Abstract
Background and aims
For rectal carcinoma treated according to the concept of total mesorectal excision (TME surgery), the independent influence of regional lymph node metastasis on the locoregional recurrence risk is still in discussion. A reliable assessment of this risk is important for an individualised selective indication for neoadjuvant radio-/radiochemotherapy.
Methods
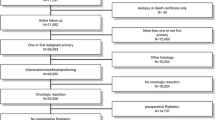
Analysis of literature, especially of the last 20 years, and consideration of pathological and oncological basic research. Multivariate analysis of data of the Erlangen Registry of Colorectal Carcinoma.
Results
The clinical assessment of the pretherapeutic regional lymph node status by the present available imaging methods is still unreliable. The analysis of the association between pretherapeutic regional lymph node status and locoregional recurrence risk has to be based on follow-up data of patients treated by primary surgery and has to be distinguished between patients treated by conventional and optimised quality-assured TME surgery, respectively. Data from Erlangen show an increase of the local recurrence risk for patients with at least four involved regional lymph nodes.
Conclusions
For patients with at least four involved regional lymph nodes, a neoadjuvant radiochemotherapy may be indicated. However, today, the pretherapeutic diagnosis is uncertain and results in overtherapy in 40%. Thus, in case of positive lymph node findings by imaging methods, the benefits and risk of neoadjuvant therapy in such situations should always be discussed with the patient in the sense of informed consent and shared decision.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
There is no discussion that for patients with rectal carcinoma, regional lymph node metastases (RLNM) are indicators of an increased risk of distant metastases. In contrast, the independent influence of RLNM on locoregional recurrence (LR) is still in discussion. In this context, it has to be differentiated according to type and quality of surgery (conventional or total mesorectal excision (TME) surgery), and the use of multimodal therapy has to be considered. In the following, ‘TME surgery’ is used for following the concept of total mesorectal excision for carcinomas of the middle and lower third and of partial mesorectal excision (PME) for carcinomas of the upper third, in each case with sharp dissection in the pelvis [1–3].
The subject of the association between the pretherapeutic regional lymph node status and the risk of LR directly influences the selection of patients for neoadjuvant treatment. Thus, this topic has practical clinical relevance, especially in the present time of general demand for a more selective and individualised indication for neoadjuvant treatment, preventing under- as well as overtreatment [4–10]. In the following, the actual data of literature including new data from the Erlangen Registry of Colorectal Carcinoma (ERCRC) [11] will be analysed.
Preliminary remarks and definitions
In the description of the pretherapeutic regional lymph node status according to the rules of the TNM classification [12], it is distinguished between a clinical and a pathological classification (cN/pN). The clinical assessment of the pretherapeutic lymph node status is associated with uncertainty. The real situation is described by the results of the histopathological examination of the resection specimens, however, only in case of primary surgery. Following neoadjuvant treatment, the pathological examination of the regional lymph nodes describes the situation following neoadjuvant treatment (ypN); thus, in case of neoadjuvant treatment, the pretherapeutic lymph node status can be assessed only clinically (cN), but not pathologically.
Between Western Countries and Japan, there are differences in the anatomic subdivision of the rectum. In Japan, ‘lower rectum’ includes all tumours below the peritoneal reflection, corresponding to tumours of the middle and low third of the rectum, about <11–12 cm from the anal margin. In the Western countries, ‘lower or low rectum’ is used only for tumours of the lower third of the rectum (lower margin <6–7.5 cm from the anal margin).
Whether for analysis of the association between the pretherapeutic regional lymph node status and the risk of LR only patients with primary surgery or also patients with neoadjuvant treatment can be included depends on the reliability of the clinical diagnosis of RLNM. Thus, in the following, at first, the accuracy of the present imaging methods concerning regional lymph nodes will be discussed.
In the lymphatic spread of the rectal carcinoma, it has to be further distinguished between the predominant spread within the mesorectum upwards and the spread to lateral pelvic nodes. The latter will be discussed in a separate section.
Possibilities of clinical assessment of pretherapeutic regional lymph node status
With regard to the possibilities of pretherapeutic diagnosis of RLNM, it has to be distinguished between the lymph nodes in the mesorectum and the lateral pelvic lymph nodes.
The present clinical assessment of mesorectal lymph nodes is associated with considerable uncertainty [5, 8, 13, 14]. According to two meta-analyses [13, 15] and three systematic literature reviews [16–18], no significant differences between EUS, CT, and MRI with respect to staging the nodal status have been found (Table 1). However, in these reviews, exact information about the proportion of patients with neoadjuvant treatment and about the use of endorectal coil for MRI are partly missing.
High-resolution MRI employing pelvic phase-array coils is the best modality to evaluate the relation between tumour and fascia mesorectalis (the later plane of surgery and circumferential resection margin). Thus, today, MRI can be considered as the established modality of choice for pre-operative staging and selection for neoadjuvant treatment [5, 8, 19, 20]. Near details of present day efficiency of MRI in the assessment of the pretherapeutic mesorectal lymph node status can be seen in Table 2. The pooled results are disappointing: positive predictive value only 63%, accuracy only 71%. A similar value for accuracy (380/502 = 76%) is reported from the National Cancer Center Hospital, Tokyo [21]. In this retrospective study (1988–2002, 817 patients) the lymph node status has been assessed by ‘CT and/or MRI’ and included for patients at or below the peritoneal reflection the lateral pelvic lymph nodes.
Summarising, it has to be stated that a reliable assessment of the pretherapeutic mesorectal regional lymph node status is not possible by the present imaging modalities [13, 14, 22].
An improvement in lymph node staging by the contrast agent ultrasmall super paramagnetic iron oxide-enhanced MRI was expected in future [8, 22–24]. However, this contrast medium is no more available at present. The results of the multi-slice (multi-detector row) CT (MDCT) seem to be similar to MRI [25–28]; however, the available data are limited.
The diagnosis of four or more involved mesorectal lymph nodes (cN2) is a further problem. Table 3 shows the results of four relevant studies (2000–2006, n = 362). The pooled positive predictive value is only 60%. Forty percent of the positive findings are false, i.e., the results are near to purely coincidental values. Thus, the pretherapeutic MRI findings of cN2 cannot be considered as basis of an indication for neoadjuvant therapy.
The possibilities of clinical assessment of lateral pelvic lymph nodes could be studied only in Japan where patients with T3 and T4 rectal carcinomas below the peritoneal reflection (designated as lower rectal carcinoma according to the Japanese Society for Cancer of the Colon and Rectum, 1997) [29] have been treated by primary TME surgery with extended lateral pelvic lymphadenectomy (D3 lymphadenectomy) [3]. In a comparison between mesorectal and lateral pelvic lymph nodes [30], the results of MRI proved to be better for lateral than for mesorectal nodes: positive predictive value 56% (10/18) versus 46% (12/26), negative predictive value 91% (10/11) versus 81% (22/27), false positive findings 15% (8/53) versus 26% (14/53) and overall accuracy 83% (44/53) versus 64% (34/53). Only the last difference is statistically significant (p = 0.046).
In this context, it has to be emphasised that an involvement of lateral pelvic lymph nodes is in most cases associated with positive mesorectal lymph nodes: Sugihara et al. [31]: 103/129 (80%) and Ueno et al. [32]: 31/41 (76%).
Regional lymph node metastasis and the risk of locoregional recurrence
The following deals with the problem whether absence or presence of regional lymph node metastasis (N0 or N1,2) has an independent influence on the risk of LR (the impact of the number of involved lymph nodes is discussed in the following section). In this respect, it is essential to distinguish between conventional and optimised and quality-assured TME surgery.
As shown above, the pretherapeutic clinical assessment of the regional lymph node status is uncertain. Thus, a reliable analysis of the association between pretherapeutic regional lymph node status and the risk of LR is possible only by using the histopathological assessment of the pretherapeutic regional lymph node status, i.e., the pN status after primary surgery (without neoadjuvant treatment) describing the pretherapeutic situation.
Following conventional surgery, the different frequency of LR for pN0 and pN1,2 patients is proven for a long time already [33–39].
For the actual optimised TME surgery, a correlation between pN and LR seems unlikely for theoretical reasons. The TME surgery is characterised by the complete removal of the lymphatic drainage upwards as a package limited by fascias, thus, regional lymph nodes—except, lateral pelvic nodes (see below)—do not remain as origin of LR.
For patients treated by primary surgery following the concept of TME, two publications include relevant multivariate analyses dealing with the influence of pN0 and pN1,2, respectively, on the risk of LR. In both studies, the LR rates for pN0 and pN1,2 were not different. In the largest study [40] (n = 686), the crude LR rate for all patients was 7%, the hazard ratios compared to pN0 = 1.0 were for pN1 1.5 (95% CI, 0.8–3.1) and for pN2 1.4 (95% CI, 0.6–3.4; p = 0.49). In the study of Ross et al. [41] (212 patients after exclusion of 17 patients with distant metastasis, in 11 patients = 5.2% neoadjuvant radiotherapy), the crude LR rates were 16/112 = 14% for pN0 and 10/100 = 10% for pN2 (p = 0.41).
Other multivariate analyses of the association between pN status and LR in patients treated by primary TME surgery refer to selected subgroups, e.g., stage II patients treated by anterior resection alone [42] or pT1 and 2 patients only [43] or patients treated by intersphincteric resection only [44] and are, for the general question of the indication for neoadjuvant treatment, not relevant. The same applies to the study of Eriksen et al. [45] because the multivariate analysis includes only 1,676 (67.6%) of 2,480 pT3 patients, namely, those with known circumferential resection margin (CRM) status; thus, the results cannot be considered as representative for all pT3 patients. The multivariate study of Bufalari et al. [46] cannot be considered relevant because of the very limited number of patients (n = 73).
Recently Fujita et al. [21] reported the treatment results for 817 patients with rectosigmoid, rectal and anal carcinomas, clinical stage II and III. A multivariate analysis performed for pretherapeutic clinical factors only showed the pretherapeutic clinical assessment of regional lymph nodes (including lateral pelvic nodes in rectal carcinomas at and below the peritoneal reflection; cN+) as statistically significant factor affecting LR. This study is questionable because of insufficient technique in carrying out the residual tumour (R) classification (only one block histologically examined), missing data on the circumferential resection margin (CRM) status, missing differentiation between rectosigmoid, rectal and anal canal carcinomas in the multivariate analysis and the limitation of the multivariate analysis to clinical factors only. Thus, for the problem under discussion this study cannot be considered.
Summarising, it can be stated that there are no reliable data indicating that in patients treated by optimised TME surgery, any involvement of regional lymph is associated with an increased LR rate and requires neoadjuvant or adjuvant radiotherapy.
It has to be pointed out that following neoadjuvant treatment patients with RLNM (ypN+) represent a negative selection of the pretherapeutically lymph node positive patients, namely no (or not sufficiently) responding patients. For these patients, the proportion of pretherapeutically lymph node positive patients (cN+) remains unknown because the clinical assessment of lymph node metastasis is not sufficiently reliable (see previous discussion). The statistically significant correlation between ypN and LR after neoadjuvant radiochemotherapy (Rödel et al. [47]; n = 344) and neoadjuvant long-course radiotherapy (Larsen et al. [48]; n = 204), respectively, is not relevant for the question of indications for neoadjuvant treatment because from this correlation cannot be concluded to an association between the pretherapeutic lymph node status and the LR rate.
Number of involved regional lymph nodes and the risk of locoregional recurrence
A different prognosis, depending on the number of involved regional lymph nodes (1–3 versus ≥4), has already been described in the mid of the last century [49, 50] and was the reason for the subdivision of lymph node positive patients in the Dukes’ stages C1 and C2 and the (p)N1 and (p)N2 categories of the TNM classification. Moran et al. [51] confirmed the higher LR rates in cases of pN2 with data on conventional surgery without neoadjuvant treatment.
In the registry of the Norwegian Rectal Cancer Project [40], the risk of LR in patients treated by primary TME surgery was for pN1 and pN2 nearly identical (see previous discussion). In contrast, in the multivariate analysis of Ross et al. [41], a significant increase of the LR rate depending on the number of involved regional lymph nodes has been reported. However, further details, especially with regard to the cut-off value, are missing.
In a univariate analysis, Cecil et al. [52] demonstrated that following (low) anterior resection according to the principles of TME surgery and ‘only minimal’ use of neoadjuvant radiotherapy, the crude LR in patients with more than eight involved regional lymph nodes increases significantly in comparison with patients with no lymph node metastasis and 1–8 involved nodes: 3/13(23%) versus 13/457(2.8%; p = 0.008).
Because of these inconsistent data, the relationship between number of involved regional lymph nodes and the risk of locoregional recurrence was analysed on the basis of the data of the ERCRC from a time period with use of primary TME surgery (without neoadjuvant therapy) in the vast majority of patients, i.e., January 1, 1986 to January 31, 1995. Inclusion criteria, patients’ characteristics, LR rates and the results of uni- and multivariate analysis of risk factors for LR are presented in Table 4. While there is no statistically significant difference between pN0 and pN1, there are highly significant differences (p < 0.001) between pN1 and pN2 in the multivariate analysis too. Correspondingly, in view of locoregional recurrence risks, a subdivision between pN0,1 and pN2 is preferable because this subdivision results in the highest difference of the locoregional recurrence rates: 10.3% versus 33.5% (p < 0.001).
From the data presented in Table 4, one may conclude that in case of extensive lymph node metastasis (involvement of four or more lymph nodes, N2) the risk of locoregional recurrence is about 30% and thus, a neoadjuvant radio-/radiochemotherapy is indicated. However, it has to be taken into consideration that in such patients, the prognosis is determined in the first place by the high risk of distant metastasis. Moreover, there is the problem of pretherapeutic diagnosis of N2 by imaging. As shown in Table 3, the positive predictive value is at present only 60%. Thus, the pretherapeutic clinical finding cN2 cannot be considered as certain basis for an indication for neoadjuvant radiotherapy. However, in this situation, the patient is to be included in the decision (see further discussion).
Problems of lateral pelvic lymph nodes
The predominant and typical lymphatic drainage of the rectum is directed upwards in the mesorectum to the nodes along the superior rectal and inferior mesenteric arteries. In addition, there is a lateral lymphatic drainage to the lateral lymph node compartment. The latter has been studied predominantly in Japan where an extended lateral pelvic lymph node dissection (pelvic side wall dissection, D3 dissection) has been performed routinely for years. According to the JSCCR [29] the lateral nodes include: (1) middle rectal root nodes (lateral to the pelvic nerve plexus); (2) internal iliac nodes; (3) obturator nodes; (4) median and lateral sacral nodes; (5) external iliac nodes; (6) common iliac nodes and (7) aortic bifurcation nodes. According to the TNM classification [12], involvement of the stations 1–4 is classified as regional lymph node metastasis, of stations 5–7 as distant metastasis.
In the Japanese literature 1998–2008, the frequency of lateral lymph node metastasis in rectal carcinoma is reported as about 10% (Mori et al. [53]: 40/906 = 4.4%; Takahashi et al. [54]: 57/632 = 9.0%; Koda et al. [55]: 35/265 = 13.2% and Sugihara et al. [31]: 129/930 = 13.8%, pooled value 261/2733 = 9.5%, 95% CI 8.4–10.7%). Not included in these figures are cases with immunohistochemical findings of tumour cells only [56–58] because the prognostic relevance of such findings is not proven.
The most important risk factors for lateral node metastases are the tumour site (tumours below the peritoneal reflection, especially tumours with a distal margin ≤4 cm [59] or ≤6.5 cm from anal margin [54] and involvement of mesorectal nodes [31, 54, 60]. Other factors are direct involvement of the circumferential resection margin by tumour [58, 61], G3,4 [59], cT3,4/pT2-4, tumour diameter ≥4 cm and female gender [31].
For rectal carcinomas ≤8 cm from the anal margin, a score for the estimation of the risk of lateral lymph node metastasis has been published by Ueno et al. [59]. Three risk factors are considered: distal margin of tumour 4 cm or less from the anal margin, histological type other than adenocarcinoma G1 or 2 and involvement of mesorectal lymph nodes. The frequencies of lateral lymph node metastasis are 3% (1/34) for zero, 8% (10/120) for one, 33% (24/73) for two and 60% (6/10) for three risk factors, respectively.
In patients with cT3,4 carcinomas below the peritoneal reflection, since many years in Japan, an extended lateral pelvic lymph node dissection has been performed; since the early 1990s, with pelvic autonomic nerve preservation [53, 62–66].
This Japanese strategy found no acceptance in western countries because
-
in comparison with TME surgery, the benefit of additional extended lateral pelvic lymph node dissection for survival could not be proven;
-
increased long-term urinary and sexual dysfunction;
-
longer operation time and
Today, in Europe, for low cT3,4 carcinomas neoadjuvant radio-/radiochemotherapy generally is used [9, 72–77]. This is increasingly accepted as an alternative to extended lateral pelvic node dissection in Japan too [21, 55, 59, 78–80].
Implications for the indication to neoadjuvant therapy
For a long time, regional lymph node metastases have been considered as independent factor not only for distant metastases, but also for LR. This has changed in the era of TME surgery. Today, in case of careful and quality-assured TME for middle and lower rectal carcinoma and PME for upper rectal carcinoma, an increased risk for LR cannot be assumed for each patient with regional lymph node metastasis.
Frequently, all patients with clinically positive regional lymph nodes are treated with neoadjuvant radio-/radiochemotherapy as proposed by many actual guidelines. In the USA, it has been recommended to treat T1,2 tumours with clinically diagnosed regional lymph node metastasis by primary surgery [81]. This has been accepted in the last actualisation of the German guidelines [76] too.
Today, increasingly, the indication for neoadjuvant treatment is based on MRI. In this case, the regional lymph node status is usually not considered [45, 72, 75, 77, 82–84].
Recent data, limited so far (Table 4), show that involvement of four or more regional lymph nodes (N2) is an independent risk factor for LR in TME surgery too. Thus, an indication for neoadjuvant radiotherapy may be concluded. This is in agreement with the assessment of N2 as a poor prognostic factor and the use of neoadjuvant chemoradiation for such patients [8, 23, 73, 74, 85]. Future clinical trials should be based on a more differentiated indication of neoadjuvant treatment in stage III diseases with detailed documentation of lymph node findings in the imaging diagnosis.
However, there is the problem that with today’s available imaging methods, the involvement of four or more regional lymph nodes can preoperatively be diagnosed only with 60% certainty (Table 3). In this case, neoadjuvant radiotherapy is in 40% overtreatment associated with considerable late adverse effects. Thus, this situation is a typical example for the requirement to discuss risks and benefits with the patient [86, 87]. A differentiated shared discussion in the sense of an informed consent should take place in any such case.
References
Head RJ, Husband EM, Ryall RD (1982) The mesorectum in rectal cancer surgery—the clue to pelvic recurrence? Br J Surg 69:613–616
Büchler MW, Heald RJ, Maurer CA, Ulrich B (eds) (1998) Rektumkarzinom: Das Konzept der Totalen Mesorektalen Exzision. Karger, Basel
Havenga K, Enker WE, Norstein J et al (1999) Improved survival and local control after total mesorectal or D3 lymphadenectomy in the treatment of primary rectal cancer: an international analysis of 1411 patients. Eur J Surg Oncol 25:368–374
Frileux P, Burdy, Aegerter P et al (2007) Surgical treatment of rectal cancer: results of a strategy for selective preoperative radiotherapy. Gastroenterol Clin Biol 31:934–940
Mortensen MM, Khatri VP, Bennett JJ, Petrelli NJ (2007) Total mesorectal excision and pelvic node dissection for rectal cancer: an appraisal. Surg Oncol Clin N Am 16:177–197
Wieder HA, Rosenberg R, Lordick F et al (2007) Rectal cancer: MR imaging before neoadjuvant chemoradiotherapy for prediction of tumor-free circumferential resection margins and long-term survival. Radiology 243:744–751
Moser L, Ritz J-P, Hinkelbein W, Höcht S (2008) Adjuvant and neoadjuvant chemoradiation or radiotherapy in rectal cancer—a review focusing on open questions. Int J Colorect Dis 23:227–236
Smith N, Brown G (2008) Preoperative staging of rectal cancer. Acta Oncol 47:20–31
Hermanek P, Hohenberger W, Fietkau R, Rödel C (2009) Individualized MRI-based neoadjuvant chemoradiation for middle and lower rectal cancer. Colorectal Disease. doi:10.1111/j.1463-1318.2009.02076.x
Ulrich A, Weitz J, Büchler MW (2009) Strahlentherapie bei Rektumkarzinom: wird zu viel bestrahlt? Chirurg 80:266–273
Merkel S, Meyer T, Göhl J, Hohenberger W (2002) Late locoregional recurrence in rectal carcinoma. Eur J Surg Oncol 28:716–722
UICC (2002) In: Sobin LH, Wittekind Ch (eds) TNM classification of malignant tumours, 6th edn. Wiley, New York
Lahaye MJ, Engelen SME, Nelemans PJ et al (2005) Imaging for predicting the risk factors—the circumferential resection margin and nodal disease—of local recurrence in rectal cancer: a meta-analysis. Ultrasound CT MRI 26:259–268
Engelen SME, Beets GL, Beets-Tan RGH (2007) Role of preoperative local and distant staging in rectal cancer. Onkologie 30:141–145
Bipat S, Glas AS, Slors FJM et al (2004) Rectal cancer: local staging and assessment of lymph node involvement with endoluminal US, CT, and MR imaging – A meta-analysis. Radiology 232:773–783
Heriot AG, Grundy, Kumar D (1999) Preoperative staging of rectal carcinoma. Br J Surg 86:17–25
Kwok H, Bissett IP, Hill GL (2000) Preoperative staging of rectal cancer. Int J Colorectal Dis 15:9–20
Skandarajah AR, Tjandra JT (2006) Preoperative locoregional imaging in rectal cancer. ANZ J Surg 76:497–504
O’Neil BDP, Brown G, Heald RJ et al (2007) Non-operative treatment after neoadjuvant chemoradiotherapy for rectal cancer. Lancet Oncol 8:625–633
Klessen C, Rogalla P, Taupitz M (2007) Local staging of rectal cancer: the current role of MRI. Eur Radiol 17:379–389
Fujita S, Yamamoto S, Akasu T, Moriya Y (2008) Outcome of patients with clinical stage II or III rectal cancer treated without adjuvant radiotherapy. Int J Colorect Dis 23:1073–1079
Beets-Tan R, Beets GL (2008) MRI and lymph node staging in rectal cancer. Abstract. Eur J Surg Oncol 34:1002
Engelen S, Lahaye MJ, Beets-Tan RG et al (2008) Tailored treatment of primary rectal cancer based on MRI: does it reduce the number of incomplete resections? Abstract. Ann Oncol 19(Suppl):i17
Lahaye MJ, Engelen SME, Kessels AGH et al (2008) USPIO-enhanced MR imaging for nodal staging in patients with primary rectal cancer: predictive criteria. Radiology 246:804–811
Kim CK, Kim SH, Choi D (2007) Comparison between 3-T magnetic resonance imaging and multi-detector row computed tomography for the preoperative evaluation of rectal cancer. J Comput Assist Tomogr 31:853–859
Kulinna C, Scheidler J, Strauss T et al (2004) Local staging of rectal cancer: assessment with double-contrast multislice computed tomography and transrectal ultrasound. J Comput Assist Tomogr 28:123–130
Sinha R, Verma R, Rajesh A, Richards CJ (2006) Diagnostic value of multidetector row CT in rectal cancer staging: comparison of multiplanar and axial images with histopathology. Clin Radiol 61:924–931
Taylor A, Slater A, Mapstone N et al (2007) Staging rectal cancer: MRI compared to MDCT. Abdom Imaging 32:323–327
Japanese Society for Cancer of the Colon and Rectum (1997) Japanese classification of colorectal carcinoma (Response assessment of nonsurgical treatment for colorectal carcinoma), 1st Engl edn. Kanehara & Co Ltd, Tokyo, pp 4–5
Arii K, Takifuji K, Yokoyama S et al (2006) Preoperative evaluation of pelvic lateral lymph nodes of patients with lower rectal cancer: comparison study of MR imaging and CT in 53 patients. Langenbecks Arch Surg 391:449–454
Sugihara K, Kobayashi H, Kato T et al (2006) Indication and benefit of pelvic sidewall dissection for rectal cancer. Dis Colon Rectum 49:1663–1672
Ueno H, Mochizuki H, Hashiguchi Y et al (2007) Potential benefit of lateral pelvic node dissection for rectal cancer located below the peritoneal reflection. Ann Surg 245:80–87
Morson BC, Vaughan EG, Bussey JHR (1963) Pelvic recurrence after excision of rectum for carcinoma. Brit Med J ii:13–18
Phillips RKS, Hittinger R, Bleskovsky L et al (1984) Local recurrence following ‘curative’ surgery for large bowel cancer. II. The rectum and sigmoid. Br J Surg 71:17–20
Jass JR, Atkin WS, Cuzick J et al (1986) The grading of rectal cancer: historical perspectives and a multivariate analysis of 447 cases. Histopathology 10:437–459
Rinnert-Gongora S, Tartter PI (1989) Multivariate analysis of recurrence after anterior resection for colorectal carcinoma. Am J Surg 157:573–576
Zirngibl H, Husemann B, Hermanek P (1990) Intraoperative spillage of tumor cells in surgery for rectal cancer. Dis Colon Rectum 33:610–614
McCall JL, Cox MR, Wattchow DA (1995) Analysis of local recurrence rates after surgery alone for rectal cancer. Int J Colorect Dis 10:126–132
Park YJ, Park KJ, Park J-G et al (1999) Prognostic factors in 2230 Korean colorectal cancer patients: analysis of consecutively operated cases. World J Surg 23:721–729
Wibe A, Rendedal PR, Svensson E et al (2002) Prognostic significance of the circumferential resection margin following total mesorectal excision for rectal cancer. Br J Surg 89:327–334
Ross A, Rusnak C, Weinerman B et al (1999) Recurrence and survival after surgical management of rectal cancer. Am J Surg 177:392–395
Law WL, Ho JWC, Chan R et al (2005) Outcome of anterior resection for stage II rectal cancer without radiation: role of adjuvant chemotherapy. Dis Colon Rectum 48:218–226
Chok KSH, Law WL (2007) Prognostic factors affecting survival and recurrences of patients with pT1 and pT2 colorectal cancer. World J Surg 31:1485–1490
Akasu T, Takawa M, Yamamoto S et al (2008) Intersphincteric resection for very low rectal adenocarcinoma. Univariate and multivariate analyses of risk factors for recurrence. Ann Surg Oncol 15:2668–2676
Eriksen MT, Wibe A, Haffner J, Wiig JN, on behalf of the Norwegian Rectal Cancer Group (2007) Prognostic groups in 1676 patients with T3 rectal cancer treated without preoperative radiotherapy. Dis Colon Rectum 50:156–167
Bufalari A, Roselli C, Giustozzi G, Moggi L (2000) Locally advanced rectal cancer: a multivariate analysis of outcome risk factors. J Surg Oncol 74:2–10
Rödel C, Martus P, Papadopoulos T et al (2005) Prognostic significance of tumor regression after preoperative chemoradiotherapy for rectal cancer. J Clin Oncol 23:8688–8696, correspondence 24(2006):1319
Larsen SG, Wiig JN, Dueland S, Giercksky K-E (2008) Prognostic factors after preoperative irradiation and surgery for locally advanced rectal cancer. Eur J Surg Oncol 34:410–417
Astler CB, Coller FA (1954) The prognostic significance of direct extension of carcinoma of the colon and rectum. Ann Surg 139:846–852
Dukes CE, Bussey HJR (1958) The spread of rectal cancer and its effect on prognosis. Br J Cancer 12:309–320
Moran MR, James EC, Rothenberger DA, Goldberg SM (1992) Prognostic value of positive nodes in rectal cancer. Dis Colon Rectum 35:579–581
Cecil TD, Sexton R, Moran BJ, Heald RJ (2004) Total mesorectal excision results in low local recurrence rates in lymph node-positive rectal cancer. Dis Colon Rectum 47:1145–1150
Mori T, Takahashi T, Yasuno M (1998) Radical resection with autonomic nerve preservation and lymph node dissection techniques in lower rectal cancer surgery and its results: the impact of lateral lymph node dissection. Langenbeck’s Arch Surg 383:409–415
Takahashi T, Ueno M, Azekura K, Ohta H (2000) Lateral node dissection and total mesorectal excision for rectal cancer. Dis Colon Rectum 43:859–868
Koda K, Saito N, Oda K et al (2004) Evaluation of lateral lymph node dissection with preoperative chemo-radiotherapy for the treatment of advanced middle to lower rectal cancers. Int J Colorect Dis 19:188–194
Shimoyama M, Yamazaki T, Suda T, Hatakeyama K (2003) Prognostic significance of lateral lymph node micrometastases in lower rectal cancer. An immunohistochemical study with CAM5.2. Dis Colon Rectum 46:333–339
Hara M, Tirai T, Nakanishi H et al (2007) Isolated tumor cell in lateral lymph node has no influence on the prognosis of rectal cancer patients. Int J Colorect Dis 22:911–917
Wang Cc, Zhou Z-G, Yu Y-Y et al (2007) Patterns of lateral pelvic lymph node metastases and micrometastases for patients with lower rectal cancer. Eur J Surg Oncol 33:463–467
Ueno M, Oya M, Azekura K et al (2005) Incidence and prognostic significance of lateral lymph node metastasis in patients with advanced low rectal cancer. Br J Surg 92:756–763
Shiozawa M, Akaike M, Yamada R et al (2007) Lateral lymph node dissection for lower rectal cancer. Hepato-Gastroenterol 54:1066–1070
Ueno H, Mochizuki H, Hashiguchi Y, Hase K (2001) Prognostic determinants of patients with lateral nodal involvement by rectal cancer. Ann Surg 234:190–197
Hojo K, Sawada T, Moriya Y (1989) An analysis of survival and voiding, sexual function after wide iliopelvic lymphadenectomy in patients with carcinoma of the rectum, compared with conventional lymphadenectomy. Dis Colon Rectum 32:128–133
Hojo K, Vernava AM, Sugihara K, Katumata K (1991) Preservation of urine voiding and sexual function after rectal cancer surgery. Dis Colon Rectum 34:532–539
Enker WE (1992) Potency, cure, and local control in the operative treatment of rectal cancer. Arch Surg 127:1396–1402
Moriya Y, Sugihara K, Akasu T, Fujita S (1995) Patterns of recurrence after nerve-sparing surgery for rectal adenocarcinoma (with special reference to loco-regional recurrence). Dis Colon Rectum 38:1162–1168
Sugihara K, Moriya Y, Akasu T, Fujita S (1996) Pelvic autonomic nerve preservation for patients with rectal carcinoma. Oncologic and functional outcome. Cancer 78:1871–1880
Harnsberger JR, Vernava AM III, Longo WE (1994) Radical abdominopelvic lymphadenectomy: historic perspective and current role in the surgical treatment of rectal cancer. Dis Colon Rectum 37:73–87
MacFarlane JK (1997) Lateral node dissection—a critique. In: Soreide O, Norstein J (eds) Rectal cancer surgery. Optimisation–standardisation–documentation. Springer, Berlin Heidelberg New York, pp 255–263
Nelson H, Petrelli N, Carlin A et al (2001) Guidelines 2000 for colon and rectal surgery. J Natl Cancer Inst 93:583–596
Bruch H-P, Schwandner O (2002) Die totale mesorektale Exzision beim Rektumkarzinom—das Dissektionsprinzip ohne kontrollierte Daten. Viszeralchirurgie 37:6–11
Koch M, Kienle P, Antolovic D et al (2005) Is the lateral lymph node compartment relevant? Recent Results Cancer Res 165:40–45
Crawshaw A, Hennigan R, Smedley FH, Leslie MD (2003) Perioperative radiotherapy for rectal cancer: the case for a selective pre-operative approach-the third way. Colorectal Disease 5:367–372
Burton S, Brown G, Daniels I et al (2006) MRI directed multidisciplinary team preoperative treatment strategy: the way to eliminate positive circumferential margins? Brit J Cancer 94:351–357
Chau I, Brown G, Cunningham D et al (2006) Neoadjuvant capecitabine and oxaliplatin followed by synchronous chemoradiation and total mesorectal excision in magnetic-resonance imaging-defined poor risk rectal cancer. J Clin Oncol 24:668–674, discussion 4664–4666
Junginger Th, Hermanek P, Oberholzer K, Schmidberger H (2006) Rektumkarzinom: Behandeln wir zu häufig neoadjuvant? Vorschläge zu einer selektiveren, MRT-basierten Indikation. Zentralbl Chir 131:275–284
Schmiegel W, Reinacher-Schick A, Arnold D et al (2008) S3-Leitlinie “Kolorektales Karzinom”—Aktualisierung 2008. Ergebnis einer evidenzbasierten Konsensuskonferenz (8–9.Juni 2007). Z Gastroenterol 46:799–840
Strassburg J, Junginger T, Trinh T et al (2008) Magnetic resonance imaging (MRI)-based indication for neoadjuvant treatment of rectal carcinoma and the surrogate endpoint CRM status. Int J Colorect Dis 23:1099–1107
Nagawa H, Muto T, Sunouchi K et al (2001) Randomized controlled trial of lateral node dissection vs nerve-preserving resection in patients with rectal cancer after preoperative radiotherapy. Dis Colon Rectum 44:1274–1280
Watanabe T, Tsurita G, Muto T et al (2002) Extended lymphadenectomy and preoperative radiotherapy for lower rectal cancers. Surgery 132:27–33
Kusunoki M, Inoue Y (2007) Current surgical management of rectal cancer. Dig Surg 24:115–119
Libuti SK, Tepper JE, Saltz LB, Rustgi AK (2005) Cancer of the rectum. In: DeVita VT Jr, Hellman S, Rosenberg SA (eds) Cancer. Principles & practice of oncology, 7th edn. Lippincott, Williams & Wilkins, Philadelphia, pp 1110–1125
Wiggers T, van de Velde CJH (2002) The circumferential margin in rectal cancer: recommendations based on the Dutch Total Mesorectal Excision Study. Eur J Cancer 38:973–976
Pahlman L (2005) Indications for long-term radiotherapy. In: Büchler MW, Heald RJ, Ulrich B, Weitz J (eds) Rectal cancer treatment. Recent Results Cancer Research 165:212–220
MERCURY Study Group (2006) Diagnostic accuracy of preoperative magnetic resonance imaging in predicting curative resection of rectal cancer: prospective observational study. Br Med J 333:779–784
Brown G, Daniels IR (2005) Preoperative staging of rectal cancer: the MERCURY research project. Recent Results Cancer Res 165:58–74
Daugherty CK (2005) Ethical issues. In: DeVita VT Jr, Hellman S, Rosenberg SA (eds) Cancer. Principles & practice in oncology, 7th edn. Lippincott, Williams & Wilkins, Philadelphia, pp 2747–2758
Ubel PA (2006) Patient decision making. In: Chang AE, Ganz PA, Hayes DF et al (eds) Oncology. An evidence-based approach. Springer Science, New York, pp 177–183
Glas AS, Lijmer JG, Prins MH et al (2003) The diagnostic odds ratio. A single indicator of test performance. J Clin Epidemiol 56:1129–1135
Kim NK, Kim MJ, Park JK et al (2000) Preoperative staging of rectal cancer with MRI, accuracy and usefulness. Ann Surg Oncol 7:732–737
Botterill ID, Blunt DM, Quirke P et al (2001) Evaluation of the role of preoperative magnetic resonance imaging in the management of rectal cancer. Colorectal Dis 3:295–303
Gagliardi G, Bayar S, Smith R, Salem RR (2002) Preoperative staging of rectal cancer using magnetic resonance imaging with external phase-arrayed coils. Arch Surg 137:447–451
Brown G, Radcliffe AG, Newcombe RG et al (2003) Preoperative assessment of prognostic factors in rectal cancer using high-resolution magnetic resonance imaging. Br J Surg 90:355–364
Matsuoka H, Nakamura A, Masaki T et al (2003) A prospective comparison between multidetector-row computed tomography and magnetic resonance imaging in the preoperative evaluation of rectal carcinoma. Amer J Surg 185:556–559
Branagan G, Chave H, Fuller C et al (2004) Can magnetic resonance imaging predict circumferential margins and TNM stage in rectal cancer? Dis Colon Rectum 47:1317–1322
Oberholzer K, Junginger T, Kreitner KF et al (2005) Local staging of rectal carcinoma and assessment of the circumferential resection margin with high-resolution MR imaging using an integrated parallel acquisition technique. JMRI 22:101–108
Ferri M, Laghi A, Mingazzini P et al (2006) Pre-operative assessment of extramural invasion and sphincteral involvement in rectal cancer by magnetic resonance imaging with phase-array coil. Colorectal Dis 7:387–393
Kim CK, Kim SH, Chun HK et al (2006) Preoperative staging of rectal cancer: accuracy of 3-Tesla magnetic resonance imaging. Eur Radiol 16:972–980
Adeyemo D, Hutchinson R (2009) Preoperative staging of rectal cancer: pelvic MRI plus abdomen and pelvic CT. Does extrahepatic abdomen imaging matter? A case for routine thoracic CT. Colorect Dis 11:259–263
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00384-010-0932-7
Rights and permissions
About this article
Cite this article
Hermanek, P., Merkel, S., Fietkau, R. et al. Regional lymph node metastasis and locoregional recurrence of rectal carcinoma in the era of TNM surgery. Implications for treatment decisions. Int J Colorectal Dis 25, 359–368 (2010). https://doi.org/10.1007/s00384-009-0864-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-009-0864-2