Abstract
Purpose
The majority of patients with node-negative colorectal cancer have excellent 5-year survival prospects, but up to a third relapse. Strategies to identify patients at higher risk of adverse outcomes are desirable to enable optimal treatment and follow-up. The aim of this study was to examine postoperative mortality and longer-term survival by mode of presentation for patients with node-negative colorectal cancer undergoing surgery with curative intent.
Methods
Patients from 16 hospitals in the west of Scotland between 2001 and 2004 were identified from a prospectively maintained regional clinical audit database. Postoperative mortality and 5-year relative survival by mode of presentation were recorded.
Results
Of 1,877 patients with node-negative disease, 251 (13.4 %) presented as an emergency. Those presenting as an emergency were more likely to be older (P = 0.023), have colon rather than rectal cancer (P < 0.001), have pT4 stage disease (P < 0.001), have extramural vascular invasion (P = 0.001), and receive surgery under the care of a nonspecialist surgeon (P < 0.001) compared to those presenting electively. The postoperative mortality rate was 3.3 % after elective and 12.8 % after emergency presentation (P < 0.001). Five-year relative survival was 91.8 % after elective and 66.8 % after emergency presentation (P < 0.001). The adjusted relative excess risk ratio for 5-year relative survival after emergency relative to elective presentation was 2.59 (95 % CI 1.67–4.01; P < 0.001) and 1.90 (95 % CI 1.00–3.62; P = 0.049) after exclusion of postoperative deaths.
Conclusions
Emergency presentation of node-negative colorectal cancer treated with curative intent was independently associated with higher postoperative mortality and poorer 5-year relative survival compared to elective presentation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer is the third most common cancer in western Europe, with around 40,000 new cases diagnosed annually in the UK alone [1]. Outcome following diagnosis remains poor with around half of those undergoing curative procedures surviving to 5 years [1, 2]. The main determinant of colorectal cancer survival is stage at presentation [3]. However, in the case of early stage disease, other factors related to both the patient and the tumour itself are of increasing importance [4, 5].
Emergency presentation of colorectal cancer has long been associated with poorer short-term outcomes [6, 7]. Furthermore, it has been reported that longer-term outcomes in patients with colorectal cancer who present as an emergency are poorer than those who have their procedure in an elective setting [7–9]. However, there has been limited adjustment for additional putative tumour, treatment and surgeon-specific determinants of outcome.
In addition, the proportion of patients presenting with early stage colorectal cancer is predicted to increase. More than 60 % of colorectal cancers detected through faecal occult blood test (FOBt) screening programmes are node-negative [10, 11]. However, node-negative disease can create a management dilemma as up to the third will develop metastases within 5 years without adjuvant treatment [12]. Therefore, it is vital to identify negative prognostic factors in node-negative disease to determine which patients would benefit from both adjuvant therapy and from more aggressive follow-up regimes [13].
The aim of the present study was to examine the impact of emergency presentation on both short and longer-term outcomes in a mature cohort of patients with node-negative colorectal cancer managed with a curative intent.
Methods
Details of patients with node-negative (Dukes’ stage A/B; Stage I/II; pTanypN0 pM0) colorectal cancer undergoing surgery with curative intent in 16 hospital sites from 1 January 2001 to 31 December 2004 were extracted from the prospectively maintained clinical audit database of the West of Scotland Colorectal Cancer Managed Clinical Network. Individual patient records were then linked to the Scottish Cancer Registry (SMR06). Details included age, sex, deprivation category, mode of presentation, site of tumour, T-stage, degree of tumour differentiation, presence of extramural vascular invasion, lymph node yield and specialty of surgeon (colorectal specialist or nonspecialist general surgeon).
Tumours were classified according to their anatomical site as per the International Classification of Disease version 10 (ICD-10). Lesions from the caecum to the sigmoid colon were classified as colon cancers (C18). Carcinomas of the rectosigmoid junction and rectum were classified as rectal cancers (C19-C20). Tumours of the appendix (C18.1) and anus (C21) were excluded.
The extent of tumour stage was assessed by TNM staging based on histological examination of the resected specimen. Patients were deemed to have had a curative resection if the operating surgeon considered that there was no macroscopic residual tumour and were verified histologically as a complete margin negative resection (R0). Mode of presentation was defined as emergency if presentation was with significant rectal bleeding, intestinal obstruction, perforation or other presentations resulting in an unplanned emergency hospital admission. All other routes of presentation were considered elective. Individual consultant surgeons were identified as colorectal specialists or nonspecialists by panel members of the corresponding colorectal cancer multidisciplinary team (MDT) of the units under study using a similar method, as described previously [5].
Socioeconomic circumstances were measured using the area-based Scottish Index of Multiple Deprivation (SIMD) 2006 score based on postcode of residence at diagnosis [14]. SIMD scores are presented in five groups with 1 representing the least and 5 representing the most deprived areas.
Patient records were linked to the General Registry Office for Scotland (GROS) death records. Minimum follow-up of survivors was 5 years. Postoperative mortality was defined as any death occurring within 30 days of initial surgery. Relative survival, expressed as the ratio of the overall survival of study participants and the survival that would be expected when only to the background mortality adjusting from age, sex and deprivation category, was estimated up to 5 years. Annual age, sex and SIMD-specific Scottish life-tables produced by the London School of Hygiene and Tropical Medicine were used to estimate background population mortality in the relative survival analysis.
The West of Scotland Cancer Surveillance Unit obtained permission to obtain cancer registry data both from Caldicott Guardians of all health boards in the west of Scotland and from the Information Services Division of the NHS in Scotland privacy advisory committee. Permission to obtain clinical audit data was granted by the West of Scotland Colorectal Cancer Managed Clinical Network advisory board. As this study was a retrospective review of clinical practice, no formal ethical approval was required.
Statistical methods
Comparisons of the association between baseline clinicopathological characteristics, treatment variables and mode of presentation were made using the χ 2 test and Student’s t-test where appropriate. Survival time was calculated from date of surgery to date of death or censor with a minimum of 5 years follow-up (date of censor 31 December 2010). Relative survival estimates were calculated using the Ederer II method [15]. Patients were excluded from the relative survival analysis if no follow-up time was calculable (i.e. death on day of surgery). The Hakulinen-Tenkanen approach to model excess mortality was used for the multivariate relative survival analysis [16]. Relative excess risk (RER) ratios are presented with 95 % confidence intervals (95 % CI) and P < 0.050 was considered statistically significant. Analysis was performed using STATA software package version 11(IC) (Statacorp, TX, 2009).
Results
A total of 1,877 patients (53.4 % male) who underwent surgery for node-negative colorectal cancer with curative intent from 1 January 2001 to 31 December 2004 were included. A total of 696 (37.1 %) were aged 75 years or over, and 522 (27.8 %) were from the most deprived areas. The mean age at surgery was 70.3 years (SD 11.0; range 23.2 to 97.8 years). A total of 1,404 (74.8 %) received surgery under the care of a specialist colorectal surgeon. Some 701 (37.4 %) of patients had rectal cancer, 1,610 (85.8 %) had well or moderately differentiated tumours, 193 (10.3 %) had evidence of extramural vascular invasion and 900 (48.0 %) had pT3 stage tumours. The overall postoperative mortality rate was 4.5 %. The overall 5-year relative survival rate was 88.5 % (95 % CI 85.7–91.1).
Mode of presentation
Univariate associations between baseline clinicopathological characteristics and mode of presentation are shown in Table 1. Of these, 1,626 (86.6 %) presented electively and 251 (13.4 %) as an emergency. Of the emergency group, 144 (57.4 %) presented with obstruction, 62 (24.7 %) with rectal bleeding, 39 (15.5 %) with perforation and 6 (2.4 %) via other emergency routes. Patients presenting as an emergency were more likely to be older (P = 0.023) and to receive surgery under the care of a nonspecialist general surgeon (P < 0.001). More patients with colonic tumours and fewer patients with rectal lesions presented as an emergency (P < 0.001). Patients presenting as an emergency were more likely to have pT4 stage tumours (P < 0.001) and have extramural vascular invasion (P < 0.001). There was no significant association with gender, socioeconomic group, lymph node yield or degree of tumour differentiation and mode of presentation.
Postoperative mortality
Univariate and multivariate analyses of factors associated with postoperative mortality are shown in Table 2. Emergency presentation was independently associated with poorer short-term survival. The postoperative mortality rate was 3.3 % in patients who presented electively compared to 12.8 % in those who presented as an emergency (P < 0.001). Compared to those who presented electively, those presenting as an emergency had a more than a three-fold increased risk of dying within 30 days of surgery (adjusted odds ratio 3.35 (95 % CI 1.92–5.84); P < 0.001). Advancing age and deprivation were also independently associated with increased postoperative mortality.
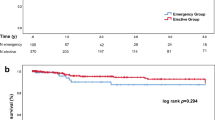
Five-year relative survival
Two patients (one elective and one emergency) died on the day of surgery and were excluded from the relative survival analysis. Univariate and multivariate analysis of factors associated with 5-year relative survival are shown in Table 3. Emergency presentation was independently associated with poorer longer-term survival. Relative survival at 5 years after surgery was 91.8 % (95 % CI 88.9–94.5) after elective presentation compared to 66.8 % (95 % CI 58.5–74.5) in those presenting as an emergency (P < 0.001) (Fig. 1). For those presenting as an emergency, the 5-year relative survival rate was 67.8 % (95 % CI 56.8–77.9) for those presenting with obstruction, 55.3 % (95 % CI 33.8–76.5) for perforation, 71.4 % (95 % CI 55.1–85.0) for rectal bleeding and 62.3 % (95 % CI 13.8–100.2) for those presenting via other emergency routes. Patients presenting as an emergency had a significantly increased risk of dying from colorectal cancer at 5 years compared to those presenting electively (adjusted RER 2.59 (95 % CI 1.67–4.01); P < 0.001). Advancing age, pT4 stage tumours, <12 lymph nodes examined and the presence of extramural vascular invasion were also independently associated with poorer 5-year relative survival.
Unadjusted and multiply adjusted relative excess risk (RER) ratios for 5-year relative survival following surgery for colorectal cancer by mode of presentation are shown in Table 4. The unadjusted RER ratio for emergency relative to elective presentation was 4.98 (95 % CI 3.30–7.50; P < 0.001). After adjustment for case-mix, tumour, treatment variables and exclusion of postoperative deaths, emergency presentation remained significantly associated with poorer relative survival at 5 years (adjusted RER 1.90 (95 % CI 1.00–3.62); P = 0.049). This suggests that emergency presentation has an on-going adverse effect on longer-term survival after the immediate postoperative period.
Discussion
This study shows that emergency presentation of node-negative colorectal cancer treated with curative intent was independently associated with a higher postoperative mortality and a poorer 5-year relative survival after adjustment for other treatment and clinicopathological variables associated with adverse outcome. Emergency presentation of colorectal cancer has previously been associated with poorer outcomes [6]. However, the findings in this present study highlight the negative impact of emergency presentation in those with node-negative colorectal cancer. Current strategies such as national bowel screening programmes have been effective in improving the early diagnosis of colorectal cancer by increasing the proportion of those diagnosed with node-negative cancers [10]. The incidence of node-negative colorectal cancer is therefore likely to increase over coming years. Therefore an additional advantage of bowel screening may be to reduce the proportion of those presenting to surgery via nonelective routes thus leading to further improved outcomes. Further evaluation of bowel screening initiatives and the mode of presentation of node-negative colorectal cancer are therefore required.
In this study, it was also noted that those who presented for surgery as an emergency were more likely to be older, have colon cancer, have more advanced T-stage, have tumours displaying extramural vascular invasion and receive surgery under the care of a nonspecialist surgeon. This suggests that patients presenting via a nonelective route have additional factors associated with poorer outcome and may have more aggressive tumour phenotypes. However, after adjustment for these treatment and clinicopathological characteristics associated with poorer outcomes and excluding postoperative deaths, emergency presentation remained independently associated poorer longer-term survival in this cohort. The adjusted relative excess risk ratio of emergency presentation is remarkably similar to the risk adjusted hazard ratio for cancer-specific survival noted in a previous publication from a similar geographical area a decade prior to the present study [7]. This implies that emergency presentation remains an important cause of poor outcomes in patients undergoing surgery for colorectal cancer. However, as to whether this will persist in the postscreening era is yet to be determined. Furthermore, the fact that this disparity remains despite adjustment for available clinicopathological characteristics suggests that there may be additional hitherto undetermined factors that play a role in dictating outcome in emergency presentation.
One explanation is that there are other physiological features of the patient presenting as an emergency that have not been adjusted for herein. For example, various preoperative risk scores, such as the Physiological and Operative Severity Score for the enUmeration of Mortality and morbidity (POSSUM), have been shown to be of prognostic significance [17]. Whilst this may account for the difference in postoperative mortality observed in the present study, POSSUM is not designed to predict longer-term survival [18]. It is now recognised that outcome following a diagnosis of colorectal cancer represents a complex interaction between tumour and host. One measure increasingly recognised as predictive of poorer longer-term cancer-specific survival is an elevated host inflammatory response [19, 20]. The systemic inflammatory response, as evidenced by the modified Glasgow Prognostic Score (mGPS) or the Neutrophil to Lymphocyte Ratio (NLR), is a validated method of achieving long-term prognostic stratification in patients undergoing surgery for colorectal cancer [21, 22]. There is some evidence that patients who present as an emergency have a more pronounced systemic inflammatory response. This has been shown to correlate with poorer cancer-specific survival [23, 24]. However, it remains to be determined whether the presence of a preoperative systemic inflammatory response may explain the impact of emergency presentation on cancer outcome.
In the present study, it was also of interest that specialist surgeons were less likely to perform emergency operations. Often the physiologically unwell, emergency patient presents with more technically challenging surgical pathology requiring a more complex procedure more suited to a specialist surgeon. Indeed, a previous study of the role of surgical specialisation on outcomes in emergency colorectal surgery identified increased mortality and morbidity in those treated by a nonspecialist [25]. In the current era of increasing surgeon sub-specialisation there have been recommendations that surgical management of the colorectal emergency patient should be assigned to a dedicated colorectal team [26]. In the present study, those treated by a nonspecialist surgeon did have higher rates of postoperative mortality and lower longer-term survival. However, these associations were no longer observed when other explanatory clinicopathological characteristics were adjusted for. This study therefore offers only limited evidence to support a strategy of increasing sub-specialisation for emergency colorectal surgery provision.
The main strengths of the present study are that it includes details on a large number of clinicopathological variables that have not previously been assessed in combination with regards to emergency presentation. In particular, the inclusion of vascular invasion is of particular relevance in node-negative disease [27, 28]. The quality of the data sources is also high due to their prospective nature and the limited missing data. A further strength of this study methodology is the use of relative survival to assess longer-term outcomes. Relative survival analyses are regarded as the gold standard for assessing longer-term outcome in patients with cancer with the advantage of being able to adjust for variations in background mortality rates and life expectancy [29, 30]. This allows for the inclusion and assessment of both cancer-specific and cancer-consequent deaths. However, direct comparison of outcomes with similar previous studies is not possible as these often present overall or cancer-specific survival rates only.
One particular limitation of this study is the lack of additional information on patient factors such as American Society of Anaesthesiologist (ASA) grade, measure of comorbidities, body habitus (BMI) or smoking status. The proportion of patients receiving chemotherapy following surgery was thought to be low as it was not routine clinical practice to administer adjuvant chemotherapy for node-negative disease out with the confines of a trial during the study period. However, no details of such therapy were available for inclusion in this work. A further limitation of this study was the lack of available data regarding the mode of surgery as per the NCEPOD Classification of Intervention (e.g. immediate (<minutes), urgent (<hours), expedited (<days), elective (planned)), extent of resection or on subsequent surgical procedures performed. The finding that there was no difference in average lymph node yield between those presenting as an emergency compared to electively suggest that the extent of surgical resection was similar between groups. However, further detailed study examining the influence of additional patient, tumour and treatment-related factors on outcome following surgery with curative intent for node-negative colorectal cancer is urgently required.
In conclusion, patients with node-negative colorectal cancer treated with a curative intent who presented as an emergency had higher postoperative mortality, lower 5-year relative survival and higher rates of adverse clinicopathological features when compared to patients presenting electively in this series. Furthermore, the disparity in longer-term outcome by mode of presentation remained after adjustment for case-mix, tumour and surgeon-specific variables and exclusion of postoperative deaths. Emergency presentation of node-negative colorectal cancer is therefore a significant independent risk factor for poor outcome. Clinicians should consider offering adjuvant chemotherapy to improve longer-term outcomes of such patients. Therefore, further study of the determinants of poorer outcome following emergency presentation of node-negative colorectal cancer is required and should include an examination of the role of the host response and effect of adjuvant therapies.
References
Cancer Research UK. Available at http://www.cancerresearchuk.org/cancer-info/cancerstats/types/bowel/. Accessed Apr 2013
Oliphant R, Nicholson GA, Horgan PG, Molloy RG, McMillan DC, Morrison DS (2013) Deprivation and colorectal cancer surgery: longer-term survival inequalities are due to differential postoperative mortality between socioeconomic groups. Ann Surg Oncol 20:2132–2139
Dukes CE, Bussey HJ (1958) The spread of rectal cancer and its effect on prognosis. Br J Cancer 12:309–320
Compton CC, Fielding LP, Burgart LJ, Conley B, Cooper HS, Hamilton SR et al (2000) Prognostic factors in colorectal cancer. College of American Pathologists Consensus Statement 1999. Arch Pathol Lab Med 124:979–994
Oliphant R, Nicholson GA, Horgan PG, Molloy RG, McMillan DC, Morrison DS (2013) Contribution of surgical specialisation to improved colorectal cancer survival. Br J Surg 100:1388–1395
Anderson JH, Hole D, McArdle CS (1992) Elective versus emergency surgery for patients with colorectal cancer. Br J Surg 79:706–709
McArdle CS, Hole DJ (2004) Emergency presentation of colorectal cancer is associated with poor 5-year survival. Br J Surg 91:605–609
McMillan DC, McArdle CS, Morrison DS (2010) A clinical risk score to predict 3-, 5- and 10-year survival in patients undergoing surgery for Dukes B colorectal cancer. Br J Cancer 103:970–974
Gunnarsson H, Holm T, Ekholm A, Olsson LI (2011) Emergency presentation of colon cancer is most frequent during summer. Colorectal Dis 13:663–668
Morris EJ, Whitehouse LE, Farrell T, Nickerson C, Thomas JD, Quirke P et al (2012) A retrospective observational study examining the characteristics and outcomes of tumours diagnosed within and without of the English NHS Bowel Cancer Screening Programme. Br J Cancer 107:757–764
Roxburgh C, McTaggart F, Balsitis M, Diament R (2013) The impact of the bowel screening programme on the diagnosis of colorectal cancer in Ayrshire and Arran. Colorectal Dis 15:34–41
Eisenberg B, Decosse JJ, Harford F, Michalek J (1982) Carcinoma of the colon and rectum: the natural history reviewed in 1704 patients. Cancer 49:1131–1134
Horgan PG, McMillan DC (2010) Surgeons and selection of adjuvant therapy for node-negative colonic cancer. Br J Surg 97:1459–1460
Scottish Index of Multiple Deprivation (2006) Available at http://www.scotland.gov.uk/topics/statistics/SIMD. Accessed Feb 2013
Hakulinen T (1982) Cancer survival corrected for heterogeneity in patient withdrawal. Biometrics 38:933–942
Hakulinen T, Tenkanen L (1987) Regression analysis of relative survival rates. Appl Stat 36:309–317
Jones HJ, de Cossart L (1999) Risk scoring in surgical patients. Br J Surg 86:149–157
Copeland GP, Jones D, Walters M (1991) POSSUM: a scoring system for surgical audit. Br J Surg 78:355–360
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144:646–674
Colotta F, Allavena P, Sica A, Garlanda C, Mantovani A (2009) Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis 30:1073–1081
McMillan DC (2013) The systemic inflammation-based Glasgow Prognostic Score: a decade of experience in patients with cancer. Cancer Treat Rev 39:534–540
Walsh SR, Cook EJ, Goulder F, Justin TA, Keeling NJ (2005) Neutrophil-lymphocyte ratio as a prognostic factor in colorectal cancer. J Surg Oncol 91:181–184
Catena F, Ansaloni L, Avanzolini A, Di Saverio S, D'Alessandro L, Maldini Casadei M et al (2009) Systemic cytokine response after emergency and elective surgery for colorectal carcinoma. Int J Colorectal Dis 24:803–808
Crozier JE, Leitch EF, McKee RF, Anderson JH, Horgan PG, McMillan DC (2009) Relationship between emergency presentation, systemic inflammatory response, and cancer-specific survival in patients undergoing potentially curative surgery for colon cancer. Am J Surg 197:544–549
Biondo S, Kreisler E, Millan M, Fraccalvieri D, Golda T, Frago R et al (2010) Impact of surgical specialization on emergency colorectal surgery outcomes. Arch Surg 145:79–86
National Institute of Clinical Excellence. Guidance on Cancer Services–improving outcomes in colorectal cancers (2004) Available at http://www.nice.org.uk/nicemedia/pdf/CSGCCfullguidance.pdf. Accessed April 2013
Petersen VC, Baxter KJ, Love SB, Shepherd NA (2002) Identification of objective pathological prognostic determinants and models of prognosis in Dukes’ B colon cancer. Gut 51:65–69
Roxburgh CS, McMillan DC, Anderson JH, McKee RF, Horgan PG, Foulis AK (2010) Elastica staining for venous invasion results in superior prediction of cancer-specific survival in colorectal cancer. Ann Surg 252:989–997
Dickman PW, Sloggett A, Hills M, Hakulinen T (2004) Regression models for relative survival. Stat Med 23:51–64
Berrino F, Esteve J, Coleman MP (1995) Basic issues in estimating and comparing the survival of cancer patients. IARC Sci Publ 132:1–14
Acknowledgments
The authors thank all the surgeons who participated, the West of Scotland Colorectal Cancer Managed Clinical Network advisory board who gave permission for MCN audit data to be used in this study, and the London School of Hygiene and Tropical Medicine for providing the Scotland-specific life-tables used in the relative survival analyses.
Conflicts of interest
All authors declare no conflict of interests.
Source of funding
No funding received.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Oliphant, R., Mansouri, D., Nicholson, G.A. et al. Emergency presentation of node-negative colorectal cancer treated with curative surgery is associated with poorer short and longer-term survival. Int J Colorectal Dis 29, 591–598 (2014). https://doi.org/10.1007/s00384-014-1847-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-014-1847-5