Abstract
Purpose
Deterioration of anorectal function after long-course preoperative chemoradiotherapy combined with surgery for rectal cancer is poorly defined. We conducted a prospective study to evaluate the acute and long term effects of preoperative chemoradiotherapy on anorectal function and quality of life of the patients.
Methods
There were 26 patients in surgery group and 31 patients in preoperative chemoradiotherapy group. Anorectal function and quality of life of the patients were assessed by anorectal manometry, incontinence score, quality of life questionnaire.
Results
Significant lower resting pressures in both groups and lower maximal squeeze pressures in the preoperative chemoradiotherapy group were observed after postsurgical evaluations compared with the paired pretreatment ones. In the surgery group, both the Wexner continence score, FIQL score, and the rectoscopy score were comparable before and after surgery, whereas significant worsening in the Wexner score was observed in the preoperative chemoradiotherapy group postoperatively (P < 0.01). Significant reduction in anal canal resting pressures and squeeze pressures, Wexner score, and FIQL score were observed immediately after the completion of preoperative chemoradiotherapy. Significant lower maximal squeeze pressures and worsening of the Wexner scores were observed in the preoperative chemoradiotherapy group compared to the surgery group during the postoperative assessments (P < 0.05 and P < 0.01, respectively).
Conclusions
Both total mesorectal excision and preoperative chemoradiotherapy may adversely affect the anorectal function. Careful selection of the patients who will benefit from neoadjuvant therapy and identifying the patients with a high risk of developing functional problems may help to improve functional outcomes for the treatment of rectal cancer.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Currently preoperative chemoradiotherapy (CRT) combined with total mesorectal excision (TME) is the standard procedure in sphincter-preserving therapy for stage II and III rectal cancer. Neoadjuvant CRT in patients with locally advanced rectal cancer has proven to show oncologic benefits on local control and long-term survival [1–3]. After preoperative CRT, downstaging or complete regression of the tumor may occur which may result in an increase in the number of sphincter-saving operations performed [1, 4, 5]. Both preoperative CRT and low anterior resection (LAR) may impair anorectal functions which has major negative implications on the quality of life (QoL) of the patient. The main effects of pelvic irradiation on deterioration of anorectal function are vascular toxicity and damage to the anal sphincter muscle and pudendal nerve [6, 7].
The aim of this study was to evaluate the acute and long-term effects of pelvic irradiation as a neoadjuvant treatment for rectal cancer on anorectal function and QoL of the patients by using several different tools (anorectal manometry, incontinence score, QoL questionnaire, and rectoscopy).
Patients and methods
Between February 2002 and March 2006, 57 patients with localized rectal cancer were prospectively constituted the intent-to-treat population in the Colorectal Unit of Department of Surgery, Dokuz Eylul University Hospital, Izmir, Turkey.
Pretreatment evaluation included clinical history, general clinical examination, digital rectal examination, a complete blood workup, blood chemistry profile, carcinoembryonic antigen assessment, rigid proctosigmoidoscopy and/or colonoscopy, tumor biopsy, chest X-ray, computed tomography of the abdomen, pelvis, and thorax, and endorectal coil magnetic resonance imaging (ERMRI). In patients for whom it was impossible to pass the ERMRI probe through stenosing rectal tumors, surface MRI was utilized for local staging.
Patients who had undergone prior pelvic surgery or pelvic radiotherapy (RT), patients who had received postoperative pelvic RT and patients who had had a local excision or abdominoperineal resection (APR), and patients who had unresectable tumor were excluded from the study. The treatment regimen was assessed according to the patient's tumor location, stage, age, concomitant medical conditions, and World Health Organization performance status in a multidisciplinary team approach including colorectal surgeons, medical oncologists, radiation oncologists, pathologists, radiologists, and gastroenterologists. The study was approved by the Ethics Committee of Dokuz Eylul University, School of Medicine.
Eligible patients were divided into two groups: surgery group, patients treated with only surgery (n = 26) and preoperative CRT group, patients who underwent CRT before surgery (n = 31). Tumor localization was subsequently subdivided into lower rectum (0 to 5 cm from anal verge), middle rectum (5.1 to 10 cm), and upper rectum (10.1 to 15 cm). Patients in the preoperative CRT group were further subdivided according to the tumor location as middle rectum (n = 12) and lower rectum (n = 18).
Assessment of continence
Wexner continence score: the Wexner continence score is a questionnaire, which scores the severity of fecal incontinence [8]. The scoring system is composed of five items which are focused on type and frequency of incontinence (solid, liquid, gas, and wearing of a pad) and lifestyle alterations. Frequency is scored as follows: 0= never; 1= rarely (<1/month); 2= sometimes (<1/week, ≥1/month); 3= usually (<1/day, ≥1/week); 4= always (≥1/day). Overall score is the sum of the scores of individual items and the lowest score 0 represents perfect continence and the highest score 20 represents worst incontinence.
Anorectal manometry: manometric evaluation of anal sphincter function was performed in our institution's Anorectal Physiology Laboratory. An eight-channel catheter with a water perfusion system was used for the investigation (Medical Measurement Systems, Enschede, The Netherlands) and digitized measurements were analyzed with a computer software. One surgeon (A.E.C.) routinely performed anorectal manometry. Each patient was instructed to empty the rectum before the examination. With the patient in the left lateral position and hips flexed at 90°, the catheter was introduced from the anus. Anal canal resting and squeeze pressures, the first sensation (FS) of rectal filling, maximal tolerable volume (MTV), and presence of rectoanal inhibitory reflex (RAIR) were measured.
Assessment of macroscopical changes
Macroscopical changes on anal canal and rectal mucosa were scored by rectoscopy according to the presence of mucosal pallor or atrophy, telangiectasia, contact bleeding, ulceration, and loss of compliance [9] (each item adds one point to the overall score).
Assessment of quality of life
Quality of life was assessed by the fecal incontinence quality of life questionnaire [FIQL] [10] which is a specific questionnaire to measure health-related QoL in patients with fecal incontinence. In this questionnaire, there are 29 items which are further grouped into four functional subscales: life style (ten items), coping/behavior (nine items), depression/self perception (seven items), and embarrassment (three items). Scores for items are assigned a value from 1 (worst) to 4 (optimal). Scale scores are the mean response to all items in the scale.
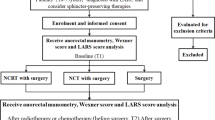
Assessments for continence, macroscopical changes, and QoL were performed before surgery and postoperatively for patients in the surgery group and before and immediately after the completion of preoperative CRT, before surgery, and postoperatively for patients in the preoperative CRT group (Fig. 1).
Chemoradiation protocol
Patients with stage II or III rectal carcinoma in the middle or lower rectum were treated with 6-MV photons by a four-field pelvis technique. The fields extended from L5/S1 level superiorly to the lower border of obturator foramina inferiorly, with a 1 to 1.5 cm margin on the bony pelvic inlet. Patients received RT 1.8 Gy/day, 5 days/week to give a total 25 fractions over a period of 5 weeks for a total of 4,500 cGy with concurrent chemotherapy (5-fluorouracil 225 mg/m2/day infusion for 5 days/week during a period of 5 weeks).
Surgery
The surgical technique included a mesorectal excision as described previously [11]. A total mesorectal excision was performed for tumors in the lower and middle rectum; for patients with upper rectal tumors, the mesorectum was divided 5 cm from the distal border of the tumor with high ligation of the inferior mesenteric artery. If the tumor was attached to adjacent parietes or viscera, en bloc excision was performed. A temporary diverting loop ileostomy was constructed in all patients who had preoperative CRT. In patients who had sphincter invasion and in whom 1 cm distal border was not achieved, APR was performed. In the preoperative CRT group, patients underwent surgery 8 weeks after the completion of CRT.
Statistical analysis
Quantitative data were expressed as mean ± SD; scores were expressed as median and range. The Mann–Whitney U test and the t test were used to compare median scores and mean values, respectively. The Wilcoxon signed rank test was used for nonparametric comparison of dependent variables. Frequencies between different groups were calculated by means of the Fisher's exact test. The Paired samples t test was used to compare the values in the same patient during the treatment. Repeated measurement analyses were used for comparison of anorectal manometrical changes between the subgroups of preoperative CRT during the treatment; P < 0.05 was considered to be significant in all analyses.
Results
Fifty-seven patients gave informed consent to participate in the study. The mean patient age was 61 years (range, 25–85 years) and male/female ratio was 1:8. Twenty-four patients underwent resection and anastomosis without preoperative CRT (surgery group), and 20 patients underwent resection and anastomosis after CRT (preoperative CRT group). In the surgery group, one patient underwent APR and one patient underwent transanal local excision. In the preoperative CRT group, three patients were considered as having unresectable tumors due to the diagnosis of frozen pelvis detected either by preoperative radiological imaging just before the surgery or at the laparotomy; seven patients underwent APR and one patient who had coronary vascular disease died due to acute coronary syndrome during preoperative CRT (Fig. 2).
No anastomotic leakage was observed in either group. Preoperative CRT did not result in significant morbidity. The most frequent adverse effect of preoperative CRT was grade 1–2 skin irritation which affected 47% of the patients; two patients had grade four intestinal adverse effects. Intermittent diarrhea was controlled with symptomatic therapy. Three patients (9.7%) showed histopathological complete response, and 16 patients (51.6%) showed ypT and/or ypN downstaging in the preoperative CRT group.
The demographic data of the study population, tumor characteristics, and pretreatment evaluations are presented in Table 1. No significant differences were observed in terms of age, sex, and pretreatment evaluations between the groups. Patients in the preoperative CRT group had more advanced and distally located tumors. Postoperative evaluations were repeated after a median of 417 days (range, 149–477 days). The pressures in the anal canal showed significant lower resting pressures (RP) in both groups and lower maximal squeeze pressures (SP) in the preoperative CRT group after surgery compared with paired pretreatment ones (Fig. 3). In the surgery group, both the Wexner continence score, FIQL score, and rectoscopy score were comparable before and after surgery where as significant worsening in the Wexner score observed in the preoperative CRT group postoperatively compared with the pretreatment ones (3 vs. 0; P < 0.01). Table 2 presents the comparison of postoperative evaluations of the groups. Patients in the preoperative CRT group had significantly lower maximal SP (144.4 ± 28.2 mmHg vs. 166.8 ± 23.1 mmHg) and had a significant worsening of the median Wexner continence scores (3 vs. 0) compared with the patients treated with only surgery (P < 0.05 and P < 0.01, respectively) during the postoperative assessments.
In the preoperative CRT group, resting and squeeze anal canal pressures were significantly reduced by CRT, and the Wexner continence score and FIQL (both subscales) were adversely affected during CRT (Table 3). Demographical characteristics and pretreatment evaluations were comparable for patients in the preoperative CRT group according to the tumor localization which was subdivided into the middle and lower rectum. The only significant difference was observed in the maximal RP (MRP), which was adversely affected in patients with middle rectal tumors during the treatment (P < 0.015).
The threshold for first sensation and maximum tolerable volume measurements and disappearance of RAIR were not significantly different between the groups or during the different periods of the study.
Macroscopical changes assessed and scored by rectoscopy revealed no significant difference between the groups or during the different periods of the study.
Discussion
Efforts to improve outcomes for the treatment of rectal cancer continued with adjuvant and neoadjuvant CRT after the introduction of TME. Randomized trials have demonstrated improved oncological outcomes and lower toxicity of preoperative CRT [1, 12]. Administration of preoperative CRT may also lead to an increase in the number of sphincter-saving procedures performed because the tumor size is reduced before surgery [1, 13, 14]. Both preoperative CRT and surgery can impair anorectal functions and may adversely affect the patient's QoL especially for deep-sated tumors. Health-related QoL is an important consideration when evaluating the efficacy of treatment. In our study, we aimed to assess the effects of preoperative CRT on anorectal functions and patients QoL.
The main pathogenesis for impairment of anorectal functions with pelvic RT is the irradiation of the anal canal. Irradiation may damage the myenteric plexus and inhibit the impulse conduction, or it may directly damage the anal sphincter muscles and cause fibrosis [9, 15–17]. The long-term effects of postoperative RT on anorectal functions have been studied in a randomized study where patients with resectable rectal cancer were randomized to surgery alone or surgery combined with postoperative RT [18]. They reported worse anorectal dysfunction, measured as stool frequency, fecal urgency, and fecal incontinence in patients who had postoperative RT than that of patients who had received no adjuvant therapy. Although this was a randomized study with a long observational period, in all cases, sphincters were irradiated which may lead to an overemphasis on the risk of anorectal dysfunction. Also the irradiation of the neorectum may contribute to the negative results in patients who received postoperative RT. The functional effects of irradiation on anorectal function are dose dependent [19]. The effects of a preoperative short-course RT administration on the risk of developing fecal incontinence in patients who underwent LAR have been studied in randomized and nonrandomized studies [15, 20, 21]. Pollack et al. [15] concluded that short-course RT, including the anal sphincters, impairs anorectal function. There were no significant differences in QoL scores between irradiated and nonirradiated patients in Swedish and Dutch trials [15, 20] whereas Murata et al. [21] reported worsened QoL in irradiated patients. Currently, the effects of preoperative long-course radiation on anorectal function have not been studied in a randomized trial. Results of three studies assessing the effects of preoperative long-course CRT on anorectal functions in patients who underwent surgery with or without preoperative CRT were summarized in Table 4 [16, 22, 23]. There are several other studies evaluating postoperative anorectal function and/or QoL in patients who underwent preoperative long-course CRT. Wagman et al. [24] and Lim et al. [6] reported worsened incontinence scores and Tjandra et al. [25] reported impaired QoL in patients who underwent preoperative long-course CRT. In our study, we observed an impairment of the Wexner score at the postoperative long-term evaluations in patients who underwent preoperative CRT; which did not significantly impaired the patients QoL assessed by FIQL questionnaire.
Total mesorectal excision and anastomosis can lead to anterior resection syndrome which is characterized by urgency, frequent bowel movements, and some degree of fecal incontinence. Impairment of innervation by pelvic nerve injury and loss of rectal reservoir function after surgery may contribute to the alteration of continence and QoL. We demonstrated that only TME results in reduction of sphincter pressures without any significant change in the Wexner score and patients' QoL. Addition of preoperative CRT to TME results in reduction of both resting and squeeze anal canal pressures and Wexner continence score without any significant effect on patients QoL. As our two groups are not balanced for tumor localization and stage, those effects may not only due to preoperative CRT. We performed additional analysis excluding upper rectal tumors in surgery group. The only difference was between Wexner scores; there was no significant difference between groups.
The disappearance of RAIR and decrease in maximum-tolerated volume may result in increased stool frequency and may contribute to the negative effects of sphincter impairment on QoL in patients who underwent preoperative CRT. Our results showed lower MTVs and RAIR disappearance in the preoperative CRT group during postoperative evaluations, but the differences between the surgery and preoperative CRT groups were not significant.
Lim et al. and Ammann et al. investigated the relation between the tumor localization and effects of preoperative CRT on anorectal function, and Ammann et al. showed impairment of MRP, MTV, and FS in patients with middle rectal tumors. In our study, we only observed a significant impairment of MRP during preoperative CRT in patients with middle rectal cancer. These results may contribute to the hypothesis of Varma et al. [9] proposing that the internal anal sphincter, because of its fixed anatomical position and small volume, is particularly susceptible to the effects of irradiation.
In conclusion, both TME and CRT may adversely affect the anorectal function to some degree. Selection of the patients who will benefit from neoadjuvant therapy, identifying the patients with a high risk of developing functional problems, avoiding unnecessary irradiation of the anal sphincters, and the acceptance of modern three-dimensional conformal RT techniques may all help to improve functional outcomes for the treatment of rectal cancer.
One goal of surgeons and oncologists who work with rectal cancer patients is to improve their health-related quality of life issues. Therefore, as new technological innovations in this field move toward even more advanced “state of the art” capabilities, weighing the possible oncological outcomes for patients along with the potential deleterious effects on functional results will continue to present a formidable challenge.
References
Sauer R, Becker H, Hohenberger W et al (2004) Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med 351:1731–1740
Kapiteijn E, Marijnen CA, Nagtegaal ID et al, Dutch Colorectal Cancer Group (2001) Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med 345:638–646
Theodoropoulos G, Wise WE, Padmanabhan A et al (2002) T-level downstaging and complete pathologic response after preoperative chemoradiation for advanced rectal cancer result in decreased recurrence and improved disease-free survival. Dis Colon Rectum 45:895–903
Wheeler JM, Dodds E, Warren BF et al (2004) Preoperative chemoradiotherapy and total mesorectal excision surgery for locally advanced rectal cancer: correlation with rectal cancer regression grade. Dis Colon Rectum 47:2025–2031
Terzi C, Canda AE, Sagol O et al (2008) Survivin, p53, and Ki-67 as predictors of histopathologic response in locally advanced rectal cancer treated with preoperative chemoradiotherapy. Int J Colorectal Dis 23:37–45
Lim JF, Tjandra JJ, Hiscock R, Chao MW, Gibbs P (2006) Preoperative chemoradiation for rectal cancer causes prolonged pudendal nerve terminal motor latency. Dis Colon Rectum 49:12–19
Frykholm GJ, Glimelius B, Påhlman L (1993) Preoperative or postoperative irradiation in adenocarcinoma of the rectum: final treatment results of a randomized trial and an evaluation of late secondary effects. Dis Colon Rectum 36:564–572
Jorge JM, Wexner SD (1993) Etiology and management of fecal incontinence. Dis Colon Rectum 36(1):77–97
Varma JS, Smith AN, Busuttil A (1985) Correlation of clinical and manometric abnormalities of rectal function following chronic radiation injury. Br J Surg 72(11):875–878
Rockwood TH, Church JM, Fleshman JW et al (2000) Fecal ıncontinence quality of life scale: quality of life instrument for patients with fecal incontinence. Dis Colon Rectum 43:9–16
Heald RJ, Ryall RD (1986) Recurrence and survival after total mesorectal excision for rectal cancer. Lancet 1:1479–1482
Wong RK, Tandan V, De Silva S, Figueredo A (2007) Pre-operative radiotherapy and curative surgery for the management of localized rectal carcinoma. Cochrane Database Syst Rev 2:CD002102
Minsky BD (1997) Adjuvant therapy for rectal cancer—a good first step. N Engl JMed 336:1016–1017
Valentini V, Glimelius B, Minsky BD et al (2005) The multidisciplinary rectal cancer treatment: main convergences, controversial aspects and investigational areas which support the need for a European Consensus. Radiother Oncol 76:241–250
Pollack J, Holm T, Cedermark B, Holmström B, Mellgren A (2006) Long-term effect of preoperative radiation therapy on anorectal function. Dis Colon Rectum 49:345–352
Ammann K, Kirchmayr W, Klaus A et al (2003) Impact of neoadjuvant chemoradiation on anal sphincter function in patients with carcinoma of the midrectum and low rectum. Arch Surg 138:257–261
Da Silva GM, Berho M, Wexner SD et al (2003) Histologic analysis of the irradiated anal sphincter. Dis Colon Rectum 46:1492–1497
Lundby L, Jensen VJ, Overgaard J, Laurberg S (1997) Long-term colorectal function after postoperative radiotherapy for colorectal cancer. Lancet 350:564
Kusunoki M, Shoji Y, Yanagi H et al (1993) Anorectal function after preoperative intraluminal brachytherapy and colonic J pouch-anal anastomosis for rectal carcinoma. Br J Surg 80:933–935
Dahlberg M, Glimelius B, Graf W, Påhlman L (1998) Preoperative irradiation affects functional results after surgery for rectal cancer: results from a randomized study. Dis Colon Rectum 41:543–549
Murata A, Brown CJ, Raval M, Phang PT (2008) Impact of short-course radiotherapy and low anterior resection on quality of life and bowel function in primary rectal cancer. Am J Surg 195:611–615
Gervaz P, Rotholtz N, Pisano M et al (2001) Quantitative short-term study of anal sphincter function after chemoradiation for rectal cancer. Arch Surg 136(2):192–196
Pietsch AP, Fietkau R, Klautke G, Foitzik T, Klar E (2007) Effect of neoadjuvant chemoradiation on postoperative fecal continence and anal sphincter function in rectal cancer patients. Int J Colorectal Dis 22:1311–1317
Wagman R, Minsky BD, Cohen AM, Guillem JG, Paty PP (1998) Sphincter preservation in rectal cancer with preoperative radiation therapy and coloanal anastomosis: long term follow-up. Int J Radiat Oncol Biol Phys 42:51–57
Tjandra JJ, Reading DM, McLachlan SA et al (2001) Phase II clinical trial of preoperative combined chemoradiation for T3 and T4 resectable rectal cancer: preliminary results. Dis Colon Rectum 44:1113–1122
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Canda, A.E., Terzi, C., Gorken, I.B. et al. Effects of preoperative chemoradiotherapy on anal sphincter functions and quality of life in rectal cancer patients. Int J Colorectal Dis 25, 197–204 (2010). https://doi.org/10.1007/s00384-009-0807-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-009-0807-y