Abstract
Background
Superficial surgical site infections are a common post-operative complication. They also place a considerable financial burden on healthcare. The use of prophylactic negative pressure wound therapy has been advocated to reduce wound infection rates. However, there is debate around its routine use. The purpose of this trial is to determine if prophylactic negative pressure wound therapy reduces post-operative wound complications in patients undergoing laparotomy.
Methods/design
This multi-centre randomised controlled trial will compare standard surgical dressings (control) to two competing negative pressure wound therapy dressings (Prevena™ and PICO™). All patients will be over 18 years, who are undergoing an emergency or elective laparotomy. It is intended to enrol a total of 271 patients for the trial.
Discussion
The PROPEL trial is a multi-centre randomised controlled trial of patients undergoing laparotomy. The comparison of standard treatment to two commercially available NPWT will help provide consensus on the routine management of laparotomy wounds.
Trial registration
This study is registered with ClinicalTrials.gov (NCT number NCT03871023).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
In the era of enhanced recovery after surgery, improving modifiable peri-operative and post-operative factors is essential to improve patient outcomes [1, 2]. Surgical site complications are a major burden to the healthcare system [3]. Superficial site infections (SSIs) can complicate the post-operative course significantly, often necessitating a longer length of stay, antibiotic therapy, and re-intervention for wound issues [4, 5].
In recent years, there have been various advances in reducing surgical site infection rates [6,7,8,9]. Despite improvements, SSIs remain a common cause of post-operative morbidity [10], especially following colorectal and emergency abdominal surgery [11].
The use of a suction pump for treatment of infected wounds was first described by a number of Soviet scientists, with positive results for the treatment of suppurative wounds [12, 13]. Negative pressure wound therapy (NPWT) was then described as a novel therapy for chronic wounds, following a 1997 animal model study [14]. NPWT in open wound management has been well described and is now an established therapy [15,16,17].
NPWT as delivered by a surgical incision management system (SIMS) is a novel approach to improve wound healing. The use of NPWT on closed incisions was first described by Gomoll et al. This 2006 series of orthopaedic trauma cases demonstrated satisfactory healing [18]. Stannard et al showed a 1.9 times higher relative risk of infection among a control group when compared to NPWT in low extremity fractures [19]. It has subsequently been shown to reduce SSI rates in a variety of surgical procedures [20,21,22].
In a 2016 meta-analysis of 10 studies, reporting on 1311 incisions, a reduction in wound infection and seroma formation with NPWT was observed when compared to standard dressings. However, due to heterogeneity among the studies, no firm recommendations were made [23].
Recent RCTs estimate that the incidence of SSI for open visceral surgery range 15–25% when using standard dressings [24,25,26]. There remains debate over the efficacy of prophylactic NPWT for laparotomy incisions in the acute and elective care surgery setting.
PICO™ (Smith & Nephew) and Prevena™ (KCI) wound management systems are two of the most widely utilized NPWT. However, there has yet been no trial which directly compares these systems. The PICO trial (2017) showed a significant reduction in SSI rate and length of stay among patients with laparotomy wounds treated with the PICO dressing vs standard care [27]. In contrast, the NEPTUNE trial failed to show any difference in wound infection when comparing Prevena™ to standard dressings in colorectal surgery [28].
Patients undergoing elective or emergent laparotomy are at a higher risk of SSI. Given the significant patient morbidity and potential cost associated with SSI, there is a definite need for interventions to reduce its incidence. Overall, NPWT has been shown to have a positive impact on decreasing SSI. However, there is a current lack of evidence supporting its prophylactic use. We hypothesise that patients randomised to negative pressure wound therapy will have a lower incidence of SSI compared to those managed with standard dressings.
Methods/design
Study objectives
This is a prospective study to assess the efficacy of two competing wound management systems. The aim of this study is to determine if prophylactic negative pressure wound therapy confers a lower rate of superficial site infection or reduces wound complications in both emergency and elective laparotomy wounds. Ultimately, this may produce consensus on management of laparotomy wounds, improving the post-operative course and reducing costs.
Study design
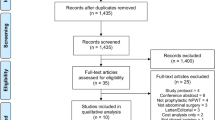
The PROPEL trial is a multi-centre, randomised controlled trial (RCT). Consent will be obtained from patients for entry to the trial during which discussion of the relevant procedure necessitating a laparotomy. Three treatment arms will be established. The control arm will receive a standard transparent waterproof dressing. The first treatment arm will receive a closed-incision negative pressure therapy device (Prevena™ Incision Management System, KCI, an Acelity company, San Antonio, TX), while the comparative (second) treatment arm will receive a closed-incision negative pressure therapy device (PICO™ Smith & Nephew Healthcare Ltd. Healthcare House 101 Hessle Road Hull HU3 2BN) (Fig. 1).
Primary and secondary endpoints
The primary endpoint of this study is presence of SSI with confirmation of microbiological infection at day 5 post-operative. The secondary endpoints include wound appearance at 30 days post-operative, wound appearance at 3 months post-operative, length of hospital stay, need for antibiotic use, and home wound care/use of antibiotics, hospital mortality.
Study population
Inclusion criteria:
-
Patients over 18 years
-
Emergency or elective laparotomies
-
Benign or malignant conditions
Exclusion criteria:
-
Pregnancy
-
Relook laparotomy
The study will run over an 18-month period, across four centres in the Republic of Ireland. The study hypothesis is that NPWT will result in a 20% reduction of SSI based on current literature [27]. Powering it at 90% with alpha and beta being 0.05 and 0.1, respectively, will mean that a total of 246 patients will be needed for statistical analysis. We will enrol 10% extra (total number = 271) to account for attrition and dropout.
Ethics
The PROPEL trial is designed and proposed in accordance with the principles of the Declaration of Helsinki and “good clinical practice” (GCP) guidelines. The protocol has been approved by the ethics committee at St. James Hospital Dublin and consent was obtained from other participating centres. Eligible patients presenting for laparotomy will be counselled, and written informed consent will be obtained. All three treatment strategies are generally accepted; therefore, there is no additional risk.
This study will receive no financial aid. Both products are already on the formulary of the included hospitals.
Randomisation and blinding
Patients will be randomized into one of the three groups using a computer-generated random number. Sealed envelopes will be placed in the operating theatre and used to identify dressings for patients at time of closure.
Wound closure
Wound closure will be performed in a standardised fashion as detailed below. Each centre will use a wound protector upon entering the peritoneal cavity and at all times attempt to keep contamination to a minimum.
-
Surgical gloves will be changed prior to commencement of closure and new clean instruments will be used.
-
The wound edges will be washed with povidone iodine after removing the wound protector.
-
The fascial layer will be closed with slowly absorbable monofilament (1–0 loop PDS).
-
Using the sterile ruler from a marking pen kit, this will be placed in the wound to calculate the depth of subcutaneous tissue from the fascial layer to the skin surface in centimetres; the skin will then be closed with skin clips with the wounds appropriately everted. The depth of the subcutaneous tissue will be recorded and the ruler removed and discarded
-
The length of the laparotomy wound will be calculated in centimetres and recorded.
-
The randomised dressing will then be applied.
-
In the event of NPWT failure, a new dressing will be applied.
Statistical analysis
The statistical data from this study will be reported in accordance with the guidelines set by the CONSORT consensus statement. Data will be analysed in clinically relevant categories with chi-squared analysis used to detect differences between groups.
Binary logistic regression modelling will be used. Multivariable models will be built to produce odds ratios (ORs) to account for the impact of predictive variables when assessing outcomes. The OR represents the odds of an adverse event (e.g., all-cause 30-day readmission) occurring. Variable selection will be based upon those which are statistically significant at univariable analysis, and those which are clinically significant but not statistical.
Study standards
Primary end points. Wounds will be inspected on the fifth post-operative day for any sign of superficial site infection/seroma/haematoma/abscess. The Southampton Scoring System [29] (illustrated in Appendix Table 1) will be employed to categorise the wound from grade I to grade V, ranging from normal healing to severe wound infection or haematoma. The wound will be swabbed on day 5 post-operative for culture and sensitivity. The swab will be taken from any area of exudation. If there is no exudate present, the swab will be taken at the proximal, middle and distal thirds of the wound. In the event of a subcutaneous collection, developing patients will be randomised to image-guided drainage or opening of the wound and packing.
Secondary end points. Wound healing will be evaluated again at 30 days and 3 months post-operatively, either on the ward or in the outpatient setting. Cosmetic appearance will be evaluated using the latest version of The Patient and Observer Scar Assessment Scale (POSAS) [30, 31] (illustrated in Appendix Figs. 2 and 3) Length of hospital stay, antibiotic use, and need for home wound care will also be recorded. Slice-o-matic software will be utilised on patients who undergo a pre-operative CT scan to assess the effect of subcutaneous adiposity and sarcopenia on SSI development.
Data collection
Variables to be collected:
-
Age, gender, body mass index, American Society of Anaesthesiologists Physical status classification system
-
Body fat percentage and muscle mass in patients who undergo pre-operative CT
-
Admission date and operation date
-
Operation/procedure performed
-
Type and location of wound
-
Indication
-
Co-morbidities; diabetes, immunosuppression, renal disease, cancer, etc.
-
Smoking status
-
Evidence of wound complication at post-operative day 5 (Appendix Table 1)
-
Method of management. (Radiological guided drainage versus opening of wound)
-
Length of hospital stay
-
Need for antibiotic therapy and duration of use
-
Duration of wound treatment in the community
Local data collection will be managed by surgical trainees at that hospital. This data will be stored on hospital password-protected computers in an Excel sheet with pseudo-anonymization applied.
Discussion
The PROPEL trial is the first randomized controlled trial comparing two competing NPWT (PICO™ and Prevena™). There is a lack of evidence supporting the use of prophylactic negative pressure wound therapy in general surgical laparotomies.
A 2018 meta-analysis by Sahebally et al. examining 1189 colorectal/general surgical incisions revealed a reduced SSI rate at 30 days [32]. However, of the three RCTs included in that study, only one examined a commercially available, single-use, wound management systems (PICO Trial) [27]. While there have been a number of prospective and retrospective publications examining NPWT, there remains a lack of high-quality, multi-centre RCTs. It is hoped that the PROPEL trial will contribute to the current literature and the development of guidelines for the routine use of NPWT following elective and emergency laparotomies.
The primary end point for this study is evidence of wound infection (SSI) at day 5 post-operatively. The Southampton Scoring System [29] was chosen with a view to standardising SSI diagnosis across the four centres partaking in this trial. This will help identify any difference in SSI overall incidence or severity between treatment arms. Various wound scoring systems exist, the Southampton system is among the most widely recognised and practical [33, 34]. It has been shown to be effective when used in routine post-operative follow-up [35]. POSAS will also be used to evaluate the scar at 30 days. This has been shown to be the most consistently reliable and feasible in comparison to other scar assessment scales [36, 37]. We have adopted the updated version of scale from the POSAS website.
Negative-pressure wound therapy improves healing in a variety of mechanisms. The hypoxic environment created at the wound site results in increased levels of circulating interleukins and increased growth factor expression, stimulating angiogenesis, granulation, and extracellular matrix remodelling [38, 39]. Negative pressure has been shown to stimulate micro-vessel stabilisation and maturation in the late stages of wound healing, resulting in increased angiogenesis and improved healing [40]. In addition, it has also been shown to reduce post-operative seroma formation, reduce bacterial bioburden and improve wound contraction [41,42,43].
SSIs are large source of expenditure for healthcare systems, with an estimated cost of over £90 million per year, largely due to increased length of stay [44]. Alternative strategies for reducing SSI rates, such as healing via secondary intention and traditional negative pressure canisters, are similarly costly while also being extremely labour intensive. In contrast, prophylactic NWPT devices, such as those examined in this study, are ergonomic, disposable and extremely compact. In select cases, this allows for patients to be discharged home with a device applied, but without the immobility associated with a traditional negative pressure device. While there is a significant cost associated with prophylactic NWP, this would be justified if NWPT was shown to infer a 15% reduction in SSI [45].
NPWT represents a wealth of potential benefit, not only for healthcare systems in the developed world but also in developing countries where SSI rates are significantly higher [46]. The prophylactic wound management systems in this study are single-use, easily applied and cheaper relative to the cost of managing SSIs. As new devices are developed, their costs may decrease significantly, making them more accessible and cost-effective [47]. Their use, along with education of healthcare providers, may play a significant role in reducing complications [46]. This trial will provide evidence regarding the efficacy of prophylactic NPWT at a time where the benefits are still contended.
References
Ljungqvist O, Scott M, Fearon KC (2017) Enhanced recovery after surgery: a review. JAMA Surg 152(3):292–298
Gustafsson UO et al (2019) Guidelines for perioperative care in elective colorectal surgery: enhanced recovery after surgery (ERAS). World J Surg 43(3):659–695
Pearson A (2009) Historical and changing epidemiology of healthcare-associated infections. J Hosp Infect 73(4):296–304
Smith RL et al (2004) Wound infection after elective colorectal resection. Ann Surg 239(5):599–605 discussion 605–7
Mangram AJ et al (1999) Guideline for prevention of surgical site infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control 27(2):97–132 quiz 133–4; discussion 96
McCartan DP et al (2013) Purse-string approximation is superior to primary skin closure following stoma reversal: a systematic review and meta-analysis. Tech Coloproctol 17(4):345–351
O'Leary DP et al (2013) Adhesive strip wound closure after thyroidectomy/parathyroidectomy: a prospective, randomized controlled trial. Surgery 153(3):408–412
Stulberg JJ et al (2010) Adherence to surgical care improvement project measures and the association with postoperative infections. JAMA 303(24):2479–2485
Dellinger EP et al (2005) Hospitals collaborate to decrease surgical site infections. Am J Surg 190(1):9–15
Mujagic E et al (2014) Evaluating the optimal timing of surgical antimicrobial prophylaxis: study protocol for a randomized controlled trial. Trials 15:188
Taylor GD et al (1995) The effect of surgical wound infection on postoperative hospital stay. Can J Surg 38(2):149–153
Davydov IA et al (1986) Vacuum therapy in the treatment of suppurative lactation mastitis. Vestn Khir Im I I Grek 137(11):66–70
Kostiuchenok BM et al (1986) Vacuum treatment in the surgical management of suppurative wounds. Vestn Khir Im I I Grek 137(9):18–21
Morykwas MJ, Argenta LC (1997) Nonsurgical modalities to enhance healing and care of soft tissue wounds. J South Orthop Assoc 6(4):279–288
Lord AC et al (2015) Successful management of abdominal wound dehiscence using a vacuum assisted closure system combined with mesh-mediated medial traction. Ann R Coll Surg Engl 97(1):e3–e5
Mukhi AN, Minor S (2014) Management of the open abdomen using combination therapy with ABRA and ABThera systems. Can J Surg 57(5):314–319
Bertelsen CA et al (2014) Outcome of negative-pressure wound therapy for open abdomen treatment after nontraumatic lower gastrointestinal surgery: analysis of factors affecting delayed fascial closure in 101 patients. World J Surg 38(4):774–781
Gomoll AH, Lin A, Harris MB (2006) Incisional vacuum-assisted closure therapy. J Orthop Trauma 20(10):705–709
Stannard JP et al (2012) Incisional negative pressure wound therapy after high-risk lower extremity fractures. J Orthop Trauma 26(1):37–42
Atkins BZ et al (2009) Does negative pressure wound therapy have a role in preventing poststernotomy wound complications? Surg Innov 16(2):140–146
Chadi SA et al (2014) Incisional negative pressure wound therapy decreases the frequency of postoperative perineal surgical site infections: a cohort study. Dis Colon Rectum 57(8):999–1006
Matatov T et al (2013) Experience with a new negative pressure incision management system in prevention of groin wound infection in vascular surgery patients. J Vasc Surg 57(3):791–795
Hyldig N et al (2016) Meta-analysis of negative-pressure wound therapy for closed surgical incisions. Br J Surg 103(5):477–486
Mihaljevic AL et al (2014) Multicenter double-blinded randomized controlled trial of standard abdominal wound edge protection with surgical dressings versus coverage with a sterile circular polyethylene drape for prevention of surgical site infections: a CHIR-Net trial (BaFO; NCT01181206). Ann Surg 260(5):730–737 discussion 737–9
Diener MK et al (2014) Effectiveness of triclosan-coated PDS Plus versus uncoated PDS II sutures for prevention of surgical site infection after abdominal wall closure: the randomised controlled PROUD trial. Lancet 384(9938):142–152
Pinkney TD et al (2013) Impact of wound edge protection devices on surgical site infection after laparotomy: multicentre randomised controlled trial (ROSSINI Trial). BMJ 347:f4305
O'Leary DP et al (2017) Prophylactic negative pressure dressing use in closed laparotomy wounds following abdominal operations: a randomized, controlled, open-label trial: the P.I.C.O. trial. Ann Surg 265(6):1082–1086
Murphy PB et al (2018) Negative pressure wound therapy use to decrease surgical nosocomial events in colorectal resections (NEPTUNE): a randomized controlled trial. Ann Surg 270(1):38-42
Bailey IS et al (1992) Community surveillance of complications after hernia surgery. BMJ 304(6825):469–471
Draaijers LJ et al (2004) The patient and observer scar assessment scale: a reliable and feasible tool for scar evaluation. Plast Reconstr Surg 113(7):1960–1965 discussion 1966–7
van de Kar AL et al (2005) Reliable and feasible evaluation of linear scars by the Patient and Observer Scar Assessment Scale. Plast Reconstr Surg 116(2):514–522
Sahebally SM et al (2018) Negative pressure wound therapy for closed laparotomy incisions in general and colorectal surgery: a systematic review and meta-analysis. JAMA Surg 153(11):e183467
Petrica A et al (2009) Accuracy of surgical wound infection definitions—the first step towards surveillance of surgical site infections. TMJ 59(3–4):362–365
Bruce J et al (2001) The quality of measurement of surgical wound infection as the basis for monitoring: a systematic review. J Hosp Infect 49(2):99–108
Reilly JS (1999) The effect of surveillance on surgical wound infection rates. J Tissue Viability 9(2):57–60
Idriss N, Maibach HI (2009) Scar assessment scales: a dermatologic overview. Skin Res Technol 15(1):1–5
Vercelli S et al (2009) How to assess postsurgical scars: a review of outcome measures. Disabil Rehabil 31(25):2055–2063
Glass GE et al (2014) Systematic review of molecular mechanism of action of negative-pressure wound therapy. Br J Surg 101(13):1627–1636
Huang C et al (2014) Effect of negative pressure wound therapy on wound healing. Curr Probl Surg 51(7):301–331
Ma Z et al (2016) Negative pressure wound therapy promotes vessel destabilization and maturation at various stages of wound healing and thus influences wound prognosis. Exp Ther Med 11(4):1307–1317
Weed T, Ratliff C, Drake DB (2004) Quantifying bacterial bioburden during negative pressure wound therapy: does the wound VAC enhance bacterial clearance? Ann Plast Surg 52(3):276–279 discussion 279–80
Banwell P, Withey S, Holten I (1998) The use of negative pressure to promote healing. Br J Plast Surg 51(1):79
López-Cano M, Armengol-Carrasco M (2013) Use of vacuum-assisted closure in open incisional hernia repair: a novel approach to prevent seroma formation. Hernia 17(1):129–131
Payne C, Edwards D (2014) Application of the single use negative pressure wound therapy device (PICO) on a heterogeneous group of surgical and traumatic wounds. Eplasty 14:e20
Heard C et al (2017) Cost-effectiveness analysis alongside a pilot study of prophylactic negative pressure wound therapy. J Tissue Viability 26(1):79–84
Sawyer RG, Evans HL (2018) Surgical site infection-the next frontier in global surgery. Lancet Infect Dis 18(5):477–478
Ramadhar AJ, Abraham F, McAllen C (2018) “Gravity” - a new simple negative pressure wound therapy self-build design for low income countries. J Med Eng Technol 42(7):518–524
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The protocol has been approved by the ethics committee at Tallaght University Hospital/St. James Hospital Dublin and consent was obtained from other participating centres.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Donlon, N.E., Boland, P.A., Kelly, M.E. et al. Prophylactic negative wound therapy in laparotomy wounds (PROPEL trial): randomized controlled trial. Int J Colorectal Dis 34, 2003–2010 (2019). https://doi.org/10.1007/s00384-019-03398-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-019-03398-9