Abstract
Background and objective
Sensor technology, in particular wearable inertial sensors, has the potential to help researchers objectively assess the functionality of older adults. The following review provides an overview about the possible use of sensor technology to detect and prevent pre-frailty and frailty.
Method
A systematic literature search in PubMed and the Cochrane Library was conducted. Articles were selected according to the following criteria: frail and/or pre-frail population, use of wearable and non-wearable sensor technology to measure or enhance human movements or activities of daily living and a focus on frailty assessment.
Results
A total of 28 publications were found. Sensor-derived parameters obtained during assessment of gait, functional performances and physical activity were reported to be relevant for screening and monitoring pre-frailty and frailty; however, current findings are limited to cross-sectional studies, which do not allow establishment of a causal relationship between motor performance, physical activity and specific frailty states. No study monitored specific activities of daily living.
Discussion
Outcome variables from technology-based assessment seem to provide valuable information for frailty assessment. Strenuous testing conditions as well as increased variability in gait, functional performance and physical activity may be useful in identifying frailty. Outcome variables derived from gait, motor assessment and physical activity must still be validated in large cohorts and under daily living conditions in order to develop robust screening tools for pre-frailty and frailty. Further research should focus on specific activities of daily living in pre-frail or frail older adults and technology-based approaches for intervention and prevention.
Zusammenfassung
Hintergrund und Zielsetzung
Sensortechnologie und speziell tragbare Inertialsensorik kann die Funktionalität älterer Menschen messen und bewerten. Im folgenden Review wird ein Überblick gegeben, inwieweit Sensortechnologie (Pre-)Frailty erkennen und der Prävention dienen kann.
Methoden
Eine systematische Literaturrecherche in PubMed und Cochrane Library wurde mit folgenden Einschlusskriterien durchgeführt: (pre-)fraile Studienpopulation, Einsatz tragbarer und/oder nicht tragbarer Sensortechnologie zum Messen oder Fördern von Bewegung und Aktivitäten des täglichen Lebens und Fokus auf Frailty-Assessment.
Ergebnisse
Insgesamt 28 Artikel wurden identifiziert. Sensorparameter für den Gang, das motorische Assessment und die körperliche Aktivität eignen sich zum Screening und Monitoring von (Pre-)Frailty. Kausalbeziehungen zwischen Sensorparametern und Frailty-Status können aufgrund mangelnder Längsschnittstudien jedoch bislang nicht abgeleitet werden. Ein sensorbasiertes Monitoring spezieller Aktivitäten des täglichen Lebens erfolgte nicht.
Diskussion
Technologiegestützte Assessmentparameter können wertvolle Informationen zum Frailty-Assessment beitragen. Sensorparameter von Gang, motorischem Assessment und körperlicher Aktivität sollten in großen Stichproben und unter Alltagsbedingungen validiert werden, um robuste Screening-Instrumente für (Pre-)Frailty zu entwickeln. Zukünftige Projekte sollten sich darüber hinaus auf spezifische sensorbasiert gemessene Aktivitäten des alltäglichen Lebens und technologie-gestützte Ansätze zur Prävention und Intervention bei (Pre-)Frailty fokussieren.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Current demographic changes in industrialized societies will lead to a significant increase of older people over 80 years old. Frailty is more prevalent in advanced age [1] and the demand for care increases with worsening states of frailty [2]. This trend prompts a need to find alternative ways of care and support. Current assessments of functionality of older people in hospitals and in private practices are limited in their ability to reflect everyday performance and to evaluate patients’ true capabilities in a natural scenario. Numerous researchers have suggested that information technology (IT) and sensor technology, in particular wearable inertial sensors, are important tools for overcoming these problems. Information technology is defined as “the use of computers and telecommunications equipment (with their associated microelectronics) to send, receive, store and manipulate data” [3]. Sensor technology means the use of sensors to measure or control changes of biological or technical systems [4]. Inertial sensors in this field are used to measure translational and rotational acceleration of the body of a human being. Specific sensor-based parameters, such as velocity peaks, stride time or stride length derived from performance-based tests, including gait or sit-to-stand transition, seem to provide relevant information on clinical parameters that may allow screening for or even diagnosing frailty [5, 6]. Various information about individual behavior and performance including mobility radius, transition speed, gait variability and muscle strength of upper and lower extremities can be measured by sensor technology [7–9]. Life rhythms and specific activities of daily living (ADL) can be detected by functional and activity patterns, for example with the help of room sensors [10, 11]. Sensor technology can also be a resource-saving way to record an individual’s movement in everyday life, particularly during specific risk periods, such as following hospital discharge. As the diagnostic information on the entire daily routine of a person cannot be documented in a laboratory environment, an objective long-term monitoring, allowing the detection even of subtle changes, can only be provided by sensor technology. This information can complement cross-sectional assessments by healthcare professionals. Furthermore, sensor technology may provide more specific and more accurate measurements than traditional assessments. For example, sensor-derived spatiotemporal parameters will allow the evaluation of single phases of the timed up and go (TUG) test or of a sit-to-stand test. This may allow early detection of frailty development and in turn tailor personalized interventions based on a sensor-derived risk profile.
In recent years, several studies have been published about the application of IT/sensor technology in frail older adults. In the following review, we provide an overview about the current evidence for assessing frailty features by means of sensor technology. The aim of this review is to describe the potential of IT and sensor technology to objectively assess the functionality and especially the mobility of pre-frail and frail older adults in clinical settings and in everyday life. More specifically, we would like to address the following questions: to what extent is it possible to use portable or room sensors for detecting pre-frailty? Which sensor-based assessment approaches are currently available? To what extent are these approaches suitable for use in a routine clinical setting or at home?
Methods
In this study two physiotherapists, one geriatrician, one sports scientist and two computer scientists cooperated to create the following combination of search terms for the search in PubMed:
Frail elderly, frail, pre-frail, pre-frailty, sensor, ehealth, techn, coach, assessment, mhealth, mobile health, accelerometer, tele, virtu, smart health and health informatics
The search strategy for the Cochrane Database was the following:
frail elderly or frail or pre-frail or pre-frailty or prefrail and sensor or ehealth or techn or mhealth or mobile health or tele or virtu or smart health or health informatics or accelerometer.
Two reviewers (A.H. and L.D.) independently selected relevant documents using the following criteria for inclusion:
-
1.
A study population of frail and/or pre-frail older adults,
-
2.
the use of wearable and non-wearable sensor technology to measure or enhance human movements or activities of daily living,
-
3.
a focus on frailty assessment.
If there were divergent results the document was discussed until a consensus was reached. Study protocols, conference summaries and abstracts of posters or lectures were excluded from the analysis. Furthermore, we eliminated articles in languages other than English or German. As the focus of this review is on current and upcoming aspects of frailty and technology, we decided to include only publications since the year 2000. A total of 28 records in the categorie “frailty assessment”.
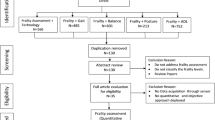
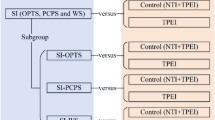
The category “frailty assessment” was then divided into the subcategories “measurement of specific parameters to detect frailty” with the subgroups: gait parameters and frailty, performance-based measures of frailty (with TUG, sit-to-stand and stand-to-sit), static balance parameters related to frailty, objective physical activity assessment (with general physical activity and sedentary behavior, step counts, different types of activities), hybrid frailty assessments combining technology and conventional measures and measurement of activities of daily living and daily habits in the context of frailty (see Table 1).
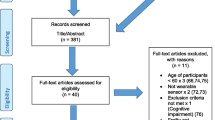
The overall process of literature searching, extraction and categorization is shown in the modified preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow diagram (Fig. 1).
Modified PRISMA flow diagram according to Moher et al. 2009 [12]
Technology in care and healthcare of frail older adults
Frailty assessment
Frailty has been defined as “a clinical state in which there is an increase in an individual’s vulnerability for developing increased dependency and/or mortality when exposed to a stressor” [13]. Frailty can occur as the result of diseases and medical conditions and it is an important prognostic factor for older persons to develop disabilities, being institutionalized or hospitalized and having a higher rate of mortality [14, 15]. There are two major approaches to defining frailty: one is the deficit accumulation approach of Rockwood [16] that relies on multimorbidity as the major predictor of frailty [17]. The other is the Fried physical phenotype of frailty, which focuses on specific, potentially treatable causes of frailty [18]. In addition to these two major approaches, other frailty definitions, such as the Groningen frailty indicator (GFI) and the Edmonton frail scale (EFS), include psychosocial as well as physical components [19].
To date, the most commonly used and robust frailty definition is based on the physical phenotype criteria provided by Fried et al. (2001) [19–21]. According to Fried et al. frailty is present when at least three of the following five criteria are met: weight loss, exhaustion, weak grip strength, slow walking speed and low physical activity [21]. A pre-frailty state is diagnosed when one or two of these criteria are present. As a mechanical model, the physical phenotype criteria of frailty show overlap with other physical assessments and also with modern definitions of sarcopenia. In addition to the Fried criteria, physical assessments have also been used to diagnose frailty. Measurements of upper extremity strength (e. g. grip strength) and those of lower extremity strength (e. g sit-to-stand time) have both been proven to be sensitive when a diagnosis of frailty is intended. Among mobility tests, gait assessments have emerged as being the most sensitive [22]. Several studies have reported that technology-based spatiotemporal gait parameters can distinguish different frailty states, although direct comparison of study results is limited due to differences in the gait assessment protocols applied [23, 24]. Recent advances in ambulatory technology-based measurements allow the recording of habitual daily physical activity over the course of several days, weeks or even months. Particularly for the monitoring of changes of frailty status over time, these measurements are considered to be highly valuable as the basis for specific and targeted interventions to reverse frailty as well as to understand the dynamic nature of frailty itself [25]. We found 28 articles documenting technology-based screening and diagnosis of frailty. The respective instruments ranged from electronic walkway systems and IT-connected furniture, such as easy chairs with pressure sensors to body-worn sensors including triaxial accelerometers and smartphones. These tools have been used to measure specific frailty-related parameters, to complement existing screening tools and to build and modify screening tools that detect and monitor frailty.
Measurement of specific parameters to detect frailty
In six articles we found technology-based measurements of gait parameters, physical activity, strength and balance that were expected to detect frailty. Walkway systems, cameras, force platforms and, in the most recent studies, wearable sensors were commonly used for technology-based frailty analysis. Participants were defined as frail, pre-frail or robust according to different frailty definitions. Of the studies four used the definition according to Fried et al. (2001) [6, 8, 21, 23, 26, 27]. In one study, participants were defined as frail without an underlying definition [28].
Gait parameters and frailty
Recently, Schwenk et al. [23] provided an overview on studies which used gait analyses to identify frailty. Most studies used electronic walkway systems. Only one out of eleven studies used wearable sensor technology for assessing gait in this respect. The other studies used cameras, force platforms and foot switches. Among the spatiotemporal gait parameters evaluated in this review, gait speed during habitual walking best distinguished among the three Fried frailty subgroups of frail, pre-frail and robust. According to Mohler et al. (2014), gait speed is a reliable measure to identify frailty, although results can be influenced by walking distance [25]. During fast walking, gait variability, reduced cadence and increased step width variability showed high effect sizes to separate pre-frail from robust older adults. On the other hand, stride length and double support distinguished best between frail and pre-frail individuals in a pooled analysis [23]. In line with the findings from this review Schwenk et al. (2015) recently demonstrated that gait speed was a relevant parameter for the identification of pre-frailty in a cohort of 125 older adults in a community living center [6]. Stride length and double support were the most relevant gait parameters for distinguishing between the three frailty states. All parameters in this study were measured by wearable sensor technology. Stride time was relevant for distinguishing frail and pre-frail study participants from robust older adults [6]. While a reduced cadence may be a sensitive parameter for an early diagnosis of frailty, the progression of frailty (from pre-frail to frail) may be strongly associated with reduced step length.
Dual-task walking speed has also been suggested as an early predictor of frailty [23]. Moreover, Thiede et al. (2016) found the highest effect sizes for between-group discrimination for double support during habitual normal walking speed, for speed variability during dual task walking and for trunk sway during fast walking [8]. Previous studies have reported that dual task conditions give further information on the risk of falls and cognitive reserves [29] and especially the latter factor may also play a role in the development of frailty. Physiological reserves including cognitive reserves decrease when frailty worsens. In addition, when frail individuals are exposed to an external stressor, serious health events, such as falls, are more likely to occur [30].
In a smaller group of 65 seniors, Moe-Nilssen and Helbostad (2005) found step width normalized to a walking speed of 0.9 m/s not to be different between frail and non-frail subjects. In contrast, other specific parameters, including interstride trunk acceleration and trunk variability, were relevant for identifying frailty. Trunk variability classified 80 % of the subjects correctly into their respective group and was assessed by a triaxial accelerometer [28]. In another study by Martinez-Ramirez et al. (2015), the root mean square of trunk acceleration and total harmonic distortion were significantly different among frailty states [26]. These results suggest that specific gait parameters beyond walking speed are affected by frailty.
Performance-based measures of frailty
Sensor-based measurements of the TUG test, an extended version of the test and sit-to-stand and stand-to-sit transitions have been tested in eight papers and are described in the following chapter. Measurement instruments were wearable inertial sensors with accelerometers and gyroscopes as well as pressure sensors. Study results were intended to show that wearable sensors can either complement and improve traditional testing methods in testing accuracy with additional parameters during test subphases [31] or enable automated non-expert assessments [5]. In all articles, participants were defined as frail according to the definition by Fried et al. (2001) [21].
Timed up and go test (TUG)
Galan-Mercant and Cuesta-Vargas [31] measured acceleration and balance parameters in the 10 m extended TUG test (10 m gait, armless chair) using a smartphone in different subphases of the test. In the sit-to-stand and stand-to-sit subphases and in the gait go and gait come subphases, the accelerometer showed significantly less acceleration in frail older adults. In the turnaround subphase, the gyroscope data for velocity were significantly lower. Frail persons seemed to perform the test more cautiously. The conventional TUG test was again assessed with accelerometer and gyroscope sensors by Greene et al. (2014) [5]. With the sensor data, participants were classified as frail or robust with mean accuracy of 75.20 % stratified by gender, compared to 71.82 % using TUG test time alone. The authors concluded that a simple assessment of frailty involving a well-known mobility test, such as the TUG test and inertial sensors can be fast and effective and can be conducted by non-experts [5]. These results suggest that specific gait parameters beyond walking speed are affected by frailty.
Sit-to-stand and stand-to-sit
Sit-to-stand and stand-to-sit transitions have also been measured with inertial sensors attached to the chest, the lower back or the hips. In 2014 Millor et al. published a review to assess the role of body motion sensors in sit-to-stand and stand-to-sit transitions. They identified sixteen different parameters related to transition performance as potentially meaningful for disabilities and impairments. Transition duration is the most used parameter and frail older adults seem to have longer and more variable transition duration [32]. Significant longer sit-to-stand and stand-to-sit transition duration in frail older adults with a single inertial sensor attached to the chest was assessed in a study by Ganea et al. (2011) [33]. Lower maximum and minimum acceleration values in the vertical axis in frail elderly compared to robust older adults were described by Galan-Mercant and Cuesta-Vargas (2013), and can be explained by less strength in concentric and eccentric contraction of the quadriceps femoris muscle. For the assessment researchers affixed a smartphone to the participants’ chest [34]. Decreased smoothness of the transition pattern and dynamics of trunk movement occurred in frail older adults. An assessment after three weeks of a rehabilitation program showed that smoothness of transition pattern had the highest improvement effect size and discriminative performance in frail older adults [33]. Furthermore, velocity and trunk displacement allowed differentiation between different frailty states and frequency domain measurements seem to be higher for elderly fallers [32]. In addition, velocity peaks and modified impulse parameters in the stand-up and sit-down phases of the 30 s chair stand test could significantly differentiate subjects along different frailty states according to Millor et al. (2013). The trunk orientation range during the impulse phase also had this potential [35]. Ganea et al. (2012) confirmed a classification algorithm of trunk acceleration patterns of sit-to-stand and stand-to-sit phases within a real world environment with an accuracy rate of up to 89 % [36]. Performance in a five times sit-to-stand test, a TUG test and quiet standing balance was assessed by Greene et al. (2014) using a platform that combines inertial and pressure sensors. Participants wore five inertial sensors with a triaxial accelerometer and a triaxial gyroscope. The Nintendo Wii balance board was used to measured balance. The combination of the three tests assessed frailty better than any single test or sensor measurement alone, with 94 % accuracy for men and 84 % for women [37].
Static balance parameters related to frailty
Studies on the use of instrumented static balance assessment for frailty assessment are controversial and four studies were found on this aspect. The participants in all studies were defined as pre-frail or frail according to Fried et al. (2001) [21]: two studies did not identify any differences in balance parameters between frail and robust older adults [6, 8] while two others found differences [38, 39]. Schwenk et al. (2015) found hip sway and mean center of mass sway to be relevant for the identification of pre-frailty. No balance parameter could distinguish between the three frailty levels: robust, pre-frail and frail [6]. Also Thiede et al. (2016) did not identify any significant difference in balance parameters [8]. In contrast, Martinez-Ramirez et al. (2011) found higher values in the sway of the center of mass in postural balance in a feet together with eyes closed standing balance position in a frail group compared to the robust group [38]. Galan-Mercant and Cuesta-Vargas (2014) found the accelerometer in a smartphone was able to analyze the kinematics of the Romberg test between frail and non-frail elderly people in 18 subjects. The highest significant difference between groups was found in the accelerometer values in peak acceleration [39].
Objective physical activity assessment
Aside from daily physical activity, such as steps per day, walking bout duration or time spent in specific body positions, the individual degree of sedentary behavior is an important risk factor for frailty and eight studies met the abovementioned inclusion criteria. Physical activity and sedentary behavior were measured using wearable inertial sensors with accelerometers and gyroscopes in all studies. Results were interpreted to be used to improve accuracy of traditional assessments [40] or to aid in the development of instrumented screening assessments for home usage to detect or predict (pre-)frailty [6, 27]. Frailty definitions included the frailty criteria of Fried [6, 21, 27], the GFI [41] and low walking speed [42, 43].
General physical activity and sedentary behavior
Several methods to estimate general physical activity have been described. Song et al. (2015) [42] assessed physical activity using an accelerometer, describing sedentary time (<100 counts per minute) and moderate intensity activity (>2020 counts per minute) with the help of intensity thresholds used by the National Cancer Institute on a minute by minute basis [44]. They found a significant relationship between daily sedentary time and incidence of physical frailty after 2 years [42]. In a similar approach Chen et al. (2015) [40] measured physical activity objectively via accelerometers as one of the Fried criteria. Physical activity was defined as energy expenditure in kilocalories per kilogram of body weight per day (kcal/kg/day) and a score in the lowest 20 % of energy expenditure was defined as low physical activity. This resulted in a cut-off of 6.20 kcal/kg/day for men and of 7.13 kcal/kg/day for women [40].
With increasing frailty a reduction in walking bout duration has also been shown. Walking bout duration variability was the most relevant physical activity parameter for distinguishing among the three frailty levels in a study by Schwenk et al. (2015) [6]. Upper body movements were underestimated in sensor-derived data provided by waist-mounted accelerometers in a study by Theou et al. (2012). This problem could be solved by a combined approach including heart rate monitoring and portable electromyography (EMG) [7].
Step counts
Theou et al. (2012) found a correlation between accelerometer-derived step counts and frailty [7] and Schwenk et al. (2015) found steps per day to be a relevant parameter for the identification of pre-frailty [6]. Soaz and Diepold (2015) validated a step detection algorithm for a single waist-worn triaxial accelerometer and found a mean sensitivity (99.1 %) for gait speed between 0.2 m/s and 1.5 m/s. False positives were reduced by 73 % and two different characteristic step patterns, one for normal and one for frail walking were recognized [43]. McCullagh et al. (2015) did a review to examine the value and reliability of current motion sensors to measure step count in frail older hospitalized patients in 24 validation studies. A total of fifteen motion sensors (eight pedometers, six accelerometers and one sensor system) were tested in older adults. According to the authors “further validation studies are required to determine which, if any, motion sensor can accurately measure step-count” [45].
Different types of activities
In the literature, sitting, standing, lying and walking have been measured as different types of activity. Different definitions of frailty were used in the respective studies, such as the GFI [41] and Fried’s frailty criteria [6, 21, 27, 41, 46]. Schwenk et al. (2015) found lower amounts of walking activity as well as an increased percentage of sitting in pre-frail older adults compared to robust older adults [6]. Longer typical walking episodes assessed with one inertial sensor appeared to be a sensitive predictor of prospective falls in frail older adults in a study by Mohler et al. (2016) [27]. Hollewand et al. (2016) carried out an observational study with eighteen frail elderly subjects to validate the accelerometer-based DynaPort system (McRoberts, The Hague, The Netherlands) of detecting physical activity. Sensitivity and specificity for locomotion were 83.3 % and 100.0 %, respectively. Sensitivity was sufficient for sitting with 94.4 % and specificity was sufficient for lying at 100 % and standing at 93.3 % [46]. According to a review by McCullagh et al. (2015), motion sensors accurately measured time in an upright position in frail older hospitalized patients in 24 validation studies [45].
Hybrid frailty assessments combining technology and conventional measures
Some groups combined technology with conventional methods for frailty assessment and developed new (multicomponent) systems with room sensors and wearable sensors to detect frailty and four studies were categorized in this section. The aims of these studies were to conduct automated frailty assessment and monitoring [47, 48] and to improve traditional frailty assessments [7]. Different frailty definitions ranged from expert assessment to modified frailty criteria based on those of Fried [21, 47, 49]. Chang et al. (2013) developed an eFurniture system to measure frailty indicators in older adults’ homes. Reaction time was measured via a scale with a laser light, which the person has to catch and with an automated TUG test with pressure sensors under a chair. Weakness, slowness and weight were measured via pressure sensors under the chair in the TUG test and a 30 s sit-to-stand test. Balance in gait and standing was measured with a balance pad and functional reach with an automated functional reach test. Physical activity was assessed by an electronic questionnaire. Compared with expert assessment, sensitivity was 79.71 % and specificity 86.25 % [47]. Another home-based assessment was developed by Hewson et al. (2013). This system is based on a series of remote tests with objects in peoples’ homes. Grip strength and exhaustion was measured by a modified grip ball. A triaxial accelerometer in a smartphone was used to estimate gait velocity and physical activity level and a bathroom scale to assess weight loss. Single case graphs were shown but this article did not describe any statistical analyses [49]. A system by Theou et al. (2012) collected accelerometer-based physical activity measurements over ten days as well as EMG readings, global positioning system (GPS) activity data and information from the Minnesota Leisure Time Activity Questionnaire (MLTAQ) to screen for frailty. Physical activity data derived from the overall system explained 54 % of the variance in the frailty index. Any single tool alone only accounted for a maximum of 16 % of the variance [7]. Fontecha et al. (2013) described the development of a system for collecting and combining accelerometer-measured gait analyses and risk factors for frailty from patient records. The system was pilot-tested in ten patients [48].
Measurement of activities of daily living and daily habits related to frailty
In addition to measurements of specific assessments and general physical activity, activity patterns and daily routines in long-term monitoring can also be assessed by sensors. In two studies general daily habits were assessed with room sensors combined in home monitoring systems [10, 50]. Motion sensors, vision sensors and audio technology were used to detect usual and unusual behavioral patterns. In one study the EFS was used to classify patients as frail [50]. In the other study, the authors assumed most residents of the independent living facility to be frail without applying a precise definition [10]. Alexander et al. (2011) developed an early warning system for functional decline using a network of motion sensors, bed sensors and stove sensors. The sensors provided information about patterns of daily habits as a motion density, showing usual sleeping hours, time out of the apartment and certain activities in the apartment [10]. Changes in daily habits were also evaluated by de Folter et al. (2014) where each home was equipped with either two motion sensors, or one motion and one bed usage sensor. The authors defined requirements, drew up designs and evaluated the results. Data were depicted according to the individual case [50]. The study quality differed widely among the 28 studies which have been included in the present review. In eight studies a potential risk of incomplete reporting of outcome data had to be recorded [10, 26, 35, 43, 47–50]. A low risk for selective reporting could only be observed in three of the 28 studies. In those three studies information was provided on the registration of the studies in a study register and on the respective study trial number [6, 27, 46]. In nine studies the recruitment process was not described in sufficient detail to estimate if a consecutively recruited study sample was included [8, 31, 33, 34, 36, 38, 47–49], a further nine studies did not clearly state the inclusion criteria [7, 10, 35, 38, 43, 47–50] and in thirteen articles the process of patient selection could be criticized as possibly biased [7, 31, 33–36, 38, 42, 43, 47–50]. The applied diagnostic criteria for frailty could have introduced bias in five studies [26, 28, 42, 43, 49]. An overview of the included studies is presented in Table 2. Reviews have not been included.
Discussion
Overall, the results presented in this review suggest that technology-based measurements have a high potential for screening, monitoring and preventing frailty. Numerous studies have shown that specific parameters derived from motor assessments and physical activity monitoring are helpful for the identification of frailty and for the differentiation of frailty levels, such as non-frail, pre-frail and frail. Studies aimed to improve the accuracy of traditional assessments for better and earlier detection of (pre-)frailty using objective parameters. Another goal, especially for home assessment and in everyday life, has been to develop an automated assessment system. Currently, no proven automated assessment system for (pre-)frailty seems to exist.
Gait parameters and frailty
Several sensor-derived spatiotemporal gait parameters seem to provide valuable information for the diagnosis of frailty and the discrimination of frailty levels. In particular, stride length and double support time emerged as sensitive discriminating variables besides gait speed [6, 8, 23, 25]. Schwenk et al. (2015) assumed that a lower extremity strength and/or a more cautious gait are responsible for reduced spatial gait parameters which seems to be linked with the progression of frailty [8, 23]. Temporal parameters, such as reduced cadence based on stride time, could distinguish pre-frailty [23]. Furthermore, increased variability in several gait variables, including step width and trunk sway, seem to provide valuable information for the early diagnosis of frailty [6, 8, 23, 25]. Explanatory power can be improved when older adults with lower physiological reserves are put under stress by walking at maximum speed or by adding a cognitive task in a dual task test set-up [23]. Decline in the sensorimotor system and/or in cognitive function can both contribute to this effect [23]. It is important to take psychometric aspects as well as the underlying frailty model into account when new assessment strategies such as dual tasking or the addition of an item to an existing assessment tool should be tested in the future. At the moment, these findings are limited to cross-sectional study designs, which do not allow us to establish a causal relationship between changes in gait characteristics and the development of frailty. Longitudinal studies are needed to provide evidence for a causal relationship between sensor-derived gait parameters and frailty.
Performance-based measures of frailty
In performance-based measures of frailty, the TUG test subphases and sit-to-stand transition showed differences in frail and robust older study participants. Transition duration was longer and more variable in frail older adults [5, 31, 55]. Similar to increased gait variability, more variable results in performance-based measurements, such as sit-to-stand, indicate more unstable performances. Future studies should test the hypothesis that increased variability in motor measures is a specific symptom of frailty. Furthermore, power measures should be included in future studies, as Regterschot et al. (2015) showed associations between chest power during sit-to-stand transition and objective as well as self-reported functional status [56]. Interestingly, a battery of three performance measurements improved the accuracy of frailty assessment [37]. This indicates that different sensor-based mobility assessments, focusing on basic mobility activities such as gait, rising from a chair and turning, may provide the most valuable information for a diagnosis of frailty. It has to be noted that most of the current findings are limited to small study samples. Variables derived from performance-based tests, such as acceleration, velocity, power and trunk displacement should therefore be confirmed in larger cohorts thereby allowing the development of robust diagnostic tools. In this context Regterschot et al. (2016) found a lower accuracy of sensor-based measures, e. g. in sit-to-stand transitions, compared to laboratory methods, e. g. with force plates. They concluded that a wearable sensor-based method cannot yet replace laboratory testing but could be a practical method which would be appropriate for clinical practice [9]. Reliable cut-off values and quality standards still have to be defined. Large cohorts would facilitate the development of evaluation models based on sensor-derived performance measures which could automatically distinguish the different frailty states. In the daily routine decision rules (e. g. decision trees and fuzzy logic) could improve the evaluation of sensor-derived performance measures in daily activities [36].
Static balance parameters related to frailty
Of the studies two did not show frailty-related differences in sensor-derived balance parameters, while two other studies did [38, 39]. In one study, the small sample size could explain the inability to make definitive conclusions [8]. In another study that distinguished between frail and non-frail older adults, the researchers conducted a discrete wavelet transformation of the acceleration and orientation signals from the inertial sensors. The authors assumed that this evaluation method was superior to other evaluation methods, such as sway area or non-localized Fourier transformed technique calculations [38]; however, the wavelet analysis was unable to differentiate between frailty states. The limited number of studies and the inconclusive results therefore do not allow a conclusion about the added value of static balance assessment and the most appropriate method for frailty screening at the moment.
Objective physical activity assessment
Daily sedentary time and walking bout duration allowed a diagnosis of frailty and step counts identified pre-frail and frail older adults [6, 7, 42]. In general, physical activity is reduced with worsening frailty level [6, 7]. Step counts per day were relevant to identify pre-frailty and correlated with frailty [6, 7]. In step detection, one major problem with most step detection algorithms for single waist-worn accelerometers is the loss of accuracy at low speeds (<0.8 m/s) [57]. Further validation studies are required [45, 57] and their use in frail elderly populations is therefore currently limited. The instruments under study should be validated according to recommendations for standardizing validation procedures assessing physical activity of older persons by monitoring body postures and movements, as Lindemann et al. (2013) pointed out. They noted that video analysis or direct observation by at least two persons is a valid reference criterion for validation studies [58]. Differences between older adults living in rural areas and urban environments as well as population-based specifics should also be considered while defining cut-off values [7].
Different types of activity were measured with inertial sensors [6, 21, 27, 46]. Hollewand et al. (2016) found an accelerometer-based system to have insufficient specificity for sitting and insufficient sensitivity for lying and standing and they therefore found it to be not suitable for measuring different types of activity in frail older adults [46]. This indicates the importance of using instruments that have been validated for this specific target group. Another important activity is stair climbing. Coley et al. (2004) documented a 97 % sensitivity and 94 % specificity for stair climbing in three older adults with mobility impairment [59]. As cycling is a common activity in heathy older adults [2], it should also be tested in future studies [60]. In everyday physical activity, walking bout duration was the most relevant physical activity parameter for differentiating the three frailty levels. With respect to the measurement of physical activity in daily routine, it may be assumed that sensor-based documentation can quantify the frailty-associated decline of routine physical activity and thereby help researchers to more accurately evaluate the individual frailty level. Schwenk et al. (2015) found a continuous reduction in the variability of walking episodes with increasing frailty level and assumed that this more static and less complex physical activity behavior in frail individuals can also be measured in routine physical activity behavior [6]. The application of different definitions of frailty has limited the comparability of studies. Participants were classified using gait speed [42, 43] or by applying the deficit accumulation model [40] or Fried’s frailty criteria. In one study the GFI (which also includes psychosocial factors) [46] was used.
Hybrid frailty assessments combining technology and conventional measures
With regard to hybrid frailty assessments general conclusions cannot be drawn as different systems and a different focus were applied in the respective studies. Again, different definitions of frailty limit comparability. Chang et al. (2013) utilized an expert assessment as the reference to test the accuracy of their home monitoring system [47]. The latter assessment was based on clinical routine instead of precise test results; therefore, it can be argued that it would have been appropriate to target identical test parameters. With regard to the other home-based assessment method by Hewson et al. (2013) it has to be noted that its validation was based on each single item of the criteria of Fried; however, outcomes were not compared to the original frailty criteria. The authors plan a longitudinal study to test technological performance, diagnostic capability based on two frailty definitions, usage and user friendliness. The user and authorized personnel gain access to the data via a remote server [49]. This is an important feature for the practical use of home monitoring systems. In this context questions concerning data protection and ethical aspects have to be addressed. Physical activity measurement with different methods appeared to be the most relevant component in the system by Theou et al. (2012) [7]. To improve the accuracy of this specific assessment methodology, a combination with other frailty-related parameters, such as strength, should be considered.
Measurement of activities of daily living and daily habits in the context of frailty
The literature also revealed two different sensor systems to detect daily activity patterns [10, 50]. One system was not intended to detect frailty but deterioration of functionality and overall health status [10]. In another project, changes in daily habits were evaluated. During the user-centered design process differences in opinion between researchers and clinicians emerged. While the researchers preferred having as many features and information as possible, clinicians preferred transparency and simplicity by focusing only on one single feature [50]. Various set-ups for the monitoring of health aspects and daily habits were developed but no cut-off values were calculated. Basic and routine ADL, such as handwashing or transfers, could be detected in older adults [11, 61, 62]. Further challenges in creating home monitoring systems for activity monitoring in pre-frail and frail older adults include cost-effectiveness and minimally invasive as well as unobtrusive solutions [50]. Robben et al. (2016) recently defined a model to assess functional health in a standardized way by using room sensors. Functional decline was detected in three case studies [63]. Further studies in pre-frail and frail older adults should follow. In the studies described, frailty definitions widely varied. The physical phenotype model (which is a mechanical model and therefore shows relevant overlap with other physical assessments and also with modern diagnostic criteria of sarcopenia) was predominantly used. The reported results must therefore be interpreted with caution against this background. A comprehensive evaluation of frailty definitions, including psychosocial factors, was not given in this review focusing on sensor-based assessments. Nevertheless, it became clear that an international consensus on the diagnosis of frailty is urgently needed. In addition, an international consensus on the standards of functional testing in frail individuals would also improve the overall comparability of results and would allow performance of meta-analysis in the future.
Limitations
One limitation of this review is that the literature search was only done in two major databases, PubMed and Cochrane. Potentially relevant results from other databases have not been included in this review. Another limitation is that only specific categories related to frailty were included in this review. Other categories, including “care”, “gerontechnology in general”, “ethical aspects”, “method assessment” and “user requirements and experiences” were excluded. Furthermore, cost-effectiveness was not addressed as up to now only one article has focused on this aspect [10]. In this overview, we did not specifically evaluate the quality of each single study. With the intention to provide a comprehensive overview on past and ongoing activities in this field, we included all studies not only those that in our perception had adequate quality and sample size. There is an ultimate need for future studies to be performed with high methodological quality, which must be based on adequate sample sizes and clearly stated a priori hypotheses. Up to now only very few studies fulfilled these criteria. Due to the widely varying test protocols and frailty definitions, we did not perform a meta-analysis.
Conclusion
Technology-based measurements seem to have high potential for diagnosing, monitoring and preventing (pre-)frailty. Specific sensor-derived parameters provided by wearable inertial sensors during gait, motor assessments and physical activity show high potential for the diagnosis, the monitoring and the prevention of (pre-)frailty. Several gait variables, including step width and trunk sway provide valuable information for an early diagnosis of (pre-)frailty. More variable outcomes in motor assessments may indicate more unstable performance in general. Further studies should test this hypothesis. Future studies with high methodological quality should be performed to validate these parameters in this population. In this context the importance of consistency in frailty diagnosis and of testing procedures has to be stressed. Furthermore, current findings are limited due to cross-sectional studies, which do not allow a causal relationship to be established. The relevance of outcome variables derived from gait, motor assessment and physical activity should be confirmed in larger cohorts and in daily routine. The definition used most frequently in aforementioned studies was the one provided by Fried et al. (2001) [21].
Sensor-derived parameters of specific ADL in (pre-)frail older adults have not been reported. As a loss of ability to participate in ADL could be a sign of becoming frail or a worsening frailty level, further studies should particularly focus on the ADL. Room sensors alone or in combination with wearable sensors seem appropriate for this approach. The attitude of older users towards wearable sensors has to be adequately appreciated in this context.
References
Collard RM, Boter H, Schoevers RA, Oude Voshaar RC (2012) Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc 60:1487–1492. doi:10.1111/j.1532-5415.2012.04054.x
Dapp U, Minder CE, Anders J, Golgert S, von Renteln-Kruse W (2014) Long-term prediction of changes in health status, frailty, nursing care and mortality in community-dwelling senior citizens-results from the Longitudinal Urban Cohort Ageing Study (LUCAS). BMC Geriatr 14:141. doi:10.1186/1471-2318-14-141
Daintith J (2009) A dictionary of physics, 6th edn. Oxford University Press, Oxford
Morgenstern U, Kraft M (eds) (2014) Biomedizinische Technik – Faszination, Einführung, Überblick. De Gruyter, Berlin
Greene BR, Doheny EP, O’Halloran A, Anne Kenny R (2014) Frailty status can be accurately assessed using inertial sensors and the TUG test. Age Ageing 43:406–411. doi:10.1093/ageing/aft176
Schwenk M, Mohler J, Wendel C, D’Huyvetter K, Fain M, Taylor-Piliae R, Najafi B (2015) Wearable sensor-based in-home assessment of gait, balance, and physical activity for discrimination of frailty status: baseline results of the Arizona frailty cohort study. Gerontology 61:258–267. doi:10.1159/000369095
Theou O, Jakobi JM, Vandervoort AA, Jones GR (2012) A comparison of physical activity (PA) assessment tools across levels of frailty. Arch Gerontol Geriatr 54:e307–e314. doi:10.1016/j.archger.2011.12.005
Thiede R, Toosizadeh N, Mills JL, Zaky M, Mohler J, Najafi B (2016) Gait and balance assessments as early indicators of frailty in patients with known peripheral artery disease. Clin Biomech (Bristol, Avon) 32:1–7. doi:10.1016/j.clinbiomech.2015.12.002
Regterschot GRH, Zhang W, Baldus H, Stevens M, Zijlstra W (2016) Accuracy and concurrent validity of a sensor-based analysis of sit-to-stand movements in older adults. Gait Posture 45:198–203. doi:10.1016/j.gaitpost.2016.02.004
Alexander GL, Rantz M, Skubic M, Koopman RJ, Phillips LJ, Guevara RD, Miller SJ (2011) Evolution of an early illness warning system to monitor frail elders in independent living. J Healthc Eng 2:337–363
Ranasinghe DC, Shinmoto Torres RL, Hill K, Visvanathan R (2014) Low cost and batteryless sensor-enabled radio frequency identification tag based approaches to identify patient bed entry and exit posture transitions. Gait Posture 39:118–123. doi:10.1016/j.gaitpost.2013.06.009
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med 6:e1000097. doi:10.1371/journal.pmed.1000097
Morley JE, Vellas B, van Kan GA, Anker SD, Bauer JM, Bernabei R et al (2013) Frailty consensus: a call to action. J Am Med Dir Assoc 14:392–397. doi:10.1016/j.jamda.2013.03.022
Cesari M, Prince M, Thiyagarajan JA, de Carvalho IA, Bernabei R, Chan P et al (2016) Frailty: an emerging public health priority. J Am Med Dir Assoc 17:188–192. doi:10.1016/j.jamda.2015.12.016
Morley JE (2014) Frailty screening comes of age. J Nutr Health Aging 18:453–454. doi:10.1007/s12603-014-0457-9
Rockwood K, Theou O, Walston J (2015) Operationalizing frailty using the frailty phenotype and deficit accumulation approaches. Interdiscip Top Gerontol Geriatr 41:66–73. doi:10.1159/000381164
Bandeen-Roche K, Seplaki CL, Huang J, Buta B, Kalyani RR, Varadhan R et al (2015) Frailty in older adults: a nationally representative profile in the united states. J Gerontol A Biol Sci Med Sci 70:1427–1434. doi:10.1093/gerona/glv133
Fabbri E, Zoli M, Gonzalez-Freire M, Salive ME, Studenski SA, Ferrucci Aging Multimorbidity L (2015) New tasks, priorities, and frontiers for integrated gerontological and clinical research. J Am Med Dir Assoc 16:640–647. doi:10.1016/j.jamda.2015.03.013
Buta BJ, Walston JD, Godino JG, Park M, Kalyani RR, Xue Q‑L et al (2016) Frailty assessment instruments: systematic characterization of the uses and contexts of highly-cited instruments. Ageing Res Rev 26:53–61. doi:10.1016/j.arr.2015.12.003
Drey M, Pfeifer K, Sieber CC, Bauer JM (2011) The Fried frailty criteria as inclusion criteria for a randomized controlled trial: personal experience and literature review. Gerontology 57:11–18. doi:10.1159/000313433
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J et al (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56:M146–M156
Kim M‑J, Yabushita N, Kim M‑K, Nemoto M, Seino S, Tanaka K (2010) Mobility performance tests for discriminating high risk of frailty in community-dwelling older women. Arch Gerontol Geriatr 51:192–198. doi:10.1016/j.archger.2009.10.007
Schwenk M, Howe C, Saleh A, Mohler J, Grewal G, Armstrong D, Najafi B (2014) Frailty and technology: a systematic review of gait analysis in those with frailty. Gerontology 60:79–89. doi:10.1159/000354211
Najafi B, Helbostad JL, Moe-Nilssen R, Zijlstra W, Aminian K (2009) Does walking strategy in older people change as a function of walking distance? Gait Posture 29:261–266. doi:10.1016/j.gaitpost.2008.09.002
Mohler MJ, Fain MJ, Wertheimer AM, Najafi B, Nikolich-Zugich J (2014) The Frailty syndrome: clinical measurements and basic underpinnings in humans and animals. Exp Gerontol 54:6–13. doi:10.1016/j.exger.2014.01.024
Martinez-Ramirez A, Martinikorena I, Gomez M, Lecumberri P, Millor N, Rodriguez-Manas L et al (2015) Frailty assessment based on trunk kinematic parameters during walking. J Neuroeng Rehabil 12:48. doi:10.1186/s12984-015-0040-6
Mohler MJ, Wendel CS, Taylor-Piliae RE, Toosizadeh N, Najafi B (2016) Motor performance and physical activity as predictors of prospective falls in community-dwelling older adults by frailty level: application of wearable technology. Gerontology. doi:10.1159/000445889
Moe-Nilssen R, Helbostad JL (2005) Interstride trunk acceleration variability but not step width variability can differentiate between fit and frail older adults. Gait Posture 21:164–170. doi:10.1016/j.gaitpost.2004.01.013
Gillain S, Petermans J (2013) Contribution of new techniques to study the gait in old populations. Ann Phys Rehabil Med 56:384–395. doi:10.1016/j.rehab.2013.05.002
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K (2013) Frailty in elderly people. Lancet 381:752–762. doi:10.1016/S0140-6736(12)62167-9
Galan-Mercant A, Cuesta-Vargas AI (2014) Differences in trunk accelerometry between frail and non-frail elderly persons in functional tasks. BMC Res Notes 7:100. doi:10.1186/1756-0500-7-100
Millor N, Lecumberri P, Gomez M, Martinez-Ramirez A, Izquierdo M (2014) Kinematic parameters to evaluate functional performance of sit-to-stand and stand-to-sit transitions using motion sensor devices: a systematic review. IEEE Trans Neural Syst Rehabil Eng 22:926–936. doi:10.1109/TNSRE.2014.2331895
Ganea R, Paraschiv-Ionescu A, Bula C, Rochat S, Aminian K (2011) Multi-parametric evaluation of sit-to-stand and stand-to-sit transitions in elderly people. Med Eng Phys 33:1086–1093. doi:10.1016/j.medengphy.2011.04.015
Galan-Mercant A, Cuesta-Vargas AI (2013) Differences in trunk accelerometry between frail and nonfrail elderly persons in sit-to-stand and stand-to-sit transitions based on a mobile inertial sensor. JMIR Mhealth Uhealth 1:e21. doi:10.2196/mhealth.2710
Millor N, Lecumberri P, Gomez M, Martinez-Ramirez A, Izquierdo M (2013) An evaluation of the 30-s chair stand test in older adults: frailty detection based on kinematic parameters from a single inertial unit. J Neuroeng Rehabil 10:86. doi:10.1186/1743-0003-10-86
Ganea R, Paraschiv-lonescu A, Aminian K (2012) Detection and classification of postural transitions in real-world conditions. IEEE Trans Neural Syst Rehabil Eng 20:688–696. doi:10.1109/TNSRE.2012.2202691
Greene BR, Doheny EP, Kenny RA, Caulfield B (2014) Classification of frailty and falls history using a combination of sensor-based mobility assessments. Physiol Meas 35:2053–2066. doi:10.1088/0967-3334/35/10/2053
Martinez-Ramirez A, Lecumberri P, Gomez M, Rodriguez-Manas L, Garcia FJ, Izquierdo M (2011) Frailty assessment based on wavelet analysis during quiet standing balance test. J Biomech 44:2213–2220. doi:10.1016/j.jbiomech.2011.06.007
Galan-Mercant A, Cuesta-Vargas AI (2014) Mobile Romberg test assessment (mRomberg). BMC Res Notes 7:640. doi:10.1186/1756-0500-7-640
Chen S, Honda T, Chen T, Narazaki K, Haeuchi Y, Supartini A, Kumagai S (2015) Screening for frailty phenotype with objectively-measured physical activity in a west Japanese suburban community: evidence from the Sasaguri Genkimon Study. BMC Geriatr 15:36. doi:10.1186/s12877-015-0037-9
Peters LL, Boter H, Buskens E, Slaets JPJ (2012) Measurement properties of the Groningen Frailty Indicator in home-dwelling and institutionalized elderly people. J Am Med Dir Assoc 13:546–551. doi:10.1016/j.jamda.2012.04.007
Song J, Lindquist LA, Chang RW, Semanik PA, Ehrlich-Jones LS, Lee J et al (2015) Sedentary behavior as a risk factor for physical frailty independent of moderate activity: results from the osteoarthritis initiative. Am J Public Health 105:1439–1445. doi:10.2105/AJPH.2014.302540
Soaz C, Diepold K (2015) Step detection and parameterization for diagnosis and monitoring of functional decline using a single waist-worn accelerometer. IEEE Trans Biomed Eng. doi:10.1109/TBME.2015.2480296
Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M (2008) Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc 40:181–188. doi:10.1249/mss.0b013e31815a51b3
McCullagh R, Brady NM, Dillon C, Horgan NF, Timmons S (2015) A review of the accuracy and utility of motion sensors to measure physical activity of frail older hospitalised patients. J Aging Phys Act. doi:10.1123/japa.2014-0190
Hollewand AM, Spijkerman AG, Bilo HJ, Kleefstra N, Kamsma Y, van Hateren KJ (2016) Validity of an accelerometer-based activity monitor system for measuring physical activity in frail elderly. J Aging Phys Act. doi:10.1123/japa.2014-0290
Chang Y‑C, Lin C‑C, Lin P‑H, Chen C‑C, Lee R‑G, Huang J‑S, Tsai T‑H (2013) eFurniture for home-based frailty detection using artificial neural networks and wireless sensors. Med Eng Phys 35:263–268. doi:10.1016/j.medengphy.2011.09.010
Fontecha J, Hervas R, Bravo J, Navarro FJ (2013) A mobile and ubiquitous approach for supporting frailty assessment in elderly people. J Med Internet Res 15:e197. doi:10.2196/jmir.2529
Hewson DJ, Jaber R, Chkeir A, Hammoud A, Gupta D, Bassement J et al (2013) Development of a monitoring system for physical frailty in independent elderly. Conf Proc IEEE Eng Med Biol Soc 2013:6215–6218. doi:10.1109/EMBC.2013.6610973
de Folter J, Gokalp H, Fursse J, Sharma U, Clarke M (2014) Designing effective visualizations of habits data to aid clinical decision making. BMC Med Inform Decis Mak 14:102. doi:10.1186/s12911-014-0102-x
Rockwood K, Andrew M, Mitnitski A (2007) A comparison of two approaches to measuring frailty in elderly people. J Gerontol Ser A Biol Sci Med Sci 62(7):738–743
Mitnitski AB, Mogilner AJ, Rockwood K (2001) Accumulation of deficits as a proxy measure of aging. The Sci World J 1:323–336. doi:10.1100/tsw.2001.58
Espinoza S, Fried L (2007) Risk factors for frailty in the older adult. Clin Geriatr 15(6):37–44
Rolfson DB, Majumdar SR, Tsuyuki RT, Tahir A, Rockwood K (2006) Validity and reliability of the Edmonton Frail Scale. Age Ageing 35(5):526–529. doi:10.1093/ageing/afl041
Weiss A, Herman T, Plotnik M, Brozgol M, Giladi N, Hausdorff JM (2011) An instrumented timed up and go: the added value of an accelerometer for identifying fall risk in idiopathic fallers. Physiol Meas 32:2003–2018. doi:10.1088/0967-3334/32/12/009
Regterschot GRH, Zhang W, Baldus H, Stevens M, Zijlstra W (2015) Sensor-based monitoring of sit-to-stand performance is indicative of objective and self-reported aspects of functional status in older adults. Gait Posture 41:935–940. doi:10.1016/j.gaitpost.2015.03.350
Marschollek M, Goevercin M, Wolf KH, Song B, Gietzelt M, Haux R, Steinhagen-Thiessen E (2008) A performance comparison of accelerometry-based step detection algorithms on a large, non-laboratory sample of healthy and mobility-impaired persons. Conf Proc IEEE Eng Med Biol Soc 2008:1319–1322. doi:10.1109/IEMBS.2008.4649407
Lindemann U, Zijlstra W, Aminian K, Chastin SFM, de Bruin ED, Helbostad JL, Bussmann JBJ (2013) Recommendations for standardizing validation procedures assessing physical activity of older persons by monitoring body postures and movements. Sensors (Basel) 14:1267–1277. doi:10.3390/s140101267
Coley B, Najafi B, Paraschiv-Ionescu A, Aminian K (2005) Stair climbing detection during daily physical activity using a miniature gyroscope. Gait Posture 22:287–294. doi:10.1016/j.gaitpost.2004.08.008
Geraedts HAE, Zijlstra W, van Keeken HG, Zhang W, Stevens M (2015) Validation and user evaluation of a sensor-based method for detecting mobility-related activities in older adults. PLOS ONE 10:e0137668. doi:10.1371/journal.pone.0137668
Ranasinghe DC, Shinmoto Torres RL, Sample AP, Smith JR, Hill K, Visvanathan R (2012) Towards falls prevention: a wearable wireless and battery-less sensing and automatic identification tag for real time monitoring of human movements. Conf Proc IEEE Eng Med Biol Soc 2012:6402–6405. doi:10.1109/EMBC.2012.6347459
Huisingh-Scheetz MJ, Kocherginsky M, Magett E, Rush P, Dale W, Waite L (2016) Relating wrist accelerometry measures to disability in older adults. Arch Gerontol Geriatr 62:68–74. doi:10.1016/j.archger.2015.09.004
Robben SMB, Pol MC, Buurman BM, Krose BJA (2016) Expert knowledge for modeling functional health from sensor data. Methods Inf Med. doi:10.3414/ME15-01-0072
Acknowledgements
We would like to thank Sandra Hellmers, Sebastian Fudickar and Thomas Gerhardy for the help with the literature search terms and the literature search.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
L. Dasenbrock, A. Heinks, M. Schwenk and J.M. Bauer state that they have no competing interests.
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Dasenbrock, L., Heinks, A., Schwenk, M. et al. Technology-based measurements for screening, monitoring and preventing frailty. Z Gerontol Geriat 49, 581–595 (2016). https://doi.org/10.1007/s00391-016-1129-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00391-016-1129-7