Abstract
Purpose
We retrospectively analyzed preoperative levels of carbohydrate antigen (CA) 19-9 in colorectal cancer (CRC) patients to determine the prognostic value of CA19-9 in CRC patients with normal carcinoembryonic antigen (CEA) levels.
Methods
A total of 639 patients who underwent curative surgery at Taipei Veterans General Hospital between 2002 and 2006 were enrolled. We excluded 254 patients (39.7 %) with high preoperative CEA levels and analyzed 385 patients with normal CEA levels. The measured endpoint was the postoperative disease-free survival (DFS). The prognostic value of CA19-9 was determined using log-rank test and Cox regression analysis.
Results
High CA19-9 levels were significantly associated with advanced disease and were detected in 5.8 % of patients with stage I disease, 11.7 % of those with stage II disease, and 22.5 % of those with stage III disease (P < 0.001). The 5-year DFS in patients with normal CA19-9 levels was 82.0 %, which was significantly higher than that in patients with high CA19-9 levels (68 %; P < 0.001). In a multivariate analysis, the most important independent factor affecting the 5-year DFS was tumor–node–metastasis stage (95 % CI, 1.26–2.36; HR = 1.72). After stratification by other factors, high CA19-9 level remained an independent prognostic factor for patients with normal CEA levels. Patients with high CA19-9 levels also showed a higher incidence of lung metastasis (23.1 %) than those with normal CA19-9 levels (7.2 %).
Conclusions
CA19-9 may be a prognostic factor for CRC patients with normal CEA levels. An aggressive follow-up protocol for lung metastasis should be used for these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In Taiwan, colorectal cancer (CRC) is the most common form of cancer and the third leading cause of death [1]. Approximately 50 % of patients with CRC eventually develop distant metastases, resulting in poor outcomes even when these patients have resectable primary tumors. The factors associated with outcomes include tumor stage and levels of carcinoembryonic antigen (CEA) [2]. CEA, a tumor marker, is widely used as an indicator of disease progression or recurrence after resection of primary CRC; currently, CEA level is considered as important as tumor–node–metastasis (TNM) stage [3–8]. However, in CRC patients with normal CEA levels, the 5-year recurrence rate remains as high as 20 % [9]. Several studies have suggested that analyzing CEA in combination with another tumor marker—carbohydrate antigen (CA) 19-9—may increase the prognostic sensitivity [10–12].
CA19-9 is the carbohydrate determinant (sialylated lacto-N-fucopentaose II) of a circulating antigen that functions as an adhesion molecule and plays a role in tumor progression [13]. CA19-9 testing is not used routinely in the management of CRC patients since it is less sensitive than CEA testing [7]. However, many clinicopathologic investigations of CRC have shown it to be a tumor marker [10–13]. In previous studies, the impact of CA19-9 has been masked by variations in CEA. Therefore, the present study aimed to clarify the prognostic value of CA19-9 in patients with curable CRC who have normal CEA levels.
Material and methods
Patients and clinical findings
A total of 2,379 CRC patients who underwent surgery at the Taipei Veterans General Hospital from 2002 to 2006 were initially screened for enrollment in this study. Before surgery, several surveillance procedures were performed, including colonoscopy and computed tomography (CT) scans of the area from the neck to the pelvis. For patients with symptomatic bone pain or high CEA levels, whole-body bone scans were performed. Two hundred one patients who received preoperative chemoradiotherapy, 171 patients who underwent emergency surgery due to obstruction or perforation, 72 patients who had positive or close margins (<1 mm), and 411 patients with distant metastatic disease at the time of surgery were excluded from this study. We also excluded 886 patients whose preoperative CA19-9 levels were not recorded. All clinical findings were recorded in detail prospectively and were stored in computerized files. The database included the following information: (1) name, gender, age, family history, and major medical problems; (2) location, size, gross appearance, stage, differentiation, and important pathological prognostic features of the tumor; and (3) type of operation, complications, recurrence, and follow-up conditions. The disease stage was determined according to the TNM classification system of the American Joint Committee on Cancer [14]. The important pathological features of the tumors were defined according to the consensus statement of the College of American Pathologists [2] and included lymphovascular invasion, intratumoral lymphocytic infiltration, mucinous components, and tumor border configuration (expansive versus infiltrative). After surgery, patients were monitored every 3 months for the first 2 years and every 6 months thereafter. At each visit, imaging studies, including chest radiography and either abdominal ultrasonography or abdominopelvic CT, were performed. Colonoscopy was performed 6 months to 1 year after surgery and every 3 years thereafter. Unscheduled CT, whole-body bone scan, or positron emission tomography was performed for patients with increased serum levels of CEA or CA19-9 or for symptomatic patients. Serum levels of CEA and CA19-9 were measured by radioimmunoassay at the Department of Nuclear Medicine, Taipei Veterans General Hospital. High CEA level was defined as a level exceeding 5 ng/mL. High CA19-9 level was defined level exceeding 37 U/mL according to guidelines defined by the manufacturer of the test kit.
Statistical analysis
The statistical endpoint of the analyses was disease-free survival (DFS) from the date of surgery. The group distributions for each clinicopathologic trait were compared using two-tailed Fisher’s exact procedure and the chi-square test. Numerical values were compared using Student’s t test. Data are expressed as mean±standard deviation. Kaplan–Meier survival curves were plotted and compared using the log-rank test. A multivariate analysis was performed using the Cox proportional hazard model. Statistical significance was defined as P < 0.05. Statistical analyses were performed using SPSS for Windows version 13.0 software.
Results
A total of 639 patients, including 131 (20.5 %) with high CA19-9 levels, were enrolled in this study initially. Of 254 patients with high CEA levels, 79 (31.1 %) also had high CA19-9 levels, a significantly higher percentage than that among patients with normal CEA levels (13.5 %, P < 0.001). After exclusion of the 254 patients (39.7 %) with high preoperative CEA levels, 385 cases with normal CEA levels remained available for further analysis. The patient population was composed of 255 men (66.2 %) and 130 women (33.8 %). The mean age at tumor resection was 67.2 ± 13.7 years (range, 20–96 years; median, 70.7 years). Regarding tumor locations, 261 (67.8 %) were colonic and 124 (32.2) were rectal. In terms of tumor stage, 103 (26.8 %) were stage I tumors; 162 (42.1 %), stage II tumors, and 120 (31.2 %), stage III tumors. Twenty-seven (16.6 %) patients with stage II tumors and 96 (80 %) with stage III tumors received 5-fluorouracil (5-FU)-based chemotherapy.
The baseline characteristics of the CRC patients enrolled in this study are presented in Table 1. High CA19-9 levels were significantly associated with advanced disease status. In particular, 5.8 % of the patients with stage I tumors, 11.7 % of the patients with stage II tumors, and 22.5 % of the patients with stage III tumors had high CA19-9 levels (P < 0.001). Further, high CA19-9 levels were significantly associated with advanced tumor depth. In patients with T1 tumors, 4.4 % had high CA19-9 levels, and among those with T4 tumors, 22.2 % had high CA19-9 levels. Spread to the lymph nodes (LNs) was also associated with CA19-9 levels. Of the 50 patients with N2 tumors, 28 % had high CA19-9 levels, but only 10 % of patients with N0 tumors had high CA19-9 levels. Other clinicopathologic factors, including differentiation, lymphovascular invasion, mucinous component, location, and gender, were not associated with high CA19-9 levels.
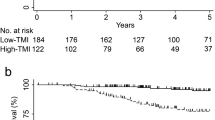
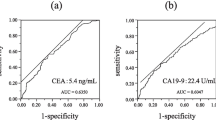
Over a median follow-up period of 56 months (range, 6–176 months), CRC recurred in 68 patients (42 cases of liver metastasis, 36 cases of lung metastasis, and 10 cases of peritoneal carcinomatosis). According to a univariate analysis, the 5-year DFS rate in patients with normal CA19-9 levels was 82.0 % (Table 2), which was significantly higher than that in patients with high CA19-9 levels (68 %; P < 0.001). Other factors influencing the 5-year DFS in the univariate analysis included advanced disease, poor tumor differentiation, mucinous adenocarcinoma, and lymphovascular invasion. According to a multivariate analysis (Table 3), the most important independent factor affecting the 5-year DFS was TNM stage (95 % confidence interval (CI), 1.26–2.36; hazard ratio (HR) = 1.72). After stratification by other factors, high CA19-9 level remained an independent prognostic factor for patients with normal CEA levels. According to the subgroup analysis shown in Fig. 1, CA19-9 had the greatest value as a prognostic factor in patients with stage III disease. For patients with stage III disease and normal CA19-9 levels, the 5-year DFS rate was 64 %, which was significantly higher than that in patients with high CA19-9 levels (41 %, P < 0.001). The prognostic value of CA19-9 levels decreased in patients with earlier stages of disease. Among stage II patients, the impact of CA19-9 was marginally significant (normal CA19-9 vs. high CA19-9; 86 vs. 78 %; P = 0.048). Among stage I patients, no difference was found between the survival of patients with high CA19-9 levels and patients with normal CA19-9 levels. Of the 123 patients who received chemotherapy, the patients with the high CA19-9 levels showed a 5-year DFS of 43.6 %, which was significantly lower than that in patients with normal CA19-9 levels (70.7 %, P < 0.001). In patients who did not receive chemotherapy, the 5-year DFS was similar in patients with high and normal CA19-9 levels (82.3 vs. 86.7 %; P = 0.163).
Survival curves by stage of disease (green: high CA19-9 level; blue: normal CA19-9 level). a For patients with stage I disease, CA19-9 levels did not predict patient outcomes. b For patients with stage II disease, the 5-year DFS of those with normal CA19-9 levels was 86 %, which was significantly higher than that of patients with high CA19-9 levels (P = 0.048). c For patients with stage III disease, the 5-year DFS of those with high CA19-9 levels was 41 %, but that of patients with normal CA19-9 levels was 64 % (P = 0.004)
Discussion
This study demonstrates that CA19-9 level may be a prognostic marker for CRC patients with normal CEA levels. Unlike CEA, which has been used as an independent prognostic factor for CRC in several consensus treatment guidelines, the value of CA19-9 has been overlooked, especially in patients with high CEA levels [3–8]. Indeed, in our cohort, the prognostic value of CEA was superior to that of CA19-9. Without stratification by CEA level, the 5-year DFS of patients with high CA19-9 levels was 75.4 %, which did not significantly differ from that of patients with normal CA19-9 levels (81.4 %, P = 0.103). Therefore, CA19-9 may not be a valuable prognostic marker for CRC patients with high CEA levels. Furthermore, of the CRC patients enrolled in this study, nearly 40 % had high CEA levels, but only 20 % had elevated levels of CA19-9. Previous studies have suggested that the relatively low sensitivity of CA19-9 testing in patients with CRC may be because patients with a Lewisa-b- genotype cannot synthesize the CA19-9 antigen since the antigenic determinant of CA19-9 is a sialylated derivative of the Lewisa antigen [15, 16]. Since the sensitivity of CA19-9 testing is low and since its prognostic value can be masked by CEA, CA19-9’s utility as a prognostic factor is limited to patients with normal CEA levels.
Only 13.5 % of CRC patients with normal CEA levels had high CA19-9 levels. Among these patients, CA19-9 emerges as a prognostic predictor since high CA19-9 levels were associated with advanced disease. Among patients with stage I disease, only 6.1 % had high CA19-9 levels; this increased to 23.6 % in those with stage III disease. Further, high levels of CA19-9 were associated with deeper tumor invasion and spreading to the LNs. In the univariate and multivariate analyses, CA19-9 was as an independent prognostic factor in addition to TNM stage, differentiation, and lymphovascular invasion. Moreover, patients with poorly differentiated tumors showed higher CA19-9 levels. These results are comparable to those of previous studies [10–12]. We also found that patients with high levels of CA19-9 also had a higher risk of lung metastasis, indicating that the prognostic value of CA19-9 is not restricted to primary CRC alone. Of the 52 patients with high CA19-9 levels, 15 developed distant metastases, including 12 cases of lung metastases (23.1 %). In contrast, of the 333 patients with normal CA19-9 levels, 53 had tumor recurrence, including lung metastases (24 cases, 7.2 %). These results suggest that CA19-9 is a surrogate marker for hematogenous metastasis. Therefore, in patients with high levels of CA19-9, aggressive screening for lung metastasis should be mandatory. Previous studies have shown that cancer cells expressing CA19-9 can adhere to endothelial cells through E-selectin. The attachment between cancer cells and endothelial cells is an important process in tumor metastasis [17, 18]. The present study reveals that CA19-9 level is relevant as a prognostic factor for patients with intermediate disease but not for those with early disease. Only 6 % of patients with stage I disease had high CA19-9 levels. Moreover, in patients with stage I disease, the 5-year DFS was almost 90 %. However, in order to achieve statistical significance supporting the role of CA19-9 as a prognostic factor for patients with stage I disease, the minimum required sample size is estimated to be 2,000 cases.
There are various molecular biological differences between colon and rectal cancers, which result to their clinicopathologic differences [19–21]. We performed separate analyses according to different tumor locations (Supplement Table) and found similar CA19-9 levels, tumor behavior, and patient outcomes between patients with cancers of the colon and rectum.
For patients with stage III or high-risk stage II CRC, current guidelines of National Comprehensive Cancer Network recommend 5-FU-based chemotherapy [22]. Our study showed that patients with high CA19-9 levels had poor outcomes, especially patients who underwent chemotherapy (Fig. 2). For patients who did not undergo chemotherapy, however, CA19-9 level was not a prognostic marker. These results suggest that high CA19-9 level is a marker of aggressive tumor behavior but not an indicator of chemotherapeutic response.
Survival curves by status of chemotherapy (green: high CA19-9 level; blue: normal CA19-9 level). a For patients receiving chemotherapy, the 5-year DFS of patients with high CA19-9 levels was 43.6 % and that of patients with normal CA19-9 levels was 70.7 %. b For patients who did not undergo chemotherapy, CA19-9 level was not a predictor of patient outcomes
Our study has limitations associated with its retrospective nature since we did not employ CA19-9 testing as part of the routine preoperative surveillance or the follow-up procedures after colon cancer surgery. Consequently, nearly 60 % of the CRC cases were excluded at the time of enrollment. We do not know if the inclusion of these cases would have had influenced the patient outcome statistics. Furthermore, follow-up data on CA19-9 levels were unavailable; therefore, we could not investigate whether increased CA19-9 levels preceded tumor recurrence, as is the case for CEA levels. In addition, we enrolled only those patients for whom preoperative CEA and CA19-9 data were available. Therefore, the kinetics of CA19-9 level could not be established in order to clarify whether it could be used as a surrogate indicator of tumor clearance. In the future, prospective studies in which CA19-9 kinetics are analyzed through routine measurement of CA19-9 levels at follow-up are required, especially for patients with normal CEA levels.
In conclusion, CA19-9 may be a valuable prognostic marker for CRC patients with normal CEA levels. For patients with increased CA19-9 levels, an aggressive follow-up protocol for hematogenous metastasis should be considered.
Abbreviations
- CEA:
-
Carcinoembryonic antigen
- CRC:
-
Colorectal cancer
- DFS:
-
Disease-free survival
References
The Department of Health, the Executive Yuan, Taiwan (2007) Cancer registry annual report (December 2007). The Department of Health, the Executive Yuan, Taiwan
Compton CC, Fielding LP, Burgart LJ, Conley B, Cooper HS, Hamilton SR, Hammond ME, Henson DE, Hutter RV, Nagle RB, Nielsen ML, Sargent DJ, Taylor CR, Welton M, Willett C (2000) Prognostic factors in colorectal cancer. College of American Pathologists Consensus Statement 1999. Arch Pathol Lab Med 124:979–994
Desch CE, Benson AB 3rd, Somerfield MR, Flynn PJ, Krause C, Loprinzi CL, Minsky BD, Pfister DG, Virgo KS, Petrelli NJ (2005) Colorectal cancer surveillance: 2005 update of an American Society of Clinical Oncology practice guideline. J Clin Oncol 23:8512–8519
Compton C, Fenoglio-Preiser CM, Pettigrew N, Fielding LP (2000) American Joint Committee on Cancer Prognostic Factors Consensus Conference: Colorectal Working Group. Cancer 88:1739–1757
Bast RC Jr, Ravdin P, Hayes DF, Bates S, Fritsche H Jr, Jessup JM, Kemeny N, Locker GY, Mennel RG, Somerfield MR (2001) 2000 update of recommendations for the use of tumor markers in breast and colorectal cancer: clinical practice guidelines of the American Society of Clinical Oncology. J Clin Oncol 19:1865–1878
Duffy MJ, van Dalen A, Haglund C, Hansson L, Klapdor R, Lamerz R, Nilsson O, Sturgeon C, Topolcan O (2003) Clinical utility of biochemical markers in colorectal cancer: European Group on Tumour Markers (EGTM) guidelines. Eur J Cancer 39:718–727
Locker GY, Hamilton S, Harris J, Jessup JM, Kemeny N, Macdonald JS, Somerfield MR, Hayes DF, Bast RC Jr (2006) ASCO 2006 update of recommendations for the use of tumor markers in gastrointestinal cancer. J Clin Oncol 24:5313–5327
Duffy MJ, van Dalen A, Haglund C, Hansson L, Holinski-Feder E, Klapdor R, Lamerz R, Peltomaki P, Sturgeon C, Topolcan O (2007) Tumour markers in colorectal cancer: European Group on Tumour Markers (EGTM) guidelines for clinical use. Eur J Cancer 43:1348–1360
Lin JK, Lin CC, Yang SH, Wang HS, Jiang JK, Lan YT, Lin TC, Li AF, Chen WS, Chang SC (2011) Early postoperative CEA level is a better prognostic indicator than is preoperative CEA level in predicting prognosis of patients with curable colorectal cancer. Int J Colorectal Dis 26:1135–1141
Nakagoe T, Sawai T, Tsuji T, Jibiki MA, Nanashima A, Yamaguchi H, Yasutake T, Ayabe H, Arisawa K (2003) Preoperative serum level of CA19-9 predicts recurrence after curative surgery in node-negative colorectal cancer patients. Hepatogastroenterology 50:696–699
Chen CC, Yang SH, Lin JK, Lin TC, Chen WS, Jiang JK, Wang HS, Chang SC (2005) Is it reasonable to add preoperative serum level of CEA and CA19-9 to staging for colorectal cancer? J Surg Res 124:169–174
Nozoe T, Rikimaru T, Mori E, Okuyama T, Takahashi I (2006) Increase in both CEA and CA19-9 in sera is an independent prognostic indicator in colorectal carcinoma. J Surg Oncol 94:132–137
Del Villano BC, Brennan S, Brock P, Bucher C, Liu V, McClure M, Rake B, Space S, Westrick B, Schoemaker H, Zurawski VR Jr (1983) Radioimmunometric assay for a monoclonal antibody-defined tumor marker, CA 19–9. Clin Chem 29:549–552
Greene FLPD, Fleming ID, Fritz AG, Balch CM, Haller DG, Morrow M (2002) AJCC cancer staging manual, 6th edn. Springer, Chicago
Magnani JL, Nilsson B, Brockhaus M, Zopf D, Steplewski Z, Koprowski H, Ginsburg V (1982) A monoclonal antibody-defined antigen associated with gastrointestinal cancer is a ganglioside containing sialylated lacto-N-fucopentaose II. J Biol Chem 257:14365–14369
Nakayama T, Watanabe M, Teramoto T, Kitajima M (1997) CA19-9 as a predictor of recurrence in patients with colorectal cancer. J Surg Oncol 66:238–243
Berg EL, Magnani J, Warnock RA, Robinson MK, Butcher EC (1992) Comparison of L-selectin and E-selectin ligand specificities: the L-selectin can bind the E-selectin ligands sialyl Le(x) and sialyl Le(a). Biochem Biophys Res Commun 184:1048–1055
Nakayama T, Watanabe M, Teramoto T, Kitajima M (1997) Slope analysis of CA19-9 and CEA for predicting recurrence in colorectal cancer patients. Anticancer Res 17:1379–1382
Redson M (2001) Carcinogenesis in the GI tract: from morphology to genetics and back again. Mod Pathol 230:309–318
Distler P, Holt PR (1997) Are right and left-sided colon neoplasms distinct tumors? Dig Dis 15:302–311
Thibodeau SN, Bren G, Schaid D (1993) Microsatellite instability in cancer of the proximal colon. Science 260:816–819
Engstrom PF, Arnoletti JP, Benson AB 3rd, Chen YJ, Choti MA, Cooper HS et al (2009) NCCN Clinical Practice Guidelines in Oncology: colon cancer. Natl Compr Cancer Netw 7:778–831
Acknowledgments
This study was supported by a grant from Taipei Veterans General Hospital. (VGH100C-007, VGH100E2-008).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplement Table 1
(DOC 32 kb)
Rights and permissions
About this article
Cite this article
Lin, PC., Lin, JK., Lin, CC. et al. Carbohydrate antigen 19-9 is a valuable prognostic factor in colorectal cancer patients with normal levels of carcinoembryonic antigen and may help predict lung metastasis. Int J Colorectal Dis 27, 1333–1338 (2012). https://doi.org/10.1007/s00384-012-1447-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-012-1447-1