Abstract
Purpose
Neoadjuvant chemoradiation (NCRT) may be avoided in some patients with T3-staged rectal cancer undergoing radical resection. We aimed to evaluate the accuracy of endorectal ultrasound (ERUS) in the nodal staging of uT3 tumors and hence the decision for administration of NCRT.
Methods
Patients with uT3-staged rectal cancer who underwent proctectomy were retrospectively identified. The accuracy of ERUS for detecting nodal involvement was determined for patients who did not undergo NCRT. In order to evaluate the impact of use of NCRT, oncologic outcomes, functional outcomes, and quality of life (QOL) were compared for patients who received NCRT (group A) and those who did not (group B).
Results
For 384 patients who were included, ERUS overstaging rate for nodal involvement was 6.3 % while understaging rate was 23.2 %. For the 289 patients in group A and 95 in group B, Kaplan–Meier analysis showed similar 5-year local recurrence rates (3.5 %), overall survival (76.9 vs 75.6 %), and disease-free survival (87.9 vs 88.1 %). Node positivity on final pathology was however associated with worse 5-year local recurrence (9.3 vs 4.3 %). For patients undergoing restorative resection, NCRT was associated with worse functional outcomes but QOL was similar.
Conclusions
ERUS identification of nodal involvement used as a criterion for NCRT carries a greater risk for undertreatment than overtreatment. Undertreatment adversely affects oncologic outcomes. While there is functional impairment related to NCRT, its effect on QOL is non-significant. The decision for omitting neoadjuvant chemoradiation for uT3 rectal cancer should hence not be based on ERUS nodal staging alone.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The introduction of total mesorectal excision (TME) for rectal cancer has resulted in improved oncological outcomes [1]. Preoperative chemoradiation (neoadjuvant chemoradiotherapy, NCRT) in stage II and III tumors has further reduced local recurrence [2, 3] and therefore is considered standard of care for these tumor stages in many centers [4]. Recent data supports low local recurrence rates with surgery alone in favorable MRI-staged T3 tumors, including favorable stage III tumors [5]. While the role of MRI in the staging and pretreatment evaluation of rectal cancer continues to develop, whether endorectal ultrasound (ERUS) reliably identifies which patients with ultrasound staged T3 (uT3) rectal cancer may not benefit from NCRT has not been specifically assessed. In terms of ERUS, the presence of nodal involvement may be expected to guide this decision, with ERUS node positive (uN+) patients being considered an indication for NCRT, and a selective approach to NCRT being reserved for ERUS node negative (uN−) patients. While some studies have evaluated the accuracy of ERUS in nodal staging [6–8], the impact of any inaccuracy on outcomes in terms of oncologic or functional outcomes would be expected to be clinically relevant. The aim of this study was to hence answer this question based on an evaluation of the risks and benefits of NCRT for patients with uT3 rectal cancer in the context of the accuracy of ERUS in the staging of this group of patients.
Material and methods
All patients with uT3 middle and lower third rectal cancers (distance from anal verge <10 cm), who underwent proctectomy between 1993 and 2007, were identified from a prospectively maintained, IRB-approved, colorectal cancer database in the Department of Colorectal Surgery at the Cleveland Clinic. Patients with distant metastasis and those with tumors other than adenocarcinoma of the rectum were excluded.
Data collection
Information obtained included patient gender, age, American Society of Anesthesiologist (ASA) score, comorbidities (diabetes, hypertension, cardiovascular, and respiratory diseases), body mass index (BMI), ERUS staging, tumor size and distance from anal verge, radiochemotherapy regimen, type of procedure performed, level of anastomosis, postoperative course, pathological findings, oncological outcomes, and functional outcomes. Details of the postoperative course included information on length of stay, cardiovascular and pulmonary complications, urinary incontinence, bowel obstruction, wound infection and dehiscence, anastomotic leak and pelvic abscesses, readmission, reoperation, and 30-day mortality rates. Patients who received NCRT (group A) and did not receive NCRT (group B) were compared for the above characteristics and outcomes.
Accuracy of ERUS
The accuracy of ERUS in evaluating nodal involvement and especially the risk of understaging or overstaging disease was assessed in the subgroup of patients who underwent surgery without NCRT based on a correlation of the uT and uN stage with the final pathology (pT and pN stage) after resection.
Neoadjuvant chemoradiotherapy
NCRT has been used selectively, based primarily on the discretion of the individual surgeon, at our institution since 1993 (the beginning of our study). Patients who received NCRT at outside institutions underwent initial assessment at our institution prior to therapy elsewhere. The radiation dose, regimen, and the chemotherapeutic agents administered varied over the course of time. In general, chemotherapy was 5-fluorouracil (5-FU)-based, preoperative radiotherapy delivered through a three or four fields technique with a median dose of 50.4 (interquartile range 48.9–50.4) Gy.
Surgery
All operations were performed at the Cleveland Clinic in the Department of Colorectal Surgery with curative intent using TME. Surgery was performed after a minimum interval of 4 weeks from completion of NCRT, when administered. Surgical procedures were classified as restorative when bowel continuity was reconstructed. Restorative surgical procedures were classified as reservoir surgery when proctectomy or proctocolectomy was combined with ileal pouch-anal anastomosis, coloanal anastomosis with coloplasty, and colonic J-pouch anal anastomosis. Other procedures such as coloanal anastomosis, colorectal anastomosis, and pull-through were considered non-reservoir surgery.
Oncologic outcomes
Overall survival (OS), disease-free survival (DFS), and local recurrence (LR) rates were compared for uT3 patients who did (group A) and did not (group B) receive NCRT. Patient survival was verified using the Social Security Death Master File. Patients in the surgery-only group (group B), were evaluated for the presence or absence of lymph nodes involvement on final pathology. LR rates were also compared between pathologic T3 node negative (pT3N-) and node positive disease (pT3N+) within the group B patients.
Functional outcome measurements
Since any decision regarding the risk/benefit of NCRT needs to take its effect on anorectal function, functional outcomes, and quality of life (QOL) results were compared for patients who underwent restorative resection. Patients who underwent abdominoperineal resection (APR), pelvic exenteration, and Hartmann’s procedure were excluded with the inclusion of only patients with a functioning anastomosis without a permanent stoma. Long-term functional outcomes were measured by number of day and night time bowel movements; urgency; control of solid, liquid, and gas; and pad use. QOL was evaluated by measuring the physical (PCS) and mental component (MCS) scales from the SF-36 questionnaire. Follow-up questionnaires were obtained during office visits, or via phone calls and mail. The last functional and QOL questionnaire from each patient was selected for the comparison analysis. Functional outcomes and QOL were compared for patients in groups A and B to evaluate the effect of NCRT on these outcomes. Only patients that filled their questionnaires at least 180 days after surgery were included in the comparison analysis.
Statistical analysis
Data for patients who received NCRT (group A) or not (group B) were compared. Data is presented as mean and standard deviation (SD) or median and range. Chi-squared, Fisher’s exact probability tests, or Wilcoxon rank sum tests were used when appropriate to compare for baseline characteristics such as demographics, pathological diagnosis, perioperative factors, complications, and functional outcomes between two groups. Kaplan–Meier analysis was performed to analyze oncological outcomes. P value less than 0.05 was considered statistically significant for individual tests.
Results
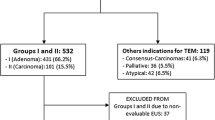
Three hundred and eighty-four patients with uT3, clinical M0, rectal cancer underwent proctectomy between 1993 and 2007. Of these patients, 289 (75.3 %) patients underwent NCRT (group A) and 95 (24.7 %) did not undergo NCRT (group B).
Accuracy of ERUS in the detection of nodal involvement
ERUS accuracy for detection of nodes was evaluated in the 95 patients who did not undergo NCRT (group B). For 21 patients with involved nodes identified on ERUS, and hence deemed to be uTN+, six patients (28.6 %) did not have any involved nodes on final pathology (pTN0). Thus in terms of nodal staging, ERUS overstaged only 6.3 % (6/95) of patients. In contrast, of the 67 patients defined as node negative by ERUS, 22 (32.8 %) patients were actually node positive on final pathology. Thus, based on nodal staging alone, 23.2 % (22/95) patients were hence understaged. A decision to omit NCRT, based on ERUS, in patients staged as uT3N0, would have led to undertreatment of these 22 patients (23.2 %; Table 1).
Comparison of patients who did (group A) and did not receive NCRT (group B)
Patients in group A were significantly younger and more often male. The two groups were similar in their ASA score, comorbidities, and BMI. Tumors in both groups were similar in terms of their distance from the anal verge and pretreatment size. Preoperative uN staging demonstrated node positive disease in 40.8 % of patients in group A and 23.1 % in group B (P = 0.001). Overall there were 207 patients with uT3N0 disease, 140 (67.6 %) of them received NCRT and 67 (32.4 %) did not. From the 132 patients with uT3N+ disease, 111 (84.1 %) received NCRT and 21 (15.9 %) did not receive NCRT. APR was more commonly performed in group B (46.3 vs 28.4 %, P = 0.002). No statistically significant difference in tumor differentiation was noticed between the two groups. However, examination of the resected specimen revealed smaller tumors in the group treated with NCRT (2.6 vs 4.2 cm, P < 0.001). Pathologic complete response rate to NCRT was 17.2 % (Table 2).
Table 3 provides the information on postoperative complications which were similar between the two groups. Length of stay, readmission, reoperation, and 30-day mortality rates were also similar.
Oncological outcomes
The follow-up time was comparable between group A (median 4.5 (range, 0–14) years) and group B (median 5.9 (range, 0.1–14.3) years). A Kaplan–Meier analysis showed similar 5-year local recurrence rates in groups A and B (3.5 % for each group, P = 0.8). The 5-year OS (76.9 vs 75.6 %, P = 0.85) and DFS rates (87.9 vs 88.1 %, P = 0.77) were also similar for groups A and B (Fig. 1).
Of the patients who did not undergo NCRT, there were 49 patients with pathologic stage T3 tumors. Of these, 25 (51 %) were node positive while 24 (49 %) were node negative on final pathology. The 5-year LR rates for patients with pT3N− tumors was 4.3 % and for patients with pT3N+ tumors 9.3 % (P = 0.48)
Functional outcomes
One hundred and forty-seven patients met the criteria for functional and QOL analysis. Out of these patients, 126 (85.7 %) patients underwent NCRT (group A) and 21 (14.3 %) patients did not undergo NCRT (group B). Functional follow-up times were similar for the two groups. Median functional follow-up time for group A was 2.1 years (range 0.5–5 years), and 2 years (range 0.8–5 years) for group B. Patients in group A were significantly younger than those in group B. The two groups were similar in gender, ASA score, and BMI. Procedure type (with or without reservoir), anastomosis height, and anastomosis type (stapled vs. hand-sewn), were also similar. Three patients (14.3 %) in group B received postoperative radiation. Functional outcomes for patients undergoing restorative resection were worse for patients who underwent NCRT in terms of pad use and control of solid stool. However, QOL assessed by SF-36 was similar between groups. Figure 2 demonstrates the change in anorectal function over the follow-up period (Table 4, Fig. 2).
Discussion
The oncological benefits of NCRT have been well established in locally advanced rectal cancer [9]. However, in contrast to patients with T4 tumors or nodal involvement, the threshold for the use of neoadjuvant chemoradiation in certain T3 tumors may be higher with a greater consideration of the relative risks and benefits for these patients. An evaluation of the oncologic benefit of NCRT in the context of the risk of potential complications and adverse functional outcomes is especially important in any attempt to individualize treatment strategies for this subgroup of patients. Since the decision whether to administer NCRT is made preoperatively, the accuracy of the imaging modality utilized limits this decision. There is emerging data from the United Kingdom supporting the use of rectal MRI as an efficient tool for preoperative staging and for decision making on omitting NCRT in certain clinical T3 tumors [5]. Nonetheless, MRI is still not as commonly used as ERUS in the clinical staging of rectal cancer and protocols utilized during MRI staging have not been standardized across institutions and especially vary in different countries. Whether ERUS is as effective as MRI in this sub-classification of T3 tumors is relatively unclear.
Previous studies found overstaging rates for T stage to be as high as 20 % and understaging rates for N stage as high as 39 % [6, 7]. In a series from Garcia-Aguilar et al. [8] that included 131 uT3 tumors, under- and overstaging rates for T stage were 2 and 28 % respectively while understaging rate for N stage (unrelated to T stage) was 11 % and overstaging rate was 24 %. Our study focused solely on tumors that were staged by ERUS as T3 (uT3). These tumors are classified accordingly as stage II or above and therefore, patients with such tumors would have been offered NCRT in most centers. This strategy would have led to an overtreatment (overstaging) rate of 33.7 % (pT1N0 and pT2N0) which is consistent with the results of the study by Garcia-Aguilar et al. [8] while the understaging rate is irrelevant to treatment strategy. The over- and understaging rates for N stage in our study were 6.3 and 23.2 %, respectively, all designated to NCRT according to current guidelines.
While MRI definition of a favorable T3 tumor is mainly based on the circumferential radial margin, in terms of ERUS, the presence of nodal involvement usually guides this decision. The presence of lymph nodes in T3 rectal cancer is likely to support the use of NCRT in most patients. Hence, in order to answer the question of whether NCRT can be selectively administered in patients with rectal cancer staged as T3 by ERUS, we chose to determine the accuracy of ERUS in nodal staging to evaluate the potential risk for undertreatment or overtreatment with NCRT. Oncologic outcomes for patients of comparable stage (pT3N+) who did not undergo NCRT were utilized to assess the effect of this undertreatment due to involved lymph nodes not having been detected on ERUS. In order to determine the potential consequences of administration of NCRT to patients who were overstaged by ERUS, perioperative outcomes were determined for patients who received NCRT in comparison to those who did not undergo NCRT. In order to evaluate any adverse effect of NCRT on anorectal function, functional outcomes and QOL were also compared after restorative rectal resection for patients who received NCRT in comparison to those who did not.
When comparing outcomes for the patients who did and did not receive NCRT, oncologic outcomes including LR, OS, and DFS were similar for both groups in our study. It could be argued that a careful preoperative assessment of these patients with the selective use of NCRT in those deemed to be at higher risk of recurrence and avoidance of NCRT in those considered to be at a lower risk or unlikely to withstand chemoradiation led to these results. In particular, the addition of NCRT may not improve local recurrence rates for patients with T3 rectal cancer without nodal involvement, undergoing TME by surgeons well-trained in the technique [10]. However, the finding that a greater proportion of patients who underwent surgery without NCRT did not have lymph node involvement on preoperative assessment may have been responsible for these results. Further, two thirds of patients with node negative disease and the majority of patients with node positive disease on ERUS received NCRT suggesting that surgery alone was selectively utilized in a few patients and may also have been responsible for these outcomes. Nonetheless, these findings may support a selective approach to the use of NCRT in patients with uT3-staged rectal cancer undergoing surgery.
Evaluation of the potential effect of lymph nodal involvement on LR for the patients who underwent surgery alone, suggested that the estimated 5-year risk of LR was higher for those with lymph nodes involved (9.3 %) when compared to those without nodes involved (4.3 %). When considering this in the context of the accuracy of ERUS for nodal staging, ERUS understaged disease in 23.2 %, suggesting that basing the decision whether to avoid NCRT based on nodal involvement on ERUS alone would have led to undertreatment and potentially adverse oncologic outcomes for these understaged patients. Although the LR rate of 3.5 % for the patients who did not receive NCRT is acceptably low and consistent with other large prospective cohorts, basing the decision as to whether to proceed with NCRT on ERUS detection of involved lymph nodes alone, could lead to an increased rate of LR due to this underdetection of patients with involved nodes.
In contrast, only 6.3 % patients with involved nodes identified on ERUS were node negative and hence overstaged from the node standpoint. Using node positivity on ERUS as a criterion for NCRT would have led to overuse of NCRT in only this 6.3 % of patients. A comparison of the perioperative outcomes, functional outcomes and QOL for patients who underwent or did not undergo NCRT was performed in order to evaluate the potential consequences of overtreatment. Conclusions regarding the impact of NCRT on anorectal function vary in the literature. While some authors [11–13] have reported impaired functional outcomes, others [14, 15] have reported contrasting results. In our study the two groups had similar postoperative complications, in particular, there was no increased risk of anastomotic complications such as leak and stricture, as one might expect from radiation to the anastomotic area. This is consistent with multiple previous randomized controlled trials [16, 17]. When evaluating functional outcomes, after a sufficiently long median follow-up period of 2 years, these were worse for the patients undergoing restorative resection after NCRT with greater pad use, and worse control of solid stool. However, QOL was similar regardless of whether the patients did or did not receive NCRT suggesting that although there was a statistical difference in some of the measured anorectal functions, these differences were not clinically significant enough to alter quality of life at the time of follow-up. Other measured anorectal functions, as bowel movements at night, and loss of control for gas and liquid stool were also worse in the group receiving NCRT but did not reach statistically significant differences.
Some limitations of the current study need to be considered. This is a retrospective study and the shortcomings inherently associated with this design are hence likely present. Specifically, the decision for neoadjuvant vs. no neoadjuvant therapy was based on the individual impression of the surgeon and reasons for the use or avoidance of NCRT were difficult to evaluate retrospectively. This implies a selection bias. However, the paucity of published large cohorts specifically addressing this subgroup of patients, with uT3-staged tumors not treated with NCRT, in the TME era, makes this information valuable.
The two groups differed in terms of age and there were differences in the NCRT regimen employed. Although the two groups were similar in relation to procedure type and use of a reservoir, the surgical technique might have varied among surgeons. Reasons for the use or avoidance of NCRT in some patients were difficult to evaluate retrospectively. Although potential factors that could influence functional outcome were carefully considered and controlled for when comparing results, we do not routinely obtain anorectal manometry preoperatively. Thus, we were unable to ascertain whether differences in functional results could be related to other factors such as preoperative sphincter function, and injury to the sphincters during surgery
Conclusion
Nodal involvement on final pathology is associated with worse LR for T3 stage mid and lower third rectal cancer patients who undergo rectal resection without NCRT. Since the false positive rate was only 6.3 % for patients with nodal disease identified on ERUS, this supports the administration of NCRT for these patients to reduce the LR. The similar perioperative outcomes and long-term QOL despite the worse functional outcomes with NCRT prior to surgery further supports this approach. For patients who are deemed to be node negative on ERUS, the risk of undertreatment in 23.2 % of patients supports a judicious consideration of NCRT based on anticipated oncologic outcomes, functional results, and QOL data on a case by case basis rather than ERUS findings alone. In good risk patients, where tumor factors such as bulk, location or histology, and patient anatomy suggest anticipated difficulty during surgery or worse oncologic outcomes, NCRT needs to be strongly considered despite potential worse functional outcomes. In contrast, in patients with more favorable tumor-related factors or anticipated problems with sphincter function or difficulty with the ability to tolerate NCRT, this can be selectively avoided after a due discussion of the risks and benefits of this approach with the patient. The ability of MRI to more accurately predict clearance of the circumferential resection margins and lymph nodal involvement further clarifies such a selection.
References
Law WL, Chu KW (2001) Impact of total mesorectal excision on the results of surgery of distal rectal cancer. Br J Surg 88:1607–1612
Kapiteijn E, Marijnen CA, Nagtegaal ID, Putter H, Steup WH, Wiggers T, Rutten HJ, Pahlman L, Glimelius B, van Krieken JH, Leer JW, van de Velde CJ, Dutch Colorectal Cancer Group (2001) Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med 345:638–646
Sebag-Montefiore D, Stephens RJ, Steele R, Monson J, Grieve R, Khanna S, Quirke P, Couture J, de Metz C, Myint AS, Bessell E, Griffiths G, Thompson LC, Parmar M (2009) Preoperative radiotherapy versus selective postoperative chemoradiotherapy in patients with rectal cancer (MRC CR07 and NCIC-CTG C016): a multicentre, randomised trial. Lancet 373(9666):811–820
Diaz-Gonzalez JA, Arbea L, Aristu J (2007) Rectal cancer treatment: improving the picture. World J Gastroenterol 13(44):5805–5812
Taylor FG, Quirke P, Heald RJ, Moran B, Blomqvist L, Swift I, Sebag-Montefiore DJ, Tekkis P, Brown G, MERCURY study group (2011) Preoperative high-resolution magnetic resonance imaging can identify good prognosis stage I, II, and III rectal cancer best managed by surgery alone: a prospective, multicenter, European Study. Ann Surg 253(4):711–719
Nesbakken A, Lovig T, Lunde OC, Nygaard K (2003) Staging of rectal carcinoma with transrectal ultrasonography. Scand J Surg 92:125–129
Jürgensen C, Teubner A, Habeck JO, Diener F, Scherübl H, Stölzel U (2011) Staging of rectal cancer by EUS: depth of infiltration in T3 cancers is important. Gastrointest Endosc 73(2):325–328
Garcia-Aguilar J, Pollack J, Lee SH, Hernandez de Anda E, Mellgren A, Wong WD, Finne CO, Rothenberger DA, Madoff RD (2002) Accuracy of endorectal ultrasonography in preoperative staging of rectal tumors. Dis Colon Rectum 45:10–15
Engstrom PF, Arnoletti JP, Benson AB 3rd, Chen YJ, Choti MA, Cooper HS, Covey A, Dilawari RA, Early DS, Enzinger PC, Fakih MG, Fleshman J Jr, Fuchs C, Grem JL, Kiel K, Knol JA, Leong LA, Lin E, Mulcahy MF, Rao S, Ryan DP, Saltz L, Shibata D, Skibber JM, Sofocleous C, Thomas J, Venook AP, Willett C, National Comprehensive Cancer Network (2009) NCCN clinical practice guidelines in oncology: rectal cancer. J Natl Compr Canc Netw 7:838–881
Peeters KC, Marijnen CA, Nagtegaal ID, Kranenbarg EK, Putter H, Wiggers T, Rutten H, Pahlman L, Glimelius B, Leer JW, van de Velde CJ, Dutch Colorectal Cancer Group (2007) The TME trial after a median follow-up of 6 years: increased local control but no survival benefit in irradiated patients with resectable rectal carcinoma. Ann Surg 246(5):693–701
Dahlberg M, Glimelius B, Graf W, Påhlman L (1998) Preoperative irradiation affects functional results after surgery for rectal cancer: results from a randomized study. Dis Colon Rectum 41:543–549
Ammann K, Kirchmayr W, Klaus A, Mühlmann G, Kafka R, Oberwalder M, De Vries A, Ofner D, Weiss H (2003) Impact of neoadjuvant chemoradiation on anal sphincter function in patients with carcinoma of the midrectum and low rectum. Arch Surg 138:257–261
Pollack J, Holm T, Cedermark B, Holmström B, Mellgren A (2006) Long-term effect of preoperative radiation therapy on anorectal function. Dis Colon Rectum 49(3):345–352
Rullier E, Goffre B, Bonnel C, Zerbib F, Caudry M, Saric J (2001) Preoperative radiochemotherapy and sphincter-saving resection for T3 carcinomas of the lower third of the rectum. Ann Surg 234:633–640
Urso E, Serpentini S, Pucciarelli S, De Salvo GL, Friso ML, Fabris G, Lonardi S, Ferraro B, Bruttocao A, Aschele C, Nitti D (2006) Complications, functional outcome and quality of life after intensive preoperative chemoradiotherapy for rectal cancer. Eur J Surg Oncol 32:1201–1208
Hyams DM, Mamounas EP, Petrelli N, Rockette H, Jones J, Wieand HS, Deutsch M, Wickerham L, Fisher B, Wolmark N (1997) A clinical trial to evaluate the worth of preoperative multimodality therapy in patients with operable carcinoma of the rectum. Dis Colon Rectum 40:131–139
Marijnen CA, Kapiteijn E, van de Velde CJ, Martijn H, Steup WH, Wiggers T, Kranenbarg EK, Leer JW, Cooperative Investigators of the Dutch Colorectal Cancer Group (2002) Acute side effects and complications after short-term preoperative radiotherapy combined with total mesorectal excision in primary rectal cancer: report of a multicenter randomized study. J Clin Oncol 20:817–825
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shapiro, R., Ali, U.A., Lavery, I.C. et al. Endorectal ultrasound does not reliably identify patients with uT3 rectal cancer who can avoid neoadjuvant chemoradiotherapy. Int J Colorectal Dis 28, 993–1000 (2013). https://doi.org/10.1007/s00384-013-1645-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-013-1645-5