Abstract
Aims
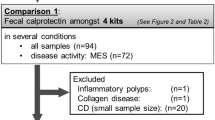
Objective of this study was to compare the assay characteristics of a new fecal calprotectin rapid test with an enzyme-linked immunosorbent assay (ELISA). The second aim was to assess the potential of measuring fecal calprotectin as screening method for intestinal inflammation and colorectal malignancies.
Patients and methods
One hundred forty patients with lower gastrointestinal symptoms referred to colonoscopy provided fecal samples (56, control group; 18, diverticulosis; 29, colorectal adenoma; 8, colorectal carcinoma (CRC); 18, active inflammatory bowel disease (IBD); 11, intestinal infections). Feces were analyzed by two assay methods.
Results
Compared to the control group (median 25.8 µg/g), calprotectin levels were significantly increased in adenoma (66.3 µg/g), CRC (164 µg/g), intestinal infections (306 µg/g), and active IBD (797 µg/g). An adequate diagnostic accuracy could be found for active IBD with a sensitivity, specificity, and an area under the curve (AUC) of 100%, 79%, and 0.955 (ELISA) vs. 89%, 80%, and 0.896 (rapid test). Similar results were obtained for CRC (100%, 79%, 0.922 vs. 100%, 80%, 0.948) whereas in adenomas a low sensitivity, specificity, and AUC of 55%, 79%, and 0.686 vs. 52%, 80%, and 0.666 were found for fecal calprotectin.
Conclusions
Both fecal calprotectin assays are effective in identifying active IBD and CRC but lack analytical sensitivity in separating CRC from adenoma as well as adenoma from the control group. The new calprotectin rapid test is a convenient method for assessing the calprotectin level in an outpatient setting. Henceforth, it provides a precondition for the fecal calprotectin method to challenge fecal occult blood testing in further evaluations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The interest in fecal calprotectin as a noninvasive screening parameter for intestinal inflammation is increasing due to its potential as a clinically relevant marker and valuable diagnostic means in patients with gastrointestinal (GI) symptoms [1]. Fecal calprotectin levels have been reported to be significantly elevated in patients with inflammatory and neoplastic conditions, particularly in active inflammatory bowel disease (IBD) [2–12] and colorectal carcinoma (CRC) [13–20].
Calprotectin is a 36 kDa calcium-binding protein with antimicrobial [21] and antiproliferative [22] properties, which constitutes up to 60% of the cytosolic proteins in neutrophil granulocytes [23] and plays an important role in inflammatory processes [24]. It is excreted in feces and remains stable against bacterial degradation [19]. The presence of calprotectin in feces is a consequence of neutrophils’ migration into the GI tissue. Various pathological conditions of the intestine induce an increased permeability of the mucosa. This leads to an increased migration of granulocytes and monocytes towards chemotactic substances into the bowel [25]. Bacterial components derived from the intestinal lumen act as stimuli for the release of mediators, such as calprotectin, from the cells mentioned above and thus the amount rises in inflammatory states resulting from infections, IBD, or neoplasia [26].
At present, the most widely accepted noninvasive screening method for detecting GI abnormalities is fecal occult blood (FOB) testing. However, as it relies on the occurrence of intestinal bleeding, this method underestimates the incidence of polyps, precancerogenous lesions, and inflammatory diseases, which are not necessarily associated with measurable bleeding [25]. By contrast, calprotectin enters the gut lumen continuously through leukocyte-enriched neoplastic tissues in consequence of an inflammatory process rather than relying on intermittent vascular disruption [27]. Currently, fecal calprotectin can be measured with commercially available enzyme-linked immunoabsorbent assays (ELISA), which are marketed by several suppliers. At present, the method is only used occasionally in the routine diagnostics of clinical laboratories. The dispatch of stool samples to a clinical laboratory represents a logistical challenge for the office-based gastroenterologist attending to outpatients. Therefore, a simple semiquantitative rapid test for fecal calprotectin has been developed. The objective of this development was to provide a method for a rapid and facile measurement of fecal calprotectin which can be applied in the outpatient setting. This would feature an indispensable precondition to challenge the esteemed FOB method, which is well accepted by patients and gastroenterologists due to its noninvasive, rapid, and cheap performance, in a large multicenter trial.
The purpose of this study was to evaluate the diagnostic accuracy of the new calprotectin rapid test compared to an established ELISA test in detecting colonoscopy-proven intestinal inflammatory diseases and colorectal malignancies as well as to assess the potential of measuring fecal calprotectin as screening marker for those malignancies.
Patients and methods
Patients
The study was conducted as an open multicenter case control trial with 140 patients referred to colonoscopy. Samples were collected in the gastroenterological departments of the following hospitals: Katharinenhospital, Karl-Olga-Hospital, Robert-Bosch-Hospital, and in three outpatient gastroenterologies, all of them based in Stuttgart, Germany.
The patients enrolled in this study were at least 18 years old and underwent colonoscopy according to a medical indication (gastrointestinal disorders) or for CRC screening–preventive medical checkup. Exclusion criteria were known extraintestinal inflammatory diseases such as rheumatoid arthritis, chronic arthritis–sinusitis, and urinary tract infection. Patients whose medical history included nonsteroidal anti-inflammatory drugs or anticoagulants have also been excluded as these agents have been reported to cause increased fecal calprotectin levels due to enteropathy [28, 29]. However, fecal calprotectin of the specimens of those patients were also measured as they allow the comparison of the rapid test with a calprotectin ELISA. A total of 140 patients (62 male, 78 female, mean age 58 years, range 20–85) referred to colonoscopy for clarification of lower GI symptoms (n = 50), altered bowel habit (n = 10), weight loss (n = 3), by reason of occult blood–rectal bleeding (n = 22), search of tumor (n = 6), resectional surgery (n = 3), follow-up (n = 29), or routine checkup (n = 17) were included. In a case report form, each patient’s medical history and results of the endoscopic examination were recorded by the responsible physician. Patients with normal diagnostic findings (n = 56) were assigned to the control group (group 0), whereas the remaining 84 patients were grouped into five groups according to the colonoscopic and histological findings: diverticulosis (group I), colorectal adenoma (group II), CRC (group III), active IBD (group IV), and intestinal infections (group V; Table 1).
The protocol was approved by the local ethical committee and conducted in accordance to the Declaration of Helsinki. Informed consent was obtained from every participant. In a subsequent amendment, the possibility was admitted to include patients with known active IBD and no requirement for colonoscopy, confirmed by other means such as sonography.
Methods
Patients provided a single stool sample of 10–20 g for calprotectin measurement before the bowel was prepared for colonoscopy. Outpatients were asked to keep samples refrigerated and to return them within 24 h. Specimens were stored in screw-capped plastic containers and were labeled in a pseudonymized manner upon receipt.
Although the stability of calprotectin up to 1 week at room temperature has been reported [1, 12, 27], a cold chain was maintained for all samples throughout. Upon receipt, samples were stored at +4°C in the hospitals or outpatient gastroenterologies and shipped in an insulated box to the central laboratory within the next 6 days. Specimens were preserved at −20°C and assayed within the next 3 months. As calprotectin is a remarkably stable protein [25, 28], this delay in testing is not anticipated to affect the results. Calprotectin was quantified using two methods from the same extract:
-
1.
An improved commercial quantitative calprotectin (MRP8/14) ELISA kit, Bühlmann Laboratories AG (Schönenbuch, Switzerland) and
-
2.
A new semiquantitative calprotectin rapid test (Prevista GmbH & Co KG, Munich, Germany), the details of which are described below.
The samples were extracted by using a commercial fecal sample preparation kit (Roche Diagnostics GmbH, Mannheim, Germany), which allowed the samples to be handled in a hygienic manner.
After thawing, single aliquots of 50 mg were suspended in 2.5 ml of extraction buffer (B-Cal-Ex, Bühlmann Laboratories AG, Schönenbuch, Switzerland) in the sample preparation tubes and homogenized for 2 min with a Vortex mixer. For performance of the ELISA, we followed the manufacturer’s instructions. After centrifugation of the extract for 5 min at 10,000 rpm, the supernatant was diluted 1:50 with incubation buffer. A 100-μl sample was pipetted in duplicate into the antibody-covered wells of the microtiter plates. After 30-min incubation at room temperature, washing was followed by the addition of 100 μl of enzyme label and 30-min incubation and after subsequently adding 100-μl substrate and incubation at room temperature for 15 min in a dark place the optical density values were read at 450 nm. Calprotectin was expressed as micrograms per gram feces.
The same fecal extract was assayed with the calprotectin rapid test which is a chromatographic immunoassay. The centrifugation step can be elided for routine use and was only applied to provide uniform samples for comparison between the ELISA and the rapid test. The test device, a lateral flow test, has a test line and a control line. The test line contains anti-calprotectin monoclonal antibodies and the control line contains anti-immunoglobulin antibodies both of which have been dried on the membrane. Gold-conjugated anti-calprotectin antibodies are dried on the conjugate pad. The sample is dripped on the conjugate pad where the gold-labeled anti-calprotectin antibodies bind to the calprotectin from the sample. The labeled sample migrates across the membrane via capillary action. Once the sample passes the test line, the gold-labeled calprotectin samples are bound by the immobilized line of anti-calprotectin antibodies. Excess labeled antibodies migrate beyond the test line to the control line where they are immobilized by the anti-immunoglobulin antibodies. The presence of the control line indicates that the sample has passed the test line.
To perform the assay, 25 µl of the extracted sample followed by 75 µl of the running buffer were pipetted on the conjugate pad and the assay was allowed to incubate for 10 min. The results were read within the next 5 min and documented with a digital camera. The intensities of the test line were appraised with an ordinal scaling spanning from 0 to 5 for a better comparison with the quantitative ELISA values and statistical analyzes (Fig. 1). All analyzes have been performed by the same person who was blinded to the clinical diagnosis and to the results of the ELISA test. To minimize the interobserver variability, sample analyses were carried out accumulated for comparative interpretation of the test line.
Statistics
Statistical analysis of calprotectin levels and intensities of the test lines between groups were performed using the nonparametric Mann–Whitney test as the results were not normally distributed. To compare the two tests, results have been correlated according to Spearman and the χ 2 test was performed. Parameters of test reliability, including sensitivity and specificity, and negative and positive predictive value were calculated with the results of both methods. In accordance with previous studies, the cutoff for the ELISA test was defined to be 50 µg/g in coincidence with the cutoff value for the rapid test chosen by the manufacturer. All values have also been calculated for the cutoff 100 µg/g but have been disapproved in terms of using the calprotectin method as a screening test which requires a high sensitivity. Receiver operator characteristics (ROC) curves (plot of “sensitivity” against “1 minus specificity” at different levels of calprotectin) including all study groups with intestinal diseases (II–V) and for each study group separately have been constructed. Areas under the curves (AUC) were calculated to compare the diagnostic accuracy of the two methods.
All statistics were performed using GraphPad Prism, version 4, for Windows.
Results
In comparison to the control group (group 0; median 25.8 µg/g, 25–75% percentile, 16.3–42.3 µg/g), calprotectin levels were significantly increased in patients with adenoma (group II; 66.3 µg/g, 24.3–137 µg/g, p = 0.005 ELISA, p = 0,002 rapid test), CRC (group III; 164 µg/g, 125–491 µg/g, p < 0.001 both methods), active IBD (group IV; 797 µg/g, 160–1,752 µg/g, p < 0.001 both methods), and intestinal infections (group V; 306.2 µg/g, 45–815 µg/g, p = 0.002 ELISA, p < 0.001 rapid test). In active IBD, there was no difference found in fecal calprotectin levels of patients with Crohn’s disease (CD; group IVa; 541 µg/g, range 70–2899 µg/g, n = 9) and those having ulcerative colitis (UC; group IVb; 648 µg/g, range 92–1754 µg/g, n = 9). In patients with diverticulosis (group I; 43.8 µg/g, 17.3–61.0 µg/g, p = 0.313 ELISA, p = 0.871 rapid test), calprotectin concentrations did not significantly differ from the control group and were below the reference level of 50 µg/g [29]. Both test methods provided similar results (Fig. 2a,b).
a Log fecal calprotectin concentration [µg/g] measured by calprotectin ELISA in the different diagnostic groups. Median values with 25% and 75% percentile are shown. Except diverticulosis (p = 0.313), all diagnostic groups differed significantly from controls (adenoma p = 0.005, carcinoma p < 0.001, active IBD p < 0.001, intestinal infection p = 0.002). The dotted line shows the cutoff 50 µg/g. b Appraisement of the intensity of the test line with a scale from 0 to 5 using the calprotectin rapid test in the different diagnostic groups. Median values with 25% and 75% percentile are shown. All diagnostic groups differed significantly from controls (adenoma p = 0.002, carcinoma p < 0.001, active IBD p < 0.001, intestinal infection p < 0.001), except diverticulosis (p = 0.871). The dotted line shows the cutoff for normality. c Correlation of the line intensity of the new calprotectin rapid test with the values [µg/g] measured with a conventional calprotectin ELISA test. N = 140, Spearman correlation coefficient r = 0.862, p < 0.001
Percentage positivity rates of the ELISA test and the rapid test for the study groups are shown in Table 2. Twenty-one percent (ELISA) vs. 20% (rapid test) out of the control group turned out to have false positive results. In the diverticulosis group, only 22% (both methods) had elevated levels of calprotectin. In the adenoma group, 55% (ELISA) vs. 52% (rapid test) of the patients could be identified but all patients diagnosed with CRC by colonoscopy and histology had positive test results with both methods. An equivalent positivity rate of 100% was obtained in patients with active IBD determined with the ELISA method, whereas the rapid test yielded in a slightly lower positivity rate (89%) as calprotectin was falsely negative in two patients. Intestinal infection could be identified in 64% (both methods) of the cases.
Correlation of the line intensity of the rapid test with the calprotectin values of the ELISA test was highly significant (r = 0.862, p < 0.001) and both methods were found to be homogenous (χ 2 = 106.71, p < 0.001; Fig. 2c).
Table 3 summarizes the overall performance of the two tests and their positive predictive value, negative predictive value (NPV), sensitivity, specificity, and AUC of the ROC analysis.
The cutoff of 50 µg/g resulted in unsatisfactory prediction of diagnosis in the adenoma group. Clear results were obtained for CRC and active IBD (NPV and sensitivity 100%) by both test methods, except results of IBD patients determined with the rapid test, which have been slightly lower (NPV 96%, sensitivity 89%) as calprotectin was falsely negative in two patients.
The clinical utility of the two methods was compared in ROC curves for overall intestinal disease, adenoma, CRC, and active IBD (Fig. 3). Measurement of fecal samples resulted in a high clinical utility for CRC and IBD (Table 3). For overall intestinal diseases, AUC values were 0.808 (ELISA) vs. 0.783 (rapid test) whereas the ROC curve of the adenoma group showed an inadequate AUC. Evaluating the data of the ROC analyses, the conventional ELISA method was slightly better than the new rapid test likely because of the imprecise ordinal scaling of the rapid test compared to the quantitative calprotectin measurement of the ELISA test.
Receiver operator curve for fecal calprotectin determined by a new rapid test and a conventional ELISA test in detecting patients with a overall intestinal diseases, b adenoma, c carcinoma, and d active IBD. All curves are statistically significant (a, c, d: p < 0.001, b: p < 0.01) with the area beneath them being greater than 50%
Discussion
Fecal calprotectin has been proposed as a marker of increased GI permeability in inflammation. This study demonstrates the usefulness of fecal calprotectin for detection of colonic inflammation occurring in the course of IBD. We used 50 µg/g as a reasonable reference value for the cutoff between normal and pathologic as proposed in earlier clinical studies employing calprotectin as a screening marker [20, 30]. This cutoff level was chosen by the manufacturer of the rapid test and found to be optimal in the present study as confirmed by the ROC data. All patients with active IBD as assessed by colonoscopy had a fecal excretion of calprotectin greater than 50 µg/g and all except two had clearly positive results in the rapid test. In the case of those two patients, intestinal inflammation was moderate and the calprotectin values obtained by the ELISA test were only slightly above the cutoff level.
One of the diagnostic challenges in clinical gastroenterology is differentiating patients with endoscopically identifiable “organic disease” such as inflammation or malignancies from “functional disorders” such as irritable bowel syndrome (IBS) since both groups of diseases share many clinical symptoms. It is known that levels higher than 50 µg/g but lower than 100 µg/g can be detected in patients with functional symptoms. Moreover, in such cases, the possibility of day-to-day variations has to be considered as shown by a study in which intraindividual biological variability of fecal calprotectin was found on repeated assessments in 64% of the patients without neoplasm or inflammation [31]. However, in the present study, active IBD was well predicted by the calprotectin measurement and the high sensitivity and specificity indicate that the calprotectin test is useful in differentiating patients with active IBD from those with IBS belonging to the “control group.” Considering a false positive result of a patient with functional symptoms, we suggest that the lower cutoff at the level of 50 µg/g is suitable for a screening test as the purpose of the test is to identify patients who deserve further monitoring or examination.
It was previously reported that fecal calprotectin is elevated in active IBD but not in quiescent IBD with no obvious inflammatory state [2, 5, 8, 9]. The calprotectin test has potential to differ whether clinical symptoms in patients with known IBD are caused by acute episodes or noninflammatory complications underlying IBS. However, von Roon et al. [32] reasoned that while this finding is likely to be affirmed for patients with severe IBD it is not feasible for patients with low probability of IBD and “mild functional-like symptoms.”
In our study, we could not find any differences between calprotectin levels in active CD and active UC. Higher levels have been reported to be preferably found in patients with CD than in those with UC [12, 32]. However, the calprotectin levels may not only depend on disease type but also on organic location. As stated by Tibble et al. [33], it is likely that this finding is of clinical significance because the range of calprotectin values in both CD and UC is wide and the test is thus not useful for a differential diagnosis.
In this study, we show that the calprotectin method is not applicable for detecting diverticulosis since the values of those patients were below the reference value and showed poor parameters of test reliability. As long as diverticulosis does not progress into diverticulitis, the anatomical changes of the mucosa do not increase the migration of neutrophils into the gut lumen.
Interestingly, we were able to identify CRC with a sensitivity of 100% with both test methods and to show a high diagnostic accuracy for this condition. Recruitment of neutrophils to the tumor is probably due to the local production of chemotactic factors [15, 18, 19] provoking an exudative response. However, other studies showed contradictory results and even described fecal calprotectin as a poor marker for the detection of CRC [16, 31]. The difference of our results compared to the cited studies might be explained by the small sample size of patients with CRC (n = 8) in this study. CRC is associated with a local acute inflammatory reaction [19], probably of variable intensity, and therefore may not be uniformly characterized by significant neutrophilic infiltrate. Nevertheless, the sensitivity and specificity of calprotectin in CRC we found were similar to those in several previous reports [18, 14, 19, 26]. In accordance to the studies cited above, the present study confirms a satisfactory specificity and sensitivity of calprotectin as a marker in a high-risk population for endoscopically confirmed GI disorders. The neutrophil infiltrate in the neoplastic tissues is discussed to be a function of volume of the neoplasm [34] and therefore the calprotectin test could underdiagnose early malignancies when used as a screening test in a symptomless population. Based on the findings of a relatively low sensitivity (55% ELISA, 52% rapid test) and specificity (79%, 80%) and an inadequate AUC in the diagnosis of adenomas, fecal calprotectin cannot be recommended as a screening test for precancerogenous lesions for normal-risk individuals. Four studies have utilized FOB alongside fecal calprotectin as screening marker [16, 19, 35, 36]. The comparative sensitivity of the FOB test for colorectal neoplasia was found to range from 3% to 43% with higher specificity at 90–97% [32]. However, the sensitivity and specificity of the calprotectin test of 52–55% and 79–80% for adenomas and 62–65% and 79–80% for adenomas and CRC as a combined group, which are shown in this study and also found in previous studies [19, 35, 36], indicate that while neither test is ideal for CRC screening the fecal calprotectin test appears to be superior to the FOB test. Calprotectin, also present in blood, enters the bowel lumen continuously as part of an inflammatory process rather than a result of intermittent bleeding from the tumor and may therefore be advantageous to the FOB test as adenomatous polyps often do not bleed [19]. So far, considering fecal calprotectin testing as alternative to FOB testing was beyond question, due to the comparatively more expensive and time-consuming performance. D’ Inca et al. [34] expressed recently the necessity for a spot test for fecal calprotectin without any extraction process for everyday use in unselected patients with lower GI symptoms. The new validated calprotectin rapid test is advantageous in the performance compared with the ELISA method. Results could be read in about 10 min, whereas the performance of the ELISA test required approximately 3–4 h. Moreover, no special equipment is needed. The rapid test is a suitable alternative for the ELISA test. For gastroenterologists working mainly with outpatients processing only small sample numbers and requiring fast results, this method is cost-efficient in the daily evaluation of clinical cases and outpatients. In respect to the intraobserver variability, using an ordinal scale for the appraisement of the line intensity cannot be recommended. In the routine diagnostic, the rapid test should rather be used as a qualitative test, giving an indefinite direction of the severeness of the GI inflammation. As the test is considered to be used as a screening test, which requires further diagnostic examination when a result is positive, this should not pose a drawback.
Although calprotectin as a nonspecific test for all organic intestinal diseases in general (groups II–IV) is less sensitive (77% ELISA, 72% rapid test) than testing separately for IBD and CRC, it is still a useful screening test. Fagerberg et al. [37] concluded that a negative test indicates a low probability of mucosal inflammation. Other diagnoses may be considered first if the patient has uncertain symptoms. A positive test will help to decide in proceeding with endoscopy and prioritizing those patients as they are likely to be urgent cases.
Fecal calprotectin as a diagnostic test to distinguish organic from functional disorders may be interesting to reduce invasive procedures such as colonoscopy.
In conclusion, the study confirmed that both fecal calprotectin assays accurately identify active IBD and CRC. Fecal calprotectin was not found to be an adequate marker for diverticulosis. Fecal calprotectin was a poor marker for separating CRC from adenoma as well as adenoma from the control group. It is therefore not ideal as a screening marker for all colorectal proliferative disorders. On the other hand, it is likely to be advantageous to the presently recommended FOB test and should be considered as a valuable alternative that deserves further evaluation. With the new developed calprotectin rapid test, a possibility comes up to realize this method quickly and with small efforts in the clinical and outpatient routine diagnostics. A large multicenter trial is needed to test the herewith validated calprotectin rapid test alongside FOB testing.
References
Gearry R, Barclay M, Florkowski C, George P, Walmsley T (2005) Faecal calprotectin: the case for a novel non-invasive way of assessing intestinal inflammation. NZMJ 118:1444–1451
Carroccio A, Iacono G, Cottone M, Di Prima L, Cartabellotta F, Cavataio F et al (2003) Diagnostic accuracy of fecal calprotectin assay in distinguishing organic causes of chronic diarrhea from irritable bowel syndrome: a prospective study in adults and children. Clin Chem 49:861–867
Costa F, Mumolo MG, Ceccarelli L, Bellini M, Romano MR, Sterpi C et al (2005) Calprotectin is a stronger predictive marker of relapse in ulcerative colitis than in Crohn’s disease. Gut 54:364–368
Gaya D, Mackenzie JFR (2002) Faecal calprotectin: a bright future for assessing disease activity in Crohn’s disease. Q J Med 95:557–558
Limburg PJ, Ahlquist DA, Sandborn WJ, Mahoney DW, Devens ME, Harrington JJ et al (2000) Fecal calprotectin levels predict colorectal inflammation among patients with chronic diarrhea referred for colonoscopy. Am J Gastroenterol 95:2831–2837
Poullis A, Foster R, Northfield TC, Mendall MA (2002) Review article: faecal markers in the assessment of activity in inflammatory bowel disease. Aliment Pharmacol Ther 16:675–681
Røseth AG, Schmidt PN, Fagherol MK (1999) Correlation between faecal excretion of indium-111-labelled granulocytes and calprotectin, a granulocyte marker protein, in patients with Inflammatory bowel disease. Scand J Gastroenterol 34:50–54
Røseth AG, Aadland E, Grzyb K (2004) Normalization of faecal calprotectin: a predictor of mucosal healing in patients with inflammatory bowel disease. Scand J Gastroenterol 39:1017–1020
Tibble J, Teahon K, Thjodleifsson B, Roseth A, Sigthorsson G, Bridger S et al (2000) A simple method for assessing intestinal inflammation in Crohn’s disease. Gut 47:506–513
Tibble JA, Sigthorsson G, Bridger S, Fagerhol MK, Bjarnason I (2000) Surrogate markers of intestinal inflammation are predictive in relapse in patients with inflammatory bowel disease. Gastroenterology 119:15–22
Tibble JA, Bjarnason I (2001) Non-invasive investigation of inflammatory bowel disease. World J Gastroenterol 7:460–465
Vermeire S, Assche G, Rutgeerts P (2006) Laboratory markers in IBD: useful, magic or unnecessary toys? Gut 55:426–431
Johne B, Kronborg O, Tøn H, Kristinsson J, Fuglerud P (2001) A new faecal calprotectin test for colorectal neoplasia. Clinical results and comparison with previous methods. Scand J Gastroenterol 36:291–296
Tibble JA, Sigthorsson G, Bridger S, Fagerhol MK, Bjarnason I (1998) Fecal calprotectin concentration in patients with colorectal carcinoma. Dis Colon Rectum 41:316–321
Kristinsson J, Armbruster CHR, Ugstad M, Kriwanek S, Nygaard K, Ton H et al (2001) Fecal excretion of calprotectin in colorectal cancer: relationship to tumor characteristics. Scand J Gastroenterol 36:202–207
Limburg PJ, Devens ME, Harrington JJ, Diehl NN, Mahoney DW, Ahlquist DA (2003) Prospective evaluation of fecal calprotectin as screening biomarker for colorectal neoplasia. Am J Gastroenterol 98:2299–2305
Poullis A, Foster R, Shetty A, Fagherol MK, Mendall MA (2004) Bowel inflammation as measured by fecal calprotectin: a link between lifestyle factors and colorectal cancer risk. Cancer Epidemiol Biomark Prev 13:279–284
Roseth AG, Kristinsson J, Fagerhol MK, Schjonsby H, Aadland E, Nygaard K et al (1993) Fecal calprotectin: a novel test for the diagnosis of colorectal cancer? Scand J Gastroenterol 28:1073–1076
Tibble J, Sigthorsson G, Foster R, Sherwood R, Fagherol M, Bjarnason I (2001) Faecal calprotectin and faecal occult blood tests in the diagnosis of colorectal carcinoma and adenoma. Gut 49:402–408
Kronborg O, Ugstad M, Fuglerud P, Johne B, Hardcastle J, Scholefield JH et al (2000) Faecal calprotectin levels in a high risk population of colorectal neoplasia. Gut 46:795–800
Steinbakk M, Naess-Andresen CF, Lingaas E, Dale I, Brandtzaeg P, Fagerhol MK (1990) Antimicrobial actions of calcium binding leucocyte L1 protein, calprotectin. Lancet 336:763–765
Yui S, Mikami M, Tsurumaki K, Yamazaki M (1997) Growth inhibitory and apoptosis inducing activities of calprotectin derived from inflammatory exudate cells on normal fibroblasts: regulation by metal ions. J Leukoc Biol 61:50–57
Fagherol MK, Andersson KB, Naess-Andresen CF, Brandtzaeg P, Dale I (1990) Calprotectin (the L1 leucocyte protein). In: Smith VL, Dedman JR (eds) Stimulus response coupling: the role of intracellular calcium-binding proteins. CRC, Boca Raton, pp 187–210
Brun JG, Ulvestad E, Fagherol MK, Jonsson R (1994) Effects of human calprotectin (L1) on in vitro immunoglobulin syntheses. Scand J Immunol 40:675–680
Johne B, Fagerhol MK, Lyberg T, Prydz H, Brandtzaeg P, Naess-Andresen CF et al (1997) Functional and clinical aspects of the myelomonocyte protein calprotectin. J Clin Pathol 50:113–123
Summerton CB, Longlands MG, Wiener K, Shreeve DR (2002) Faecal calprotectin: a marker of inflammation throughout the intestinal tract. Eur J Gastroenterol Hepatol 14:841–845
Røseth AG, Fagherol MK, Aadland E, Schjonsby H (1992) Assessment of the neutrophil dominating protein calprotectin in feces. Scand J Gastroenterol 27:793–798
Tibble JA, Sigthorsson G, Foster R, Fagherol MK, Røseth A, Bjarnasson I (1999) High prevalence of NSAID enteropathy as shown by a simple faecal test. Gut 45:362–366
Tibble JA, Sigthorsson G, Foster R et al (1998) NSAID enteropathy: a new simple diagnostic test. Gut 42:142
Fagherol MK (2000) Calprotectin, a faecal marker of organic gastrointestinal abnormality. Lancet 356:1783–1784
Husebye E, Tøn H, Johne B (2001) Biological variability of fecal calprotectin in patients referred for colonoscopy without colonic inflammation or neoplasm. Am J Gastroenterol 96(9):2683–2687
von Roon CA, Karamountzos L, Purkayastha S, Reese GE, Darzi AW, Teare JP et al (2007) Diagnostic precision of fecal calprotectin for inflammatory bowel disease and colorectal malignancy. Am J Gastroenterol 102:1–11
Tibble JA, Sigthorsson G, Foster R, Forgacs I, Bjarnason I (2002) Use of surrogate markers of inflammation and Rome criteria to distinguish organic from non-organic intestinal disease. Gastroenterology 123:450–460
D’Incà R, Dal Pont E, Di Leo V, Ferronato A, Fries W, Vettorato MG et al (2007) Calprotectin and lactoferrin in the assessment of intestinal inflammation and organic disease. Int J Colorectal Dis 22:429–437
Kristinsson J, Nygaard K, Aadland E, Barstad S, Sauar J, Hofstad B et al (2001) Screening of first degree relatives of patients operated for colorectal cancer: evaluation of fecal calprotectin vs. hemoccult II. Digestion 64:104–110
Hoff G, Grotmol T, Thiis-Evensen E, Bretthauer M, Gondal G, Vatn MH (2004) Testing for faecal calprotectin (PhiCal) in the Norwegian Colorectal Cancer Prevention trial on flexible sigmoidoscopy screening: comparison with an immunochemical test for occult blood (FlexSure OBT). Gut 53:1329–1333
Fagerberg UL, Lööf L, Myrdal U, Hansson L-O, Finkel Y (2005) Colorectal inflammation is well predicted by fecal calprotectin in children with gastrointestinal symptoms. JPGN 40:450–455
Acknowledgements
The authors gratefully acknowledge the excellent assistance of Prof. W. Zoller, MD, A. Schreiber, MD, (Katharinenhospital), E. Fröhlich, MD, M. Schmidt, MD, (Karl-Olga-Hospital), Prof. E. Stange, MD, (Robert-Bosch-Hospital), H. Gölkel, MD, Th. Bühler MD, Prof. B. Klump, MD, K. Teubner, MD, D. Vogler, MD, A. Maier, MD, and A. Mühlhöfer, MD, in recruiting patients and kindly providing samples.
Author information
Authors and Affiliations
Corresponding author
Additional information
Support for analytical kits: Prevista GmbH & Co. KG, Munich, Germany.
Rights and permissions
About this article
Cite this article
Damms, A., Bischoff, S.C. Validation and clinical significance of a new calprotectin rapid test for the diagnosis of gastrointestinal diseases. Int J Colorectal Dis 23, 985–992 (2008). https://doi.org/10.1007/s00384-008-0506-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-008-0506-0