Abstract
Purpose
The purpose of this study was to investigate the prognostic role of distal clearance margin (DCM) in lower rectum cancer surgery.
Materials and methods
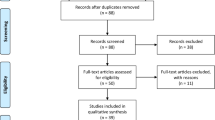
Two-hundred-three cancer patients underwent total rectal resection, possibly followed by adjuvant chemoradiotherapy. DCM was classified as positive or negative (<1, ≥1 cm) and investigated with multivariable proportional hazard models.
Results
A total of 52 deaths, 19 local relapses, 40 distant metastases, and three second primaries were observed as first events. Five-year survival with positive, negative <1, or negative ≥1 cm DCM was 51%, 81%, and 69%, respectively (p = 0.018). The difference was significant between positive and negative DCM (p = 0.031), not between negative <1 and ≥1 cm (p = 0.106). Local and distant 5-year incidences according to DCM were 30%, 8%, and 8% (p = 0.006) and 38%, 26%, and 19% (p = 0.857), respectively.
Conclusions
DCM, but not tumor size, is a prognostic factor after sphincter-saving surgery, which is safe whenever a negative margin is achieved.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
So far, the optimal extent of distal clearance margin (DCM) in rectal cancer surgery is under evaluation.
Despite some positive clinical results demonstrating the adequacy to shrink the DCM under the largely accepted 2 cm [1–4] and the pathological evidence of the limited distal intramural diffusion of rectal cancers [5−7], as documented also in our past experience [8, 9], this topic remains a matter of discussion.
Therefore, we planned to review our patient data affected by cancer located in the lower rectum, in order to evaluate oncologic adequacy of the reduction of DCM and the possibility to perform a sphincter-saving surgery (SSS) in these cases.
Material and methods
Patient characteristics
Six hundred and twenty seven patients were operated on at the Colorectal Cancer Surgery Unit of the National Cancer Institute of Milano, Italy, between 1990 and 2004 for cancers located in the lower part of the rectum. Surgery consisted of total rectal resection (TRR) followed by a coloendoanal anastomosis (CEAA).
The present investigation considered a selected subset of 203 patients not submitted to computed tomography (CT) and/or radiotherapy (RT) before surgery with an adequate follow-up.
Most patients (88%) presented with a primary lesion located within 5 cm from the anal margin. Many of these patients had refused an abdominoperineal resection (APR) in other hospitals and were referred to our unit for a further evaluation and a possible SSS.
The patients were operated on according to standardized criteria of staging and treatment after documenting lack of infiltration in the pelvic floor and anal sphincter as well as the histological absence of disease at the level of distal margin of resection by a frozen section exam during surgery. The surgical approach consisted of TRR extended down to the pelvic floor in combination with a total mesorectum excision (TME) and an abdominopelvic lymphadenectomy and followed by a CEAA. All the procedures were performed strictly according to these modalities by the three senior surgeons of the staff.
On the basis of the histological report, all B2 and C patients (Astler and Coller classification) received CT (Machover in 22 scheme or Folfox schedule in all other cases) and RT (three-field technique of 5,040 cGy) as adjuvant treatment after radical resection.
Surgical technique
We used the surgical technique described by Parks and Percy [10] in 1982, adding a colic reservoir as reported more recently by Lazorthes et al. [11] and described previously in detail [12–14].
The rectum was mobilized off the sacrum using sharp dissection along the parietal pelvic fascias, ensuring en bloc TME according with the technique proposed by Heald [15].
The lateral dissection included sharp dissection of all of the fatty connective tissue and lymphatics surrounding the external and internal iliac vessels, seminal vesicles, superior gluteal, and obturator arteries. This technique allowed en bloc resection of all draining rectal lymphatics with the specimen. The rectum was completely dissected down to the anorectal junction, exposing the levator muscles. The sigmoid colon was divided proximally using a gastrointestinal anastomosis (GIA) stapler. The rectum is sectioned distally just above the pelvic floor.
The remaining sigmoid was then used to prepare a 7-cm-long J-shaped reservoir using a GIA stapler. Afterwards, a complete mucosectomy of the upper anal canal was performed and the reservoir was drawn to the anus and opened; a side-to-end pouch endoanal anastomosis with the external sphincter and anal mucosa was performed using 12–14 interrupted 4/0 resorbable sutures, at the level of the dentate line.
A temporary lateral colostomy on the distal transversum was performed in all patients.
Pathological evaluation
A specific and highly accurate gross pathological evaluation was conducted by a single pathologist (SA) in 175 cases. This allowed us to identify in each specimen a great number of nodes (median 41; range 32–54). In the remaining 28 cases, the macroscopic exam was performed by other pathologists according to standardized and routine criteria (median number of nodes 25; range 19–34).
All specimens were immediately sent to the laboratory and the DCM was measured both on fresh material a few minutes after resection and again after fixation in 4% formalin solution for 24 h. Finally, the extent of DCM was confirmed microscopically measuring its size on histological preparation; this remained the main and conclusive value in case of discrepancy with the macroscopic measurements.
Statistical methods
Analyses mainly focused on the prognostic effect of DCM. The end points were overall survival (OS), local recurrence (LR), and distant metastasis (DM). DM concurrent with LR was analyzed as DM. Time to occurrence of any event was computed from the date of surgery to the date when the event was first recorded or censored at the date of last follow-up assessment in event-free subjects.
The OS curves were estimated by Kaplan–Meier method and plotted in the strata defined by DCM (positive, negative <1 cm, negative ≥1 cm). Comparisons between the Kaplan–Meier curves were carried out by means of the log-rank test. A multivariable Cox model was also performed to analyze the prognostic effect of DCM on OS, including Astler–Coller stage for the purpose of adjustment.
LR and DM were analyzed in a competing-risk framework. In LR (DM) analysis, the following were regarded as competing events: DM (LR), not explained deaths, second primary tumor, whichever occurred first. Descriptive analyses were based on estimating the crude cumulative incidence curves (CCI), which plot the probability of developing an event by a specific time; comparisons between curves were based on the Gray test [16]. Multivariable analyses with the Fine and Gray models [17] were also carried out to investigate the prognostic effect of DCM with adjustment for Astler–Coller stage.
In all the models, DCM and Astler–Coller stage were modeled as categorical covariates by using dummy variables. Checking of the proportional hazard assumption implied by the models relied on the graphical analysis of Schoenfeld residuals [18].
We used SAS™ (SAS Institute Inc., Cary, NC, USA, 2000) and the R software (R Development Core Team (2006). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. ISBN 3-900051-07-0, URL http://www.R-project.org, last access: November 21st 2007) to perform the modeling and statistical calculations. P values are two-sided and we considered as significant P values below the 5% conventional threshold; for all the models, the p values reported are at Wald test.
Results
The main characteristics of the 203 patients are described in Table 1, overall and according to DCM.
Frozen section of distal margin was free of tumor in all cases. However, definitive microscopical exam documented foci of disease at the level of surgical resection line in 25 patients (12%). Nineteen of these patients with positive DCM underwent further surgery (APR plus definitive colostomy) based on this histological feature. In 178 patients, the DCM was tumor free at frozen section and definitive pathological evaluation.
The pathological study documented a DCM lower than 1 cm in about half of the cases (46%) with a negative margin; 35.9% of these were cancer free at the level of regional nodes. A similar distribution was observed in the subset with a DCM above 1 cm.
Among the 175 patients with accurate nodal staging, 117 (66.9%) were N+, including 33 (18.9%) presenting with micrometastases in the regional nodes.
Median follow-up time was 61 months (interquartile range 38–92 months). Table 2 shows the number of events (death for any cause; local relapse and distant metastasis as first events) and the 5-year probability estimates of event occurrence together with the corresponding 95% confidence intervals, according to distal clearance margin. Overall, 52 deaths were observed, 43 of which followed disease recurrence. Nineteen patients developed a local relapse as first event, 40 a distant metastasis, and three a second primary tumor.
The OS curves in distinct DCM groups (Fig. 1) differed significantly (p = 0.019), whereby the subset of patients with positive margins showed a 5-year survival (51%) lower than that in the subsets with negative DCM ≥ 1 cm (69%) or <1 cm (81%), respectively (Table 2). At the multivariable analysis (Table 3), the overall prognostic effect of DCM, adjusted for Astler–Coller stage, was statistically significant (p = 0.018). In particular, for a given stage, the presence of a positive versus negative margin more than doubled the risk of death (hazard ratio, 2.3; p = 0.031), whereas no significant difference was detected between negative DCM < 1 cm versus ≥1 cm (p = 0.106). Astler–Coller stage was also significant (p = 0.008), with a threefold increase of the risk for C1–C2 versus B1–B2 stage (p = 0.017).
Figure 2 shows the CCI curves of local relapse (left panel) and distant metastasis (right panel) according to DCM. The overall comparison between curves yielded a significant result for local relapse (p = 0.004) but not for distant metastasis (p = 0.703). In particular, the curves for negative limited or larger DCM were overlapping for both the end points, whereas a difference was observed for the local relapse curve in patients with positive DCM, the 5-year probability being of local relapse in this group 30% compared to about 8% in patients with negative DCM (Table 2). The multivariable analysis confirmed the above results, indicating a significant overall effect of DCM on local relapse (p = 0.006), due to the difference between positive versus negative DCM (p = 0.002) and not on distant metastasis (p = 0.857). Opposite results were obtained for Astler–Coller stage, which was prognostic for distant metastasis (p < 0.001) and not for local relapse (p = 0.857).
Discussion
The present study is providing data supporting the possibility to reduce the DCM down to 1 cm or less in rectal cancer in order to perform a restorative surgery in those cases where, for technical reason, a greater margin is not achievable.
As a matter of fact, shrinking the extent of surgery represented a main goal in the past years in different areas of surgical oncology. The positive results achieved in many prospective randomized studies allowed the optimization of the treatment and the production of consistent benefits in terms of quality of life for patients affected with different types of cancer such as melanoma [19] or breast malignancies [20].
For low rectal cancers, the possibility to plan a randomized study aimed at validating the use of SSS as an alternative to a APR is limited by practical and ethical reasons.
Anyway, there are different clinical–pathological evidences derived from the recent better definition of the natural history of this disease supporting an extensive use of conservative surgical approaches in the therapy of this peculiar cancer.
It is now clear that rectal cancer is a pelvic disease with a tendency to spread towards perirectal tissue; meanwhile, the distal intramural spreading is an uncommon and limited feature.
This is documented by the rarity of the pathological evidence of disease into the rectal wall under the lower tumor burden [9, 21, 22] and by the relevant role that the mesorectum and its complete removal are now gaining in planning a radical and rational treatment of this cancer [23–26]. The high incidence of local relapse after apparent radical APR, recorded in the past years in many papers [27, 28], compared with the current 3–5% recurrence rate after TME [15] is further confirmation that in many low rectal cancer the extensive demolition of the sphincter and pelvic floor has no biological justification and that the correct dissection of the perirectal structures remains the critical point in attempting cure for this disease.
Based on this observations, some surgeons started to reduce extent of DCM in a series of patients with low rectal cancer demonstrating the adequacy of 1-cm DCM without compromising oncological outcome [1–8]. Most of these studies showed that a smaller DCM does not correlate with high local recurrence rates neither with disease-free and overall survival [2–4, 6] confirming the validity of this approach.
In a previous paper, we have already reported a 3.4% versus a 5% relapse rate for patients having ≤1- or >1-cm DCM in a group of cases including only pN0 patients in order to avoid any bias correlated with major prognostic factors as the spread of disease into the regional nodal basin [8].
The present study confirms these results in a series including both pN0 and pN+ patients and demonstrates that no additional clinical benefit is correlated with a DCM greater than 1 cm. At the same time, a positive distal margin of resection and a positive nodal status remain relevant negative prognostic factors affecting patient final status.
The inclusion in the study of cases never treated before surgery by RT or CT stresses the relevance of the results but it also may suggest the possibility to adopt a conservative approach in those cases obtaining a great downstaging of the primary tumor after preoperative RT–CT for lesions located just above the anorectal ring.
Other studies designed on a prospective basis, if possible, are warranted in the near future on this topic. So far anyway, many findings are demonstrating the safety of this approach whenever a larger DCM is not achievable, remaining that a TME and a radical nodal dissection must be in any case applied.
It is also desirable that further confirmations of these data and a larger diffusion of the concepts of mesorectum, circumferential margin, and distal intramural spreading as well as a better knowledge of the biological history of this disease will allow the refusal of the APR as the golden standard of treatment for the large majority of cancer sited in the lower part of rectum and anorectal area.
References
Guillem JG, Chessin DB, Shia J (2007) A prospective pathologic analysis using whole-mount sections of rectal cancer following preoperative combined modality therapy. Implications for sphincter preservation. Ann Surg 245:88–93
Kuvshinoff B, Maghfoor I, Miedema B (2001) Distal margin requirements after preoperative chemoradiotherapy for distal rectal carcinomas: are < or =1 cm distal margins sufficient. Ann Surg Oncol 8:163–169
Moore HG, Riedel E, Minsky BD (2003) Adequacy of 1-cm distal margin after restorative rectal cancer resection with sharp mesorectal excision and preoperative combined-modality therapy. Ann Surg Oncol 10:80–85
Vernava AM III, Moran M, Rothenberger DA et al (1992) A prospective evaluation of distal margins in carcinoma of the rectum. Surg Gynecol Obstet 175:333–336
Kwok SP, Lau WY, Leung KL et al (1996) Prospective analysis of the distal margin of clearance in anterior resection for rectal carcinoma. Br J Surg 83:969–972
Shirouzu K, Isomoto H, Kakegawa T (1995) Distal spread of rectal cancer and optimal distal margin of resection for sphincter-preserving surgery. Cancer 76:388–392
Paty PB, Enker WE, Cohen AM et al (1994) Treatment of rectal cancer by low anterior resection with coloanal anastomosis. Ann Surg 219:365–373
Andreola S, Leo E, Belli F et al (2001) Adenocarcinoma of the lower third of the rectum surgically treated with a <10-MM distal clearance: preliminary results in 35 N0 patients. Ann Surg Oncol 8:611–615
Andreola S, Leo E, Belli F et al (1997) Distal intramural spread in adenocarcinoma of the lower third of the rectum treated with total rectal resection and coloanal anastomosis. Dis Colon Rectum 40:25–29
Parks AG, Percy JP (1982) Resection and sutured colo-anal anastomosis for rectal carcinoma. Br J Surg 62:301–304
Lazorthes F, Fages P, Chiotasso P et al (1986) Resection of the rectum with construction of a colonic reservoir and colo-anal anastomosis for carcinoma of the rectum. Br J Surg 73:136–139
Leo E, Belli F, Andreola S et al (2004) Sphincter-saving surgery for low rectal cancer. The experience of the National Cancer Institute. Milano Surg Onc 13:103–109
Leo E, Belli F, Andreola S et al (1999) Total rectal resection and complete mesorectum excision followed by coloendoanal anastomosis as the optimal treatment for low rectal cancer. The experience of the National Cancer Institute of Milano. Ann Surg Onc 7:125–132
Leo E, Andreola S, Belli F et al (2001) Sphincter-preserving procedures: the experience of the National Cancer Institute of Milan. Tumori 87:28–30
Heald RJ (1995) Total mesorectal excision is optimal surgery for rectal cancer a Scandinavian consensus. Br J Surg 82:1297–1299
Gray RJ (1988) A class of k-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat 16:1141–1154
Fine JP, Gray RJ (1999) A proportional Hazards model for the subdistribution of competing risk. JASA 94:496–509
Schoenfeld D (1982) Partial residuals for the proportional hazards regression model. Biometrika 69:239–241
Veronesi U, Banfi A, Salvadori B et al (1990) Breast conservation is the treatment of choice in small breast cancer long-term results of a randomised trial. Eur J Cancer 26:668–670
Veronesi U, Cascinelli N, Adamus J (1988) Primary cutaneous melanoma 2 mm or less in thickness. Results from a randomised study comparing wide with narrow surgical excision a preliminary report. N Eng J Med 318:1159–1162
Heald RJ, Moran BJ, Ryall RD et al (1978) Rectal cancer: the Basingstoke experience of total mesorectal excision, 1978–1997. Arch Surg 133:894–899
Heald RJ, Husband EM, Ryall RD (1982) The mesorectum in rectal cancer surgery—the clue to pelvic recurrence. Br J Surg 69:613–616
Heald RJ Ryall RDH (1986) Recurrence and survival after total mesorectal excision for rectal cancer. Lancet 1:1479–1482
MacFarlane JK, Ryall RDH, Heald RJ (1993) Mesorectal excision for rectal cancer. Lancet 341:457–460
Enker WE, Thaler HT, Cranor ML et al (1995) Total mesorectal excision in the operative treatment of rectal cancer. J Am Coll Surg 181:335–346
Havenga K, Enker WE, Norstein J et al (1999) Improved survival and local control after total mesorectal excision or D3 lymphadenectomy in the treatment of primary rectal cancer an international analysis of 1411 patients. Eur J Surg Onc 25:368–374
Karanjia ND, Schache DJ, North WR, Heald RJ (1990) “Close shave” in anterior resection. Br J Surg 77:510–512
Carlsson U, Lasson A, Ekelund G (1987) Recurrence rates after curative surgery for rectal carcinoma, with special reference to their accuracy. Dis Colon Rectum 30:431–434
Acknowledgments
This study was partially supported by the Italian Association for Cancer Research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leo, E., Belli, F., Miceli, R. et al. Distal clearance margin of 1 cm or less: a safe distance in lower rectum cancer surgery. Int J Colorectal Dis 24, 317–322 (2009). https://doi.org/10.1007/s00384-008-0604-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-008-0604-z