Abstract
Background
Reduced glomerular filtration rate (GFR) is strongly associated with reduced survival in patients with chronic heart failure (CHF). Our aim was to determine different pathophysiologic markers that are associated with reduced renal function in CHF.
Methods and results
We studied 86 patients with CHF (58 ± 12 years, 78% male). GFR and renal blood flow (RBF) were determined by 125I-Iothalamate and 131I-Hippuran clearances. Filtration fraction (FF) was calculated. We determined haemoglobin levels, endothelial function, inflammatory status, plasma renin activity (PRA) and N-terminal pro brain natriuretic peptide (NT-proBNP). Urinay albumin excretion (UAE) was measured in 24 h urine. Mean GFR was 74 ± 28 ml/min/1.73 m2. GFR was strongly related to RBF (r = 0.915, P < 0.001), FF (r = 0.546, P < 0.001), but only weakly to endothelial function and PRA. In multivariate analysis, RBF (r = 0.938, P < 0.001), FF (r = 0.786, P < 0.001) and haemoglobin levels (r = −0.520, P < 0.001) were independently associated with GFR. UAE was mainly dependent on RBF (r = −0.401, P < 0.001) and increased exponentially with decreasing RBF. RBF was mainly associated with NT-proBNP (r = −0.561, P < 0.001) and PRA (r = −0.422, P < 0.001).
Conclusion
Reduced GFR is mainly dependent of decreased RBF in patients with CHF. Endothelial function and neurohormonal activation showed only mild associations with GFR. NT-proBNP showed a strong relationship with RBF, and may be used as a marker of reduced renal perfusion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
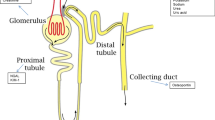
Renal dysfunction has consistently been found to be a strong and independent prognostic factor in patients with chronic heart failure (CHF) [15, 16, 26, 27]. Almost two decades ago, Ljungman et al. [21] showed that renal blood flow (RBF), due to a decreased cardiac output, is the most important determinant of renal function as estimated by reduced glomerular filtration rate (GFR) in CHF patients not on angiotensin converting enzyme (ACE) inhibitors. Generally, in these CHF patients GFR was maintained in spite of reduced RBF by predominant post-glomerular vasoconstriction, as apparent from an elevated filtration fraction (FF).
In the last two decades, drug treatment for CHF has changed with the introduction of ACE-inhibitor, angiotensin II receptor blocker (ARB), and beta-blocker therapy [1, 33]. Considering the effects of ACE-inhibition and ARB therapy on renal afferent and particularly efferent vasomotor tone, it is questionable whether the findings of Ljungman on glomerular hemodynamics still apply to the current CHF population, where all patients are on Renin Angiotensin System-blockade. Evaluation of emerging risk factors show that CHF is not only characterised by impaired hemodynamics, but also endothelial activation [6], atherosclerosis and inflammation [29], neurohormonal activation [2], and sympathetic nervous system activation (SNS) [2, 7]. Furthermore, we recently showed that not only reduced renal perfusion but also venous congestion is an important determinant of renal impairment [8, 9].
The aim of the current study was therefore, first, to determine the relationship of GFR with RBF and FF in CHF patients on current standard therapy, including ACE-inhibitor and/or ARB therapy. Second, we investigate the relative contribution of a number of domain specific biomarkers on indices of renal impairment, to determine easy obtainable markers of renal impairment and potential targets for risk profiling and therapy.
Methods
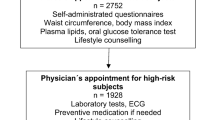
Patient population
Outpatient CHF patients, aged ≥18 years and clinically stable, were asked to participate in this study. Patients were recruited from the outpatient CHF-clinic of the University Medical Center Groningen, The Netherlands. CHF was defined as a left ventricular ejection fraction (LVEF) <45%. Patients were required to be on ACE-inhibitor and/or ARB therapy, and all medication had to be stable for at least 1 month. Administration of medication was not allowed during renal function measurement. Exclusion criteria included stroke or myocardial infarction within the last three months, cardiac surgery or angioplasty within the last 3 months or scheduled to undergo these procedures, unstable angina pectoris, primary renal disease, patients with prior organ transplant, or chronic use of renal function compromising medication. The study protocol was approved by the institutional ethics committee. All patients gave written informed consent. In this study 110 patients were included. Twenty four patients were excluded for this analysis, because of missing haematocrit or urinalysis data. In total 86 patients were eligible for the current analysis.
Study design
On the first day, GFR and RBF were measured by the clearances of Iothalamate and Hippuran. Body weight and length were determined just before renal function measurement started. In addition, during renal measurements, blood pressure and heart rate were determined. Systolic and diastolic blood pressure measurements were calculated as the mean of the last two out of ten consecutive measurements during 10 minutes in sitting position with an automatic Dinamap XL Model 9300 series device (Johnson–Johnson Medical INC, Tampa, Florida). MAP was calculated as 1/3 systolic pressure + 2/3 diastolic pressure.
Renal function measurement by Iothalamate clearance
GFR and effective renal plasma flow (ERPF) were measured by constant infusion of radiolabelled tracers, 125I-Iothalamate and 131I-Hippuran as described before [11]. The body surface area (BSA) was calculated as 0.007184 × weight0.425 × length0.725, and GFR and ERPF were expressed per 1.73 m2 of BSA. Renal blood flow (RBF) was calculated as ERPF/1-haematocrit. The FF was calculated as the ratio of GFR and ERPF and expressed as percentage. GFR and RBF were expressed per 1.73 m2 of BSA. Renal vascular resistance (RVR) was calculated as (MAP/ERPF) × (1-haematocrit) and expressed in mmHg/ml/min.
Cardio-renal (hemodynamic) parameters
RBF, FF, LVEF, MAP and N terminal pro brain natriuretic peptide (NT-proBNP) were used as markers for the cardio-renal hemodynamic status of the patients. LVEF was determined by nuclear ventriculography or echocardiography using Simpsons rule. NT-proBNP was measured by electrochemiluminescence immunoassay on the Roche Elecsys (Roche diagnostics, Netherlands). Peak oxygen consumption (peak VO2 (ml/min/kg)) were extracted from medical records if available.
Renin angiotensin system parameters
Plasma renin activity (PRA) and Angiotensin II (Ang II) were used as markers for renin angiotensin system (RAS) activity. PRA was measured by an immunoradiometric assay (Nichols Institute Diagnostics, Middlesex, United Kingdom). Ang II was measured by specific radioimmunoassays after SepPak extraction of plasma. Analyses were performed in a routine setting according to the guidelines of the manufacturer.
Endothelial function parameters and inflammation
Von Willebrand factor (vWf), plasma nitrite/nitrate (NOx) and asymmetric di-methyl arganine (ADMA), soluble vascular adhesion molecule 1 (sVCAM-1), and soluble E-selectin (sES) were used as markers for endothelial damage and activation. vWF was determined using a validated in-house ELISA, as described previously. NOx was determined in plasma after ultrafiltration through a 10 kDa molecular weight cut-off filter (Millipore BV). A colorimetric assay was used according to the instructions of the manufacturer (Cayman Chemical Company, Ann Abor, MI). ADMA was determined in plasma using a commercially available ELISA kit (DLD diagnostika GmbH, Hamburg, Germany) according to the instructions as supplied by the manufacturer. Serum levels of sVCAM-1 and sES were determined by commercially available ELISA kits (R&D Systems, Abingdon, UK and Bender Med Systems, Vienna, Austria, respectively) according to the manufacturer’s instructions.
High sensitive CRP was (hs-CRP) determined by nephelometry with a threshold of 0.156 mg/l and intra- and inter-assay coefficients of less than 4.4% and 5.7%, respectively (BNII N, Dade Behring, Marburg, Germany). CRP levels below the detection level were scored as 0.156 mg/l.
Urinalysis
Urinary albumin concentrations were determined by nephelometry (Dade Behring Diagnostics, Marburg, Germany). Serum and urine creatinine was determined by Kodak Ektachem dry chemistry (Eastman Kodak, Rochester, NY, U.S.A.). Urinary albumin excretion was determined as the mean of two 24-h urine collections.
The investigation conforms to the principles outlined in the Declaration of Helsinki.
Statistical analyses
Data are given as mean ± standard deviation when normally distributed, as median and interquartile range when skewed distributed, and as frequencies and percentages for categorical variables. Correlations between GFR, RBF, FF and various variables were performed using partial correlation coefficients, adjusted for age and gender. In multivariate analysis, beta coefficients are shown. Non-normally distributed continuous variables were log-transformed. Multivariate stepwise linear regression analysis, including all univariate associated variables (P < 0.10), was used to investigate independent contributions of different variables. In our primary analysis, we investigated the relationships between FF, RBF and GFR. Furthermore, we assessed the relationship between other pathophysiologic variables and GFR. Fractional polynomial modelling was used to visualize the relationship between RBF, RVR, FF, and GFR. In secondary analysis, we investigated the pathophysiologic factors related to the closest determinants of GFR, namely RBF and FF. Finally, again fractional polynomial modelling was used to investigate the possibility of a curvilinear effect between NT-proBNP and RBF. A P value < 0.05 was considered statistically significant. Statistical analyses were performed using SPSS, Chicago version 12.0 and STATA, College Station, Texas, version 9.0.
Results
The baseline characteristics of the 86 patients are presented in Table 1. The studied population consisted of predominantly male patients (78%) with a mean age of 58 ± 12 years. The severity of CHF ranged from NYHA I to IV with an average of 2.3 ± 0.8. All patients received RAS-inhibition (85% ACE-inhibitor). The majority was treated with beta-blockers (86%) and diuretics (65%). Mean LVEF was 27 ± 9% and mean GFR was slightly impaired (74 ± 28 ml/min/1.73 m2).
Relationship of cardiorenal (hemodynamic), endothelial dysfunction and inflammation parameters with GFR
In univariate regression analysis, RBF was the main determinant of GFR (r = 0.888, P < 0.001), accounting for over 80% of the variance in GFR. Also FF (r = 0.573, P < 0.001), RVR (r = −0.707, P < 0.001), and UAE (r = −0.306, P = 0.005) were related to GFR. Curvilinear fitting of RBF, RVR and FF with GFR revealed that the relationship between FF and GFR showed a drop-off in the lower ranges of GFR and RBF (Fig. 1). No early increase in FF was observed with decreasing RBF. FF started to decrease when RBF dropped below approximately 350 ml/min/1.73 m2. RVR showed an exponential increase with decreasing RBF.
Table 2 shows the relationship between GFR and other parameters. Hemodynamic parameters and markers related to GFR included NT-proBNP, MAP and LVEF. Of RAS activity parameters, only PRA showed a strong and significant association with GFR. Endothelial function parameters, including sVCAM-1, vWF and plasma NOx, were moderately associated with GFR. High sensitive-CRP, as a marker of inflammation, did not show any relationship with GFR. In multivariate stepwise linear regression analysis, including all univariate associated variables, only RBF (r = 0.938, P < 0.001), FF (r = 0.786, P < 0.001) and haemoglobin levels (r = −0.520, P < 0.001) remained significant and independent predictors of GFR (adjusted R 2 = 0.953).
RVR was significantly associated with age (r = −0.420, P < 0.001) and gender (r = −0.296, P = 0.006), and by definition with MAP and RBF. In addition, RVR related to VCAM-1 (r = 0.347 P = 0.001), NT-proBNP (r = 0.556, P < 0.001), UAE (r = 0.472, P < 0.001) and haemoglobin levels (r = −0.245, P = 0.025). In multivariate analysis, only UAE (r = 0.375, P < 0.001) and NT-proBNP (r = 0.487, P < 0.001) remained significantly associated with RVR, next to age and gender.
UAE related significantly to RBF (r = −0.282, P = 0.009) and NT-proBNP (r = 0.260, P = 0.016), but not to MAP (r = 0.058, P = 0.593), FF (r = −0.002, P = 0.983), or variables related to endothelial function and inflammation. In multivariate analysis, RBF remained the only significant predictor of UAE (r = 0.401, P < 0.001), next to age and gender. Figure 2 shows the relationship between RBF and UAE.
Relationship of parameters with RBF and FF
All hemodynamic variables, including LVEF (r = 0.400, P < 0.001), MAP (r = 0.315, P = 0.003) and NT-proBNP (r = −0.644, P < 0.001), were significantly related to RBF. In parallel to GFR, only PRA was related to RBF (r = −0.412, P < 0.001), and not angiotensin II levels. Endothelial function parameters showed only weak associations with RBF, with the exception of sVCAM-1 (r = −0.343, P = 0.001). UAE was strongly related to RBF in this analysis (r = −0.401, P < 0.001). In contrast to RBF, of all hemodynamic variables, only MAP was significantly related to FF (r = 0.405, P < 0.001). PRA showed also a relationship with FF (r = −0.371, P = 0.001). Of the endothelial function parameters, only vWF showed a significant association with FF (r = −0.274, P = 0.012).
In multivariate analysis, the combination of NT-proBNP, PRA, sVCAM-1 levels and UAE was able to explain 68% of the variance in RBF. Of all individual parameters, NT-proBNP (r = −0.561, P < 0.001) and PRA (r = −0.422, P < 0.001), were the strongest determinants of RBF (Table 3). The relationship between RBF and NT-proBNP is depicted in Fig. 3. In multivariate analysis, only PRA remained associated with FF (r = −0.371, P < 0.001), but could only predict 12% of the variance in FF.
Discussion
The present study shows that RBF is the most important contributor of GFR in patients with CHF on ACE-inhibition or ARB therapy. Markers of neurohormonal activation and endothelial function showed a less pronounced relationship with GFR. Furthermore, we observed strong relationships between NT-proBNP, PRA and RBF.
Hemodynamics
We observed a parallel decline in GFR with declining RBF. This relationship was the result of a stable FF over almost the full range of RBF. Only in the extreme ranges of hypoperfusion, FF decreased in parallel with decreasing RBF. In contrast to findings by Cody and Ljungman in 34 patients with CHF not on ACE-inhibitor therapy, FF did not increase with reducing RBF [7, 21]. Apparently, this phenomenon represents the effect of ACE-inhibition which blocks the action of angiotensin II on the efferent arteriole. The finding of a disproportionate decrease in FF when RBF is severely reduced is in fact in agreement with hypofiltration that occurs in the absence of ACE-inhibition [21].
The inability to adequately increase or preserve FF can be explained by a combination of three factors: 1) low glomerular plasma flow, 2) low transcappillary hydraulic pressure and 3) reduced ultrafiltration coefficient [7]. We were able to show that reduced RBF is the main contributing factor in the condition of hypofiltration and impaired GFR in CHF patients. SNS activity, which stimulates pre-glomerular vasomotor tone, decreases RBF [12]. However, we did not measure sympathetic activity in our cohort. MAP was related to both RBF and FF in univariate analysis. Especially the latter indicates that with the decrease of FF in the lower regions of RBF, MAP decreased. This suggests that in these patients, hydraulic pressure is in fact reduced, which may be one of the mechanisms by which GFR is reduced.
Furthermore, remarkably we observed that FF decreased in the lower regions of RBF, despite an exponential increase in RVR. Total RVR is determined by both afferent and efferent vascular resistance, whereas FF is predominantly determined by efferent vascular resistance. A higher RVR due to efferent vasoconstriction would be expected to lead to an increase in FF as well, but, apparently, at the higher extreme of RVR this is not the case. Accordingly, this part of the curve is explained by a predominant increase in afferent vascular tone. A very high afferent tone, with consequently a low glomerular perfusion pressure, would require a correspondingly high efferent vascular tone to maintain filtration pressure. The divergence between RVR and FF in patients with severe renal function impairment indicates that in these patients postglomerular tone can no longer be maintained, which might be related to the use of RAS-blockade that is known to blunt efferent vasoconstriction. Thus, the striking increase in RVR is likely to represent strongly increased afferent vasoconstriction. In the light of new therapies in acute heart failure which are targeted at blocking adenosine mediated afferent vasoconstriction, this may indicate a similar pathophysiologic mechanism for reduced GFR in CHF [13]. This is further supported by similar effects of adenosine blockade in the presence of RAS blockade in either animal models of renal hypoxia or patients with CHF [10, 25], although in the latter only 59% were on RAS blocking therapy. We recently showed that also venous congestion as estimated by increased central venous pressure, may be an important determinant of GFR, especially in the condition of an impaired RBF [8, 9]. The observed decrease in GFR with higher levels of NT-proBNP in the current study might be a reflection of this finding.
Endothelial function and inflammation
Increased levels of markers of endothelial dysfunction and inflammation have been found to correlate with renal dysfunction in non-CHF patient populations [3, 28]. Interestingly, endothelial dependent vasodilatation was not associated with estimated GFR in non-CHF patients [32]. We showed that next to RBF and FF, parameters of endothelial function were related to GFR in univariate analysis. However, in multivariate analysis, no independent relationship could be established with GFR. This may suggest that the univariate relationships are attributable to the inter-relationship between endothelial function and RBF, which was confirmed in regression analysis for RBF. Of those factors measured, vWF showed the most consistent relationship with GFR and FF, while sVCAM-1 was related to RBF. Both vWF and sVCAM-1 have been shown to correlate with estimated GFR, but also to prognosis in CHF and other patient populations [6, 35]. We did not find any relationship between hs-CRP with GFR, RBF or FF. This suggests that inflammation may not be a strong mediator of renal impairment in CHF.
NT-proBNP
NT-proBNP showed an inverse relationship with both GFR and RBF. This is to our knowledge the first study that showed a strong correlation between endogenous NT-proBNP levels and RBF. In normal subjects, the active brain natriuretic peptide (BNP) may preferably increase RBF by afferent vasodilatation [20]. However, a decrease [18] or no effect on RBF, due to efferent and afferent vasomotor tone unbalance, has also been reported [34]. However, in CHF, the renal actions of BNP are known to be blunted [22]. Therefore, the absence of BNP mediated afferent vasodilatation in the lower regions of RBF may be partly responsible for the markedly reduced GFR in these patients. On the other hand, increased levels of NT-proBNP in parallel to decreased RBF may also be a consequence of more severe cardiac dysfunction. The strong relationship between RBF and NT-proBNP suggests that NT-proBNP may serve as an easily obtainable marker of renal perfusion, which is an important clinical finding because the measurement of RBF is invasive, patient-unfriendly, time-consuming and expensive. Finally, in agreement with our earlier findings, NT-proBNP levels may be a reflection of increased venous congestion, and the relationship with RBF may be a result of the effect of congestion on renal perfusion [8, 9]. The ability of NT-proBNP levels for profiling cardiorenal risk and potential target for reno-protective therapy needs to be investigated in future studies.
Renin angiotensin system activity
PRA showed a linear relationship with decreasing RBF and GFR. PRA levels are increased in CHF due to activation of renin secretion in response to different stimuli [5]. In addition, renin is especially secreted from outer cortical glomeruli in response to decreased RBF [23]. This is important, while in CHF renal blood flow is especially diminished in the cortial regions and relatively preserved in the medulla [19]. Via these pathways PRA does not only influence RBF, but RBF also has profound effects on PRA secretion. Therefore, the relationship between PRA and RBF is probably mainly driven by a marked reduction in forward flow. PRA has been shown to correlate with estimated GFR in other CHF populations, even in patients using ACE-inhibitors [14]. Higher PRA levels might also reflect more severe ACE-inhibition and/or ARB therapy. However, it is plausible, that with more severe renal impairment, ACE escape occurs, which may result in continuing efferent vasoconstriction [31]. Probably, because of a parallel decline in RBF, this is not expressed in an increase in FF.
Albumin excretion
Albuminuria is highly prevalent in CHF, and predisposes to CHF in patients with hypertension [17, 30]. We found that UAE was inversely related to GFR in our CHF population, and we observed that UAE was primarily associated with RBF. We were unable to demonstrate any relationship between UAE and markers of endothelial function and inflammation. This suggests that increased UAE in CHF reflects intrinsic renal damage, possibly due to chronic hypoperfusion. In other chronic conditions, intrarenal hypoperfusion injury progressively compromises the entire kidney [4]. Chronic renal hypoperfusion might ultimately result in reduced tubular reabsorption of albumin, suggesting also tubular dysfunction [24].
Clinical implications
Our findings have important clinical implications. First, impaired hemodynamics are the key determinants of reduced GFR. Therapies aimed at preserving GFR in CHF patients should most likely focus on preservation of RBF. It is however difficult to measure RBF in every heart failure patient, especially in those with compromised hemodynamics. Our present findings suggest that NT-proBNP levels may be used as a marker of RBF, and may therefore be a target for therapy to indirectly improve RBF and subsequent GFR. Therapy targeted at PRA levels seems to be of less interest, since the slope between PRA levels and RBF was much less pronounced. The decrease in FF, together with decrease in GFR and increase in RVR suggests that renal afferent vasoconstriction may be an important target for therapy, even in CHF. Finally, therapy should focus on preventing renal impairment below a GFR of 40 ml/min/1.73 m2 as these patients not only experience functional impairment, but also structural renal damage.
Limitations
This study is of cross-sectional design and thus only can be hypothesis generating. Similarly, cause-effect relationships cannot be distilled from cross-sectional studies. Future studies are therefore needed to intervene in the pathophysiologic mechanisms we have explored to establish the cause-effect relationships. Regretfully we were not able to determine the relationship of SNS-activation and the ultrafiltration coefficient with renal function in our patients. Both may play an important role in renal function impairment in CHF. PRA levels will be altered by ACE-inhibitor and ARB therapy, thereby limiting interpretability. Although our study was rather small, this is to our knowledge by far the largest cohort of patients comparing the results of true renal function measurements with a large number of parameters linked to the biology of impaired renal function.
Conclusion
Reduced RBF is the main determinant of impaired GFR in patients with CHF. Neurohormonal activation and endothelial function were only moderately associated with impaired GFR. NT-proBNP levels may be a non-invasive marker of RBF, and may serve as a target for therapy in future studies.
References
Bohm M, Werner N, Kindermann M (2006) Drug treatment of chronic heart failure. Clin Res Cardiol 95(Suppl 4):36–54
Bongartz LG, Cramer MJ, Doevendans PA, Joles JA, Braam B (2005) The severe cardiorenal syndrome: ‘Guyton revisited’. Eur Heart J 26:11–17
Bonomini M, Reale M, Santarelli P, Stuard S, Settefrati N, Albertazzi A (1998) Serum levels of soluble adhesion molecules in chronic renal failure and dialysis patients. Nephron 79:399–407
Brezis M, Rosen S (1995) Hypoxia of the renal medulla–its implications for disease. N Engl J Med 332:647–655
Brown MJ (2007) Renin: friend or foe? Heart 93:1026–1033
Chong AY, Freestone B, Patel J, Lim HS, Hughes E, Blann AD, Lip GY (2006) Endothelial activation, dysfunction, and damage in congestive heart failure and the relation to brain natriuretic peptide and outcomes. Am J Cardiol 97:671–675
Cody RJ, Ljungman S, Covit AB, Kubo SH, Sealey JE, Pondolfino K, Clark M, James G, Laragh JH (1988) Regulation of glomerular filtration rate in chronic congestive heart failure patients. Kidney Int 34:361–367
Damman K, van Deursen VM, Navis G, Voors AA, van Veldhuisen DJ, Hillege HL (2008) Increased central venous pressure is associated with impaired renal function and mortality in a broad spectrum of patients with cardiovascular disease. J Am Coll Cardiol accepted for publication
Damman K, Navis G, Smilde TD, Voors AA, van der BW, van Veldhuisen DJ, Hillege HL (2007) Decreased cardiac output, venous congestion and the association with renal impairment in patients with cardiac dysfunction. Eur J Heart Fail 9:872–878
Dittrich HC, Gupta DK, Hack TC, Dowling T, Callahan J, Thomson S (2007) The effect of KW-3902, an adenosine A1 receptor antagonist, on renal function and renal plasma flow in ambulatory patients with heart failure and renal impairment. J Card Fail 13:609–617
Donker AJM, Vanderhem GK, Sluiter WJ, Beekhuis H (1977) Radioisotope method for simultaneous determination of glomerular-filtration rate and effective renal plasma-flow. Neth J Med 20:97–103
Evans RG, Eppel GA, Anderson WP, Denton KM (2004) Mechanisms underlying the differential control of blood flow in the renal medulla and cortex. J Hypertens 22:1439–1451
Givertz MM, Massie BM, Fields TK, Pearson LL, Dittrich HC (2007) The effects of KW-3902, an adenosine A1-receptor antagonist, on diuresis and renal function in patients with acute decompensated heart failure and renal impairment or diuretic resistance. J Am Coll Cardiol 50:1551–1560
Hillege HL, Girbes AR, de Kam PJ, Boomsma F, de ZD, Charlesworth A, Hampton JR, van Veldhuisen DJ (2000) Renal function, neurohormonal activation, and survival in patients with chronic heart failure. Circulation 102:203–210
Hillege HL, Nitsch D, Pfeffer MA, Swedberg K, McMurray JJ, Yusuf S, Granger CB, Michelson EL, Ostergren J, Cornel JH, de ZD, Pocock S, van Veldhuisen DJ (2006) Renal function as a predictor of outcome in a broad spectrum of patients with heart failure. Circulation 113:671–678
Hillege HL, van Gilst WH, van Veldhuisen DJ, Navis G, Grobbee DE, de Graeff PA, de Zeeuw D (2003) Accelerated decline and prognostic impact of renal function after myocardial infarction and the benefits of ACE inhibition: the CATS randomized trial. Eur Heart J 24:412–420
Ingelsson E, Sundstrom J, Lind L, Riserus U, Larsson A, Basu S, Arnlov J (2007) Low-grade albuminuria and the incidence of heart failure in a community-based cohort of elderly men. Eur Heart J 28:1739–1745
Jensen KT, Carstens J, Pedersen EB (1998) Effect of BNP on renal hemodynamics, tubular function and vasoactive hormones in humans. Am J Physiol 274:F63–F72
Kilcoyne MM, Schmidt DH, Cannon PJ (1973) Intrarenal blood flow in congestive heart failure. Circulation 47:786–797
La Villa G, Fronzaroli C, Lazzeri C, Porciani C, Bandinelli R, Vena S, Messeri G, Franchi F (1994) Cardiovascular and renal effects of low dose brain natriuretic peptide infusion in man. J Clin Endocrinol Metab 78:1166–1171
Ljungman S, Laragh JH, Cody RJ (1990) Role of the kidney in congestive heart-failure—relationship of cardiac index to kidney-function. Drugs 39:10–21
Marcus LS, Hart D, Packer M, Yushak M, Medina N, Danziger RS, Heitjan DF, Katz SD (1996) Hemodynamic and renal excretory effects of human brain natriuretic peptide infusion in patients with congestive heart failure: a double-blind, placebo-controlled, randomized crossover trial. Circulation 94:3184–3189
Nushiro N, Ito S, Carretero OA (1990) Renin release from microdissected superficial, midcortical, and juxtamedullary afferent arterioles in rabbits. Kidney Int 38:426–431
Pollock CA, Poronnik P (2007) Albumin transport and processing by the proximal tubule: physiology and pathophysiology. Curr Opin Nephrol Hypertens 16:359–364
Prevot A, Huet F, Semama DS, Gouyon JB, Guignard JP (2002) Complementary effects of adenosine and angiotensin II in hypoxemia-induced renal dysfunction in the rabbit. Life Sci 71:779–787
Ruilope LM, van Veldhuisen DJ, Ritz E, Luscher TF (2001) Renal function: the cinderella of cardiovascular risk profile. J Am Coll Cardiol 38:1782–1787
Smilde TDJ, Hillege HL, Voors AA, Dunselman PHJ, van Veldhuisen DJ (2004) Prognostic importance of renal function in patients with early heart failure and mild left ventricular dysfunction. Am J Cardiol 94:240–243
Stam F, van GC, Becker A, Dekker JM, Heine RJ, Bouter LM, Stehouwer CD (2006) Endothelial dysfunction contributes to renal function-associated cardiovascular mortality in a population with mild renal insufficiency: the Hoorn study. J Am Soc Nephrol 17:537–545
Torre-Amione G, Kapadia S, Benedict C, Oral H, Young JB, Mann DL (1996) Proinflammatory cytokine levels in patients with depressed left ventricular ejection fraction: a report from the studies of left ventricular dysfunction (SOLVD). J Am Coll Cardiol 27:1201–1206
van de Wal RM, Asselbergs FW, Plokker HW, Smilde TD, Lok D, van Veldhuisen DJ, van Gilst WH, Voors AA (2005) High prevalence of microalbuminuria in chronic heart failure patients. J Card Fail 11:602–606
van de Wal RM, Plokker HW, Lok DJ, Boomsma F, van der Horst FA, van Veldhuisen DJ, van Gilst WH, Voors AA (2006) Determinants of increased angiotensin II levels in severe chronic heart failure patients despite ACE inhibition. Int J Cardiol 106:367–372
van der Harst P, Smilde TD, Buikema H, Voors AA, Navis G, van Veldhuisen DJ, van Gilst WH (2006) Vascular function and mild renal impairment in stable coronary artery disease. Arterioscler Thromb Vasc Biol 26:379–384
van der Horst I, Voors AA, van Veldhuisen DJ (2007) Treatment of heart failure with ACE inhibitors and beta-blockers: what is next? Aldosterone receptor antagonists? Clin Res Cardiol 96:193–195
van der Zander K, Houben AJ, Hofstra L, Kroon AA, de Leeuw PW (2003) Hemodynamic and renal effects of low-dose brain natriuretic peptide infusion in humans: a randomized, placebo-controlled crossover study. Am J Physiol Heart Circ Physiol 285:H1206–H1212
Wannamethee SG, Shaper AG, Lowe GD, Lennon L, Rumley A, Whincup PH (2006) Renal function and cardiovascular mortality in elderly men: the role of inflammatory, procoagulant, and endothelial biomarkers. Eur Heart J 27:2975–2981
Acknowledgments
K. Damman and P. van der Harst are supported by the Netherlands Heart Foundation (grants 2006B157 and 2006B003, respectively). A.A. Voors and D.J. van Veldhuisen are Clinical Established Investigators of the Netherlands Heart Foundation (grants 2006T37 and D97-017, respectively). P. van der Harst is a research fellow of the Interuniversitair Cardiologisch Instituut Nederland (ICIN).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Smilde, T.D.J., Damman, K., van der Harst, P. et al. Differential associations between renal function and “modifiable” risk factors in patients with chronic heart failure. Clin Res Cardiol 98, 121–129 (2009). https://doi.org/10.1007/s00392-008-0732-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-008-0732-z