Abstract
Purpose
Perianal fistulas, and specifically high perianal fistulas, remain a surgical treatment challenge. Many techniques have, and still are, being developed to improve outcome after surgery. A systematic review and meta-analysis was performed for surgical treatments for high cryptoglandular perianal fistulas.
Methods
Medline (Pubmed, Ovid), Embase and The Cochrane Library databases were searched for relevant randomized controlled trials on surgical treatments for high cryptoglandular perianal fistulas. Two independent reviewers selected articles for inclusion based on title, abstract and outcomes described. The main outcome measurement was the recurrence/healing rate. Secondary outcomes were continence status, quality of life and complications.
Results
The number of randomized trials available was low. Fourteen studies could be included in the review. A meta-analysis could only be performed for the mucosa advancement flap versus the fistula plug, and did not show a result in favour of either technique in recurrence or complication rate. The mucosa advancement flap was the most investigated technique, but did not show an advantage over any other technique. Other techniques identified in randomized studies were seton treatment, medicated seton treatment, fibrin glue, autologous stem cells, island flap anoplasty, rectal wall advancement flap, ligation of intersphincteric fistula tract, sphincter reconstruction, sphincter-preserving seton and techniques combined with antibiotics. None of these techniques seem superior to each other.
Conclusions
The best surgical treatment for high cryptoglandular perianal fistulas could not be identified. More randomized controlled trials are needed to find the best treatment. The mucosa advancement flap is the most investigated technique available.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Perianal fistulas are a common disorder, estimated to occur in 12.3 per 100,000 men and 8.6 per 100,000 women [1]. In general, the types of perianal fistulas that are known are cryptoglandular fistulas (about 90–95 % of perianal fistulas), fistulas related to Crohn’s disease (about 1.5 %) and traumatic fistulas (about 3.5 %) [1]. A classification of fistulas was first published by Parks and colleagues, describing the course of the fistula tract (Fig. 1) [2]. Nowadays, it is also accepted to classify perianal fistulas in low and high fistulas (Fig. 1). Low fistulas involve only the distal third part of the anal sphincter complex. High fistulas involve the middle and/or upper third part of the sphincter complex.
Treatment for low perianal fistulas usually consists of a fistulotomy (Fig. 2), resulting in closure rates ranging between 80 and 100 % [3–5]. Best treatment for a high fistula has not been identified yet. In the last two decades, and even in the last 5 years, many new techniques have been developed for the treatment of these fistulas. The mucosal advancement flap (MAF) is one of the best-known and oldest techniques (Fig. 3) and results in long-term closure rates between 0 and 75 % [4, 6–8]. In the early 1990s fibrin glue (FG) was introduced as a new technique (Fig. 4) to improve long-term closure rates [9, 10]. Anal fistula plugs (FP) were introduced in 2006 and thoroughly investigated in the years after (Fig. 5) [11]. In 2007, Rojanasakul introduced the Ligation of Intersphincteric Fistula Tract (LIFT) [12], which was thought to be a breakthrough in the treatment of perianal fistulas (Fig. 6). However, recently the first study comparing MAF versus LIFT showed comparable results between the two techniques with merely 60 % closure [13]. In 2009, the first study using stem cells (SC) was published (Fig. 4) [14], and many studies are still investigating this recent technique. In 2011, an endoscopic technique and a technique using a laser probe were introduced (Figs. 7 and 8) [15, 16]. In 2014, Göttgens et al. published an article describing a combination of the MAF with platelet-rich plasma (PRP) resulting in long-term closure rates of 83 % (Fig. 4) [17]. Currently, a randomized trial is investigating this technique further.
Mucosa advancement flap. a Fistulectomy up to the sphincter muscle (1), debriding of the fistula tract (2), preparing the advancement flap with excision of the opening in the flap (3), closure of the internal fistula opening (4). b Re-fixation of the mucosa advancement flap over the internal opening
Besides the type of fistula, the aetiology of the fistula is also important because different treatments may be needed. Fistulas related to Crohn’s disease are associated with higher recurrence rate and are often treated differently compared to cryptoglandular fistulas. The most occurring fistulas are related to cryptoglandular disease.
As shown, several new techniques have been introduced recently for the closure of high perianal fistulas, but the best technique has not been identified yet. The goal of this study was to perform a systematic review and meta-analysis of all available surgical techniques identifying the superior technique for closure of high cryptoglandular perianal fistulas (HCPF).
Materials and methods
This study was performed according to methodology of the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) group [18]. Besides, the Cochrane Collaboration’s tool for assessing risk of bias was used. This review was registered on PROSPERO (CRD42013004570).
Study selection
Searches were performed in Medline (Pubmed and Ovid), Embase (Ovid) and the Cochrane library database for all relevant articles comparing surgical treatments of HCPF. No language or date limits were instituted. Relevant surgical techniques were: Fistulectomy, MAF, rectal wall advancement flaps (Fig. 9), seton treatment (ST) (Fig. 10), SC, FG, FP, LIFT, PRP, endoscopic techniques, laser probe techniques, radiofrequency techniques and combinations or variations of these techniques.
Two independent reviewers reviewed citations and abstracts and made a selection of articles. Differences in article selection were discussed and a final decision made afterwards. References in articles were searched for other relevant literature. The final search was performed on November 11, 2013.
Inclusion criteria
Only randomized controlled clinical trials (RCT) were eligible for inclusion. The trials had to compare two or more surgical techniques for the closure of HCPF.
Exclusion criteria
Studies only involving patients with other types of perianal fistulas (low fistulas, related to Crohn’s disease, traumatic) were excluded. Studies reporting on several types of fistulas were included, but data on these other types of fistulas were not used. Studies were excluded if no outcomes of interest were reported, or if insufficient data were published to extract the necessary data. Studies involving children were excluded.
Outcomes
The primary outcome was the recurrence rate. Secondary outcomes included continence level, quality of life and complications. Complications included: abscess formation, bleeding, urinary tract infections and re-operations.
Data extraction
Two reviewers independently extracted data from the selected articles on predefined forms. Data included name of the authors, year of publication, study design, characteristics of the patient population, characteristics of the included fistula type(s), in- and exclusion criteria, number of patients, and all data related to the defined outcomes.
Study quality
Two reviewers independently assessed the risk of bias in all selected studies. The Cochrane Collaboration’s tool for assessing risk of bias was used. Studies were classified as having low risk of bias, high risk of bias and unclear risk of bias. Any disagreement between reviewers was solved by consensus.
Statistical analysis
The standard mean difference (SMD) was calculated as the summary statistic for continuous variables and odds ratios (OR) were calculated for dichotomous outcomes. The meaning of results was described for the different analyses. For P values < 0.05, statistical significance was assumed only if the 95 % confidence intervals did not include the value 1 for OR or the value 0 for SMD. Between-study heterogeneity was assessed using the χ 2 and Ι 2 statistics. A fixed-effects meta-analysis was performed if study homogeneity was confirmed, and a random-effects meta-analysis if significant heterogeneity was found.
Review Manager (RevMan) 5.27 (The Nordic Cochrane Center, Copenhagen, Denmark) was used for the statistical analyses.
Results
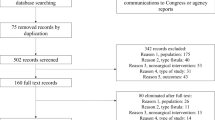
In total, 111 publications were found in the initial search. Finally, 14 publications fulfilled the inclusion criteria and were included in this review. Figure 11 shows the flow diagram of study selection. The two most occurring reasons for excluding a study were Non-RCT studies and studies not investigating HCPF.
Table 1 shows the included studies and techniques.
Fistula plug versus mucosa advancement flap
Three RCTs were identified comparing FP and MAF [19–21]. Risk of bias was defined as low for all three studies as is shown in Fig. 12. The same FPs were used in all studies and the technique of creating a MAF was comparable. Thus, a meta-analysis was performed for the primary outcome measure. The forest plot can be seen in Fig. 13. The random-effects model was used, which did not show an advantage for either technique concerning recurrence rate with an odds ratio of 1.7 (95 % CI 0.12–23.41), p = 0.69.
Regarding the secondary outcomes comparison using a meta-analysis was only possible for the complication rate. A fixed-effects model was used for this outcome, which did not show an advantage for either technique (Fig. 14) with an odds ratio of 0.32 (95 % CI 0.08–1.21), p = 0.09.
Continence levels were objectified pre- and postoperatively using the Vaizey scale in two studies [20, 21]; however, for one study, the results are not extractable [20]. Both studies do not report a significant difference in continence levels between the techniques. The third study does not report on continence status.
Only two studies report on quality of life [20, 21]. Both use a different questionnaire (respectively, the life quality scale system and the SF-36 questionnaire) and do not show a difference in quality of life between techniques.
Seton treatment versus fibrin glue
Only one RCT was identified comparing ST (n = 25) and FG (n = 39) [22]. Risk of bias in this study was regarded as low. Duration and type of ST was not clearly described. They used a cutting or a loose latex seton. They show a significant advantage of the ST over FG in recurrence rate with respectively, 12.5 and 62.0 % recurrence, p < 0.05.
Complication rate and quality of life are not measured in this study. Continence status was pre- and postoperatively objectified using the Wexner continence score. Pre-operatively, no significant difference was seen between both groups, but postoperatively, a significant rise in the incontinence score was seen in the ST group. The mean score was 5.1 in the ST group and 0.49 in the FG group, p < 0.05, postoperatively.
Advancement flap versus advancement flap + fibrin glue
Ellis et al. report on their RCT comparing an advancement flap (n = 30) with an advancement flap + FG (n = 28) [23]. This study was classified as low risk of bias (Fig. 12). Advancement flaps were either a MAF or an anodermal advancement flap depending on previous treatment failure or technical difficulty. This study only reports on recurrence rates and does not mention any secondary outcomes. Recurrence rates are not reported separately for primary and recurring fistulas.
A recurrence rate of 20.0 % was seen for the advancement flap group compared to 46.4 % for the advancement flap combined with FG, p < 0.05. A sub-group analysis showed no significant difference between the types of advancement flap used.
Mucosa advancement flap versus mucosa advancement flap + gentamicin
One study was found comparing the MAF (n = 41) and the MAF with a gentamicin collagen sponge (n = 42) placed under the advancement flap [24]. The risk of bias in this study was estimated to be low (Fig. 12). The recurrence rate for the patients receiving the gentamicin sponge compared to the MAF alone was 38.1 and 48.8 %, respectively, not significantly different.
No secondary outcomes are reported in this study.
Autologous stem cells versus autologous stem cells + fibrin glue versus fibrin glue + placebo
We identified one study investigating ASC for the treatment of HCPF [25]. It was a phase III RCT investigating safety of ASC treatment. This study had three arms: ASC injection into the fistula (n = 64) was compared to ASC injection combined with FG injection (n = 60) and also with FG injection combined with a placebo (n = 59). All fistula tracts were identified and curetted, and the internal fistula opening was closed before injections. The quality of this study was high and it was classified as having a low risk of bias (Fig. 12). No significant differences were seen in recurrence rates with respectively, 57.1, 52.4 and 37.3 % healing after 1 year, p = 0.13.
Secondary outcomes reported were continence levels and quality of life, respectively measured using the Wexner incontinence score and the SF-36. No significant differences in these outcomes were seen between groups and between pre- and postoperatively.
Island flap anoplasty versus seton treatment
The island flap anoplasty involves a cutaneous advancement flap into the rectum (Fig. 15). There was only RCT found describing this technique [26]. The authors compared it to ST. Risk of bias in this study was deemed high (Fig. 12). They included only two patients in both groups with HCPF. All other included patients had LCPF and were not treated with ST, but with a fistulotomy. Due to the poor quality and very low number of patients the recurrence rates of 0 % in both groups are not reliable. Data regarding the secondary outcomes quality of life and continence status were not extractable.
Kashaarasootra seton versus fistulectomy
A study performed by a collaboration of surgical centres in India was found comparing fistulectomy against a seton coated with Ayurvedic (called a Kshaarasootra seton) [27]. The fistulectomy was performed for the tract below the anal sphincter complex (Fig. 3). The upper part of the tract was curetted. Ayurvedic is a combination of several vegetal materials and is as far as we know only used in India. The seton was changed regularly in the outpatient clinic and eventually removed. It was a well-organized and well-performed study with a low risk of bias (Fig. 12). They included 40 HCPF in the Ayurvedic group and 33 in the fistulectomy group. The closure rates are poor with recurrence rates of 70.0 and 78.8 %, respectively, but not significantly different between the two procedures. Levels of incontinence were described to be low, but no standardized questionnaires were used.
Rectal wall advancement flap versus mucosa advancement flap
The rectal wall advancement flap (RWA) (n = 20) is compared to the MAF (n = 20) in only one study [28]. The RWA included mucosa, submucosa and the circular muscle layers, while the MAF did not include the muscle layers. Risk of bias in this study was low. The authors found a significant higher success rate in the RWA group with a recurrence rate of 10.0 versus 40.0 % in the MAF group, p < 0.05. The level of incontinence was higher in the RWA group, 10 % compared to 0 %, but this was not significantly different. The complication rate was higher in the MAF group. The complications were mostly disruption of the advancement flap and occurred in 30 % in the MAF group and in 5 % in the RWA group, p < 0.05. Quality of life is not reported.
Ligation of intersphincteric fistula tract versus mucosa advancement flap
The LIFT is a relatively new technique for treatment of HCPF. We found only one RCT involving the LIFT [29], which compared the technique to the MAF. All patients were treated with ST first for 6 months to reduce sepsis. Risk of bias was low (Fig. 12). However, the number of patients included in the trial was small with 25 patients in the LIFT group and 14 in the MAF group, and follow-up was much shorter for the LIFT group (16.4 months versus 30.0 months, respectively). No significant differences were seen for recurrence rates, with 8.0 and 4.0 % recurrence respectively. The Wexner incontinence score was used to evaluate continence status. No differences were seen for pre- and postoperative continence, nor were differences found between both groups. Complication rates were not significantly different for the techniques. Quality of life was not measured. The only differences the investigators found between both groups were a higher satisfaction rate, a lower postoperative pain score and shorter time to resuming normal activities after the LIFT.
Mucosa advancement flap versus fistulotomy + sphincter reconstruction
Perez et al. compare the MAF against a fistulotomy with sphincter reconstruction (FSR) (Fig. 16) [30]. They included 27 patients in the MAF group and 28 patients in the FSR group. Risk of bias was defined as low (Fig. 12). Recurrence rates were 7.4 and 7.1 %, respectively, not significantly different. Continence levels were measured using the Wexner incontinence score, which did not show significant differences in continence status pre- and postoperatively or between both interventions. The authors specifically reported incontinence in previously fully continent patients, which was 9.5 versus 17.4 %, p = 0.26. Complication rates were not different between both techniques. Quality of life was not measured.
Fibrin glue + antibiotics versus fibrin glue + surgical closure versus fibrin glue + antibiotics + surgical closure
We found one study comparing different treatments with FG [31]. Patients were randomized into three groups: FG + antibiotics (n = 23), FG + surgical closure (n = 23) and FG + antibiotics + surgical closure (n = 22). Surgical closure was defined as placing one suture over the internal fistula opening. The antibiotic used was cefoxitin. Risk of bias in this study was low (Fig. 12). Recurrence rates in all groups were high, with 78.3, 56.5 and 60.9 %, p = 0.38. Complication rates were not different and no changes in continence status were observed (although no standardized score was used). Quality of life was not reported.
Sphincter-preserving seton versus seton treatment
Zbar et al. report on their technique with a sphincter-preserving seton (SPS) (Fig. 10) [32]. They compare this technique with conventional ST. The SPS procedure is described as performing a MAF with closure of the internal opening and then dissecting an intersphincteric tract for the seton without injuring the internal anal sphincter. Eighteen patients were treated with the SPS and 16 with the ST. The recurrence rate was 11.1 and 6.3 % respectively, not significantly different. No differences were found in pre- and postoperative continence levels and neither were differences found between both groups. Quality of life was not reported and complication rates were not significantly different between both procedures.
Discussion
A relatively low number of RCTs investigating surgical procedures for closure of HCPF were identified making it difficult to compare all available techniques. Only two techniques could be compared in a meta-analysis: the FP and the MAF. This meta-analysis did not show a difference in recurrence rate nor in complication rate. Continence levels and quality of life were not different between both techniques, but not comparable using a meta-analysis because of different measurement tools. However, the three RCTs that were compared in this meta-analysis showed significant heterogeneity in inclusion criteria, methodology and postoperative management. One study included all HCPF [19], another only transsphincteric fistula [21], and the third both transsphincteric and intersphincteric fistulas [20]. A single study mentioned inclusion of patients from 12 years old up to only 60 years old [20]. Only one of the studies was a blinded study [21]. Regarding postoperative management one study used intravenous antibiotics for three days postoperatively instead of only prophylactic preoperative antibiotics, and the same study required sitting baths and mandatory laxatives for a significant period [20]. These differences make the result of this meta-analysis less convincing, especially taking into account that many non-randomized studies show far less favourable results for the FP [33].
For all other techniques, only one RCT could be found making it impossible to perform meta-analyses. Most available randomized studies on surgical treatment of HCPF investigate the MAF, making this technique the best investigated surgical procedure for this disease. The results of these studies do not show an advantage of the MAF over other techniques. The MAF is still the most used technique for treatment of HCPF, and most (colorectal) surgeons are well familiar with this procedure. The technique is widely adopted, and could probably still be considered the golden standard for HCPF treatment. Newer techniques like the LIFT are gaining followers and might show advantages over the MAF in the future. Up to now, there is no high-level evidence favouring any surgical technique over the others.
The main limitation of our systematic review is the limited number of RCTs that could be included. This makes it difficult to identify the best technique available to close HCPF. Newer techniques, for instance video-assisted anal fistula treatment or closure with a laser probe, have not yet been investigated widely and results should be awaited in the future [16, 15].
As far as we are aware of, there is only one other systematic review and meta-analysis comparing all available surgical interventions for PF [34]. This study does not focus specifically on HCPF or even HPF and was updated last in 2010. It seems that currently there is not much more high-quality data available compared to then, resulting in comparable findings.
However, other review articles were published in the last years, most focussing on one of the available techniques [7, 35–37, 33]. These reviews show reasonable results for healing and recurrence. The main difference with our study and the mentioned review from 2010 being that all other reviews include non-randomized and non-comparative studies. The level of evidence in these reviews is obviously less high compared to a systematic review only including randomized controlled trials. Whether our purist approach is best in this case remains questionable. We were not able to shed light on the best technique for HCPF. It would perhaps be more useful, but with less high-level evidence, to systematically show all available data on the surgical techniques and let these numbers guide us in the right direction. If no clear winner would arise from a comparison like this, it could show us which techniques would be best studied in a comparative randomized controlled trial based on available results.
We were not able to identify the best surgical technique for HCPF due to the many techniques available and the low number of RCTs. More RCTs are needed to show us the information we are seeking to define a best-treatment algorithm for HCPF. The MAF is the most investigated and most used technique. Whether or not the MAF is the best technique to use in the treatment of HCPF remains unclear until more comparative studies are available.
References
Sainio P (1984) Fistula-in-ano in a defined population. Incidence and epidemiological aspects. Ann Chir Gynaecol 73(4):219–224
Parks AG, Gordon PH, Hardcastle JD (1976) A classification of fistula-in-ano. Br J Surg 63(1):1–12
Cariati A (2013) Fistulotomy or seton in anal fistula: a decisional algorithm. Updates Surg 65(3):201–205. doi:10.1007/s13304-013-0216-1
van der Hagen SJ, Baeten CG, Soeters PB, van Gemert WG (2006) Long-term outcome following mucosal advancement flap for high perianal fistulas and fistulotomy for low perianal fistulas: recurrent perianal fistulas: failure of treatment or recurrent patient disease? Int J Colorectal Dis 21(8):784–790. doi:10.1007/s00384-005-0072-7
van Koperen PJ, Wind J, Bemelman WA, Bakx R, Reitsma JB, Slors JF (2008) Long-term functional outcome and risk factors for recurrence after surgical treatment for low and high perianal fistulas of cryptoglandular origin. Dis Colon Rectum 51(10):1475–1481. doi:10.1007/s10350-008-9354-9
Dubsky PC, Stift A, Friedl J, Teleky B, Herbst F (2008) Endorectal advancement flaps in the treatment of high anal fistula of cryptoglandular origin: full-thickness vs. mucosal-rectum flaps. Dis Colon Rectum 51(6):852–857. doi:10.1007/s10350-008-9242-3
Soltani A, Kaiser AM (2010) Endorectal advancement flap for cryptoglandular or Crohn’s fistula-in-ano. Dis Colon Rectum 53(4):486–495. doi:10.1007/DCR.0b013e3181ce8b01
Jarrar A, Church J (2011) Advancement flap repair: a good option for complex anorectal fistulas. Dis Colon Rectum 54(12):1537–1541. doi:10.1097/DCR.0b013e31822d7ddd
Hjortrup A, Moesgaard F, Kjaergard J (1991) Fibrin adhesive in the treatment of perineal fistulas. Dis Colon Rectum 34(9):752–754
Abel ME, Chiu YS, Russell TR, Volpe PA (1993) Autologous fibrin glue in the treatment of rectovaginal and complex fistulas. Dis Colon Rectum 36(5):447–449
Johnson EK, Gaw JU, Armstrong DN (2006) Efficacy of anal fistula plug vs. fibrin glue in closure of anorectal fistulas. Dis Colon Rectum 49(3):371–376. doi:10.1007/s10350-005-0288-1
Rojanasakul A, Pattanaarun J, Sahakitrungruang C, Tantiphlachiva K (2007) Total anal sphincter saving technique for fistula-in-ano; the ligation of intersphincteric fistula tract. J Med Assoc Thai 90(3):581–586
Liu WY, Aboulian A, Kaji AH, Kumar RR (2013) Long-term results of ligation of intersphincteric fistula tract (LIFT) for fistula-in-Ano. Dis Colon Rectum 56(3):343–347. doi:10.1097/DCR.0b013e318278164c
Garcia-Olmo D, Herreros D, Pascual I, Pascual JA, Del-Valle E, Zorrilla J, De-La-Quintana P, Garcia-Arranz M, Pascual M (2009) Expanded adipose-derived stem cells for the treatment of complex perianal fistula: a phase II clinical trial. Dis Colon Rectum 52(1):79–86. doi:10.1007/DCR.0b013e3181973487
Meinero P, Mori L (2011) Video-assisted anal fistula treatment (VAAFT): a novel sphincter-saving procedure for treating complex anal fistulas. Tech Coloproctol 15(4):417–422. doi:10.1007/s10151-011-0769-2
Wilhelm A (2011) A new technique for sphincter-preserving anal fistula repair using a novel radial emitting laser probe. Tech Coloproctol 15(4):445–449. doi:10.1007/s10151-011-0726-0
Gottgens KW, Vening W, van der Hagen SJ, van Gemert WG, Smeets RR, Stassen LP, Baeten CG, Breukink SO (2014) Long-term results of mucosal advancement flap combined with platelet-rich plasma for high cryptoglandular perianal fistulas. Dis Colon Rectum 57(2):223–227. doi:10.1097/DCR.0000000000000023
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62(10):e1–34. doi:10.1016/j.jclinepi.2009.06.006
Ortiz H, Marzo J, Ciga MA, Oteiza F, Armendariz P, de Miguel M (2009) Randomized clinical trial of anal fistula plug versus endorectal advancement flap for the treatment of high cryptoglandular fistula in ano. Br J Surg 96(6):608–612. doi:10.1002/bjs.6613
Ab-b-k-r MM, Wen H, Huang HG, Chu H, Lu M, Chang ZS, Ai EH, Fan K (2010) Randomized controlled trial of minimally invasive surgery using acellular dermal matrix for complex anorectal fistula. World J Gastroenterol 16(26):3279–3286
van Koperen PJ, Bemelman WA, Gerhards MF, Janssen LW, van Tets WF, van Dalsen AD, Slors JF (2011) The anal fistula plug treatment compared with the mucosal advancement flap for cryptoglandular high transsphincteric perianal fistula: a double-blinded multicenter randomized trial. Dis Colon Rectum 54(4):387–393. doi:10.1007/DCR.0b013e318206043e
Altomare DF, Greco VJ, Tricomi N, Arcana F, Mancini S, Rinaldi M, d'Urso Pulvirenti A, La Torre F (2011) Seton or glue for trans-sphincteric anal fistulae: a prospective randomized crossover clinical trial. Colorectal Dis 13(1):82–86. doi:10.1111/j.1463-1318.2009.02056.x
Ellis CN, Clark S (2006) Fibrin glue as an adjunct to flap repair of anal fistulas: a randomized, controlled study. Dis Colon Rectum 49(11):1736–1740. doi:10.1007/s10350-006-0718-8
Gustafsson UM, Graf W (2006) Randomized clinical trial of local gentamicin-collagen treatment in advancement flap repair for anal fistula. Br J Surg 93(10):1202–1207. doi:10.1002/bjs.5398
Herreros MD, Garcia-Arranz M, Guadalajara H, De-La-Quintana P, Garcia-Olmo D, Group FC (2012) Autologous expanded adipose-derived stem cells for the treatment of complex cryptoglandular perianal fistulas: a phase III randomized clinical trial (FATT 1: fistula advanced therapy trial 1) and long-term evaluation. Dis Colon Rectum 55(7):762–772. doi:10.1097/DCR.0b013e318255364a
Ho KS, Ho YH (2005) Controlled, randomized trial of island flap anoplasty for treatment of trans-sphincteric fistula-in-ano: early results. Tech Coloproctol 9(2):166–168. doi:10.1007/s10151-005-0220-7
Research ICoM (1991) Multicentric randomized controlled clinical trial of Kshaarasootra (Ayurvedic medicated thread) in the management of fistula-in-ano. Indian Council of Medical Research. Indian J Med Res 94:177–185
Khafagy W, Omar W, El Nakeeb A, Fouda E, Yousef M, Farid M (2010) Treatment of anal fistulas by partial rectal wall advancement flap or mucosal advancement flap: a prospective randomized study. Int J Surg 8(4):321–325. doi:10.1016/j.ijsu.2010.03.009
Mushaya C, Bartlett L, Schulze B, Ho YH (2012) Ligation of intersphincteric fistula tract compared with advancement flap for complex anorectal fistulas requiring initial seton drainage. Am J Surg 204(3):283–289. doi:10.1016/j.amjsurg.2011.10.025
Perez F, Arroyo A, Serrano P, Sanchez A, Candela F, Perez MT, Calpena R (2006) Randomized clinical and manometric study of advancement flap versus fistulotomy with sphincter reconstruction in the management of complex fistula-in-ano. Am J Surg 192(1):34–40. doi:10.1016/j.amjsurg.2006.01.028
Singer M, Cintron J, Nelson R, Orsay C, Bastawrous A, Pearl R, Sone J, Abcarian H (2005) Treatment of fistulas-in-ano with fibrin sealant in combination with intra-adhesive antibiotics and/or surgical closure of the internal fistula opening. Dis Colon Rectum 48(4):799–808. doi:10.1007/s10350-004-0898-z
Zbar AP, Ramesh J, Beer-Gabel M, Salazar R, Pescatori M (2003) Conventional cutting vs. internal anal sphincter-preserving seton for high trans-sphincteric fistula: a prospective randomized manometric and clinical trial. Tech Coloproctol 7(2):89–94. doi:10.1007/s10151-003-0016-6
O'Riordan JM, Datta I, Johnston C, Baxter NN (2012) A systematic review of the anal fistula plug for patients with Crohn’s and non-Crohn's related fistula-in-ano. Dis Colon Rectum 55(3):351–358. doi:10.1097/DCR.0b013e318239d1e4
Jacob TJ, Perakath B, Keighley MR (2010) Surgical intervention for anorectal fistula. Cochrane Database Syst Rev 12(5):CD006319. doi:10.1002/14651858.CD006319.pub2
Hong KD, Kang S, Kalaskar S, Wexner SD (2014) Ligation of intersphincteric fistula tract (LIFT) to treat anal fistula: systematic review and meta-analysis. Tech Coloproctol. doi:10.1007/s10151-014-1183-3
Cirocchi R, Trastulli S, Morelli U, Desiderio J, Boselli C, Parisi A, Noya G (2013) The treatment of anal fistulas with biologically derived products: is innovation better than conventional surgical treatment? An update. Tech Coloproctol 17(3):259–273. doi:10.1007/s10151-012-0948-9
Subhas G, Singh Bhullar J, Al-Omari A, Unawane A, Mittal VK, Pearlman R (2012) Setons in the treatment of anal fistula: review of variations in materials and techniques. Dig Surg 29(4):292–300. doi:10.1159/000342398
Acknowledgments
The authors thank Paul J.H. Göttgens for designing the figures showing the operative techniques.
Conflicts of interest and sources of funding
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Göttgens, K.W.A., Smeets, R.R., Stassen, L.P.S. et al. Systematic review and meta-analysis of surgical interventions for high cryptoglandular perianal fistula. Int J Colorectal Dis 30, 583–593 (2015). https://doi.org/10.1007/s00384-014-2091-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-014-2091-8