Abstract
Purposes
The present study was designed to evaluate the prognostic value of the perioperative neutrophil-to-lymphocyte ratio (NLR) for the long-term survival in patients with colorectal cancer.
Methods
This was a retrospective study of 524 patients with histologically proven stage II or III colorectal cancer who underwent curative colorectal resection. We classified patients into a low NLR group or high NLR group base on their NLR values at three time points (before surgery (Pre), on the first postoperative day (POD1), and on the third or fourth postoperative day (POD3)) and evaluated the survival according to the group.
Results
The cancer-specific survival was significantly longer in the groups with a low NLR on POD3. The disease-free survival was significantly longer in the group with a low NLR on Pre. We subsequently allocated a score of 1 to patients with a high NLR at each point and reclassified patients into those with a low perioperative NLR group (score of 0 or 1) and high perioperative NLR group (score of 2 or 3). Both the cancer-specific survival and disease-free survival rates were significantly different between the two perioperative NLR groups. Both univariate and multivariate analyses demonstrated that being in the high perioperative NLR group was an independent risk factor for both the cancer-specific survival and disease-free survival.
Conclusions
Not only the preoperative but also the postoperative NTR is thus considered to be a predictor of the long-time survival in patients with colorectal cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It has long been recognized that cancer progression is not only dependent on the local characteristics of the tumor but also on the systemic host response. In 1978, DerHagopian et al. reported “inflammatory oncotaxis,” which was a phenomenon wherein the activation and growth of dormant neoplastic cells might occur secondary to inflammation at a site distant from the primary tumor [1]. Since then, there has been increasing evidence that the inflammatory status play an important role in the progression of a variety of tumors [2–4].
Surgery is known to cause significant alterations in metabolic, immune, and endocrine functions. There have been several reports that major surgery alters multiple immune parameters and accelerates tumor growth [5, 6]. In contrast, endoscopic surgery has been reported to cause a reduced immune response compared to open surgery [7, 8]. Several reports have pointed out the possibility of favorable survival in patients with cancer treated by laparoscopic surgery, compared to patients treated by open abdominal surgery [9–11].
As prognostic markers in patients with colorectal cancer, several inflammation-based scores, such as the Modified Glasgow Prognostic Score, Prognostic Index, or the platelet to lymphocyte ratio, have been proposed [12, 13]. The preoperative neutrophil-to-lymphocyte ratio (NLR) has been receiving attention because of its performance and ease of calculation [14–16]. However, the association between the postoperative NLR and long-term survival in patients with colorectal cancer has not been fully investigated.
For these reasons, we focused on the postoperative NLR, which was considered as a simple index of the systemic inflammatory response in critically ill patients [17]. The aim of this study was to evaluate the prognostic value of the perioperative NLR for long-term survival in patients with colorectal cancer.
Patients and methods
This study was a retrospective study of 524 patients with histologically proven stage II or III colorectal cancer (TNM seventh classification [18]) who underwent a potentially curative resection via laparotomy between January 2001 and December 2006 at the National Defense Medical College Hospital (Tokorozawa, Saitama, Japan). Patients with an emergency operation, laparoscopic operation, multiple carcinoma, inflammatory bowel disease, preoperative clinical evidence of infection or other inflammatory conditions, and those undergoing resections with macro- or microscopically positive pathological margins (R1 and R2 resections) were excluded from this study. In addition, patients who had undergone re-operation within a week from the first operation, which was generally required due to postoperative complication, were also excluded. The characteristics of the patients in this study are presented in Table 1. The median age of the patients was 65 years (range 18–96 years). There were 292 men and 232 women, 381 colon cancers and 143 rectal cancers, and 250 stage II patients and 274 stage III patients.
Patients were retrospectively evaluated for clinicopathological data (age, sex, cancer site, cancer stage, postoperative infectious complications, and perioperative laboratory measurement) on the basis of their medical and nursing charts. The postoperative infectious complications in this study included incisional surgical site infections (SSIs), organ/space SSIs, enterocolitis, urinary tract infections, pneumonia, and other infections, which require some kind of clinical treatment. We calculated the NLRs before surgery (Pre), on the first postoperative day (POD1), and on the third or fourth postoperative day (POD3).
Adjuvant chemotherapy using a 5-fluorouracil (5-FU)-based regimen, such as the Roswell Park Memorial Institute (RPMI) regimen [19], Mayo regimen [20], or an oral uracil/tegafur (UFT)/leucovorin (LV) regimen [21], was recommended for patients with stage III disease or those with a high potential of recurrence based on the pathological findings. As a result, adjuvant chemotherapy was performed in 156 patients (55.9 %) with stage III cancer and 38 patients (15.1 %) with stage II cancer.
The patients were regularly observed at our hospital or the outpatient clinic. They underwent a physical examination and complete blood cell count, blood chemical analysis, and serum tumor marker evaluations every 3 months for the first 3 years after surgery and every 6 months for the following 2 years. Contrast-enhanced computed tomography was performed every 6 months, while colonoscopy was performed 1 and 3 years after surgery. After 5 years, an annual follow-up was conducted through telephone conversations with the patients or their family. The median follow-up was 59 months (range 5.2–111.6).
The primary endpoint of this study was the cancer-specific survival. The cancer-specific survival time was measured from the date of resection to the date of death due to recurrence of the primary cancer. The secondary endpoint was disease-free survival. Disease-free survival time was measured from the date of resection to the date of radiological or histological identification of recurrence of the primary cancer.
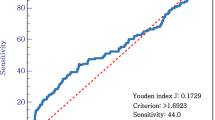
The statistical analysis was performed using the JMP software program (SAS Institute Inc., Cary, NC). The statistical analyses were performed using either the Pearson’s χ 2 test or the Wilcoxon rank sum test. The survival rates were calculated with the Kaplan-Meier method, and differences between the curves were tested using the log-rank test. The univariate and multivariate analyses were performed using the Cox proportional hazards regression model. A P value <0.05 was considered to be statistically significant.
Results
Within the observation period, 104 patients (19.8 %) developed recurrence and 74 patients (14.1 %) succumbed to recurrence of the primary tumor. Thirty patients (5.7 %) died due to other causes.
Table 2 shows the perioperative NLRs and the classification of these values. We classified the perioperative NLRs according to the median NLR. That is, the patients with higher than the median NLR were classified into the high group, and those with values lower than the median NLR were classified into the low group.
Figure 1 shows the Kaplan-Meier curves for the cancer-specific survival of patients with high and low perioperative NLR values. There was a statistically significant difference in the cancer-specific survival between the groups based on the NLR values on POD3, although there was no significant difference between the comparison of the NLR at the Pre and POD1 time points. With respect to the disease-free survival, there was a statistically significant difference between the comparisons of the NLR values on Pre, although there was no significant difference between the comparison of the NLR at the POD1 and POD3 time points (Fig. 2).
We also compared the survival time in subgroups with different stages of cancer. In the patients with stage II cancers, there was a statistically significant difference in the cancer-specific survival between the groups based on the NLR values on POD3 (Fig. 3). In patients with stage III cancers, there was a statistically significant difference in the disease-free survival between the groups based on the NLR values at the Pre and POD1 time points (Fig. 4).
In addition, we allocated a score of 1 to patients with a high NLR at each point (Pre, POD1, POD3). That is, patients with high NLR values at all points were allocated a score of 3, while patients with low NLR values at all points were allocated a score of 0. As a result, 96 patients were assigned a score of 0, 132 patients were assigned a score of 1, 124 patients were assigned a score of 2, and 110 patients were assigned a score of 3. We also reclassified patients based on this scoring system: a low perioperative NLR group (score of 0 or 1) or high perioperative NLR group (score of 2 or 3).
Table 3 shows the associations between the clinicopathological factors and perioperative NLR scores. Although the cancer site, differentiation, and postoperative infectious complications were found to be associated with the perioperative NLR score, no other clinicopathological factors were related to the score.
Figure 5 shows the Kaplan-Meier survival curves for the patients with high and low perioperative NLR scores. There was a statistically significant difference in both the cancer-specific survival and disease-free survival between the groups based on a comparison of the perioperative NLR score. The 5-year cancer-specific survival rates in patients with a high perioperative NLR score and in those with a low perioperative NLR score were 81.0 and 89.4 %, respectively. The 5-year disease-free survival rates in patients with a high perioperative NLR score and in those with a low perioperative NLR score were 75.1 and 84.5 %, respectively.
The Kaplan-Meier curves for the cancer-specific and disease-free survival after surgery with curative intent for stage II or III colorectal cancer based on the perioperative NLR score; we allocated a score of 1 to patients with a high NLR at each point and reclassified patients into a low perioperative NLR group (score of 0 or 1) and a high perioperative NLR group (score of 2 or 3)
The univariate and multivariate analyses of the clinicopathological factors and perioperative NLR score were performed. In the univariate analysis, the cancer site (colon vs rectum), T stage (T1–3 vs T4), lymph node metastases (negative vs positive), and perioperative NLR score (0, 1 vs 2, 3) were each found to be associated with the cancer-specific survival. The multivariate analysis also demonstrated that the cancer site, T stage, lymph node metastases, and perioperative NLR score were significantly associated with the cancer-specific survival (Table 4). Similarly, the multivariate analysis demonstrated that a high perioperative NLR score was an independent risk factor for the disease-free survival (Table 5).
Discussion
Conventional prognostic factors for colorectal cancer, represented by the TNM classification, were mainly based on the tumor characteristics. We herein investigated the usefulness of a host factor to support the conventional prognostic factors for risk stratification in colorectal cancer treatment. Specifically, we focused on the impact of the postoperative NLR and revealed that there were significant differences between the long-term survival after curative resection of colorectal cancer based on the postoperative NLR.
The NLR is known as an inflammation-based prognostic score and is presumed to be a combined indicator of inflammation and the immune status in patients with colorectal cancer [15, 22, 23]. Recently, numerous reports have supported the utility of the NLR as a prognostic factor in patients with colorectal cancer. However, to our knowledge, this study is the first to indicate the association between the postoperative NLR and long-term survival in patients with colorectal cancer.
Although the reason for the association between an elevated NLR and a poor prognosis remains to be elucidated, there have been several reports that have discussed potential mechanisms. First, patients with an elevated NLR are presumed to have a poorer lymphocyte-mediated immune response to malignancy and therefore an increased potential for tumor recurrence [24]. Several studies have reported that patients with weaker lymphocytic infiltration at tumor margins had a worse prognosis [25, 26]. Second, patients with an elevated NLR are presumed to have an increased number of circulating neutrophils secreting vascular endothelial growth factor (VEGF), which is a pro-angiogenic factor thought to be integral to tumor development [27]. Park et al. reported that strong VEGF-C expression on surgical specimens of intrahepatic cholangiocarcinoma was an independent and important prognostic factor [28]. On the other hand, Motomura et al. have recently reported that an elevated NLR promoted hepatocellular carcinoma recurrence after living donor liver transplantation via the promotion of inflammatory microenvironment, which was provided by interleukin-17-producing cells and tumor-associated macrophages, not via lymphocytic infiltration or VGEF [24].
In addition to the utility of the preoperative NLR as prognostic factor, there have been several reports that postoperative infectious complications in patients undergoing gastrointestinal surgery lead to poor cancer-specific survival rates [29–31]. Although the precise mechanism is still unclear, we consider that an elevated postoperative NLR, caused by infection, may influence the long-term survival. For this reason, we hypothesized that a persistently elevated NLR might affect cancer progression. To verify this hypothesis, we allocated a score of 1 to patients with a high NLR at each point (preoperatively, on POD1 and on POD3) and classified the patients according to the perioperative NLR. As a result, the univariate and multivariate analyses demonstrated that a high perioperative NLR score, which means a persistently elevated NLR during the perioperative period, is an independent risk factor for both the cancer-specific survival and disease-free survival after curative resection of colorectal cancer.
There were several possible limitations associated with our study, including its retrospective nature. In addition, there was no completely fixed protocol for perioperative care. For example, POD3 in this study includes data collected on both the third and fourth postoperative days. The perioperative NLR values of patients in this study could not all be calculated, because routine laboratory measurements were sometimes missed.
In conclusion, our study provides evidence of an association of not only the preoperative but also the postoperative NLR with the long-term survival of patients with colorectal cancer. This needs to be confirmed in prospective and appropriately designed studies. The perioperative NLR score, which has no connection with the T stage or N stage, was an independent prognostic factor in patients with colorectal cancer. Further investigations are necessary to evaluate the mechanism underlying the association between the perioperative biological status and long-term survival in patients with cancer.
References
DerHagopian RP, Sugarbaker EV, Ketcham A (1978) Inflammatory oncotaxis. JAMA 240:374–375
Balkwill F, Mantovani A (2001) Inflammation and cancer: back to Virchow? Lancet 357:539–545
Coussens LM, Werb Z (2002) Inflammation and cancer. Nature 420:860–867
Grivennikov SI, Greten FR, Karin M (2010) Immunity, inflammation, and cancer. Cell 140:883–899
Little D, Regan M, Keane RM, Bouchier-Hayes D (1993) Perioperative immune modulation. Surgery 114:87–91
Tsuchiya Y, Sawada S, Yoshioka I, Ohashi Y, Matsuo M, Harimaya Y, Tsukada Y, Saiki I (2003) Increased surgical stress promotes tumor metastasis. Surgery 133:547–555
Hiki N, Shimizu N, Yamaguchi H, Imamura K, Kami K, Kubota K, Kaminishi M (2006) Manipulation of the small intestine as a cause of the increased inflammatory response after open compared with laparoscopic surgery. Br J Surg 93:195–204
Luk JM, Tung PH, Wong KF, Chan KL, Law S, Wong J (2009) Laparoscopic surgery induced interleukin-6 levels in serum and gut mucosa: implications of peritoneum integrity and gas factors. Surg Endosc 23:370–376
Shiromizu A, Suematsu T, Yamaguchi K, Shiraishi N, Adachi Y, Kitano S (2000) Effect of laparotomy and laparoscopy on the establishment of lung metastasis in a murine model. Surgery 128:799–805
Pera M, Nelson H, Rajkumar SV, Young-Fadok TM, Burgat LJ (2003) Influence of postoperative acute-phase response on angiogenesis and tumor growth: open vs. laparoscopic-assisted surgery in mice. J Gastrointest Surg 7:783–790
Evans C, Galustian C, Kumar D, Hagger R, Melville DM, Bodman-Smith M, Jourdan I, Gudgeon AM, Dalgleish AG (2009) Impact of surgery on immunologic function: comparison between minimally invasive techniques and conventional laparotomy for surgical resection of colorectal tumors. Am J Surg 197:238–245
Proctor MJ, Morrison DS, Talwar D, Balmer SM, Fletcher CD, O’Reilly DS, Foulis AK, Horgan PG, Mcmillan DC (2011) A comparison of inflammation-based prognostic scores in patients with cancer. A Glasgow Inflammation Outcome Study. Eur J Cancer 47:2633–2641
Kwon HC, Kim SH, Oh SY, Lee S, Lee JH, Choi HJ, Park KJ, Roh MS, Kim SG, Kim HJ, Lee JH (2012) Clinical significance of preoperative neutrophil-lymphocyte versus platelet-lymphocyte ratio in patients with operable colorectal cancer. Biomarkers 17:216–222
Mallappa S, Sinha A, Gupta S, Chadwick SJ (2013) Preoperative neutrophil to lymphocyte ratio >5 is a prognostic factor for recurrent colorectal cancer. Color Dis 15:323–328
Malietzis G, Giacometti M, Askari A, Nachiappan S, Kennedy RH, Faiz OD, Aziz O, Jenkins JT (2013) A preoperative neutrophil to lymphocyte ratio of 3 predicts disease-free survival after curative elective colorectal cancer surgery. Ann Surg. Epub ahead of print
Chiang SF, Hung HY, Tang R, Changchien CR, Chen JS, You YT, Chiang JM, Lin JR (2012) Can neutrophil-to-lymphocyte ratio predict the survival of colorectal cancer patients who have received curative surgery electively? Int J Color Dis 27:1347–1357
Zahorec R (2001) Ratio of neutrophil to lymphocyte counts—rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl Lek Listy 102:5–14
Sobin LH, Compton CC (2010) TNM seventh edition: what’s new, what’s changed: communication from the International Union Against Cancer and the American Joint Committee on Cancer. Cancer 116:5336–5339
Petrelli N, Douglass HO Jr, Herrera L, Russell D, Stablein DM, Bruckner HW, Mayer RJ, Schinella R, Green MD, Muggia FM et al (1989) The modulation of fluorouracil with leucovorin in metastatic colorectal carcinoma: a prospective randomized phase III trial. Gastrointestinal Tumor Study Group. J Clin Oncol 7:1419–1426
Poon MA, O'Connell MJ, Wieand HS, Krook JE, Gerstner JB, Tschetter LK, Levitt R, Kardinal CG, Mailliard JA (1991) Biochemical modulation of fluorouracil with leucovorin: confirmatory evidence of improved therapeutic efficacy in advanced colorectal cancer. J Clin Oncol 9:1967–1972
Douillard JY, Hoff PM, Skillings JR, Eisenberg P, Davidson N, Harper P, Vincent MD, Lembersky BC, Thompson S, Maniero A, Benner SE (2002) Multicenter phase III study of uracil/tegafur and oral leucovorin versus fluorouracil and leucovorin in patients with previously untreated metastatic colorectal cancer. J Clin Oncol 20:3605–3616
Kishi Y, Kopetz S, Chun YS, Palavecino M, Abdalla EK, Vauthey JN (2009) Blood neutrophil-to-lymphocyte ratio predicts survival in patients with colorectal liver metastases treated with systemic chemotherapy. Ann Surg Oncol 16:614–622
Zhang Y, Peng Z, Chen M, Liu F, Huang J, Xu L, Zhang Y, Chen M (2012) Elevated neutrophil to lymphocyte ratio might predict poor prognosis for colorectal liver metastasis after percutaneous radiofrequency ablation. Int J Hyperth 28:132–140
Motomura T, Shirabe K, Mano Y, Muto J, Toshima T, Umemoto Y, Fukuhara T, Uchiyama H, Ikegami T, Yoshizumi T, Soejima Y, Maehara Y (2013) Neutrophil-lymphocyte ratio reflects hepatocellular carcinoma recurrence after liver transplantation via inflammatory microenvironment. J Hepatol 58:58–64
Okano K, Maeba T, Moroguchi A, Ishimura K, Karasawa Y, Izuishi K, Goda F, Usuki H, Wakabayashi H, Maeta H (2003) Lymphocytic infiltration surrounding liver metastases from colorectal cancer. J Surg Oncol 82:28–33
Jass JR (1986) Lymphocytic infiltration and survival in rectal cancer. J Clin Pathol 39:585–589
Kusumanto YH, Dam WA, Hospers GA, Meijer C, Mulder NH (2003) Platelets and granulocytes, in particular the neutrophils, form important compartments for circulating vascular endothelial growth factor. Angiogenesis 6:283–287
Park BK, Paik YH, Park JY, Park KH, Bang S, Park SW, Chung JB, Park YN, Song SY (2006) The clinicopathologic significance of the expression of vascular endothelial growth factor-C in intrahepatic cholangiocarcinoma. Am J Clin Oncol 29:138–142
Law WL, Choi HK, Lee YM, Ho JW, Seto CL (2007) Anastomotic leakage is associated with poor long-term outcome in patients after curative colorectal resection for malignancy. J Gastrointest Surg 11:8–15
Tsujimoto H, Ichikura T, Ono S, Sugasawa H, Hiraki S, Sakamoto N, Yaguchi Y, Yoshida K, Matsumoto Y, Hase K (2009) Impact of postoperative infection on long-term survival after potentially curative resection for gastric cancer. Ann Surg Oncol 16:311–318
Mirnezami A, Mirnezami R, Chandrakumaran K, Sasapu K, Sagar P, Finan P (2011) Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak: systematic review and meta-analysis. Ann Surg 253:890–899
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kubo, T., Ono, S., Ueno, H. et al. Impact of the perioperative neutrophil-to-lymphocyte ratio on the long-term survival following an elective resection of colorectal carcinoma. Int J Colorectal Dis 29, 1091–1099 (2014). https://doi.org/10.1007/s00384-014-1964-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-014-1964-1