Abstract
Background
Appendicitis can be secondary to caecal pathology (polyp or cancer). Increasing age is a risk factor for malignancy coexisting with appendicitis. There is an increased coexistence of cancer post-appendicectomy in patients aged 50–54 years. This study investigates whether post-appendicectomy patients aged over 40 years should receive further colorectal imaging and follow-up.
Methods
Retrospective data were collected for 1633 patients aged 40 years and over who underwent appendicectomy in a 10-year period (1st January 2004–31st December 2014). Data were analysed for patients with histological confirmation of acute appendicitis. Incidental appendicular tumours were excluded.
Results
One thousand fifty-five (64%) patients had histological confirmation of acute appendicitis (median age 52 years; range 40–96 years). Six hundred three patients (57%) were aged 40–54 years; 452 patients (43%) were aged 55 years or over. Twenty-six (2.5%) patients were investigated post-appendicectomy. Three (11.5%) had caecal pathology: 2 adenocarcinoma, 1 benign caecal polyp. Ten (2.2%) patients aged 55 years or over had caecal pathology. Seven (1.6%) were diagnosed with caecal cancer. No patients below age 54 years were diagnosed with caecal cancer. The incidence of caecal cancer in the study population was 0.66% (40–54.9 years 0%; 55 years and over 1.6%). Patients aged 55 years or over were more likely to develop caecal pathology than patients aged 40–54 years (p = 0.006). The odds ratio of developing caecal pathology was 6.8 times greater (95% CI 1.49–31.29) in people aged 55 years and over.
Conclusions
Patients aged 55 years or over who have undergone appendicectomy should be offered colonoscopy to exclude coexistent caecal pathology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Appendicitis is a common general surgical emergency. Luminal obstructions by faecolith, lymphoid hyperplasia or impacted stool are often causes of appendicitis, and appendicectomy continues to be the treatment of choice in acute appendicitis [1]. The majority of colon cancers are left-sided. However, coexisting caecal neoplasia can be associated with appendicitis. Neoplastic growth may obstruct the appendicular lumen, therefore causing appendicitis which may be the first manifestation of an underlying malignancy [1]. Appendicitis in patients aged over 40 years may be due to colorectal pathology and in particular, caecal cancer. Although underlying neoplasia is an uncommon cause of appendicitis [2], it is one that should be considered particularly in patients aged over 40 years.
The incidence and prevalence of appendicitis with coexisting malignancy of any kind as well as caecal cancer has been previously documented.
In their Asian population study of Taiwanese subjects, Wu et al. reported that the incidence of developing any type of cancer was 4.60 times higher in patients undergoing appendicectomy than their comparison group. 1.08% of patients undergoing appendicectomy developed some form of malignancy in the first 12 months after appendicectomy. The hazard ratio for developing colorectal cancer was 14.7 (99.9% CI 8.66–25.0) [3].
Lai et al. conducted a retrospective study of 1873 Taiwanese patients diagnosed with acute appendicitis. They report 0.85% of subjects had colorectal cancer at the time of appendicectomy or within 40 months of the initial operation. They suggest increasing age as a risk factor for malignancy coexisting with appendicitis with a mean age of 69.1 years in those patients that developed colorectal cancer. Their reported incidence of colorectal cancer in patients over age 40 years was 1.76% and 43% of all their patients had a caecal tumour [2]. Bizer et al. report 1.8% of patients aged 65 and over with proven appendicitis had underlying caecal pathology [4].
Colorectal cancer is a major health burden in modern health care systems. In the UK, it represents the second most common cause of cancer death with 40,000 new cases each year [5]. Atkin et al. suggest the incidence of all cause proximal colon cancer to be 37%. In their study, of the patients undergoing colonoscopy, 0.4% were detected to have proximal cancers and 18.8% adenomas [6]. Delays in diagnosis and treatment of colorectal cancer are known to have adverse effects on overall prognosis.
The association between colorectal cancer and appendicitis has been previously documented. However, the value of colonic imaging in patients aged 40 years or over has not been extensively investigated. There are no national recommendations to advise follow-up imaging investigations in patients aged over 40 years who have had an appendicectomy.
The aim of this study is to assess the incidence of caecal pathology in patients aged over 40 years who have undergone appendicectomy. This will allow development of strategies towards imaging the colon to prevent and detect early development of colorectal pathology.
Methods
Patients
This retrospective cohort study collected data for all patients aged 40 years or over who underwent appendicectomy between 1st January 2004 and 31st December 2014. Patients were identified using the hospital’s clinical coding electronic database. Operation notes were reviewed to confirm that these patients had undergone appendicectomy as the index procedure, rather than as part of a more extended procedure (e.g. right hemicolectomy or elective appendicectomy). The histology reports for all patients undergoing appendicectomy were reviewed. Patients with confirmed appendicitis on histology who had undergone appendicectomy as the index procedure were included for further analysis in this study.
The age of 40 years or over was chosen as much of the published evidence refers to patients in this age range. Subgroup analysis was performed for patients aged 40–54 years and those aged 55 years or over. This grouping also allowed comparison between ‘younger’ and ‘older’ patients to give an insight into any variance that may exist in the development of colorectal cancer in these groups.
Patients with appendicular pathology other than appendicitis as shown on histology were excluded from the main analysis. This project was approved by the hospital’s audit department (ID 3353).
Data
Data collected included demographics, date of appendicectomy, pre-operative imaging, histological diagnosis, follow-up imaging (radiological or endoscopic) and any operations within 24 months after initial appendicectomy. Comparison of the rates of caecal pathology (polyps and cancer) was made between age groups: patients aged 40–54 years, and 55 years and over. Patients with caecal pathology were identified by reviewing electronic reports for imaging and endoscopic procedures.
Statistical analysis
Descriptive statistics were used to characterise the data. Odds ratios were calculated to compare the association between developing caecal pathology and increasing age in patients post-appendicectomy. Statistical significance is taken as p < 0.05.
Results
A total of 1633 appendicectomies were performed during the study period. One thousand fifty-five (64%) of these were confirmed as appendicitis on histology. These patients with confirmed appendicitis on histology were included in the study cohort for further analysis. The median age of patients was 52 years (range 40–96 years). Six hundred three (57%) patients were aged 40–54 years. Four hundred fifty-two (43%) patients were aged 55 years or over (Table 1). In the age group 40–54 years, 333 (55%) patients were male and 269 (45%) were female. In the age group 55 years or over, 213 (47%) were male and 239 (53%) were female.
The overall incidence of caecal cancer in patients in this study was 0.7%. In patients aged 55 years and over, the incidence of caecal pathology (polyps and cancer) was 2.2% and the incidence of caecal cancer was 1.6%. No patients aged 40–54 years had caecal cancer.
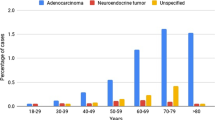
Twelve patients had some form caecal pathology (Table 2). Seven patients had caecal cancer (5 adenocarcinoma, 1 other bowel cancer, 1 metastatic cancer). Five patients had benign caecal polyps. No patients in the study cohort had inflammatory bowel disease.
Of the 7 patients that were diagnosed with caecal cancer, 3 had adenocarcinoma on returned histology immediately post-appendicectomy. One patient was detected to have caecal cancer 8 years after appendicectomy. One patient presented 6 years post-operatively with metastatic disease.
Three patients that were found to have caecal polyps underwent colonoscopy within 12 months post-appendicectomy. One of these patients had multiple polyps and went on to have an abdominoperineal resection.
Patients aged 55 years or over were statistically significantly more likely to have caecal pathology (polyp and cancer) than patients aged 40–54 years (p = 0.006). The odds ratio of developing caecal pathology (polyp and cancer) was 6.8 times greater (95% CI 1.49–31.29) in people aged 55 years and over compared with patients aged 40–54 years.
Ten patients had incidental appendicular pathology on histology (Table 3). One patient had an ascending colon tumour with subsequent palliative care management. Twenty-six (2.5%) patients received follow-up investigations for some form of bowel pathology post-appendicectomy (19 colonoscopy, 7 CT scan).
Discussion
The study confirms that patients aged 55 years and over presenting with appendicitis are more likely to have synchronous right-sided colon cancer. Of patients aged 55 years or over undergoing appendicectomy for acute appendicitis, a total of 2.2% (10/452) had some form of caecal pathology. 1.6% (7/452) of these patients were diagnosed with caecal cancer. None of the patients below age 54 years were diagnosed with caecal cancer in this study cohort.
This study supports the literature suggesting an association between caecal cancer and patients undergoing appendicectomy who are aged over 55 years.
Previous studies have reported similar incidences of appendicitis associated with caecal cancer. Lai et al. report such an incidence to be 0.85% in their cohort [2]. Bizer reports that 1.8% of patients aged 65 years or above presenting with signs of acute appendicitis had an underlying caecal cancer [4]. Khan et al. investigated patients aged over 40 years presenting with symptoms of acute appendicitis using computed tomography imaging and report a caecal cancer incidence of 1.25% [7]. Sylthe Pederson et al. show the incidence of caecal neoplasm (cancer and advanced adenoma) to be 1.5% in their retrospective study of patients post acute appendicitis [8].
The literature also recognises an increased risk of developing all types of colorectal cancer in patients undergoing appendicectomy. The population study of Taiwanese subjects by Wu et al. reports an overall hazard ratio of 14.7 (99.9% CI 8.66–2.50) for developing colorectal cancer across all ages. There is an increased risk of colorectal cancer in patients aged 45–64 years (HR 19.3, 99.9% CI 7.38–50.7) compared to those aged less than 45 years (HR 19.5, 99.9% CI 4.16–91.2) [3]. Lai et al. also present a similar pattern where the odds ratio of the incidence of colon cancer had a 38.5-fold increase among patients older than 40 with acute appendicitis compared to the general population [2].
A recent retrospective study performed in New Zealand [9] examined the rate of colorectal cancer in patients aged over 45 years presenting with appendicitis. They concluded that patients aged 45–60 years presenting with acute appendicitis had a greater than 17-fold increase of an underlying colorectal cancer than would be expected in the normal population.
In contrast, however, a Swedish population study found no excess risk for colorectal cancer in patients having undergone appendicectomy across all patients in their cohort [10]. They did not stratify for age—therefore, it is difficult to comment on the effect of age from this study.
Patients undergoing non-surgical management for acute appendicitis also show a similar pattern to the results in the current study. Enblad et al. carried out a population-based study in Sweden [11]. They showed that patients presenting with appendicitis across all ages over 20 years who undergo non-surgical management show an increased overall incidence of colorectal cancer compared to the general population. The standardised incidence ratio for right-sided cancer is 7.5 (95% CI 6.6–8.6). This is greater than that for left-sided tumours (SIR 1.4, 95% CI 0.98–2.1).
The application of Taiwanese, New Zealand and Swedish results to a UK population is difficult, although there is a general concordance towards a higher incidence of caecal cancer, and more strongly of all types of colorectal cancer in patients presenting with acute appendicitis. Variation in results from multiple studies may be explained by factors such as geography, homogeneity of populations investigated, study design, statistical powering and systematic error.
The incidence of colorectal cancer is strongly related to increasing age. In the UK in 2013–2015, 44% of all new cases per year were in people aged 75 years and over.
Age-specific incidence rates rise steeply after age 50 years: in the age group 50–54 years, the incidence per 100,000 UK population per year is 46.9 and 38.1 in males and females respectively. This increases to 84.6 and 61.5 in males and females respectively in the age group 55–59 years [12].
By anatomical site, right-sided colorectal cancer (caecum and ascending colon) accounts for 19% in males and 27% in females [13]. This pattern of distribution is similar for western populations where one third of colorectal cancers tend to be right-sided [9]. However, there is evidence to suggest that there is a shift towards right-sided malignancy with increasing age [6, 14]. In relation to the current question, where the majority of neoplasms are right-sided, and more frequent in older patients, emphasis should be placed on targeted investigation for this specific population.
It is important to consider the possibility of caecal carcinoma in patients aged over 55 years with presenting symptoms of appendicitis. Patients can present with adenocarcinoma of the appendix. Appendiceal adenocarcinoma is rare. However, synchronous colorectal neoplasia has been reported in 3–5% of patients with appendiceal neoplasia [15]. Therefore, at the very least, these patients should receive colonic investigation if such pathology is found on histological examination of the appendix.
Older patients presenting with symptoms of acute appendicitis are often investigated with a CT scan upon presentation to the acute surgical take. An argument may be made for no further investigation after reassurance of no sinister pathology on initial CT scan. However, diagnosis of colonic malignancy is difficult on CT scan, especially in the setting of acute appendicitis and an unprepared bowel. Therefore, even if pre-operative CT scan is reassuring, post-operative colonic imaging should be considered.
There is a wide variation in follow-up for patients aged over 55 years post-appendicectomy in the unit. The use of colonoscopy to investigate these patients post-appendicectomy is perhaps a powerful tool.
The overall performance of colonoscopy as a general screening tool for colorectal cancer has been shown to be satisfactory for adenoma detection and caecum intubation. Bretthauer et al. report the incidence of colorectal cancer to be 0.5% with comparable adenoma yield in both the proximal and distal colon [16]. Bokemeyer et al. report a similar incidence of 0.77% in their prospective study. They also confirm an increase in age-related incidence of both cancer and advanced adenomas [17]. Looking more specifically at patients post acute appendicitis, colonoscopy demonstrates the incidence of all types of colorectal cancer to be 1.2% with advanced adenomas 3% [8].
Given the higher prevalence of colorectal cancer in older patients in the general population alongside a further inflated risk of colorectal neoplasia coexisting with appendicitis in these older patients, a collective approach to establishing follow-up for this group would help to improve patient outcomes. Planned and agreed protocols guiding follow-up after appendicectomy towards diagnosis of colon cancer could help to prevent multiple procedures and operations.
Our results would support the recommendation that follow-up with colonoscopy in post-appendicectomy patients aged over 55 years would contribute to earlier detection of colorectal pathology. However, this is a single-centre study and generalisability to a wider UK population may be difficult without further validation. Although our sample size was similar to other studies investigating this question, a prospective, multi-centre study across the UK would provide the much-needed guidance.
Development of a risk stratification model for right-sided colorectal cancer in patients presenting primarily with acute appendicitis would serve to benefit patients through early identification of possible malignancy [6].
Increasing age is one such predictor of risk presented in the current study. As previously discussed, age-specific incidence rates increase sharply at ages 50–54 years [12]. Such stratification would be especially useful to detect pathology earlier in older patients, thereby improving overall outcomes and reducing the associated health care burden.
Conclusion
Our study supports published evidence that appendicitis is associated with an increased risk of caecal cancer, particularly in patients aged over 55 years. Clinicians should be aware to take into account patient-specific factors that may suggest an increased risk of colorectal cancer in patients aged 55 years or over.
Patients aged over 55 years who have undergone appendicectomy for acute appendicitis should receive appropriate and timely investigation for colorectal cancer.
Change history
15 February 2019
The above article originally published with an error present in Table 1 and is now presented correctly in this article.
References
Bhangu A, Soreide K, Di Saverio S, Assarsson JH, Drake FT (2015) Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet 386(10000):1278–1287
Lai H-W, Loong C-C, Tai L-C, Wu C-W, Lui W-Y (2006) Incidence and odds ratio of appendicitis as first manifestation of colon cancer: a retrospective analysis of 1873 patients. J Gastroenterol Hepatol 21(11):1693–1696
Wu SC, Chen WTL, Muo CH, Sung FC (2015) Appendicitis as an early manifestation of subsequent malignancy: an Asian population study. PLoS One 10(4)
Bizer LS (1993) Acute appendicitis is rarely the initial presentation of cecal cancer in the elderly patient. J Surg Oncol 54(1):45–46
World Health Organisation [Internet]. Available from: http://www.who.int/mediacentre/factsheets/fs297/en/. Accessed 5 May 2018
Atkin WS, Edwards R, Kralj-Hans I, Wooldrage K, Hart AR, Northover JMA, Parkin DM, Wardle J, Duffy SW, Cuzick J (2010) Once-only flexible sigmoidoscopy screening in prevention of colorectal cancer: a multicentre randomised controlled trial. Lancet 375(9726):1624–1633
Khan SA, Khokhar HA, Nasr ARH, Carton E (2013) Incidence of right-sided colonic tumors (non-appendiceal) in patient’s ≥40 years of age presenting with features of acute appendicitis. Int J Surg 11(4):301–304. https://doi.org/10.1016/j.ijsu.2013.02.004
Sylthe Pedersen E, Stornes T, Rekstad LC, Martinsen TC (2018) Is there a role for routine colonoscopy in the follow-up after acute appendicitis? Scand J Gastroenterol 53(8):1008–1012. Available from: https://www.tandfonline.com/doi/full/10.1080/00365521.2018.1485732. Accessed 2018
Shine RJ, Zarifeh A, Frampton C, Rossaak J (2017) Appendicitis presenting as the first manifestation of colorectal carcinoma: a 13-year retrospective study. N Z Med J 130(1459):25–32
Song H, Abnet C, Andren-Sandberg A, Chaturvedi A, Ye W (2016) Risk of gastrointestinal cancers among patients with appendectomy: a large-scale Swedish register-based cohort study during 1970-2009. Plos One 11(3):e0151262
Enblad M, Birgisson H, Ekbom A, Sandin F, Graf W (2017) Increased incidence of bowel cancer after non-surgical treatment of appendicitis. Eur J Surg Oncol 43(11):2067–2075. https://doi.org/10.1016/j.ejso.2017.08.016
Cancer Research UK. Incidence of colorectal cancer by age. [Internet]. Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/bowel-cancer/incidence#ref-. Accessed 27 Oct 2018
Cancer Research UK. Distribution of colorectal cancer by anatomical location [Internet]. Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/bowel-cancer/incidence#heading-Four. Accessed 27 Oct 2018
Meza R, Jeon J, Renehan AG, Luebeck EG (2010) Colorectal cancer incidence trends in the United States and United Kingdom: evidence of right- to left-sided biological gradients with implications for screening. Cancer Res 70(13):5419–5429
Khan MN, Moran BJ (2007) Four percent of patients undergoing colorectal cancer surgery may have synchronous appendiceal neoplasia. Dis Colon Rectum 50:1856–1859
Bretthauer M, Kaminski MF, Løberg M, Zauber AG, Regula J, Kuipers EJ, Hernán MA, McFadden E, Sunde A, Kalager M, Dekker E, Lansdorp-Vogelaar I, Garborg K, Rupinski M, Spaander MCW, Bugajski M, Høie O, Stefansson T, Hoff G, Adami HO, for the Nordic-European Initiative on Colorectal Cancer (NordICC) Study Group (2016) Population-based colonoscopy screening for colorectal cancer : a randomized clinical trial. JAMA Intern Med 176(7):894–902
Bokemeyer B, Bock H, Huppe D, Duffelmeyer M, Rambow A, Tacke W et al (2009) Screening colonoscopy for colorectal cancer prevention: results from a German online registry on 269 000 cases. Eur J Gastroenterol Hepatol 21(6):650–655
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard tojurisdictional claims in published maps and institutionalaffiliations.
Statement—‘What does this paper add to the literature?’
Increasing age is a significant risk factor contributing to appendicitis secondary to colorectal cancer. This study confirms that patients aged over 55 years post-appendicectomy are at increased risk of synchronous colorectal cancer. Results are in line with published literature and build the case for targeted colorectal screening for these patients.
Rights and permissions
About this article
Cite this article
Mohamed, I., Chan, S., Bhangu, A. et al. Appendicitis as a manifestation of colon cancer: should we image the colon after appendicectomy in patients over the age of 40 years?. Int J Colorectal Dis 34, 527–531 (2019). https://doi.org/10.1007/s00384-018-03224-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-018-03224-8