Abstract
Purpose
Colonoscopy and flexible sigmoidoscopy are both recommended colorectal cancer (CRC) screening strategies, but their relative effectiveness is unclear. We sought to evaluate the ability of each of these two modalities to reduce CRC mortality.
Methods
We conducted a case-control study using the Surveillance, Epidemiology, and End Results (SEER)-Medicare database. Cases were persons aged 70–85 years who died of CRC and were matched to up to three non-CRC controls. Receipt of endoscopy was ascertained from Medicare claims and endoscopy indication assigned using a validated algorithm. Conditional logistic regression models were developed to estimate the association between screening colonoscopy or sigmoidoscopy and CRC mortality. We conducted secondary analyses by race, sex, and endoscopist characteristics, and with varying duration of the look-back period.
Results
In the initial analysis using all available look-back years, screening flexible sigmoidoscopy was associated with a 35% reduction in CRC mortality (OR 0.65, 95% CI 0.48, 0.89), while screening colonoscopy was associated with a 74% reduction (OR 0.26, 95% CI 0.23, 0.30). Sigmoidoscopy was not associated with any reduction in proximal CRC mortality. The association between colonoscopy and reduced CRC mortality was stronger in the distal than the proximal colon. Results were similar in analyses using a 5-year look-back period.
Conclusions
Screening colonoscopy was associated with greater reductions in CRC mortality than screening sigmoidoscopy, and with a greater reduction in the distal than the proximal colon. These results provide additional information on the relative benefits of screening for CRC with sigmoidoscopy and colonoscopy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Screening for colorectal cancer (CRC) in average-risk individuals is recommended beginning at the age of 45 or 50 years [1,2,3]. Screening options include colonoscopy, flexible sigmoidoscopy with or without fecal occult blood or immunochemical testing (FOBT/FIT), and FOBT/FIT alone. Direct evidence on the comparative effectiveness of these screening options is scarce. In the USA, colonoscopy is the most popular screening modality; however, its efficacy is supported primarily by observational evidence [4,5,6], and methodologic issues such as missing information on endoscopy indication may affect the validity of some studies [4, 5]. Specifically, many CRC mortality studies excluded colonoscopies performed within 3–6 months of cancer diagnosis, potentially over-estimating screening effectiveness [4, 5, 7,8,9]. To reduce bias, identifying the indications for exams such as colonoscopy or sigmoidoscopy is needed, with analysis of only screening or surveillance exams during the entire period when occult CRCs or their precursors are present [10].
Both colonoscopy and sigmoidoscopy can detect and remove polyps, potentially preventing malignant transformation and decreasing CRC incidence and mortality. Both can also provide early detection of asymptomatic cancers, which might further decrease mortality. Randomized controlled trials have demonstrated reductions in overall CRC incidence and mortality with screening sigmoidoscopy [11,12,13,14,15]. Randomized controlled trials of screening colonoscopy are ongoing, but definitive results will not be available until 2022 or 2026–2027 [16,17,18]. In a population-based screening program, colonoscopy has short-term disadvantages compared to flexible sigmoidoscopy, including higher complication risk [19], greater need for sedation, higher level of operator skill, and higher overall cost.
Because colonoscopy can examine the entire colon, its effectiveness in reducing mortality is hypothesized to be superior to that of flexible sigmoidoscopy, which only directly examines the distal colon. While randomized trials have shown flexible sigmoidoscopy to be less effective for reduction of proximal than distal CRC mortality [11,12,13,14], observational colonoscopy studies also suggest differences in effectiveness by location [4,5,6]. Therefore, the comparative effectiveness of colonoscopy and sigmoidoscopy needs clarification.
Direct comparisons of colonoscopy and sigmoidoscopy in the same population would be helpful to inform patients, providers, and policy makers about CRC screening options [20]. Thus, the aim of this study was to compare the effectiveness of screening colonoscopy and flexible sigmoidoscopy in reducing CRC mortality. We used linked data from the Surveillance, Epidemiology, and End Results (SEER) program and Medicare claims [21], as well as a validated algorithm to discern indications for colonoscopy and sigmoidoscopy [22].
Methods
Case selection and control identification
The SEER database collects population-based information on incident cancers, covering approximately 28% of the US population [21]. These data are linked to the corresponding Medicare claims via a deterministic algorithm [21]. Cause of death is ascertained by SEER from death certificates. Cases were defined as individuals aged 70 to 85 years with a first diagnosis of CRC between 1996 and 2013 who subsequently died of this malignancy. Potential cases who died of other causes were excluded. Age 70 was chosen as the minimal diagnosis age so that cases would have at least 5 years in which to assess screening history (i.e., the look-back period), as Medicare enrollment most commonly begins at age 65. Potential cases were excluded if they had a prior cancer diagnosis at another site in the SEER-Medicare data. Subjects were required to have had continuous enrollment in both Part A and B fee-for-service Medicare without health maintenance organization enrollment for at least 5 years prior to the diagnosis date to maximize claims completeness. Additional exclusion criteria included receipt of a barium enema or computed tomography (CT) colonography, or a diagnosis of CRC (International Classification of Disease-9-Clinical Modification [ICD-9-CM] codes V10.05, V10.06) or inflammatory bowel disease (ICD-9-CM codes 555.x, 556.x) more than 6 months prior to the cancer diagnosis date. Subjects were also excluded if they had evidence of a colorectal resection at any time prior to the cancer diagnosis date.
Controls were identified from the 5% SEER-Medicare non-cancer sample and were matched to cases by sex, calendar year of birth, race, and SEER region of residence at the reference date (the CRC diagnosis date for the matched case). Controls were required to have been alive at the date of death of their matched case. Controls had the same requirements for Medicare enrollment and medical history as cases, and had to have an available look-back period at least as long as that of their matched case. From the eligible pool, we randomly selected up to three controls per case. If fewer than three potential controls were available, we selected all available controls. Cases without available controls were dropped from analysis.
Identification of screening/surveillance flexible sigmoidoscopy and colonoscopy
We used International Classification of Disease-9-Procedures (ICD-9-P), Current Procedural Terminology (CPT), and Healthcare Common Procedure Coding System (HCPCS) codes in the Medicare Carrier, Outpatient, and MedPAR (inpatient) files to ascertain receipt of colonoscopy and flexible sigmoidoscopy (Supplemental Table 1). We used a validated algorithm to classify the indications for colonoscopy as screening, surveillance, or diagnostic [22]. This algorithm incorporates demographic information, ICD-9-CM diagnosis and CPT/HCPCS procedure codes from the colonoscopy claim and claims in the 12 months prior, and colonoscopy site of service. We adapted this algorithm to identify indications for sigmoidoscopy, as we expected similar coding patterns as for colonoscopy. Because of poor ascertainment in claims data, we did not consider use of FOBT [23]. The vast majority of inpatient colonoscopies and sigmoidoscopies were performed for diagnostic indications; therefore, all inpatient endoscopies were classified as diagnostic. Colonoscopies and sigmoidoscopies performed for diagnostic indications were ignored in the analysis, and only subjects with screening or surveillance procedures were considered exposed.
Definition of the look-back period for ascertainment of CRC screening histories
In studying CRC mortality, the goal is to evaluate screening procedures that occur in the combined pre-invasive detectable phase (PIDP) and occult invasive phase (OIP), collectively known as the detectable preclinical phase (Supplemental Figure 1) [24]. In the PIDP, premalignant lesions such as adenomatous polyps can be identified and removed, potentially preventing their malignant transformation and reducing CRC incidence and mortality. In the OIP, an invasive cancer is already present but is asymptomatic. Screening during the OIP can result in earlier stage at diagnosis, increasing CRC survival. If a cancer is detected through investigation of symptoms, the detectable preclinical phase has passed. Therefore, exams performed for symptom evaluation should be excluded when studying cancer mortality. The detectable preclinical period cannot be directly observed; however, the PIDP is commonly estimated at up to 10 years and the OIP at 1–2 years for CRC [25].
Due to SEER-Medicare linkage protocol constraints, eligible subjects had claims available for at least 5 to 7 years before the reference date, depending upon the reference date year [26]. For this study, we conducted analyses using look-back periods of all available years or restricted to 5 years.
Exposure classification
We defined three exposure categories: (1) no screening by lower endoscopy, (2) colonoscopy screening only, and (3) flexible sigmoidoscopy screening only. The no screening by lower endoscopy group included subjects without screening/surveillance colonoscopy or sigmoidoscopy during the look-back period. The colonoscopy screening group included subjects whose first or only screening/surveillance exam during the look-back period was a colonoscopy and who had no screening sigmoidoscopies. This group also included subjects with a surveillance sigmoidoscopy after a screening/surveillance colonoscopy. The flexible sigmoidoscopy screening group included subjects whose first or only screening endoscopy in the look-back period was a sigmoidoscopy and who had no screening colonoscopies. This group also included subjects with an initial screening sigmoidoscopy followed by one or more surveillance colonoscopies. We assumed that surveillance colonoscopies in this group were performed to follow-up on abnormalities in the initial flexible sigmoidoscopy. Potential cases with more complex exposures, such receipt of both screening colonoscopy and sigmoidoscopy, were excluded along with their matched controls because of ambiguity in attributing exposure.
Covariates
Covariates included demographic, clinical, and endoscopist variables, determined at the reference date. Demographic data included residential urbanicity based on the Rural-Urban Commuting Area system (RUCA) [27] and area-level socioeconomic status, defined as the median income of the residential ZIP code from US Census data. We classified comorbidity status using an adaptation of the Charlson comorbidity index developed for SEER-Medicare data [28]. We attempted to identify family history of CRC using ICD-9-CM code V16.0 (family history-gastrointestinal neoplasm). However, we believed ascertainment of family history of CRC was unreliable because a greater proportion of controls than cases had at least one claim with these codes, and did not include this variable in our analysis.
We classified endoscopist specialty by linking the National Provider Identification (NPI) or the Unique Physician Identification Number (UPIN) of the endoscopist on the procedure claim to the American Medical Association (AMA) Physician Masterfile [29, 30]. If the identifiers could not be linked to the Masterfile, we assigned the specialty listed on the Medicare claims. Endoscopist specialty was classified as gastroenterology, surgery (including general or colorectal surgery), primary care, and other/unknown. We determined endoscopists’ polyp detection rate by aggregating data across all their colonoscopy claims in the 5% non-cancer sample. Polyp detection rate was defined as the proportion of all colonoscopies with an ICD-9-CM code for colorectal polyp (Supplemental Table 1). We did not determine polyp detection rate for sigmoidoscopy and could not estimate adenoma detection rate because pathology data were not available. Endoscopist-related variables were classified as unknown/missing for the < 1% of the Carrier and Outpatient claims with multiple physician identifiers.
Data analysis
All analyses were conducted with SAS 9.4 (SAS Institute, Cary, North Carolina). Using conditional logistic regression models, we estimated the odds ratios (OR) and 95% confidence intervals (CI) for exposure to either colonoscopy or flexible sigmoidoscopy in cases compared to controls. All models were adjusted for comorbidity, residential median income, and residential urbanicity.
To minimize bias, we conducted separate analyses for flexible sigmoidoscopy and colonoscopy using analytic time periods when utilization of each modality was relatively stable [31]. Based on screening test utilization in the eligible potential controls (Supplemental Table 1), screening flexible sigmoidoscopy was most common between 1998 and 2002. Screening colonoscopy utilization increased after 2002 and thereafter remained stable. To allow for a sufficiently long look-back period and assuming a delay between screening initiation and CRC mortality reduction, we examined screening flexible sigmoidoscopy in cases diagnosed in 1996–2006 who died in 2004–2006 and screening colonoscopy in cases diagnosed in 1996–2013 who died in 2011–2013.
Our base-case analysis used all available years of data as the look-back period, with sensitivity analyses using a 5-year look-back period [32]. In all analyses, we tabulated receipt of screening for controls only within the available look-back period of their matched case.
We developed additional models stratified by sex, race, and cancer site (proximal colon, distal colon, unknown). The proximal colon was defined as the cecum through the splenic flexure, and the distal colon as the descending colon, sigmoid colon, and rectum. We also explored whether associations differed according to endoscopist characteristics.
Results
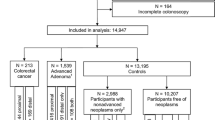
We identified 169,408 subjects as potential cases (Fig. 1). After applying exclusion criteria, 89,645 eligible cases remained. Matched controls were unavailable for 12,554 cases, leaving 77,091 incident cases available for analysis. We chose 5042 cases who died of CRC in 2004–2006 for the flexible sigmoidoscopy analysis, and 4548 cases who died in 2011–2013 for the colonoscopy analysis. The demographic characteristics of cases and controls were similar within each time period (Table 1). Approximately, 42–43% of cases had proximal tumors, depending on the analysis period (Table 2). Forty to 41% of cancers were diagnosed at distant stage.
Overall results
In the base-case flexible sigmoidoscopy analysis, 1.2% of cases had evidence of screening sigmoidoscopy vs. 1.6% of controls. In the base-case colonoscopy analysis, 6.5% of cases had evidence of screening colonoscopy vs. 21.2% of controls. Screening flexible sigmoidoscopy was associated with a 35% mortality reduction (OR 0.65; 95% CI 0.48, 0.89), while screening colonoscopy was associated with a 74% mortality reduction (OR 0.26; 95% CI 0.23, 0.30) (Table 3). In the sensitivity analysis using a 5-year look-back window, 0.9% of cases had evidence of screening sigmoidoscopy vs. 1.2% of controls, while 4.8% of cases had evidence of screening colonoscopy vs. 17.8% of controls. The magnitude of mortality reduction for both procedures was similar to the base-case analysis (Table 3).
Stratified analyses
Flexible sigmoidoscopy was associated with a 55% reduction in distal CRC mortality (OR 0.45, 95% CI 0.26, 0.77) but with no reduction in proximal CRC mortality (OR 0.84; 95% CI 0.56, 1.25) (Table 3). Colonoscopy was strongly associated with reductions in both distal (OR 0.17; 95% CI 0.13, 0.21) and proximal CRC (OR 0.38; 95% CI 0.32, 0.45). Colonoscopy was associated with similar mortality reductions in men and women, and in whites and blacks. Interpretation of subgroup results was limited for flexible sigmoidoscopy because of wide confidence intervals.
We found similar reductions in CRC mortality for colonoscopies performed by different endoscopist specialties (Table 4). There was a modest, non-significant trend towards greater reductions in CRC mortality associated with colonoscopies by providers in the highest quartile of polyp detection compared to the lowest quartile.
Discussion
We examined the effectiveness of screening flexible sigmoidoscopy and colonoscopy in reducing CRC mortality. While both procedures were associated with reductions in overall CRC mortality, the association was stronger for colonoscopy than for sigmoidoscopy. The association with screening colonoscopy was also stronger in the distal than the proximal colon, while screening sigmoidoscopy was not associated with any reduction in proximal CRC mortality. This study adds to prior literature by comparing the two screening modalities and by including only screening and surveillance colonoscopies, potentially reducing bias in our estimates. Use of the SEER-Medicare database allowed population-based ascertainment and inclusion of a large number of subjects, increasing precision of our estimates.
Our results are consistent with those obtained in randomized controlled trials of flexible sigmoidoscopy, although our subjects were generally older. The UK Flexible Sigmoidoscopy screening trial found a 31% reduction in overall CRC mortality after one-time screening sigmoidoscopy [11, 33]. The US PLCO flexible sigmoidoscopy trial found a 26% reduction in the risk of overall CRC death after screening sigmoidoscopy, with effects limited to the distal colon [12]. The NORCAPP trial also found a 27% reduction in CRC death after screening sigmoidoscopy, with benefits primarily seen in men after long-term follow-up [14, 15]. Finally, the Italian SCORE trial found a 38% reduction in CRC mortality after one-time screening sigmoidoscopy [13].
The reductions in CRC mortality with colonoscopy are consistent with prior observational studies. An analysis of the Nurses’ Health Study and the Health Professionals Follow-up Study found a 68% reduction in CRC mortality after screening colonoscopy, with stronger effects in the distal than proximal colon [6]. In a Canadian case-control study, any colonoscopy was associated with a 37% reduction in the odds of CRC death [4]. Similar case-control studies using SEER-Medicare and Veterans Administration data also found approximately 60% reductions in CRC death associated with colonoscopy, with similar differences by site [5, 34]. However, these three case-control studies were unable to determine indications for colonoscopy and excluded colonoscopies performed within 6 months of CRC diagnosis, likely introducing bias. A case-control study in the Kaiser Permanente population found a 67% reduction in the odds of death associated with screening colonoscopy, with similar reductions by cancer site [35]. In this study, only screening procedures were included.
We found similar reductions in CRC mortality associated with colonoscopies performed by different specialists. Interpretation of subgroup analyses for flexible sigmoidoscopy was limited because of the relatively small number of screening sigmoidoscopies identified. Although not statistically significant, we saw a suggestion of greater protection from CRC death after colonoscopy performed by an endoscopist with a high polyp detection rate. Others have found strong associations between adenoma detection rate and risk of interval cancers and death [36, 37].
Limitations of our study include potential inaccuracies in determining procedure indication. However, we used a validated algorithm with good discriminatory power for screening/surveillance vs. diagnostic procedures. Because of the structure of the SEER-Medicare database, the length of the available look-back period was somewhat limited, and we could not account for screening that might have occurred before the available look-back period. Nevertheless, sensitivity analyses using varying look-back periods gave similar results. We did not study the use of combined flexible sigmoidoscopy and FOBT due to potential incomplete ascertainment of FOBT. We were unable to reliably ascertain family history of CRC, but this may be a less important consideration in our older subjects.
Because of evolving patterns of screening utilization, we chose different time periods for the sigmoidoscopy and colonoscopy analyses to minimize bias [31]. This analytic choice may complicate interpretation of the comparative effectiveness of the two modalities. For example, if treatment of screen-detected CRC is improving over time, screening colonoscopy may appear to be more effective than sigmoidoscopy due to improved post-diagnosis survival in the later time periods. However, improved CRC treatment is unlikely to account for the entire magnitude of the differences seen here. Although we obtained data on specialty through the AMA Physician Masterfile for most endoscopists, for some, we were limited to information contained on the Medicare claims. Lastly, we were not able to directly examine endoscopists’ adenoma detection rates, but were limited to polyp detection rates. However, polyp detection and adenoma detection rates are correlated [38, 39].
In summary, we found that screening colonoscopy was associated with greater reductions in CRC mortality than screening sigmoidoscopy. For colonoscopy, the association was stronger in the proximal colon than the distal colon, and there was no reduction in mortality from proximal CRC associated with screening sigmoidoscopy. These results provide additional information about the relative effectiveness of the two screening modalities.
Funding support
This work was supported by a contract from the National Cancer Institute of the National Institutes of Health, HHSN261201600596P.
References
Wolf AMD, Fontham ETH, Church TR, Flowers CR, Guerra CE, LaMonte S, Etzioni R, McKenna M, Oeffinger KC, Shih YT, Walter LC, Andrews KS, Brawley OW, Brooks D, Fedewa SA, Manassaram-Baptiste D, Siegel RL, Wender RC, Smith RA (2018) Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J Clin 68:250–281
Bibbins-Domingo K, Grossman DC, Curry SJ et al (2016) Screening for colorectal cancer: US preventive services task force recommendation statement. JAMA 315:2564–2575
Rex DK, Boland CR, Dominitz JA et al (2017) Colorectal cancer screening: recommendations for physicians and patients from the U.S. multi-society task force on colorectal cancer. Am J Gastroenterol 112:1016–1030
Baxter NN, Goldwasser MA, Paszat LF, Saskin R, Urbach DR, Rabeneck L (2009) Association of colonoscopy and death from colorectal cancer. Ann Intern Med 150:1–8
Baxter NN, Warren JL, Barrett MJ, Stukel TA, Doria-Rose VP (2012) Association between colonoscopy and colorectal cancer mortality in a US cohort according to site of cancer and colonoscopist specialty. J Clin Oncol 30:2664–2669
Nishihara R, Wu K, Lochhead P, Morikawa T, Liao X, Qian ZR, Inamura K, Kim SA, Kuchiba A, Yamauchi M, Imamura Y, Willett WC, Rosner BA, Fuchs CS, Giovannucci E, Ogino S, Chan AT (2013) Long-term colorectal-cancer incidence and mortality after lower endoscopy. N Engl J Med 369:1095–1105
Brenner H, Chang-Claude J, Seiler CM, Rickert A, Hoffmeister M (2011) Protection from colorectal cancer after colonoscopy: a population-based, case-control study. Ann Intern Med 154:22–30
Weiss NS (1998) Analysis of case-control studies of the efficacy of screening for cancer: how should we deal with tests done in persons with symptoms? Am J Epidemiol 147:1099–1102
Weiss NS, Doria-Rose VP (2009) The effectiveness of colonoscopy in reducing mortality from colorectal cancer. Ann Intern Med 150:817–818
Weiss NS, McKnight B, Stevens NG (1992) Approaches to the analysis of case-control studies of the efficacy of screening for cancer. Am J Epidemiol 135:817–823
Atkin WS, Edwards R, Kralj-Hans I, Wooldrage K, Hart AR, Northover JMA, Parkin DM, Wardle J, Duffy SW, Cuzick J (2010) Once-only flexible sigmoidoscopy screening in prevention of colorectal cancer: a multicentre randomised controlled trial. Lancet 375:1624–1633
Schoen RE, Pinsky PF, Weissfeld JL, Yokochi LA, Church T, Laiyemo AO, Bresalier R, Andriole GL, Buys SS, Crawford ED, Fouad MN, Isaacs C, Johnson CC, Reding DJ, O'Brien B, Carrick DM, Wright P, Riley TL, Purdue MP, Izmirlian G, Kramer BS, Miller AB, Gohagan JK, Prorok PC, Berg CD, PLCO Project Team (2012) Colorectal-cancer incidence and mortality with screening flexible sigmoidoscopy. N Engl J Med 366:2345–2357
Segnan N, Armaroli P, Bonelli L, Risio M, Sciallero S, Zappa M, Andreoni B, Arrigoni A, Bisanti L, Casella C, Crosta C, Falcini F, Ferrero F, Giacomin A, Giuliani O, Santarelli A, Visioli CB, Zanetti R, Atkin WS, Senore C, and the SCORE Working Group (2011) Once-only sigmoidoscopy in colorectal cancer screening: follow-up findings of the Italian randomized controlled trial--SCORE. J Natl Cancer Inst 103:1310–1322
Holme O, Loberg M, Kalager M et al (2014) Effect of flexible sigmoidoscopy screening on colorectal cancer incidence and mortality: a randomized clinical trial. JAMA. 312:606–615
Holme O, Loberg M, Kalager M et al (2018) Long-term effectiveness of sigmoidoscopy screening on colorectal cancer incidence and mortality in women and men: a randomized trial. Ann Intern Med 168:775–782
Quintero E, Castells A, Bujanda L, Cubiella J, Salas D, Lanas Á, Andreu M, Carballo F, Morillas JD, Hernández C, Jover R, Montalvo I, Arenas J, Laredo E, Hernández V, Iglesias F, Cid E, Zubizarreta R, Sala T, Ponce M, Andrés M, Teruel G, Peris A, Roncales MP, Polo-Tomás M, Bessa X, Ferrer-Armengou O, Grau J, Serradesanferm A, Ono A, Cruzado J, Pérez-Riquelme F, Alonso-Abreu I, de la Vega-Prieto M, Reyes-Melian JM, Cacho G, Díaz-Tasende J, Herreros-de-Tejada A, Poves C, Santander C, González-Navarro A, COLONPREV Study Investigators (2012) Colonoscopy versus fecal immunochemical testing in colorectal-cancer screening. N Engl J Med 366:697–706
Bretthauer M, Kaminski MF, Loberg M et al (2016) Population-based colonoscopy screening for colorectal cancer: a randomized clinical trial. JAMA Intern Med 176:894–902
Dominitz JA, Robertson DJ, Ahnen DJ, Allison JE, Antonelli M, Boardman KD, Ciarleglio M, del Curto BJ, Huang GD, Imperiale TF, Larson MF, Lieberman D, OʼConnor T, OʼLeary TJ, Peduzzi P, Provenzale D, Shaukat A, Sultan S, Voorhees A, Wallace R, Guarino PD (2017) Colonoscopy vs. fecal immunochemical test in reducing mortality from colorectal cancer (CONFIRM): rationale for study design. Am J Gastroenterol 112:1736–1746
Levin TR, Conell C, Shapiro JA, Chazan SG, Nadel MR, Selby JV (2002) Complications of screening flexible sigmoidoscopy. Gastroenterology 123:1786–1792
Brett AS (2014) Flexible sigmoidoscopy for colorectal cancer screening: more evidence, persistent ironies. JAMA 312:601–602
SEER Program Overview. Available from: http://healthcaredelivery.cancer.gov/seermedicare/overview/. Accessed June 1, 2018
Ko CW, Dominitz JA, Neradilek M, Polissar N, Green P, Kreuter W, Baldwin LM (2014) Determination of colonoscopy indication from administrative claims data. Med Care 52:e21–e29
Schenck AP, Klabunde CN, Warren JL, Peacock S, Davis WW, Hawley ST, Pignone M, Ransohoff DF (2008) Evaluation of claims, medical records, and self-report for measuring fecal occult blood testing among medicare enrollees in fee for service. Cancer Epidemiol Biomark Prev 17:799–804
Weiss NS (1999) Case-control studies of the efficacy of screening tests designed to prevent the incidence of cancer. Am J Epidemiol 149:1–4
Kuntz KM, Lansdorp-Vogelaar I, Rutter CM, Knudsen AB, van Ballegooijen M, Savarino JE, Feuer EJ, Zauber AG (2011) A systematic comparison of microsimulation models of colorectal cancer: the role of assumptions about adenoma progression. Med Decis Mak 31:530–539
SEER-Medicare: Summary Table of Available Medicare Data for Cancer & Non-cancer Cases. 2017. Available from: https://healthcaredelivery.cancer.gov/seermedicare/medicare/table.html. Accessed June 1, 2018
Economic Research Service. Rural-Urban Continuum Codes: United States Department of Agriculture; 2013. Available from: http://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx. Accessed June 29, 2018
NCI Comorbidity Index Overview Bethesda, MD: National Cancer Institute. Available from: https://healthcaredelivery.cancer.gov/seermedicare/considerations/comorbidity.html. Accessed May 4, 2018
Ko CW, Dominitz JA, Green P, Kreuter W, Baldwin LM (2010) Specialty differences in polyp detection, removal, and biopsy during colonoscopy. Am J Med 123:528–535
Ko CW, Dominitz JA, Green P, Kreuter W, Baldwin LM (2010) Utilization and predictors of early repeat colonoscopy in Medicare beneficiaries. Am J Gastroenterol 105:2670–2679
Weiss NS, Dhillon PK, Etzioni R (2004) Case-control studies of the efficacy of cancer screening: overcoming bias from nonrandom patterns of screening. Epidemiology 15:409–413
Brenner H, Hoffmeister M, Stegmaier C, Brenner G, Altenhofen L, Haug U (2007) Risk of progression of advanced adenomas to colorectal cancer by age and sex: estimates based on 840,149 screening colonoscopies. Gut 56:1585–1589
Atkin W, Wooldrage K, Parkin DM, Kralj-Hans I, MacRae E, Shah U, Duffy S, Cross AJ (2017) Long term effects of once-only flexible sigmoidoscopy screening after 17 years of follow-up: the UK flexible sigmoidoscopy screening randomised controlled trial. Lancet 389:1299–1311
Kahi CJ, Pohl H, Myers LJ, Mobarek D, Robertson DJ, Imperiale TF (2018) Colonoscopy and colorectal cancer mortality in the veterans affairs health care system: a case-control study. Ann Intern Med 168:481–488
Doubeni CA, Corley DA, Quinn VP, Jensen CD, Zauber AG, Goodman M, Johnson JR, Mehta SJ, Becerra TA, Zhao WK, Schottinger J, Doria-Rose VP, Levin TR, Weiss NS, Fletcher RH (2018) Effectiveness of screening colonoscopy in reducing the risk of death from right and left colon cancer: a large community-based study. Gut 67:291–298
Corley DA, Jensen CD, Marks AR, Zhao WK, Lee JK, Doubeni CA, Zauber AG, de Boer J, Fireman BH, Schottinger JE, Quinn VP, Ghai NR, Levin TR, Quesenberry CP (2014) Adenoma detection rate and risk of colorectal cancer and death. N Engl J Med 370:1298–1306
Kaminski MF, Regula J, Kraszewska E, Polkowski M, Wojciechowska U, Didkowska J, Zwierko M, Rupinski M, Nowacki MP, Butruk E (2010) Quality indicators for colonoscopy and the risk of interval cancer. N Engl J Med 362:1795–1803
Boroff ES, Gurudu SR, Hentz JG, Leighton JA, Ramirez FC (2013) Polyp and adenoma detection rates in the proximal and distal colon. Am J Gastroenterol 108:993–999
Francis DL, Rodriguez-Correa DT, Buchner A, Harewood GC, Wallace M (2011) Application of a conversion factor to estimate the adenoma detection rate from the polyp detection rate. Gastrointest Endosc 73:493–497
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ko, C.W., Doria-Rose, V.P., Barrett, M.J. et al. Screening flexible sigmoidoscopy versus colonoscopy for reduction of colorectal cancer mortality. Int J Colorectal Dis 34, 1273–1281 (2019). https://doi.org/10.1007/s00384-019-03300-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-019-03300-7