Abstract
Background
Colorectal cancer (CRC) remains the third most common cancer in the world. Approximately in 50 percent of patients, metastatic disease is a major cause of death. Therefore, early diagnosis of CRC is crucial for a successful outcome. For the detection of circulating cancer cells, this study applied a sensitive method that employed specific tumor markers for early detection.
Methods
A total of 80 blood samples from 40 CRC patients and 40 age-matched healthy controls were collected for the study. The circulating mRNA levels of two CRC tumor markers, tumor endothelial marker 8 (TEM-8) and carcinoembryogenic antigen (CEA) were evaluated using an absolute quantitative real-time PCR assay in a Stratagene Mx-3000P real-time PCR system. GAPDH was used as the endogenous control.
Results
TEM-8 and CEA were primarily detected more in the CRC patients rather than in the controls: 22/40 vs 9/40, p=0.009 and 30/40 vs 11/40, p=0.00054, respectively. In the CRC patients, the mRNA level of these markers was significantly higher in comparison to the normal controls (p=0.018 and 0.01). The overall sensitivity of this panel was 65% with a specificity of 75%. Statistical analysis for demographic variants did not reach significant values.
Conclusions
TEM-8 and CEA markers were detected more frequently and in significantly higher levels in the blood samples of patients compared with samples from age-matched healthy controls. The copy number of CEA and TEM-8 mRNA, as detected by a real-time quantitative PCR, appears to be a promising marker for evaluating the risk of tumor spread.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nearly 400,000 lives are lost annually to colorectal cancer (CRC), the third most prevalent tumor type in the world [1, 2]. Throughout the past two decades, in spite of trifling diminution in the incidence and mortality of cancer in developed nations, such as the USA, CRC remains the third most common cancer in these countries with 50,000 deaths per year [3]. In Iran, CRC is also reported as one of the most frequent malignancies, with an incidence rate of eight per 100,000 in both sexes and a mortality rate of 1.3 in females and 1.8 in males per 100,000 [4]. As several researchers have reported, out of approximately 40–50% of CRC patients who undergo tumor resection, there is a subsequent metastasis through the bloodstream or lymphatic circulation to other organs which decreases the 5-year survival of patients with CRC [5]. Therefore, early detection with accurate methods is absolutely vital [6].
The best therapeutic method is the elimination of the tumor in its early stages. The feasibility of a successful treatment after tumor resection depends on the tumor stage. The TNM staging system is a conventional method for tumor stage investigation. Although this system can determine tumor prognoses, it has some treatment failures [7]. Consequently, several sensitive methods for molecular staging using high-throughput techniques have been developed to distinguish micrometastasis [7]. Molecular staging can now be evaluated in the lymph nodes, bone marrow, and blood of patients [8]. Real-time PCR monitoring systems have also been introduced to identify the mRNA of circulating tumor cells in cancer patients [9]. This approach allows the precise quantification of the initial template copy number, based on conversely correlating the cycle number, at which the sample fluorescence exceeds the background level, with the starting copy number [10]. Markers used for the PCR detection of tumor cells are dependent upon the particular traits of the tissue, from which the tumor originates. For instance, carcinoembryonic antigen (CEA) described as a protein with an oncofetal expression pattern, may act as a hemophilic and heterothallic cell adhesion molecule when expressed on the tumor cell surface. CEA also performs a significant function throughout embryogenesis as well as tumor development [11]. Another marker, the tumor epithelial marker 8 (TEM-8) is a type I transmembrane protein with 564 amino acids in length. It may play a role in the interaction of cells with the surrounding extracellular matrix and angiogenesis [12]. TEM-8 is unique among other cell surface TEMs as its expression is tumor specific and has not been discerned in physiologic angiogenesis in adults [13]. In this study, a quantitative real-time reverse transcription-polymerase chain reaction (RT-PCR) was applied to detect CEA and TEM-8 mRNA expression in the peripheral blood of CRC patients for the purposes of investigating the sensitivity of these markers in detecting microinvasion.
Materials and methods
Study subjects
Between March 2008 and February 2011, 80 blood samples were collected, consisting of samples from 40 CRC patients, before having surgery or other therapeutic procedures including preoperative chemotherapy or radiotherapy, and from 40 healthy volunteers with normal colonoscopy reports. In accordance with the MUMS ethical guidelines, all of the CRC patients and healthy volunteers were informed about the study and gave their written consent for the investigation.
RNA extraction and cDNA synthesis
Five milliliters of blood samples were diluted with 5 mL of phosphate-buffered saline. Peripheral blood mononuclear cells were collected using a lymphocyte separation medium. Total RNA was extracted from the cells by conventional methods using a Trizol reagent (Roche, Applied Sciences, Indianapolis, IN) according to the manufacturer’s instructions. RNA quality and quantity were evaluated at an absorbance of 260 and 280 nm using an ultraviolet spectrophotometer. First-strand cDNA was synthesized from 1 μg total RNA and oligo(dT)18 as amplification primers applying a RT-PCR kit (Fermentas, Vilnius, Lithuania).
Construction of standards
MAD-MB231 and HT29 cell lines were grown in a RPMI-1640 medium supplemented with 10% fetal bovine serum at 37°C in a 5% CO2 air environment. When grown to a confluent monolayer, MAD-MB231 and HT29 cells were harvested. The RNA from these cell lines were used for the TEM-8 and CEA standard curve, respectively. To prepare the standard curve, cDNAs were amplified and inserted into the pTZR/57 vector (Fermentas, Vilnius, Lithuania). After cloning, recombinant vectors were extracted, linearized with SacΙ, and serially diluted. Copy numbers were calculated for all standards with the following formula [14].
6.022×1023 [molecules/mole] Avogadro’s number
660 Da Average weight of a single base pair
The cloning and real-time RT-PCR primers for CEA, TEM-8, and glyceraldehyde 3-phosphate dehydrogenase (GAPDH), as an internal control, and the fluorogenic probe for TEM-8 were designed by AlleleID software 6.0, as shown in Table 1.
Quantitative real-time RT-PCR
Real-time PCR was performed in a Stratagene Mx-3000P (Stratagene, La Jolla, CA) thermocycler. SYBR green was used for the amplification of the CEA, and TaqMan probes were utilized for TEM-8 in a total volume of 20 μl using absolute quantitative, ΔCt method [15]. For CEA, each reaction consisted of: 10 μl SYBR green, 2 μl cDNA, 0.5 μl of each primer (10 pmol/μl), and 7 μl RNase-free water. Thermal cycling conditions were 10 min at 95°C followed by 45 cycles at 95°C for 40 s, 62°C for 40 s, and 72°C for 40 s. For TEM-8, the PCR reaction contained 10 μl Maxima probe master mix, 2 μl cDNA, 0.2 μl probe, 0.6 μl of each primer (10 pmol/μl), and 7.2 μl RNAse-free water. The thermal cycle program was as following: 10 min at 95°C followed by 45 cycles at 95°C for 30 s, 62°C for 40 s, and 72°C for 30 s. GAPDH was employed as an endogenous control to normalize the data. All samples were analyzed in duplicate.
Statistical analysis
All data were analyzed using SPSS version 11.1 (SPSS Inc, Chicago, IL), and P<0.05 was considered statistically significant. The Kruskal–Wallis, Mann Whitney U, and Spearman’s test were used to investigate the association of the copy number with sex, tumor location, stage and grade, and also lymph node involvement. The t test was utilized to compare the copy number of each target between cases and controls. Pearson’s correlation was used to classify age, age of onset, and tumor size.
Results
A total of 40 patients with primary colorectal cancer (male/female, 30:10; mean age, 57.4±18.76 years) and 40 healthy controls (male/female, 24:16; mean age, 57.3±7.4 years) were recruited for the study. As shown in the Table 2, the majority of the tumors were adenocarcinoma located on the distal colon, with stage IIA in the TNM staging system and varied between 1 to 5 cm in size. Most patients (75%) had intact lymph nodes representing localized tumors.
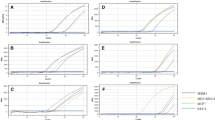
Real-time PCR analysis of the circulating mRNA levels of the two tumor markers, TEM-8 and CEA, revealed a significantly higher presence of both markers in the peripheral blood of the CRC patients than in that of the controls, 22/40 vs 9/40, p=0.0054 for TEM-8 and 30/40 vs 11/40, p=0.009 for CEA, respectively. The mRNA level of these markers in patients was significantly higher in comparison to normal controls (p=0.018 and 0.01, respectively) (Fig. 1). These two markers produced an overall sensitivity of 65% with a specificity of 75% from circulating tumor cells.
Discussion
Before metastasis becomes obvious, some tumor cells dissent from a tumor and spread through the lymph nodes and blood to distant organs [7]. Although most tumor cells are not viable, a few remaining tumor cells have the capability to form metastasis [16].Therefore, monitoring these cells in the blood and lymph nodes should be an appropriate approach for metastasis prediction and as a new staging method. To date, not many sensitive techniques have been available for the detection of disseminated tumor cells in the blood samples of CRC patients, involving flowcytometery [17], immunohistochemistry [18], and RT-PCR [19]. In contrast, qRT-PCR integrates the high efficiency of PCR and the high sensitivity and accurate quantification of spectral analysis. The efficacy of the qRT-PCR assay in the detection of CTCs in blood depends on a balance of sensitivity and specificity. In other words, the assay must be sensitive enough to detect very small numbers of tumor cells and must also be specific enough to detect transcripts for those derived from tumor cells [20]. There are tumor markers detectable in CRC patients, which can predict the early stage of metastasis; some of these markers are detectable in lymph nodes while others are present in the peripheral blood [21]. The detection rate of CTCs in the peripheral blood of CRC patients ranges from 27% to 88% [6, 22–24].
Although many markers have been investigated alone or in several panels, such as CK20, Survivin, and GCC in CRC patients, the absence of both sensitivity and specificity was shown in these experiments. Therefore, many investigators have studied different genetic alternations in the tissue and stool DNA of CRC patients in order to determine sensitivities and specific markers as a diagnostic tool [25]. To date, the lack of a single specific tumor marker for reliable detection of CRC patients remains a fundamental problem.
These experimental results shows that tumor cells are more frequently present in the circulation of colorectal cancer patients which can predict development of metastasis. Therefore, this method may be utilized to detect wide spreading of a tumor and distant metastasis earlier than any other imaging or pathology approach. Perhaps, future investigations on tumor signaling pathways and cancer stem cells will assist in developing a single marker or a panel of markers for early detection of CRC. Another issue under debate is the clinical application of this method. Future cohort studies monitoring larger number of patients seems to be necessary in order to evaluate the prognostic value of each marker and to determine the subgroup of patients with a high level of a specific tumor marker. Such patients would require more aggressive treatment including more potent chemotherapeutic regimens.
References
Pisani P, Parkin DM, Bray F, Erratum FJ (1999) Estimates of the worldwide mortality from 25 cancers in 1990. Int J Cancer 83:18–29
Burt RW, DiSario JA, Cannon-Albright L (1995) Genetics of colon cancer: impact of inheritance on colon cancer risk. Annu Rev Med 46:371–379
Greenlee RT, Hill-Harmon MB, Murray T, Thun M (2001) Cancer statistics, 2001. CA Cancer J Clin 51:15–36
Mousavi SM, Gouya MM, Ramazani R, Davanlou M, Hajsadeghi N, Seddighi Z (2009) Cancer incidence and mortality in Iran. Ann Oncol 20:556–563
Yeh CS, Wang JY, Wu CH, Chong IW, Chung FY, Wang YH et al (2006) Molecular detection of circulating cancer cells in the peripheral blood of patients with colorectal cancer by using membrane array with a multiple mRNA marker panel. Int J Oncol 28:411–420
Xu D, Li XF, Zheng S, Jiang WZ (2006) Quantitative real-time RT-PCR detection for CEA, CK20 and CK19 mRNA in peripheral blood of colorectal cancer patients. J Zhejiang Univ Sci B 7:445–451
Silva JM, Rodriguez R, Garcia JM, Munoz C, Silva J, Dominguez G et al (2002) Detection of epithelial tumour RNA in the plasma of colon cancer patients is associated with advanced stages and circulating tumour cells. Gut 50:530–534
Bustin SA, Mueller R (2006) Real-time reverse transcription PCR and the detection of occult disease in colorectal cancer. Mol Aspects Med 27:192–223
Holland PM, Abramson RD, Watson R, Gelfand DH (1991) Detection of specific polymerase chain reaction product by utilizing the 5′—3′ exonuclease activity of Thermus aquaticus DNA polymerase. Proc Natl Acad Sci USA 88:7276–7280
Gerard CJ, Olsson K, Ramanathan R, Reading C, Hanania EG (1998) Improved quantitation of minimal residual disease in multiple myeloma using real-time polymerase chain reaction and plasmid-DNA complementarity determining region III standards. Cancer Res 58:3957–3964
Schrewe H, Thompson J, Bona M, Hefta LJ, Maruya A, Hassauer M et al (1990) cloning of the complete gene for carcinoembryonic antigen: analysis of its promoter indicates a region conveying cell type-specific expression. Mol Cell Biol 10:2738–2748
Nanda A, St Croix B (2004) Tumor endothelial markers: new targets for cancer therapy. Curr Opin Oncol 16:44–49
Rmali KA, Puntis MC, Jiang WG (2005) TEM-8 and tubule formation in endothelial cells, its potential role of its vW/TM domains. Biochem Biophys Res Commun 334:231–238
Godornes C, Leader BT, Molini BJ, Centurion-Lara A, Lukehart SA (2007) Quantitation of rabbit cytokine mRNA by real-time RT-PCR. Cytokine 38:1–7
Schmittgen TD, Livak KJ (2008) Analyzing real-time PCR data by the comparative (CT) method. Nat Protoc 3:1101–1108
Shen C, Hu L, Xia L, Li Y (2008) Quantitative real-time RT-PCR detection for survivin, CK20 and CEA in peripheral blood of colorectal cancer patients. Jpn J Clin Oncol 38:770–776
Cruz I, Ciudad J, Cruz JJ, Ramos M, Gomez-Alonso A, Adansa JC et al (2005) Evaluation of multiparameter flow cytometry for the detection of breast cancer tumor cells in blood samples. Am J Clin Pathol 123:66–74
Turner RR, Giuliano AE, Hoon DS, Glass EC, Krasne DL (2001) Pathologic examination of sentinel lymph node for breast carcinoma. World J Surg 25:798–805
Ghossein RA, Bhattacharya S, Rosai J (1999) Molecular detection of micrometastases and circulating tumor cells in solid tumors. Clin Cancer Res 5:1950–1960
Zieglschmid V, Hollmann C, Bocher O (2005) Detection of disseminated tumor cells in peripheral blood. Crit Rev Clin Lab Sci 42:155–196
Ohlsson L, Hammarstrom ML, Israelsson A, Naslund L, Oberg A, Lindmark G et al (2006) Biomarker selection for detection of occult tumour cells in lymph nodes of colorectal cancer patients using real-time quantitative RT-PCR. Br J Cancer 95:218–225
Wang JY, Wu CH, Lu CY, Hsieh JS, Wu DC, Huang SY et al (2006) Molecular detection of circulating tumor cells in the peripheral blood of patients with colorectal cancer using RT-PCR: significance of the prediction of postoperative metastasis. World J Surg 30:1007–1013
Lloyd JM, McIver CM, Stephenson SA, Hewett PJ, Rieger N, Hardingham JE (2006) Identification of early-stage colorectal cancer patients at risk of relapse post-resection by immunobead reverse transcription-PCR analysis of peritoneal lavage fluid for malignant cells. Clin Cancer Res 12:417–423
Conzelmann M, Linnemann U, Berger MR (2005) Molecular detection of clinical colorectal cancer metastasis: how should multiple markers be put to use? Int J Colorectal Dis 20:137–146
Abbaszadegan MR, Tavasoli A, Velayati A, Sima HR, Vosooghinia H, Farzadnia M et al (2007) Stool-based DNA testing, a new noninvasive method for colorectal cancer screening, the first report from Iran. World J Gastroenterol 13:1528–1533
Acknowledgments
This study was supported by a grant from the Iran National Science Foundation (#85122/68) at Mashhad University of Medical Sciences. The authors sincerely thank all of their colleagues at the Human Genetics Division of the Avicenna Research Institute who contributed in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Raeisossadati, R., Farshchian, M., Ganji, A. et al. Quantitative analysis of TEM-8 and CEA tumor markers indicating free tumor cells in the peripheral blood of colorectal cancer patients. Int J Colorectal Dis 26, 1265–1270 (2011). https://doi.org/10.1007/s00384-011-1230-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-011-1230-8