Abstract
Purpose
Tumour stage is the strongest prognostic parameter in colorectal cancer. The study aimed to evaluate the prognostic impact of pT2, pT3, and pT4 sub-classification.
Methods
Three hundred eighty-one surgical colorectal cancer specimens were retrospectively re-evaluated. pT2 tumours were sub-classified according to infiltration of the inner circumferential (pT2a) or outer longitudinal (pT2b) layer of the muscularis propria. pT3 tumours were sub-classified by measuring the maximal tumour invasion beyond the outer border of the muscularis propria (pT3a ≤ 1 mm, pT3b > 1–5 mm, pT3c > 5–15 mm, and pT3d > 15 mm). pT4 tumours were sub-classified according to invasion of other organs or structures (pT4a) or perforation of the visceral peritoneum (pT4b). Data were correlated with other pathological parameters and patient outcome.
Results
Seventy pT2 tumours were re-classified as 37 pT2a and 33 pT2b tumours. There was no significant association with tumour grade, angioinvasion, or lymph node involvement and no significant impact on prognosis. Two hundred eighteen pT3 tumours were re-classified as 49 pT3a, 83 pT3b, 53 pT3c, and 33 pT3d tumours. pT3 sub-classification was significantly associated with tumour grade, angioinvasion, and lymph node involvement and proved to be an independent prognostic variable with respect to progression-free and cancer-specific survival. A cut-off level of 5 mm is recommended. Sixty-five pT4 tumours were re-classified as 15 pT4a and 50 pT4b tumours. There was no significant association with tumour grade, angioinvasion, or lymph node involvement and no significant impact on prognosis.
Conclusions
pT3 sub-classification was significantly associated with patient outcome. In contrast, pT2 and pT4 sub-classification did not show clinical significance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tumour stage reflected by the UICC TNM system is currently regarded as the strongest prognostic parameter for patients with colorectal cancer (CRC). Thus, accurate staging provides broadly applicable prognostic information, helps to evaluate the effects of treatment, and is the basis of all authoritative patient management decisions [1–3].
Patients with stage I cancer (pT1N0M0 and pT2N0M0) are generally considered to share favourable prognosis. However, a small subgroup of them will die due to local or distant recurrence after curative resection. There are limited data regarding parameters identifying patients at risk for failure in early stage disease. To date, the potential prognostic value of a pT2 sub-classification depending on depth of invasion within the muscle wall has not been assessed.
Evaluation of stage II cancer (pT3N0M0 and pT4N0M0) is critical because it determines whether adjuvant therapy should be offered [4]. Currently, parameters to identify high-risk stage II patients who might benefit from adjuvant therapy are not well-defined. According to literature data, pT3 sub-classification, referring to the maximal tumour invasion beyond the outer border of the muscularis propria, may be useful for risk stratification of affected patients [5–14] and has, thus, been included in the TNM supplement [15]. In routine surgical pathology, however, pT3 sub-classification is infrequently applied, and its prognostic significance—compared with other parameters, such as angioinvasion—still remains to be defined.
pT4 CRCs have been sub-classified into pT4a and pT4b tumours, depending on the presence of invasion into adjacent organs or structures without perforation of visceral peritoneum (pT4a) or presence of penetration of the visceral peritoneum with or without free perforation into the peritoneal cavity (pT4b) [15]. In fact, serosal penetration represents a well-established prognostic parameter in CRC [16–24]. To the best of our knowledge, however, a systematic study analysing pT4a and pT4b cancer cases with respect to possible associations with other clinicopathological parameters, as well as prognostic impact is still lacking.
Our study, therefore, aimed to evaluate the prognostic impact of pT2, pT3, and pT4 sub-classification with regard to both progression-free and cancer-specific survival, including univariate and multivariate analyses. We examined these factors for colon and rectal cancers separately and compared data with established prognostic variables, such as tumour differentiation, angioinvasion, and nodal status.
Patients and methods
Case selection
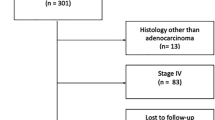
A random sample of 400 patients was selected from the files of the CRC data base of the Institute of Pathology, Medical University of Graz, Austria, covering a total of 7,909 CRCs from 7,564 patients (4,095 men and 3,469 women; ratio 1.2:1) operated upon between January 1984 and December 2005. The following patients were excluded: (i) those who underwent endoscopic polypectomy for low-risk T1 cancer due to missing data regarding nodal status; (ii) patients who underwent neoadjuvant chemotherapy due to presumptive treatment-related changes in T classification; (iii) patients with synchronous or metachronous secondary CRC; and (iv) patients with competitive invasive cancers originating from other sites if metastatic deposits were not assessed by histology.
In total, 381 specimens from 400 patients (95%) were available for review pathology. There were 215 males (56%) and 166 females (44%) (ratio 1.3:1) with a mean age of 68.5 (median 70.1, range 27.6–93.1) years. Postoperative therapy was guided by UICC stage: stage I and II patients did not receive adjuvant therapy, whereas, stage III patients were given 5-fluorouracil/folinic acid according to the Mayo Clinic regimen.
Follow-up included laboratory testing (blood count, liver enzymes, CEA, and CA19-9) at a 3-month interval for the first 3 years and a 6-month interval thereafter. Chest X-ray and abdominal ultrasound were performed at a 6-month interval for the first 3 years and yearly thereafter. Patients with rectal cancer underwent pelvic computerised tomography every 12 months.
Disease progression was defined as locoregional tumour recurrence or development of distant metastasis. The study was approved by the Ethics Committee of the Medial University of Graz, Austria.
Pathological evaluation
Patient records and histopathological slides were independently re-evaluated by two investigators (C.L. and M.J.P.) who were blinded to clinical data, especially patient outcome. A mean number of 4.5 (median 4, range 1–17) paraffin-embedded tissue blocks was available for analysis, with 352 of 381 (92.4%) cases showing at least three blocks.
Tumours located in the caecum to transverse colon were defined as right-sided cancers, and tumours located in the left colonic flexure to sigmoid colon were defined as left-sided cancers. Tumours originating from the rectosigmoid junction (ICD-O C19) or within the rectum (ICD-O C20) were summarised as rectal cancers, as originally suggested in the “5th edition of the TNM classification” from 1997 [25].
Tumour stage was assessed according to the UICC 2002 issue of the TNM classification [26]. pT3 and pT4 tumours were sub-classified according to the recommendations of the UICC 2003 TNM supplement [15]: pT3 tumours by measuring the maximal tumour invasion beyond the outer border of the muscularis propria (pT3a ≤ 1 mm, pT3b > 1–5 mm, pT3c > 5–15 mm, and pT3d > 15 mm) and pT4 tumours according to direct invasion of other organs or structures (pT4a) or perforation of the visceral peritoneum (pT4b). A pT2 sub-classification is not included in the TNM supplement. We performed pT2 sub-classification for study purpose as follows: pT2a with infiltration of the inner circumferential and pT2b with infiltration of the outer longitudinal layer of the muscularis propria. Tumour grading was performed according to the World Health Organization guidelines, assessing the extent of glandular appearance [27].
Statistical analysis
Associations between tumour classification and tumour grade, nodal status, as well as presence of lymphatic and/or venous invasion were analysed using the chi square test or the Fisher's exact test. Disease-free (progression-free) and cancer-specific survival was investigated using the Kaplan–Meier method and compared by the log-rank test. For multivariate testing, a Cox’s proportional hazards regression model was performed. All statistical calculations were performed using NCSS (Hintze, J. (2007) NCSS, LLC. Kaysville, Utah, USA www.ncss.com). All reported p values were 2-sided with significance at p < 0.05.
Results
Pathological data
Tumours were located in the caecum in 49 patients (13%), in the ascending colon in 27 (7%), at the hepatic flexure in 18 (5%), in the transverse colon in 13 (3%), at the splenic flexure in 13 (3%), in the descending colon in 15 (4%), in the sigmoid colon in 82 (22%), at the rectosigmoid junction in 15 (4%), and in the rectum in 149 patients (39%). According to our definition, 107 tumours (28%) were right-sided colon cancers, 110 (29%) were left-sided colon cancers, and 164 (43%) were rectal cancers.
Overall, classification pT1 was present in 28 (7%), pT2 in 70 (18%), pT3 in 218 (57%), and pT4 in 65 (17%) cases, respectively. Lymph node metastases were observed in 168 (44%) patients. Eighty-two (22%) patients were operated upon in UICC stage I, 125 (33%) in UICC stage II, 151 (40%) in UICC stage III, and 23 (6%) in UICC stage IV. A positive margin (R1 resection) was observed in eight (2%) cases, four pT3 and four pT4 tumours.
Histology revealed 318 conventional adenocarcinomas, 44 mucinous adenocarcinomas, three signet-ring cell carcinomas, two medullary carcinomas, one adenosquamous carcinoma, and 13 undifferentiated carcinomas. Tumour grades were G1 in 121 (32%), G2 in 138 (36%), G3 in 99 (26%), and G4 in 23 (6%) cases.
Seventy (18%) pT2 tumours were sub-classified as 37 (53%) pT2a and 33 (47%) pT2b tumours. There was no significant association with tumour grade, angioinvasion, or nodal status. Two hundred eighteen (57%) pT3 tumours were sub-classified as 49 (22%) pT3a, 83 (38%) pT3b, 53 (24%) pT3c, and 33 (15%) pT3d tumours. pT3 sub-classification was significantly associated with tumour grade, angioinvasion, and nodal status. Sixty-five (17%) pT4 tumours were sub-classified as 15 (23%) pT4a and 50 (77%) pT4b tumours. There was no significant association with tumour grade, angioinvasion, or lymph node involvement (Table 1).
Survival analysis
Follow-up data were available for 350 out of 381 (92%) patients. After a mean and median follow-up of 56 and 45 months, progressive disease was observed in 141 out of 350 (40%) patients: 118 patients who died from cancer and eleven patients who currently are alive with metastatic disease, but also seven patients who currently show no evidence of disease after metastasectomy and five patients who initially presented in poor condition due to advanced disease and who died within 30 days of surgery. Mean time to progression was 15 months (median 7, range 0–88). With respect to patients with rectal cancers, 24 out of 155 (15%) locoregional and 51 out of 155 (33%) distant recurrences were noted; seven (5%) patients experienced both locoregional and distant tumour recurrence. Actuarial 5-year recurrence-free rate for patients with locoregional recurrence and patients with systemic recurrence was 80% and 66%, respectively. Overall, both disease-free and cancer-specific survival of CRC patients was significantly associated with pT classification (p < 0.001, log-rank test; Fig. 1a, b).
pT2 sub-classification was not significantly related to patient outcome: seven out of 35 (20%) patients with pT2a and six out of 33 (18%) patients with pT2b tumours experienced disease progression (p = 0.73, log-rank test; Fig. 2a). Actuarial 5-year disease-free survival rates were 81% for patients with pT2a and pT2b disease. In addition, five (14%) patients with pT2a and five (15%) patients with pT2b tumours died of disease (p = 0.96, log-rank test; Fig. 2b).
pT3 sub-classification, however, yielded significant data. Thus, regarding both colon and rectal cancers, 11 out of 47 (23%) patients with pT3a, 23 out of 75 (30%) patients with pT3b, 29 out of 49 (59%) patients with pT3c, and 14 out of 24 (58%) patients with pT3d tumours experienced disease progression (p < 0.001, log-rank test; Fig. 3a). Actuarial 5-year disease-free survival rates for patients with pT3a, pT3b, pT3c, and pT3d disease were 75%, 69%, 44%, and 32%, respectively. In addition, ten (21%) patients with pT3a, 20 (27%) patients with pT3b, 25 (51%) patients with pT3c, and 10 (42%) patients with pT3d tumours died of disease (p = 0.001, log-rank test; Fig. 3b).
a Progression-free (p < 0.001, log-rank test) and b cancer-specific (p = 0.001, log-rank test) survival in patients with pT3 colorectal carcinoma related to tumour sub-classification (pT3a versus pT3b versus pT3c versus pT3d). c Progression-free (p = 0.008, log-rank test) and d cancer-specific (p = 0.02, log-rank test) survival in patients with pT3 colon carcinoma related to tumour sub-classification (pT3a versus pT3b versus pT3c versus pT3d). e Progression-free (p < 0.001, log-rank test) and f cancer-specific (p = 0.03, log-rank test) survival in patients with pT3 rectal carcinoma related to tumour sub-classification (pT3a versus pT3b versus pT3c versus pT3d)
With respect to site-specific prognostic evaluation, pT3 sub-classification also proved to be a significant prognosticator if colon and rectal cancers were analysed separately. Thus, in colon cancer two out of 28 (7%) patients with pT3a, ten out of 39 (26%) patients with pT3b, 13 out of 29 (45%) patients with pT3c, and five out of 14 (36%) patients with pT3d tumours experienced disease progression (p = 0.008, log-rank test; Fig. 3c). Actuarial 5-year disease-free survival rates for patients with pT3a, pT3b, pT3c, and pT3d disease were 96%, 74%, 60%, and 58%, respectively. In addition, two (7%) patients with pT3a, nine (23%) patients with pT3b, 11 (38%) patients with pT3c, and four (29%) patients with pT3d tumours died of disease (p = 0.02, log-rank test; Fig. 3d). In rectal cancer, similarly, nine out of 19 (47%) patients with pT3a, 13 out of 36 (36%) patients with pT3b, 16 out of 20 (80%) patients with pT3c, and nine out of ten (90%) patients with pT3d tumours experienced disease progression (p < 0.001, log-rank test; Fig. 3e). Actuarial 5-year disease-free survival rates for patients with pT3a, pT3b, pT3c, and pT3d disease were 72%, 70%, 30%, and 38%, respectively. In addition, eight (42%) patients with pT3a, 11 (31%) patients with pT3b, 14 (70%) patients with pT3c, and six (60%) patients with pT3d tumours died of disease (p = 0.03, log-rank test; Fig. 3f).
The 5 mm cut-off level separating pT3a/b from pT3c/d disease proved to be the strongest prognosticator in univariate Cox analysis (data not shown) and was consecutively used for multivariate testing. In multivariate, Cox’s proportional hazards regression models of pT3 patients including patient age, gender, tumour sub-classification (pT3c/d versus pT3a/b), and nodal status both presence of lymph node metastasis and tumour sub-classification proved to be independent predictors of disease progression (pT3 sub-classification; p = 0.002, risk ratio (RR) = 2.09, 95% confidence interval (CI) = 1.31–3.33; nodal disease/UICC stage III: p < 0.001, RR = 3.92, 95% CI = 2.34–6.56) and cancer-specific survival (pT3 sub-classification; p = 0.022, RR = 1.80, 95% CI = 1.09–2.96; nodal disease/UICC stage III: p < 0.001, RR = 4.28, 95% CI = 2.43–7.52). When data regarding angioinvasion and R-status were added to analysis pT3 sub-classification still proved to be an independent predictor of progression-free survival, whereas, data regarding cancer-specific survival just missed statistical significance (Table 2). Restricting data analysis to colon or rectal cancers yielded comparable results. In colon cancer (no cases with R1 resection), pT3 substaging proved to be an independent prognosticator with respect to both progression-free and cancer-specific survival (Table 3), whereas, in rectal cancer (including four cases with R1 resection), pT3 substaging served as an independent predictor of progression-free, yet, not of cancer-specific survival (Table 4).
In a final multivariate model restricted to pT3 patients lacking nodal disease (UICC stage IIA), positive resection margin (R1 resection), and presence of blood vessel invasion proved to be the only independent prognostic variables (Table 5).
pT4 sub-classification, finally, did not yield significant data with respect to patient outcome: 11 out of 13 (85%) patients with pT4a and 39 out of 47 (83%) patients with pT4b tumours experienced disease progression (p = 0.93, log-rank test; Fig. 4a). Interestingly, with regard to tumour location, 13 out of 43 (30%) patients with colon cancers and one of 17 (6%) patients with rectal cancers showed peritoneal tumour progression. Actuarial 5-year disease-free survival rates for patients with pT4a and pT4b disease were 15% and 16%, respectively. In addition, 11 (85%) patients with pT4a and 31 (66%) patients with pT4b tumours died of disease (p = 0.29, log-rank test; Fig. 4b). It is worth mentioning, however, that during the first years of follow-up the survival curves diverged markedly. Thus, actuarial 2-year disease-free and cancer-specific survival rates were lower for patients with pT4a disease (15% and 23%) than for patients with pT4b disease (21% and 61%), respectively.
Discussion
Risk stratification of CRC patients for prognostic evaluation is mainly based on the TNM staging system. In accordance with published literature data [1–3], pT classification proved significant influence on both disease-free and cancer-specific survival in our patient cohort.
pT sub-classification, which has been addressed in the TNM supplement for pT3 and pT4 disease [15], might serve as a more accurate tool to predict outcome in affected patients. Justification of pT sub-classification, however, is limited due to scarce literature data, especially with respect to pT4 disease [5–14, 16–24]. This prompted us to perform a systematic retrospective analysis of surgically resected tumour specimens in order to investigate the prognostic significance of pT2, pT3, and pT4 sub-classification in CRC.
Pathologic variables identifying patients with pT2 disease who are at high-risk for failure are not well-defined [28, 29]. To the best of our knowledge, the potential prognostic value of a pT2 sub-classification has not been investigated yet. According to our study, pT2 sub-classification, assessed by measuring the depth of muscularis propria invasion (adopting the TNM bladder cancer criteria), did not prove feasible in order to predict patient outcome. Moreover, there was no significant association with tumour grade, angioinvasion, or lymph node involvement. Small sample size (seventy pT2 tumours) and few events (only thirteen patients experienced diseases progression and ten died of disease), despite mean follow-up of nearly 6 years, may account for our findings. Thus, future (prospective) studies including more patients are warranted to fully clarify the potential prognostic impact of the proposed pT2 sub-classification.
Peritoneal involvement, the hallmark of pT4 disease, represents a well-established prognostic parameter in CRC [16–24]. Earlier studies analysing both colon and (upper) rectal carcinomas showed that serosal penetration is useful in predicting survival in affected patients [16, 17]. Restricting data analysis to colon cancer showed similar data. Thus, serosal penetration was significantly associated with tumour recurrence and reduced survival in univariate and multivariate analyses [18–22]. With respect to (upper) rectal cancers, Shepherd et al. demonstrated the independent prognostic disadvantage of peritoneal involvement already more than 10 years ago [23]. A recent prospective study by Keshava et al. confirmed these data. The authors reported that direct tumour spread to the free serosal surface independently predicts pelvic recurrence and reduced survival in rectal cancer patients [24].
pT4 CRCs may be subdivided depending on the presence of invasion into adjacent organs or structures without perforation of visceral peritoneum (pT4a) or presence of penetration of the visceral peritoneum with or without free perforation into the peritoneal cavity (pT4b). As shown in the TNM supplement [15], median survival time following surgical resection for cure was shorter for pT4b tumours (pT4bM0 46.2 months; pT4bM1 15.5 months) compared with pT4a tumours (pT4aM0 58.2 months; pT4aM1 22.7 months). This difference, however, was not statistically significant. To the best of our knowledge, a systematic analysis evaluating the pT4 sub-classification proposed in the TNM supplement with respect to associations with other histopathologic parameters, as well as impact on survival is still lacking.
In our investigation of pT4a and pT4b cancers, no significant differences with respect to tumour grade or lymph node involvement were noted. Interestingly, however, lymph vessel invasion was observed in two thirds of pT4a but only 40% of pT4b cancers. This difference, however, missed statistical significance. With respect to prognosis, patients with pT4a and pT4b cancers both shared a dismal disease course. Actuarial 5-year disease-free survival rates were almost the same, accounting for approximately 15% of cases. At 2 years follow-up, survival rate of patients with pT4a disease were even lower than those of patients with pT4b disease. Since only 65 pT4 tumours were included in our investigation, a site-specific subgroup analysis did not prove feasible (data not shown). Nevertheless, according to our investigation and available literature data, the prognostic impact of pT4 sub-classification is questionable. Future (prospective) studies are needed, and as long as the usefulness of pT4 sub-classification has not unequivocally been proven, recommendation of this classification remains arguable.
Stage II CRC patients share marked variability in clinical outcome with five-year survival rates ranging between 60 and 75 percent [14, 20, 21, 30, 31]. Assessment of pathological parameters that might enable more accurate risk stratification in order to identify high-risk patients who might benefit from adjuvant therapy remains a key issue of CRC research today. A number of studies have demonstrated usefulness of pT3 sub-classification, referring to the maximal tumour invasion beyond the outer border of the muscularis propria, for stratifying affected patients [5–14].
Whereas, data regarding the impact of pT3 sub-classification on prognosis of rectal cancer patients are manifold [5–7, 9, 11, 13], literature provides only limited information regarding the impact of pT3 sub-classification on prognosis of colon cancer patients [8]. Two other studies investigated colon and rectal cancer patients together [10, 14]. A single systematic study analysing colon and rectal cancers as separate patient subsets, however, is still lacking. To summarise existing literature data, the above-mentioned investigations assessed the importance of depth of tumour invasion beyond the outer border of the muscularis propria in univariate and multivariate analyses with respect to a five-year [5, 13] and eight-year [14] cancer-related [7, 8], recurrence-free [6], as well as overall survival [10, 12]. In our study, pT3 sub-classification yielded significant data concerning both disease progression and cancer-specific survival for patients with pT3 colon carcinomas, whereas in rectum cancer, pT3 substaging served as an independent predictor of progression-free, yet not of cancer-specific survival.
Following the TNM supplement [15], we initially applied a four-tiered approach to sub-classify pT3 disease. The 5 mm cut-off value, which has been used by other groups [7, 14], proved to be the strongest prognosticator and is, therefore, recommended for risk stratification of affected patients in routine settings. Other authors, however, applied different stratification schemes. Thus, in their studies on rectal cancer, Willett et al. [6] and Harewood et al. [11] selected 2 mm as the best cut-off value; Cawthorn et al. [5] used 4 mm while Miyoshi et al. [13] used 6 mm invasion into perirectal fat to define patient subsets with significantly different outcome. In their study on colon cancer, Merkel et al. [8] even suggested 15 mm as threshold to identify high-risk patients. In the landmark investigation by Krook et al. [32], the authors distinguished the following categories: T3A with microscopic and T3B with gross invasion into perirectal fat, as well as T3C with adherence to adjacent organs. A similar approach was made by Steel et al. [9]: the authors classified pT3 rectal cancers in minimally invasive (visible on micoscopic examination only) or advanced groups. Finally, Shinto et al. [10] classified pT3 disease according to histologic invasion beyond the subserosal elastic lamina.
Is pT3 sub-classification a crucial factor for selecting patients for adjuvant treatment who, according to standard guidelines, currently do not receive adjuvant medication? So far, only four studies specifically addressed this topic focusing on patients with stage II disease. Shinto et al. [10], using the subserosal elastic lamina as anatomic landmark for stratification, assessed their patients only with univariate analysis and data just reached marginal statistical significance (p = 0.043). In the study by Cianchi et al. [14], 5 mm invasion beyond the outer border of the muscularis propria proved to be an independent prognosticator of cancer-related death (p = 0.04). Lymph or blood vessel invasion, however, was not included in Cox analysis. In the two comprehensive studies analysing the Erlangen Registry for Colorectal Carcinoma database, Merkel et al. [7, 8] used the depth of invasion beyond the outer border of the muscularis propria as a parameter to define a high-risk group of patients. pT3 sub-classification, analysed as a single parameter, however, proved statistical significance only in univariate, yet not in multivariate testing. In our dataset, pT3 sub-classification also failed in identifying stage II high-risk patients in Cox analysis. The only independent prognostic markers in this patient subset proved to be positive resection margin (R1 resection), as well as blood vessel invasion.
There are several limitations to our study. First and foremost are the limitations inherent to retrospective analyses. By performing review pathology, we aimed to reduce interobserver variability with respect to histopathological diagnosis. Moreover, by excluding patients with polypectomized low-risk T1 cancer and missing data regarding nodal status, patients with neoadjuvant chemotherapy, patients with synchronous or metachronous secondary CRC, as well as patients with competitive invasive cancers originating from other sites if metastatic deposits were not assessed by histology, we tried to control the homogeneity of the study population. Nevertheless, the patients included in this study underwent surgical therapy by multiple surgeons from both academic and community settings. Moreover, adjuvant therapy regimens changed with the introduction of standardised 5-FU-based chemotherapy in 1990. Nonetheless, even with these limitations, our data suggest that pT3 sub-classification is relevant in CRC patients.
In conclusion, pT3 sub-classification using a cut-off value of 5 mm proved to be an independent prognostic parameter in both colon and rectal cancers. In stage II disease, however, no independent influence on outcome was observed. According to our data, pT2 and pT4 sub-classification cannot be currently recommended.
References
Compton CC (2007) Optimal pathologic staging: defining stage II disease. Clin Cancer Res 13:6862s–6870s
Compton CC (2006) Key issues in reporting common cancer specimens: problems in pathologic staging of colon cancer. Arch Pathol Lab Med 130:318–324
Quirke P, Williams GT, Ectors N et al (2007) The future of the TNM staging system in colorectal cancer: time for a debate? Lancet Oncol 8:651–657
Rosen LS, Bilchik AJ, Beart RW Jr et al (2007) New approaches to assessing and treating early-stage colon and rectal cancer: summary statement from 2007 Santa Monica Conference. Clin Cancer Res 13:6853s–6856s
Cawthorn SJ, Parums DV, Gibbs NM et al (1990) Extent of mesorectal spread and involvement of lateral resection margin as prognostic factors after surgery for rectal cancer. Lancet 335:1055–1059
Willett CG, Badizadegan K, Ancukiewicz M et al (1999) Prognostic factors in stage T3N0 rectal cancer: do all patients require postoperative pelvic irradiation and chemotherapy? Dis Colon Rectum 42:167–173
Merkel S, Mansmann U, Siassi M et al (2001) The prognostic inhomogeneity in pT3 rectal carcinomas. Int J Colorectal Dis 16:298–304
Merkel S, Wein A, Günther K et al (2001) High-risk groups of patients with Stage II colon carcinoma. Cancer 92:1435–1443
Steel MC, Woods R, Mackay JM et al (2002) Extent of mesorectal invasion is a prognostic indicator in T3 rectal carcinoma. ANZ J Surg 72:483–487
Shinto E, Ueno H, Hashiguchi Y et al (2004) The subserosal elastic lamina: an anatomic landmark for stratifying pT3 colorectal cancer. Dis Colon Rectum 47:467–473
Harewood GC, Kumar KS, Clain JE et al (2004) Clinical implications of quantification of mesorectal tumour invasion by endoscopic ultrasound: All T3 rectal cancers are not equal. J Gastroenterol Hepatol 19:750–755
Eriksen MT, Wibe A, Haffner J et al (2007) Prognostic groups in 1, 676 patients with T3 rectal cancer treated without preoperative radiotherapy. Dis Colon Rectum 50:156–167
Miyoshi M, Ueno H, Hashiguchi Y et al (2006) Extent of mesorectal tumour invasion as a prognostic factor after curative surgery for T3 rectal cancer patients. Ann Surg 243:492–498
Cianchi F, Messerini L, Comin CE et al (2007) Pathologic determinants of survival after resection of T3N0 (Stage IIA) colorectal cancer: proposal for a new prognostic model. Dis Colon Rectum 50:1332–1341
Wittekind Ch, Greene FL, Henson DE, Hutter RVP (eds) (2003) TNM supplement: a commentary on uniform use, 3rd edn. Wiley-Liss inc., New York
Newland RC, Chapuis PH, Smyth EJ (1987) The prognostic value of substaging colorectal carcinoma. A prospective study of 1117 cases with standardized pathology. Cancer 60:852–857
Newland RC, Dent OF, Chapuis PH et al (1995) Survival after curative resection of lymph node negative colorectal carcinoma. A prospective study of 910 patients. Cancer 76:564–571
Bokey EL, Chapuis PH, Dent OF et al (2003) Surgical technique and survival in patients having a curative resection for colon cancer. Dis Colon Rectum 46:860–866
Burdy G, Panis Y, Alves A et al (2001) Identifying patients with T3–T4 node-negative colon cancer at high risk of recurrence. Dis Colon Rectum 44:1682–1688
Shepherd NA, Baxter KJ, Love SB et al (1997) The prognostic importance of peritoneal involvement in colonic cancer: a prospective evaluation. Gastroenterology 112:1096–1102
Petersen VC, Baxter KJ, Love SB et al (2002) Identification of objective pathological prognostic determinants and models of prognosis in Dukes' B colon cancer. Gut 51:65–69
Chapuis PH, Dent OF, Bokey EL et al (2004) Adverse histopathological findings as a guide to patient management after curative resection of node-positive colonic cancer. Br J Surg 91:349–354
Shepherd NA, Baxter KJ, Love SB (1995) Influence of local peritoneal involvement on pelvic recurrence and prognosis in rectal cancer. J Clin Pathol 48:849–855
Keshava A, Chapuis PH, Chan C et al (2007) The significance of involvement of a free serosal surface for recurrence and survival following resection of clinicopathological stage B and C rectal cancer. Colorectal Dis 9:609–618
Sobin LH, Wittekind C (eds) (1997) TNM classification of malignant tumors, 5th edn. Wiley-Liss inc., New York
Sobin LH, Wittekind C (eds) (2002) TNM classification of malignant tumors, 6th edn. Wiley-Liss inc., New York
Hamilton SR, Vogelstein B, Kudo S (2000) Carcinoma of the colon and rectum. In: Hamilton SR, Aaltonen LA (eds) World Health Organization classification of tumours. Pathology and genetics. Tumours of the digestive system. IARC Press, Lyon, pp 105–119
Chok KS, Law WL (2007) Prognostic factors affecting survival and recurrence of patients with pT1 and pT2 colorectal cancer. World J Surg 31:1485–1490
Losi L, Ponti G, Gregorio CD et al (2006) Prognostic significance of histological features and biological parameters in stage I (pT1 and pT2) colorectal adenocarcinoma. Pathol Res Pract 202:663–670
Cianchi F, Messerini L, Palomba A et al (1997) Character of the invasive margin in colorectal cancer: does it improve prognostic information of Dukes staging? Dis Colon Rectum 40:1170–1175
Cianchi F, Palomba A, Boddi V et al (2002) Lymph node recovery from colorectal tumor specimens: recommendation for a minimum number of lymph nodes to be examined. World J Surg 26:384–389
Krook JE, Moertel CG, Gunderson LL et al (1991) Effective surgical adjuvant therapy for high-risk rectal carcinoma. N Engl J Med 324:709–715
Acknowledgments
The authors are grateful to Ms. A. Kaps for her excellent technical support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pollheimer, M.J., Kornprat, P., Pollheimer, V.S. et al. Clinical significance of pT sub-classification in surgical pathology of colorectal cancer. Int J Colorectal Dis 25, 187–196 (2010). https://doi.org/10.1007/s00384-009-0801-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-009-0801-4