Abstract
Background and aims
Caecal intubation fails up to 20% of colonoscopy in clinical practice. We aimed to assess whether (1) in patients with a prior incomplete colonoscopy with a standard adult colonoscope, a subsequent caecal intubation may be achieved with the same instrument; (2) there are factors predicting a repeated unsuccessful colonoscopy; and (3) how frequently completion can be further achieved by shifting to a standard gastroscope.
Materials and methods
Data of patients with a previously failed bowel examination referred to our community hospital for a further colonoscopy were reviewed. When caecal intubation still failed with standard colonoscope, complete colonoscopy was usually attempted by shifting to a gastroscope.
Results
Overall, 451 patients with a prior colonoscopy were considered. By using a standard colonoscope, caecal intubation rate was achieved in 285 out of 296 patients with prior complete examination and in 121 out of 155 patients with a prior failed colonoscopy (96.3% vs. 78.1%, p < .001). Caecum visualization was significantly lower when prior colonoscopy was stopped in the sigmoid tract as compared to any other proximal tract (65.1% vs. 86.9%, p < .001). After a second failed examination, colonoscopy was completed in 15 (51.7%) out of 29 cases by shifting to a standard gastroscope. No procedure-related complications were observed in the study.
Conclusions
After incomplete colonoscopy with a standard adult colonoscope, a further colonoscopy may be completed with same standard colonoscope or by using a gastroscope in the same session. A prior failed colonoscopy, particularly when stopped in the sigmoid tract, is significantly associated with a lower caecal intubation rate at second colonoscopy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Visualization of the caecal region is an indicator of colonoscopy quality. It has been suggested that a caecal intubation rate >90% and >95% should be achieved in a screening setting and in symptomatic patients, respectively, by excluding those cases failed due to inadequate bowel preparation or severe colitis [1]. Nevertheless, several studies have found a caecal intubation rate ranging from 91% to 97.7% in screening colonoscopy [2–4] and from 76.9% and 89.1% [5–7] in clinical practice—or even lower [8]. Moreover, a very large study evaluating 331,608 examinations found a caecal visualization in 86.9% of cases during routine colonoscopies [9]. Following an incomplete colonoscopy with standard adult colonoscope, colonic examination could be completed either by using double contrast barium enema, virtual colonoscopy, and magnetic resonance colonography or by a subsequent endoscopy [10]. In the latter case, caecal intubation is usually achieved by shifting to a different colonoscope, such as paediatric or slim colonoscope and single or double balloon enteroscope, or by using a gastroscope [11]. An anatomic alteration of the colon—such a neoplastic stricture—may either hinder the advancement of the instrument or result in a painful progression. Furthermore, complications could arise from the pressure released by the instrument towards the colonic wall. On the other hand, looping formation due to incorrect handling may prevent achieving the caecum in a patient with a prior complete colonoscopy.
Focusing on these aspects, the present study aimed to assess whether (1) after a failed colonoscopy with colonoscope, the caecal visualization may be achieved by using a similar standard adult colonoscope; (2) there are factors predicting unsuccessful repeated colonoscopy; and (3) in the event of failure, it is possible to complete colonoscopy by shifting to a standard gastroscope in the same session.
Materials and methods
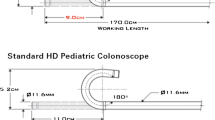
In this retrospective study, we reviewed the endoscopic reports of all patients who, following either a complete or incomplete colonoscopy in another community hospital, underwent colonoscopy in our endoscopy unit. In detail, data were extracted of a self-developed data collection file we adopted since January 2006. The medical chart of patients was also reviewed when incomplete clinical information was registered. We considered only those cases that previously underwent a colonoscopy by using a standard adult colonoscope in conscious sedation. Demographic and clinical data, including previous abdominal surgery, the colon tract reached (sigmoid tract, left flexure, transverse, right flexure, ascending, and caecum) in the previous colonoscopy, the cause of caecum intubation failure, and the previous endoscopic diagnose were analyzed. Those cases in whom this information on the index endoscopy was either unavailable or doubtful were excluded from the analysis. Those incomplete colonoscopies due to either a poor bowel preparation or a neoplastic stricture preventing the instrument to pass through were also excluded as well as planned sigmoidoscopy. Those patients who underwent colonic surgery due to a benign stricture—i.e., diverticular disease or ischemic colitis or inflammatory bowel disease (IBD)—between the first and second colonoscopy where not taken into account. In our endoscopy unit, colonoscopy was performed following a standard bowel preparation with 4,000 mL of polyethylene glycol-containing lavage solution. Five experienced endoscopists performed colonoscopy with a conscious sedation (midazolam, 2.5–5 mg i.v.) of patients. In all cases, examination was started with the patient on the left side and position was usually changed to supine when the instrument overcome the left flexure until the visualization of the caecum, defined as complete inspection of both appendiceal orifice and ileocaecal valve. Those colonoscopies in which solely the ileocaecal valve observed from a variable distance from the ascending colon were considered incomplete. For all endoscopic examinations, to minimize patient discomfort, the progression of endoscope was facilitated by an expert nurse, including pressure on the abdomen when needed [12]. All endoscopic examinations were performed by using a standard adult colonoscope (Olympus Exera II CV165, Milan, Italy). In the event of stricture, looping, or angulation in the sigmoid tract preventing or making intensely painful the passage of colonoscope, the caecal intubation was generally attempted by shifting to a standard adult gastroscope in the same session.
Statistics
Data between patient subgroup were compared by using the Student’s t test for unpaired data, χ 2 test, and Fisher’s exact test as appropriate. A p level less than.05 was considered statistically significant.
Results
During the period January 2006 and December 2008, a total of 5,017 lower endoscopies were performed, including 4,219 (84.1%) diagnostic and 798 (15.9%) screening colonoscopy. The overall caecal intubation rate was 93.4%, being 93.1% and 95.1% for diagnostic and screening endoscopy, respectively. Among these examinations, there were 474 patients who previously underwent colonoscopy. Among these patients, 296 and 178 patients had a prior complete and incomplete colonoscopy, respectively. Twenty-three out of 178 patients with an incomplete colonoscopy were excluded because the endoscopic report was not available (19 cases) or the colon tract reached in the prior endoscopy was not clearly reported (4 cases). Therefore, the final study population consisted of 451 patients (mean age, 60.1 ± 16.3; male/female [M/F], 188/263), including 296 with a previously complete colonoscopy and 155 with a partial colonoscopy.
Overall, during the endoscopy performed in our unit, the caecum was visualized in 285 out of the 296 patients who previously completed the colonoscopy and in 121 out of the 155 patients with an incomplete colonoscopy (96.3% vs. 78.1%, p < .001). In the 11 patients with previously complete colonoscopies in whom we failed caecal intubation, the cause was pain despite sedation (four cases), redundant looping (four cases), and excessive angulation (three cases). Regarding the 155 patients with a prior incomplete colonoscopy, the second examination was performed <1 year (median time, 4 months; range, 1–6) in 114 cases, whilst in the remaining 41 patients, it was carried out >1 year (median time, 16 months; range, 13–22). Data on caecal visualization by using a standard colonoscope in this patient group are provided in Table 1. The caecal intubation rate was significantly (p < 0.001) lower in those patients in whom the previous colonoscopy was interrupted in the sigmoid tract (41 out of 63, 65.1%) as compared to all the other sites cumulatively considered (80 out of 92, 86.9%). No difference emerged between patients with complete and incomplete colonoscopy as far as mean age (62.7 ± 12.7 vs. 59.2 ± 17.2 years; p = 0.19), sex distribution (M/F, 50/71 vs. 19/15; p = 0.13), and previous abdominal surgery (35.6% vs. 29.4%, p = 0.5) is concerned. Moreover, the caecal intubation rate did not significantly differ between patients who had a further colonoscopy within 1 year from those with a longer interval (88.2% vs. 76%, p = 0.11).
Caecal intubation was attempted by using a standard gastroscope in 29 out of 34 patients in whom bowel examination with standard colonoscope was still unsuccessful. In the these 29 patients, the cause of colonoscopy failure was (a) severe diverticular disease with a benign stricture and/or angulation in 20 cases (all in the sigmoid tract), (b) angulation without macroscopic lesion in 7 patients (sigmoid tract, 2; descending colon, 3; left flexure, 2), and (c) redundant looping in 2 cases (all transverse colon). As shown in Table 2, it was possible to reach the caecum in 15 (51.7%) patients and to surmount the colon tract previously reached with the colonoscope in further 4 (13.8%) cases, whilst in the remaining 10 (34.5%) patients, the examination was stopped at the same colon site (6 in sigmoid tract, 1 in descending colon, 1 in the left flexure, 2 in the transverse). Although caecal intubation rate with the gastroscope in patients with diverticular disease (12 out of 20) was twice than that in patients with either angulation or excessive looping (3 out of 9), the difference did not reach the statistical significance (60% vs. 33.3%, p = 0.13).
Overall, among the initial 150 patients in whom colonoscopy was attempted by using both standard colonoscope and gastroscope, it was possible to reach the caecum in 136 (90.7%) cases—including 121 with a colonoscope and 15 shifting to gastroscope—and to perform a partial examination overcoming the previously reached colon site in other 4 (2.6%) cases—all with gastroscope. No procedure-related complications were observed in the study.
Discussion
An accurate observation of the entire colonic mucosa during colonoscopy leads to a detection of both precancerous and neoplastic lesions [1, 13]. Total colonoscopy is the main indicator of colonoscopy quality, with caecal intubation rates higher than 90% and 95% being advised in clinical practice and screening setting, respectively [1]. The caecal intubation rates in our centre were 93.1% and 95.1%, respectively, during the considered 3-year period. Several studies have found that total colonoscopy failed up to 20% in usual practice [5–9]. A recent, nationwide, observational study performed in 278 Italian centres with more than 12,000 examinations found that complete colonoscopy was achieved in 80.7% of cases, and only 22.1% of the centres reported a caecal intubation rate >90% [14]. Different factors have been associated with caecal intubation failure of first colonoscopy, including older age of patient, female gender, low body mass index, personal history of abdominal or pelvic surgery, advanced diverticular disease, private setting, afternoon examination, colonoscopy performed by a nongastroenterologist, and low-volume colonoscopies [6, 9, 15, 16]. Therefore, a further bowel examination, generally by using an imaging technique or a further endoscopy [10, 17], is required in a considerable number of patients who failed total colonoscopy in clinical practice. Some studies have assessed the possibility to complete a failed colonoscopy by switching to a different instrument, such as paediatric colonoscope [18], variable-stiffness colonoscope [19], small calibre overtube-assisted colonoscope [20], single or double balloon enteroscope [21], or a gastroscope [22, 23]. Different devices, such as cap or overtube, have been also reported to be useful in improving colonoscopy performance [24, 25]. However, it should be noted that some of these endoscopes are either not available in all endoscopic units or they are not skilfully handled by all operators. In addition, the endoscopic procedure by using these instruments may result complex and occasionally unsafe [26].
The attempt of reaching the caecum during the same session of failed colonoscopy should be routinely pursued for different reasons. A recent population-based study highlighted that only 29.4% of these patients had a 2subsequent caecal intubation with 1 year, leaving in many patients unexplored a part of the proximal colon with the risk of overlooked neoplastic or precancerous lesions [27]. Moreover, these patients are denied of psychological benefit coming from a low risk of cancer following a complete bowel examination [28]. Few data are available in literature regarding the possibility of completing a failed caecal intubation following a further examination by using a standard colonoscope [19, 29]. Generally, a repeated colonoscopy is performed by using intravenous administration of propofol, which allow to overcome pain. However, such an approach should be scheduled according to the presence of an anaesthetist, some safety concerns being pointed out regarding propofol administration by a gastroenterologist [30]. Moreover, the use of propofol does not ensure caecal intubation, a large study showing a 12.6% failure following such an approach [31].
The present study found that, following a standard sedation with midazolam and by using an adult colonoscope, it was possible to complete a prior failed colonoscopy in more than two third of cases, suggesting a role for different experience among different operators. Of note, that caecal intubation rate was significantly lower in those patients with a prior incomplete than complete colonoscopy, indicating that a previously failed colonoscopy is a negative predictive factor for reaching the caecum. We also observed that the probability of completing a failed colonoscopy with a standard colonoscope is significantly reduced when the previous examination was stopped in the sigmoid tract—mainly due to diverticular disease with a benign stricture—whilst the other factors such as age, sex, and previous abdominal surgery, which have been associated with failure of first colonoscopy [6, 9], did not significantly affect colonoscopy completeness at second attempt with the same instrument.
A gastroscope for colonoscopy is not rarely used in either paediatric or small size adult patients. The use of such endoscope has been also proposed in the event of colonoscopy failure by using a standard colonoscope [22, 23]. Our data found that, by using a standard gastroscope, caecal intubation was successful in further half patients in whom complete colonoscopy still failed by using an adult colonoscope. Moreover, we observed that the use of a gastroscope seems to be particularly advantageous in those patients with a failed colonoscopy due to diverticular disease in the sigmoid tract, with six of every ten colonoscopies being successful with such an instrument in these cases. This would appear a relevant finding, with the diverticular disease being an independent risk factor for perforation during standard colonoscopy [32]. The usefulness of switching to a gastroscope following a failed colonoscopy with standard colonoscope was highlighted in crossover study, where a 79% caecal intubation rate was achieved [22]. Therefore, following an endoscopic approach by using a standard colonoscope and a gastroscope—both instruments available in all endoscopic units and handled by all endoscopists—it was possible to complete a failed colonoscopy in more than 90% of the attempted cases during the same session. Interestingly, in the majority of cases of failed colonoscopy with both colonoscope and gastroscope, we stopped at the same colon level reached in the prior failed colonoscopy performed in another hospital. Such a finding suggests that a particular anatomic condition (diverticular disease with stricture, redundant looping, fixed angulation, postsurgical adhesions) do exist in a definite number of patients preventing a complete colonoscopy [15]. In such a few cases with a still incomplete endoscopy, the endoscopist should probably avoid to forcefully overcome the obstacle with other endoscopes, with no instrument being the best for any situation and for any endoscopist. Imaging techniques, such as virtual colonoscopy, should probably be considered the best procedure in these cases, in order to avoid a bowel perforation [23]. A further forced endoscopic approach is probably justified only in high-risk patients, such as hereditary cancer syndromes, long-lasting inflammatory bowel disease, or the documented presence of a proximal colon lesion.
In conclusion, our data found that it is possible to safely complete bowel examination in the majority of patients with a previously incomplete colonoscopy simply by using a standard colonoscope or gastroscope. A prior failed colonoscopy, particularly when stopped in the sigmoid tract, is significantly associated with a lower caecal intubation rate at second colonoscopy. It may be suggested that a standard colonoscope do exist, but not a standard colonoscopy (Fig. 1).
The flowchart of the study 1Patients did not exhibit the report of previous failed colonoscopy (19 cases), or the previous endoscopic report did not clearly indicate the colon tract reached (4 cases) 2computed tomography (CT) colonography were performed in the same day in the Radiological Section of our hospital. 3Patients contacted by phone declared no further endoscopic or radiological examinations. ITT intention to treat, PP per protocol
References
Rex DK, Bond JH, Winawer S, Winawer S, Levin TR, Burt RW, Johnson DA, Kirk LM, Litlin S, Lieberman DA, Waye JD, Church J, Marshall JB, Riddell RH (2002) Quality in the technical performance of colonoscopy and the continuous quality improvement process for colonoscopy: recommendations of the U.S. Multi-Society Task Force on colorectal cancer. Am J Gastroenterol 97:1296–1308
Imperiale TF, Wagner DR, Lin CY, Larkin GN, Rogge JD, Ransohoff DF (2000) Risk of advanced proximal neoplasms in asymptomatic adults according to the distal colorectal findings. N Engl J Med 343:169–174
Lieberman DA, Weiss DG, Bond JH, Ahnen DJ, Garewal H, Chejfec G (2000) Use of colonoscopy to screen asymptomatic adults for colorectal cancer. N Engl J Med 343:162–168
Regula J, Rupinski M, Kraszewska E, Polkowski M, Pachlewski J, Orlowska J, Nowacki MP, Butruk E (2006) Colonoscopy in colorectal-cancer screening for detection of advanced neoplasia. N Engl J Med 335:1863–1872
Aslinia F, Uradomo L, Steele A, Greenwald BD, Raufman JP (2006) Quality assessment of colonoscopy cecal intubation: an analysis of 6 years of continuous practice at a university hospital. Am J Gastroenterol 101:721–731
Anderson JC, Gonzalez JD, Messina CR, Pollack BJ (2000) Factors that predict incomplete colonoscopy: thinner is not always better. Am J Gastroenterol 95:2784–2787
Mitchell RM, McCallion K, Gardiner KR, Watson RG, Collins JS (2002) Successful colonoscopy: completion rates and reasons for incompletion. Ulster Med J 71:34–37
Bowles CJA, Leicester R, Romaya C, Swarbrick E, Williams CB, Epstein O (2004) A prospective study of colonoscopy practice in the UK today: are we adequately prepared for national colorectal cancer screening tomorrow? Gut 53:277–283
Shah HA, Paszat LF, Saskin R, Stukel TA, Rabeneck L (2007) Factors associated with incomplete colonoscopy: a population-based study. Gastroenterology 132:2297–2230
Wong TYY, Lam WWM, So NMC, Lee JFY, Leung KL (2007) Air-inflated magnetic resonance colonography in patients with incomplete conventional colonoscopy: comparison with intraoperative findings, pathology specimens, and follow-up. Am J Gastroenterol 102:56–63
Waye JD (2000) Completing colonoscopy. Am J Gastroenterol 95:2681–2682
Hansel SL, Prechel JA, Horn B, Crowell MD, DiBaise JK (2009) Observational study of the frequency of use and perceived usefulness of ancillary manoeuvres to facilitate colonoscopy completion. Dig Liver Dis 41:812–816
Morini S, Hassan C, Zullo A, Lorenzetti R, de Matthaeis M, Stella F, Campo SMA (2009) Detection of colonic polyps according to insertion/withdrawal phases of colonoscopy. Int J Colorectal Dis 24:527–530
Radaelli F, Meucci G, Minoli G (2008) Colonoscopy practice in Italy: a prospective survey on behalf of the Italian Association of Hospital Gastroenterologists. Dig Liver Dis 40:897–904
Hanson ME, Pickhardt PJ, Kim DH, Pfau PR (2007) Anatomic factors predictive of incomplete colonoscopy based on findings at CT colonography. AJR 189:774–779
Sanaka MR, Shah N, Mullen KD, Ferguson DR, Thomas C, McCullough AJ (2006) Afternoon colonoscopies have higher failure rates than morning colonoscopies. Am J Gastroenterol 101:2726–2730
Morrin MM, Kruskal JB, Farrell RJ, Goldberg SN, McGee JB, Raptopoulos V (1999) Endoluminal CT colonography after an incomplete endoscopic colonoscopy. AJR 172:913–918
Marshall JB (1996) Use of a pediatric colonoscope improves the success of total colonoscopy in selected adult patients. Gastrointest Endosc 44:675–678
Shumaker DA, Zaman A, Katon RM (2001) Use of a variable-stiffness colonoscope allows completion of colonoscopy alter failure with the standard adult colonoscope. Endoscopy 34:711–714
Friedland S, Soetikno R (2007) Small caliber overtube-assisted colonoscopy. World J Gastroenterol 13:5933–5937
Pasha SF, Harrison ME, Das A, Corrado CM, Arnell KN, Leighton JA (2007) Utility of double-balloon colonoscopy for completion of colon examination after incomplete colonoscopy with conventional colonoscope. Gastrointest Endosc 65:848–853
Wehrmann T, Lechowicz I, Martchenko K, Riphaus A (2008) Routine colonoscopy with a standard gastroscope. A randomized comparative trial in a western population. Int J Colorectal Dis 23:443–446
Paonessa NG, Rosen L, Stasik JJ (2005) Using the gastroscope for incomplete colonoscopy. Dis Colon Rectum 48:851–854
Shida T, Takano S, Kaiho M, Miyazaki M (2008) Transparent hood attached to a gastroscope: a simple rescue technique for patients with difficult or incomplete colonoscopy. Endoscopy 40(suppl 2):e139
Hawari R, Pasricha PJ (2007) Going for the loop: a unique overtube for the difficult colonoscopy. J Clin Gastroenterol 41:138–140
Rodriguez SA, Ormeseth E, Tsuchida A (2003) Bowel perforation with variable stiffness colonoscope. Gastrointest Endosc 57:271–273
Rizek R, Paszat LF, Stukel TA, Saskin R, Li C, Rabeneck L (2009) Rates of complete colonic evaluation after incomplete colonoscopy and their associated factors: a population-based study. Med Care 47:48–52
Singh H, Turner D, Xue L, Targownik LE, Bernstein CN (2006) Risk of developing colorectal cancer following a negative colonoscopy examination: evidence for a 10-year interval between colonoscopies. JAMA 295:2366–2373
Cirocco WC, Rusin LC (1995) Factors that predict incomplete colonoscopy. Dis Colon Rectum 38:964–968
Bell GD, Quine A (2006) Preparation, premedication, and surveillance. Endoscopy 38:105–109
Radaelli F, Meucci G, Sgroi G, Minoli G (2008) Technical performance of colonoscopy: the key role of sedation/analgesia and other quality indicators. Am J Gastroenterol 103:1122–1130
Panteris V, Haringsma J, Kuipers EJ (2009) Colonoscopy perforation rate, mechanisms and outcome: from diagnostic to therapeutic colonoscopy. Endoscopy 41:941–951
Conflict of interest statement
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Morini, S., Zullo, A., Hassan, C. et al. Endoscopic management of failed colonoscopy in clinical practice: to change endoscopist, instrument, or both?. Int J Colorectal Dis 26, 103–108 (2011). https://doi.org/10.1007/s00384-010-1016-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-010-1016-4