Abstract
Purpose
Previous studies have demonstrated that obese patients (BMI >30) undergoing laparoscopic colectomy have longer operative times and increased complications when compared to non-obese cohorts. However, there is little data that specifically evaluates the outcomes of obese patients based on the degree of their obesity. The aim of this study was to evaluate the impact of increasing severity of obesity on patients undergoing laparoscopic colectomy.
Methods
A retrospective review was performed of all patients undergoing laparoscopic colectomy between 1996 and 2013. Patients were classified according to their BMI as obese (BMI 30.0–39.9), morbidly obese (BMI 40.0–49.9), and super obese (BMI >50). Main outcome measures included conversion rate, operative time, estimated blood loss, post-operative complications, and length of stay.
Results
There were 923 patients who met inclusion criteria. Overall, 604 (65.4%), 257 (27.9%), and 62 (6.7%) were classified as obese (O), morbidly obese (MO), and super obese (SO), respectively. Clinicopathologic characteristics were similar among the three groups. The SO group had significantly higher conversion rates (17.7 vs. 7 vs. 4.8%; P = 0.031), longer average hospital stays (7.1 days vs. 4.9 vs. 3.4; P = 0.001), higher morbidity (40.3 vs. 16.3 vs. 12.4%; P = 0.001), and longer operative times (206 min vs. 184 vs. 163; P = 0.04) compared to the MO and O groups, respectively. The anastomotic leak rate in the SO (4.8%; P = 0.027) and MO males (4.1%; P = 0.033) was significantly higher than MO females (2.2%) and all obese patients (1.8%).
Conclusion
Increasing severity of obesity is associated with worse perioperative outcomes following laparoscopic colectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Early in the laparoscopic era, obesity was considered a relative contraindication to a minimally invasive approach [1]. It is now known that rather than being a detriment, laparoscopy is actually beneficial to obese patients. Compared to open colectomy cases, obese patients undergoing a laparoscopic operation have decreased overall morbidity, fewer wound complications, less post-operative pain, shorter average hospital stays, and decreased mortality [2]. Previous studies have also demonstrated that obese patients [body mass index (BMI >30)] undergoing laparoscopic colectomy have worse perioperative outcomes including longer operative times and increased complications when compared to non-obese (BMI <30) cohorts undergoing identical procedures [3,4,5,6,7,8,9,10]. However, there is little data that specifically compares the challenges and outcomes of obese patients based on the degree of their obesity. We therefore aimed to evaluate the impact of the severity of obesity on perioperative outcomes in patients undergoing laparoscopic colectomy.
Methods
Following institutional review board (IRB) approval, we retrospectively reviewed the data of all patients undergoing laparoscopic colectomy between 1996 and 2013 by three surgeons at the Texas Endosurgery Institute and University Hospitals Cleveland Medical Center. Patients meeting inclusion criteria were identified by the International Classification of Diseases (ICD), 9th revision procedure codes for laparoscopic colectomy, which included 44,204–44,213. Patients were then classified according to BMI as obese (O, BMI 30.0–39.9), morbidly obese (MO, BMI 40.0–49.9), and super obese (SO, BMI >50) in conjunction with previously described World Health Organization (WHO) definitions [11]. Patients in whom colectomy was performed in conjunction with other surgical procedures and those with incomplete records were excluded from analysis. All patients underwent traditional straight laparoscopy and this series included no patients with hand-assist procedures. The primary outcomes of interest included open conversion rate, operative time (minutes), estimated blood loss (mls), post-operative complications, and post-operative length of stay in days, which were compared in O, MO, and SO cohorts. Complications were divided into wound, ileus, anastomotic leak, and systemic (i.e., sepsis, fever, pneumonia, urinary tract infection, etc.). Anastomotic leak was defined as either clinical leak requiring drainage of an abscess or return to the operating room, as well as those confirmed radiographically by CT or contrast enema.
Univariate analysis was performed using independent sample t tests, analysis of variance (ANOVA), or chi-square tests as appropriate. Statistical analysis was performed using PASW Statistics 18.0 (SPSS Inc., Chicago, Illinois) and significance was set at P < 0.05.
Results
We identified 923 patients (50.4% male) that met inclusion criteria. From these, 604 (65.4%), 257 (27.9%), and 62 (6.7%) were classified as O, MO, and SO, respectively. Clinicopathologic characteristics were similar among the three groups with the exception of the underlying diagnosis (Table 1).
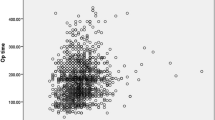
Table 2 lists the primary and secondary outcome measures. SO patients had significantly longer mean operative times (206 min; range, 75–508) compared to both O (163 min; range, 60–360) and MO patients (164 min; range, 60–440, P = 0.01). Similarly, SO patients had higher conversion rates when compared to both the O and MO cohorts (17.7 vs. 6.3 and 7.0%, P = 0.035).
While intra-operative complications, including bowel injury, ureter injury, or major vascular injury were similar among the cohorts (O 2.6 vs. MO 3.5 vs. SO 3.2%; P > 0.05); overall post-operative morbidity was higher in the SO group (40.3 vs. O 12.4 vs. MO 16.3%. P = 0.001). This included higher rates of wound infection (P < 0.001) and anastomotic leak including peri-anastomotic abscess (P = 0.027) for SO patients. MO males (p = 0.033) also had higher rates of anastomotic leak when compared to MO females and O patients of either gender. Post-operative ileus longer than 7 days was similar between the groups (P = 0.065). Systemic complications excluding urinary tract infections were similar among all three cohorts (P > 0.05). These complications in O patients included: pulmonary embolus (6), DVT alone (6), pneumonia (5), and myocardial infarction (4); MO patients included: pulmonary embolus (2), MI (1), and DVT (1); and SO patients with pulmonary embolus (1) and MI (2).
Finally, the average length of stay in the O (3.9 days, range 2–12) and MO groups (4.9 days, range 2–12) was significantly less than the SO cohort (6.7 days, range 2–27; P < 0.001).
Discussion
In the present manuscript, we have demonstrated that worse perioperative outcomes are directly correlated with increasing severity of obesity following laparoscopic colectomy. Previous studies have compared the outcomes of laparoscopic colectomy in non-obese patients to obese patients and, not surprisingly, found worse overall outcomes in the obese group, similar to other types of operations for both open and minimally invasive approaches [12, 13]. In contrast, our goal was to distinguish the impact of rising BMI within a cohort where all patients meet obesity criteria. To our knowledge, there have not been any large-scale institutional studies specifically comparing the outcomes of obese patients based on the severity and category of their obesity following laparoscopic colectomy.
Our finding of longer operative times in the SO group is somewhat expected. With increasing BMI, both the abdominal wall and visceral adiposity are increased, adding to the technical complexity of the operation [14]. Rising obesity is associated with a greater sized omentum and loss of domain within the abdomen to create space for proper exposure [15]. Furthermore, the increased adipose tissue in the mesentery often can lead to greater difficulty identifying critical structures such as the ureter and vascular pedicle prior to ligation. While mean operative times for O and MO cohorts were similar, this may be more of a reflection of the experience of the surgeon with operating in these two cohorts, as the rates of obesity (while somewhat steadying) continue to increase to the point that these are more routinely encountered patients [16, 17].
Similarly, it was somewhat expected that our rates of conversion to open increased with rising BMI. Prior studies have shown increased conversion rates to an open procedure when comparing non-obese (~5–15%) to obese (7–25%) patients [9, 18,19,20]. While our results showed a lower conversion rate than previously reported of only 4.8% in patients with a BMI of 30–40 and 7.0% in those with a BMI of 40–50, this is again likely a reflection of the increasing experience with both laparoscopic colectomy in general, as well as its use in obese patients. Yet, once the BMI rises above 50, the conversion rate appears to climb, consistent with Tekkis and associates, who found that conversion rates increase per unit of BMI (odds ratio = 1.7) [21]. It will be interesting, if in the future as experience with minimally invasive colectomy in the SO cohort increases, whether this trend will reverse. Similar to previous reports, higher T stage and previous abdominal surgery remain risk factors for conversion to open procedures [22]. Additionally, there is some data to suggest that hand-assist surgery in the MO patient may be associated with decreased rates of conversion, especially early in the surgeon’s learning curve [23].
Complication rates of 13–30% have been reported in non-obese patients undergoing laparoscopic colectomy [12, 18]. This is comparable to our results for patients with a BMI of 30–40 (13.1%). We found a slight increase in complication rate when patients’ BMI increased to between 40 and 50 (15.9%), and even higher overall complication rate for the SO cohort (41.4%), as well as when stratifying by individual complications such as wound infections, post-operative ileus, intra-abdominal abscess, and anastomotic leaks (0.2 vs. 1.2 vs. 13.8%). Previous authors have similarly demonstrated a higher rate of wound, ileus, and anastomotic leakage with comparing obese patients to non-obese [24,25,26]. Causey and associates have previously demonstrated in a population-based series of Crohn’s patients undergoing bowel resection that with every increase in BMI, the overall complication rate rose by 0.7% (95% CI 0.45–1.04%), which remained consistent with stratification by both open (0.6%) and laparoscopic approaches (1.1%; 95% CI 0.6–1.6%) [11]. However, this series included small intestine, colon, and rectal procedures and was dedicated to patients with Crohn’s disease. Prior studies have also shown significant differences in both gastrointestinal recovery and length of stay between non-obese and obese patients, with non-obese having improved outcomes in each arena [18]. Our results demonstrate this trend continues with the super obese; as post-operative length of stay also showed a similar trend with the SO cohort having even longer hospitalizations.
We acknowledge certain limitations to the present analysis. The mere nature of a retrospective analysis carries a potential source of bias related to the chart review and recording procedures. In addition, while this series was multi-institutional, all of the surgeons were extensively experienced in performing laparoscopic colectomy and the numbers may not reflect the general population as a whole. However, this is likely to be demonstrated only in lowering the overall numbers of complications and conversions, rather than the trend that was identified. Finally, the SO cohort is relatively small compared to the other two groups, composed of only 62 patients. With a larger collection of SO patients, and increasing experience in this group, our results may be altered somewhat. However, despite these limitations, we present the largest series to our knowledge of obese patients undergoing laparoscopic colectomy that have been specifically analyzed by the degree and severity of rising BMI and have demonstrated the negative impact on outcomes—even with experienced surgeons.
Conclusions
In this series of obese patients, we found that the severity of a patient’s obesity is directly correlated with their outcome, with SO patients demonstrating the most dramatic impact when compared to both MO and O patients. While laparoscopic colectomy in all patients requires meticulous perioperative care and sufficient laparoscopic experience, colorectal surgeons must be aware of challenges that the severity of obesity poses.
References
Pandya S, Murray JJ, Coller JA, Rusin LC (1999) Laparoscopic colectomy: indications for conversion to laparotomy. Arch Surg 134:471–475. doi:10.1001/archsurg.134.5.471
Hardiman K, Chang ET, Diggs BS, Lu KC (2013) Laparoscopic colectomy reduces morbidity and mortality in obese patients. Surg Endosc Other Interv Tech 27:2907–2910. doi:10.1007/s00464-013-2853-3
Gendall KA, Raniga S, Kennedy R, Frizelle FA (2007) The impact of obesity on outcome after major colorectal surgery. Dis Colon rectum 50:2223–2237. doi:10.1007/s10350-007-9051-0
Pikarsky AJ, Saida Y, Yamaguchi T et al (2002) Is obesity a high-risk factor for laparoscopic colorectal surgery? Surg Endosc Other Interv Tech 16:855–858. doi:10.1007/s004640080069
Kamoun S, Alves A, Bretagnol F et al (2009) Outcomes of laparoscopic colorectal surgery in obese and nonobese patients: a case-matched study of 180 patients. Am J Surg 198:450–455. doi:10.1016/j.amjsurg.2008.09.022
Merkow RP, Bilimoria KY, McCarter MD, Bentrem DJ (2009) Effect of body mass index on short-term outcomes after colectomy for cancer. J Am Coll Surg 208:53–61. doi:10.1016/j.jamcollsurg.2008.08.032
Delaney CP, Pokala N, Senagore AJ et al (2005) Is laparoscopic colectomy applicable to patients with body mass index >30? A case-matched comparative study with open colectomy. Dis Colon rectum 48:975–981. doi:10.1007/s10350-004-0941-0
Nitori N, Hasegawa H, Ishii Y et al (2009) Impact of visceral obesity on short-term outcome after laparoscopic surgery for colorectal cancer: a single Japanese center study. Surg Laparosc Endosc Percutan Tech 19:324–327. doi:10.1097/SLE.0b013e3181ae5442
Senagore AJ, Delaney CP, Madboulay K et al (2003) Laparoscopic colectomy in obese and nonobese patients. J Gastrointest Surg 7:558–561. doi:10.1016/S1091-255X(02)00124-5
Casillas S, Delaney CP, Senagore AJ et al (2004) Does conversion of a laparoscopic colectomy adversely affect patient outcome? Dis Colon rectum 47:1680–1685. doi:10.1007/s10350-004-0692-4
Causey MW, Johnson EK, Miller S et al (2011) The impact of obesity on outcomes following major surgery for Crohn’s disease: an American College of Surgeons National Surgical Quality Improvement Program assessment. Dis Colon rectum 54:1488–1495. doi:10.1097/DCR.0b013e3182342ccb
Kunisaki C, Makino H, Takagawa R et al (2009) Predictive factors for surgical complications of laparoscopy-assisted distal gastrectomy for gastric cancer. Surg Endosc Other Interv Tech 23:2085–2093
Seki Y, Ohue M, Sekimoto M et al (2007) Evaluation of the technical difficulty performing laparoscopic resection of a rectosigmoid carcinoma: visceral fat reflects technical difficulty more accurately than body mass index. Surg Endosc Other Interv Tech 21:929–934. doi:10.1007/s00464-006-9084-9
Watanabe J, Tatsumi K, Ota M et al (2013) The impact of visceral obesity on surgical outcomes of laparoscopic surgery for colon cancer. Int J Color Dis 29:343–351. doi:10.1007/s00384-013-1803-9
Lascano CA, Kaidar-Person O, Szomstein S et al (2006) Challenges of laparoscopic colectomy in the obese patient: a review. Am J Surg 192:357–365. doi:10.1016/j.amjsurg.2006.04.011
Flegal KM, Carroll MD, Kit BK, Ogden CL (2012) Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA 307:491–497. doi:10.1001/jama.2012.39
Flegal KM, Flegal KM, Carroll MD et al (2010) Prevalence and trends in obesity among US adults, 1999-2008. JAMA 303:235–241. doi:10.1001/jama.2009.2014
Vignali A, De Nardi P, Ghirardelli L et al (2013) Short and long-term outcomes of laparoscopic colectomy in obese patients. World J Gastroenterol 19:7405–7411. doi:10.3748/wjg.v19.i42.7405
Schwandner O, Farke S, Schiedeck THK, Bruch HP (2004) Laparoscopic colorectal surgery in obese and nonobese patients: do differences in body mass indices lead to different outcomes? Surg Endosc Other Interv Tech 18:1452–1456. doi:10.1007/s00464-003-9259-6
Lu KC, Cone MM, Diggs BS et al (2011) Laparoscopic converted to open colectomy: predictors and outcomes from the Nationwide Inpatient Sample. Am J Surg 201:630–634. doi:10.1016/j.amjsurg.2011.01.009
Tekkis PP, Senagore AJ, Delaney CP, Fazio VW (2005) Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg 242:83–91. doi:10.1097/01.sla.0000167857.14690.68
Yamamoto M, Okuda J, Tanaka K et al (2013) Evaluating the learning curve associated with laparoscopic left hemicolectomy for colon cancer. Am Surg 79:366–371
Heneghan HM, Martin ST, Kiran RP et al (2013) Laparoscopic colorectal surgery for obese patients: decreased conversions with the hand-assisted technique. J Gastrointest Surg 17:548–554. doi:10.1007/s11605-012-2089-x
Wick EC, Hirose K, Shore AD et al (2011) Surgical site infections and cost in obese patients undergoing colorectal surgery. Arch Surg (Chicago, Ill 1960) 146:1068–1072. doi:10.1001/archsurg.2011.117
Khoury W, Kiran RP, Jessie T et al (2010) Is the laparoscopic approach to colectomy safe for the morbidly obese? Surg Endosc Other Interv Tech 24:1336–1340. doi:10.1007/s00464-009-0770-2
Akiyoshi T, Ueno M, Fukunaga Y et al (2011) Effect of body mass index on short-term outcomes of patients undergoing laparoscopic resection for colorectal cancer: a single institution experience in Japan. Surg Laparosc Endosc Percutan Tech 21:409–414. doi:10.1097/SLE.0b013e31822e5fdc
Author information
Authors and Affiliations
Contributions
All above authors meet the following conditions for authorship: (a) substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data; (b) drafting the article or revising it critically for important intellectual content; (c) final approval of the version to be published.
Corresponding author
Ethics declarations
Financial disclosure
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
Ms. Madhuri Nishtala, Dr. Benjamin P. Crawshaw, Dr. Morris E. Franklin, and Justin T. Brady have no conflicts of interest or financial ties to disclose. Scott R. Steele reports receiving personal fees from Ethicon and Medtronic outside the submitted work. Conor P. Delaney reports receiving personal fees from Ethicon and Merck Pharmaceuticals outside the submitted work. Bradley J. Champagne reports receiving personal fees from Medtronic, outside the submitted work.
Rights and permissions
About this article
Cite this article
Champagne, B.J., Nishtala, M., Brady, J.T. et al. Laparoscopic colectomy in the obese, morbidly obese, and super morbidly obese: when does weight matter?. Int J Colorectal Dis 32, 1447–1451 (2017). https://doi.org/10.1007/s00384-017-2865-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-017-2865-x