass index (group 1 median 34.0 ± 22.7 IQR mg/m², group 2 median 40.2 ± 20.6 IQR mg/m²; p < 0.001 for both groups). There were also no changes between 1st and 2nd CMR within both groups (medians ± IQR, see Table 1).
Discussion
This study confirms the significant deterioration of ventricular volume and function over time in patients with congenital right heart disease and residual defects in form of predominantly pulmonary valve regurgitation. These changes have been found mainly in patients with transannular surgical repair and in a late follow-up period.
Longitudinal studies in post-operative Fallot patients usually focus on changes in RV volume after pulmonary valve replacement [18] or clinical long-term outcome. To our knowledge, this is the first study that describes the changes of volumetric and functional parameters as well as pulmonary regurgitation of two consecutive CMR examinations in a relatively large group of patients after surgical repair of TOF.
The clinical utility of CMR in follow-up examinations after correction of TOF was emphasized recently [19], and gradient echo cine-CMR is the most accurate imaging modality to determine right and left ventricular volumes and function [20–22]. Furthermore, CMR phase contrast flow measurement is the ideal method to quantify PRF non-invasively [23, 24].
Time course of RV size and pulmonary regurgitation
Right ventricular enlargement is a common finding in patients after surgical repair of TOF. Several studies showed an increase of RV-EDVI in follow-up examinations, but most studies obtained single volumetric parameters in late follow-up examinations only, so it remained unclear when the process of enlargement starts [25, 26]. Our data show that compared with healthy controls, an increase of RV-EDVI can be found in early follow-up examinations (≤5 years po) already (Fig. 2). The degree of RV enlargement and further dynamics though highly depend on the used surgical method. While RV size can remain stable over a long time when the annular ring remains intact, patients with a transannular patch show an increase of RV size caused by long-standing pulmonary regurgitation, which itself also increases over the years, particularly in late follow-up (>5 years po) and when a transannular patch was used for correction (Fig. 5). Although the percentage of patients with a transannular patch was higher in the early follow-up group (group 1: 80% vs. group 2: 60%), these patients presented with a lower PRF. As all patients of group 1 were corrected in the 1990s, this notable finding might be a result of an improved surgical technique rather than the result of a shorter follow-up period.
We assume that right ventricular enlargement is a multi-factorial process with long-standing pulmonary regurgitation being the major cause late after surgical repair [27], especially in patients with transannular patching. Furthermore, perioperative myocardial injury, insertion of non-contractile materials in the interventricular septum and RVOT may result in scarring and altered contractile myocardial function resulting in RV dilatation in addition to the volume overload in early follow-up (≤5 years po). This assumption has to be confirmed by further studies using delayed enhancement imaging for visualization of scar tissue as soon as possible after correction.
RV enlargement in association with pulmonary regurgitation has been reported to cause major long-term adverse effects as reduced exercise capacity, arrhythmia and sudden cardiac death in patients with predominantly congenital right heart disease [28]. Although the exact timing of PVR in the asymptomatic patient remains controversial, there seems to be an upper threshold for RV size [29, 30]. Three patients of our population exceeded an RV-EDVI of 150 ml/m², which might be irreversible, even after pulmonary valve replacement [31, 32].
A large number of Fallot repairs go along with deterioration of the annular ring to avoid residual stenosis. Our findings are stressing the need of close-meshed CMR follow-up examinations for the exact assessment of RV size and PRF not to miss optimal timing for PVR.
Time course of right ventricular ejection fraction
Compared with controls, RV-EF of our patients was lower in both patient groups (Fig. 4). This corresponds to previous studies, that also showed an impaired RV function in patients after correction of TOF [33]. Apart from pulmonary regurgitation, impaired RV function early after surgical repair may, like early RV enlargement, be explained by additional pre-, intra- or post-operative contributing factors, i.e., scarring. This underlines the presumptions of Niezen et al. [34], who also found reduced RV-EF in a group of 19 children about 9 years after correction of TOF.
Right ventricular function did not show significant changes in within- or between-group comparison, neither in the transannular nor in the non-transannular subgroup. It is believed that an increase of RV-EDVI late after correction can initially be compensated by the Frank–Starling mechanism, as shown by a ventricular stroke volume index, which was increased by trend in late follow-up in our study. This mechanism obviously also works in patients after corrected TOF, even in the late follow-up period and with a high-degree PR in the transannular subgroup.
It remains unclear when and in which particular patients a significant and clinically relevant impairment of RV function starts. For definite determination of the influence of the used surgical technique and age at correction on development of right ventricular function, prospective studies with homogenous patient groups are needed.
Time course of right ventricular myocardial mass
One notable finding of this study was the massive increase of RV mass index of Fallot patients compared with controls. RV hypertrophy was found in both patient groups, even in long-term follow-up, although patients with a relevant pulmonary stenosis were excluded from the study. This indicates that pre-operative hypertrophy does not regress completely in the post-operative course. This finding is in agreement with earlier studies, showing that myocardial cell diameters can regress to some extent, but not entirely after correction of TOF [32, 35], which results in a permanent increase of oxygen demand and might be an additional risk factor for the development of arrhythmias.
Limitations of the study
This is a retrospective analysis of standardized performed CMR in a heterogeneous group of patients after surgical repair of TOF. Due to this fact and the progressive development of technique of TOF surgery our patient group was inhomogeneous regarding age at repair, age at follow-up and the used mode of surgical reconstruction of the RVOT. Also time intervals between CMR examinations were irregular and division of the studied patients had to be performed.
Because of the limited availability of CMR in the past and the difficulties of performing MR examinations in infants there are no CMR examinations directly after surgical correction of TOF. Therefore, the time course of functional parameters can only be judged from initial CMR examinations. This leads to limited statistical power. Further prospective longitudinal studies with homogenous patient groups and defined intervals between CMR are necessary to evaluate the time course and prognostic impact of volumetric and functional parameters after complete correction of tetralogy of Fallot.
Patients with a manifest ventricular tachycardia and an implanted cardioverter/defibrillator had to be excluded from the study. Thus, it was not possible to correlate the obtained parameters with the most interesting subgroup of patients within the meanings of this study.
Conclusion
Alterations of ventricular volumes and function are present in almost every post-operative TOF patient. These changes are not only the result of typical long-term complications like pulmonary regurgitation and resulting ventricular volume overload. There are also early post-operative changes like impaired right ventricular ejection fraction and early RV dilatation, which may be a result of pre- or intra-operative events. Both early and late changes highly depend on the method of surgical correction with a greater dynamic in transannular patching. Apart from transannular versus non-transannular repair there might be a benefit of improved surgical techniques for patients corrected in the 1990s.
Our findings are stressing the need for regular follow-up examinations of RV volume and function after surgical repair of congenital right heart disease such as the TOF. As CMR is the gold standard for the quantification of ventricular volumes and pulmonary regurgitation, this modality should be the imaging tool of choice in follow-up examinations of TOF patients to avoid long-term irreversible major complications.
References
Norgaard MA, Lauridsen P, Helvind M, Pettersson G (1999) Twenty to thirty-seven-year follow-up after repair for tetralogy of Fallot. Eur J Cardiothorac Surg 16(2):125–130
Nollert G, Fischlein T, Bouterwek S, Bohmer C, Dewald O, Kreuzer E, Welz A, Netz H, Klinner W, Reichart B (1997) Long-term results of total repair of tetralogy of Fallot in adulthood: 35 years follow-up in 104 patients corrected at the age of 18 or older. Thorac Cardiovasc Surg 45(4):178–181
Kerst G, Kaulitz R, Sieverding L, Apitz C, Ziemer G, Hofbeck M (2010) Restrictive ventricular septal defect and critical subaortic stenosis in tetralogy of Fallot. Clin Res Cardiol 99(4):247–249
Gatzoulis MA, Balaji S, Webber SA, Siu SC, Hokanson JS, Poile C, Rosenthal M, Nakazawa M, Moller JH, Gilette PC, Redington AN (2000) Risk factors for arrhythmia and sudden cardiac death late after repair of tetralogy of Fallot: a multi-centre study. Lancet 356(9234):975–981
Louie EK, Bieniarz T, Moore AM, Levitsky S (1990) Reduced atrial contribution to left ventricular filling in patients with severe tricuspid regurgitation after tricuspid valvulectomy: a Doppler echocardiographic study. J Am Coll Cardiol 16(7):1617–1624
Lin SS, Reynertson SI, Louie EK, Levitsky S (1994) Right ventricular volume overload results in depression of left ventricular ejection fraction. Implications for the surgical management of tricuspid valve disease. Circulation 90(5 Pt 2):II209–II213
Grothoff M, Spors B, Abdul-Khaliq H, Abd El Rahman MY, Aexi-Meskishvili V, Lange P, Felix R, Gutberlet M (2006) Pulmonary regurgitation is a powerful factor influencing QRS duration in patients after surgical repair of tetralogy of Fallot. A magnetic resonance imaging (MRI) study. Clin Res Cardiol 95(12):643–649
Davlouros PA, Kilner PJ, Hornung TS, Li W, Francis JM, Moon JC, Smith GC, Tat T, Pennell DJ, Gatzoulis MA (2002) Right ventricular function in adults with repaired tetralogy of Fallot assessed with cardiovascular magnetic resonance imaging: detrimental role of right ventricular outflow aneurysms or akinesia and adverse right-to-left ventricular interaction. J Am Coll Cardiol 40(11):2044–2052
Rebergen SA, Chin JG, Ottenkamp J, van der Wall EE, de Roos A (1993) Pulmonary regurgitation in the late post-operative follow-up of tetralogy of Fallot. Volumetric quantitation by nuclear magnetic resonance velocity mapping. Circulation 88(5 Pt 1):2257–2266
Grothoff M, Spors B, Abdul-Khaliq H, Gutberlet M (2008) Evaluation of post-operative pulmonary regurgitation after surgical repair of tetralogy of Fallot: comparison between Doppler echocardiography and MR velocity mapping. Pediatr Radiol 38(2):186–191
Debl K, Djavidani B, Buchner S, Poschenrieder F, Schmid FX, Kobuch R, Feuerbach S, Riegger G, Luchner A (2009) Dilatation of the ascending aorta in bicuspid aortic valve disease: a magnetic resonance imaging study. Clin Res Cardiol 98(2):114–120
Eitel I, Fuernau G, Walther C, Razek V, Kivelitz D, Schuler G, Thiele H (2008) Delayed enhancement magnetic resonance imaging in isolated noncompaction of ventricular myocardium. Clin Res Cardiol 97(4):277–279
Schroeder J, Peterschroeder A, Vaske B, Butz T, Barth P, Oldenburg O, Bitter T, Burchert W, Horstkotte D, Langer C (2009) Cardiac volumetry in patients with heart failure and reduced ejection fraction: a comparative study correlating multi-slice computed tomography and magnetic resonance tomography. Reasons for intermodal disagreement. Clin Res Cardiol 98(11):739–747
Loukanov T, Sebening C, Springer W, Khalil M, Ulmer HE, Hagl M, Gorenflo M (2008) Replacement of valved right ventricular to pulmonary artery conduits: an observational study with focus on right ventricular geometry. Clin Res Cardiol 97(23):169–175
Gutberlet M, Boeckel T, Hosten N, Vogel M, Kuhne T, Oellinger H, Ehrenstein T, Venz S, Hetzer R, Bein G, Felix R (2000) Arterial switch procedure for D-transposition of the great arteries: quantitative evaluation of hemodynamic changes with cine MR imaging and phase-shift velocity mapping-initial experience. Radiology 214(2):467–475
Vogel M, Gutberlet M, Dittrich S, Hosten N, Lange PE (1997) Comparison of transthoracic three-dimensional echocardiography with magnetic resonance imaging in the assessment of right ventricular volume and mass. Heart 78(2):127–130
Beerbaum P, Barth P, Kropf S, Sarikouch S, Kelter-Kloepping A, Franke D, Gutberlet M, Kuehne T (2009) Cardiac function by MRI in congenital heart disease: impact of consensus training on interinstitutional variance. J Magn Reson Imaging 30(5):956–966
van Straten A, Vliegen HW, Lamb HJ, Roes SD, van der Wall EE, Hazekamp MG, de Roos A (2005) Time course of diastolic and systolic function improvement after pulmonary valve replacement in adult patients with tetralogy of Fallot. J Am Coll Cardiol 46(8):1559–1564
Knauth AL, Gauvreau K, Powell AJ, Landzberg MJ, Walsh EP, Lock JE, del Nido PJ, Geva T (2008) Ventricular size and function assessed by cardiac MRI predict major adverse clinical outcomes late after tetralogy of Fallot repair. Heart 94(2):211–216
Pattynama PM, Lamb HJ, van der Velde EA, van der Wall EE, de Roos A (1993) Left ventricular measurements with cine and spin-echo MR imaging: a study of reproducibility with variance component analysis. Radiology 187(1):261–268
Pattynama PM, Lamb HJ, van der Velde EA, van der Geest RJ, van der Wall EE, de Roos A (1995) Reproducibility of MRI-derived measurements of right ventricular volumes and myocardial mass. Magn Reson Imaging 13(1):53–63
Gutberlet M, Abdul-Khaliq H, Grothoff M, Schröter J, Schmitt B, Röttgen R, Lange P, Vogel M, Felix R (2003) Vergleich der transthorakalen 3-D echokardiographie mit der mrt zur bestimmung linksventrikulärer volumina bei patienten mit pathologischer ventrikelgeometrie aufgrund angeborener herzfehler. Fortschr Röntgenstr 175(7):942–951
Lotz J, Meier C, Leppert A, Galanski M (2002) Cardiovascular flow measurement with phase-contrast MR imaging: basic facts and implementation. Radiographics 22(3):651–671
Gutberlet M, Abdul-Khaliq H, Stobbe H, Spors B, Fröhlich M, Knollmann F, Lange P, Hetzer R, Felix R (2001) Einsatz moderner schnittbildverfahren in der diagnostik von herzklappenerkrankungen. Zeitschrift für Kardiologie 90(6):2–12
Helbing WA, Roest AA, Niezen RA, Vliegen HW, Hazekamp MG, Ottenkamp J, de Roos A, van der Wall EE (2002) ECG predictors of ventricular arrhythmias and biventricular size and wall mass in tetralogy of Fallot with pulmonary regurgitation. Heart 88(5):515–519
Abd El Rahman MY, Abdul-Khaliq H, Vogel M, Aexi-Meskishvili V, Gutberlet M, Lange PE (2000) Relation between right ventricular enlargement, QRS duration, and right ventricular function in patients with tetralogy of Fallot and pulmonary regurgitation after surgical repair. Heart 84(4):416–420
Davlouros PA, Karatza AA, Gatzoulis MA, Shore DF (2004) Timing and type of surgery for severe pulmonary regurgitation after repair of tetralogy of Fallot. Int J Cardiol 97(1):91–101
Bouzas B, Kilner PJ, Gatzoulis MA (2005) Pulmonary regurgitation: not a benign lesion. Eur Heart J 26(5):433–439
Frigiola A, Tsang V, Bull C, Coats L, Khambadkone S, Derrick G, Mist B, Walker F, van Doorn C, Bonhoeffer P, Taylor AM (2008) Biventricular response after pulmonary valve replacement for right ventricular outflow tract dysfunction: is age a predictor of outcome? Circulation 118(14Suppl):182–190
Wald RM, Lyseggen E, Oechslin EN, Webb GD, Silversides CK (2009) Variability in surgical referral patterns for pulmonary valve replacement in adults with repaired tetralogy of Fallot. Congenit Heart Dis 4(4):231–238
Therrien J, Siu SC, McLaughlin PR, Liu PP, Williams WG, Webb GD (2000) Pulmonary valve replacement in adults late after repair of tetralogy of Fallot: are we operating too late? J Am Coll Cardiol 36(5):1670–1675
Vliegen HW, van Straten A, de Roos A, Roest AA, Schoof PH, Zwinderman AH, Ottenkamp J, van der Wall EE, Hazekamp MG (2002) Magnetic resonance imaging to assess the hemodynamic effects of pulmonary valve replacement in adults late after repair of tetralogy of Fallot. Circulation 106(13):1703–1707
van Straten A, Vliegen HW, Hazekamp MG, de Roos A (2005) Right ventricular function late after total repair of tetralogy of Fallot. Eur Radiol 15(4):702–707
Niezen RA, Helbing WA, van der Wall EE, van der Geest RJ, Rebergen SA, de Roos A (1996) Biventricular systolic function and mass studied with MR imaging in children with pulmonary regurgitation after repair for tetralogy of Fallot. Radiology 201(1):135–140
Mitsuno M, Nakano S, Shimazaki Y, Taniguchi K, Kawamoto T, Kobayashi J, Matsuda H, Kawashima Y (1993) Fate of right ventricular hypertrophy in tetralogy of Fallot after corrective surgery. Am J Cardiol 72(9):694–698
Acknowledgments
This work was supported in part by a grant of the Bundesministerium für Bildung und Forschung, competence network—congenital heart disease.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Grothoff, M., Hoffmann, J., Lehmkuhl, L. et al. Time course of right ventricular functional parameters after surgical correction of tetralogy of Fallot determined by cardiac magnetic resonance. Clin Res Cardiol 100, 343–350 (2011). https://doi.org/10.1007/s00392-010-0252-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-010-0252-5