Abstract
Background
Standard therapy for locally advanced rectal cancer (LARC) is concurrent neo-adjuvant chemo-radiation using infusional 5-fluorouracil (CIV-5-FU). Capecitabine (CAP) offers a convenient oral replacement for CIV-5-FU. There is no randomized trial comparing infusional 5-FU to capecitabine. We retrospectively compared the safety and efficacy of CAP-based regimens with well-established CIV-5-FU-based regimens in LARC.
Materials and methods
We collected published data on 542 patients treated on either CIV-5-FU (197) or CAP (345) with concurrent radiation (external radiation treatment, XRT) for LARC. This included Phase I or II studies published or available from Pubmed. Safety was assessed by determining proportion of patients who experienced grade III/IV adverse effects. Efficacy was assessed by determining pathological complete response (pCR). Chi-square tests were used to compare the two regimens. A P value less than 0.05 was considered statistically significant. Statistical tests were further corrected for multiplicity using the method of Benjamini and Yekutieli (Ann Stat, 29(4):1165–1188, 2001).
Results
pCR was significantly higher in patients getting CAP vs CIV-5-FU (25 vs 13%; P = 0.008,.P adj = 0.034). Both regimens were generally well tolerated. There was no grade IV toxicity reported. Grade III hand foot syndrome was more common in the CAP group, and grade III diarrhea was more common in the CIV group.
Conclusions
CAP when compared to CIV seems to have superior efficacy with reasonable toxicities. It is reasonable to treat LARC with CAP + XRT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2007, approximately 41,420 patients will be diagnosed with rectal cancer in the USA [1]. In patients with locally advanced rectal cancer (T3, T4, or N1), neoadjuvant chemoradiation has now become a standard based on German Rectal Cancer Study [2]. Data from German Rectal Cancer Group indicate that preoperative chemo-external radiation treatment (XRT) may be a potentially better approach to this disease than postoperative radiation, both in terms of local control and reduced toxicity. Continuous intravenous infusion 5-fluorouracil (CIV-5-FU) or bolus 5-FU has been the standard chemotherapy with radiation (XRT) in locally advanced rectal cancer. Capecitabine is an oral fluoropyrimidine carbamate prodrug of 5-FU, designed to closely simulate infusional administration of 5-FU [20]. This oral drug does not only provide a convenient method of administration with reduced toxicity [4], but it improves therapeutic index because of more selective drug delivery to tumors secondary to higher expression of thymidylate phosphorylase (the enzyme responsible for capecitabine conversion to its active form) in tumor tissue when compared to corresponding normal tissue [3].
These factors generated the need to investigate the replacement of 5-FU in many cancers including in the neoadjuvant treatment for rectal cancer.
In a recent retrospective study, Cole et al. [5] assessed the safety profile of capecitabine- vs infusion 5-FU-based regimen in 3,224 patients (1,409 vs 2,825, respectively) in phase II or III studies for first- or second-(or later) line therapy for colorectal cancer. Capecitabine-based regimens were associated with significantly lower incidences of: grade III or IV hematological toxicity (3.4 vs 16.3%, P < 0.0001, P adj < 0.001), grade III or IV neutropenia (4.8 vs 27.7%, P < 0.0001, P adj < 0.001), neutropenic fever (1.2 vs 7.7%, P < 0.0001, P adj < 0.001), thrombocytopenia (2.3 vs 4.8%, P = 0.003, P adj < 0.015), and marginally significantly lower anemia (2.6 vs 4.6%, P = 0.018, P adj = 0.057). Hand–foot syndrome (HFS) was observed more frequently in patients treated with capecitabine-based rather than infusion 5-FU-based therapies (9.3 vs 6.3%, P < 0.01, P adj < 0.036). In addition, CIV therapies require an indwelling catheter and ancillary care and can lead to infections and thrombosis. Therefore, it can potentially raise the costs and affects of patient quality of life. In an interview-based questionnaire of 103 patients with incurable cancer who were likely to receive palliative chemotherapy in the future, 89% preferred oral over intravenous chemotherapy. The main reasons included convenience (57%), problems with intravenous lines (55%), and preference for home-based therapy (33%) [6].
Currently, there are no published phase III trials comparing capecitabine-based therapies with CIV-5-FU-based therapies as neoadjuvant therapy in LARC.
In this article, we will evaluate the efficacy and safety data in the literature comparing both treatment regimens in the neoadjuvant therapy for LARC.
Materials and methods
A Medline search was made for papers and abstracts published in the English language concerning phase I and II studies of neoadjuvant treatment for locally advanced rectal cancer between 1996 and 2006. The National Cancer Institution toxicity criteria were used to evaluate toxicity and safety. Many measures were used to evaluate efficacy. Studies were grouped according to the treatment regimen and were discussed separately.
A retrospective pooled analysis was carried on using data from phase I/II studies. Patients who were treated with either CIV-5-FU with radiation or capecitabine with radiation were compared using Chi-square tests. A P value less than 0.05 was considered statistically significant. Statistical tests were further corrected for multiplicity.
Results
We collected published data on 542 patients treated with either CIV-5-FU (197) or CAP (345) with concurrent radiation (XRT) for LARC. Different treatment schedules were used: concurrent continuous infusion 5-FU alone or with other chemotherapy plus radiation and concurrent oral capecitabine with or without other chemotherapy plus radiation. Safety was assessed by determining proportion of patients who experienced grade III/IV adverse effects. Efficacy was assessed by pathological complete response (pCR) and sphincter preservation (SP).
Continuous infusion 5-FU with radiotherapy
A large number of retrospective and prospective studies have used the combination of 5-FU and XRT in the treatment of gastrointestinal malignancies. 5-FU has been used as continuous or bolus infusion. Radiation-sensitizing effects of 5-FU are maximal when exposure to 5-FU occurs for at least 24 h and up to 48 h after radiotherapy exposure [7]. A survival advantage has been reported in using continuous compared to bolus 5-FU during radiation in the adjuvant treatment of resected rectal cancer [8].
A small nonrandomized prospective study compared CIV-5-FU (22 patients) to bolus 5-FU (12 patients) with concurrent radiation in neoadjuvant preoperative treatment for LARC [14]. Patients received preoperative radiotherapy concurrent with either bolus 5-FU (on days 3 to 5 and 28 to 33 of radiation) or infusional 5-FU (225 mg/m2 daily for the duration of radiation). Pathologic CR was observed in 2 of 21 (10%) patients treated with bolus 5-FU as compared to 8 of 12 (67%) for patients treated with CIV-5-FU [20]. Treatment was generally well tolerated. Four patients had to have their chemotherapy interrupted because of mucositis, two patients were in the CIV group, and two patients in the bolus 5-FU group. Two patients developed cystitis, one in each group. There was no difference in overall survival between the CIV and 5-FU group (84 vs 74% P = 0.14, P adj = 0.396).
Based on these results, multiple trials have used CIV-5-FU alone or in combination with other agents plus XRT in the neoadjuvant treatment of LARC (Tables 1 and 2).
In a nonrandomized prospective trial, 117 patients with LARC were treated preoperatively with concurrent 45 Gy in 25 fractions over 5 weeks with continuous infusion 5-FU (300 mg/m2 per day) [9]. Overall, a sphincter-saving (SP) procedure was possible in 59% of patients, and pCR was confirmed in 32 (27%) of patients.
Other smaller nonrandomized trials used concurrent infusional 5-FU from 250–1,500 mg/m2 per day with XRT before surgery in LARC. Pathological CR ranged from 10 to 28%, and SP procedure was possible from 39 to 59% [9–13]. Treatment was generally well tolerated, with no reported grade IV toxicities. Grade III toxicities included diarrhea (5%-20%) and leucopenia/neutropenia (1.6–6.6%).
Infusional CIV-5-FU + other agents with radiotherapy
There are no prospective randomized trials comparing the use of CIV-5-FU vs combination chemotherapy with XRT in the neoadjuvant treatment for LARC.
Multiple nonrandomized trials used other chemotherapy agents in addition to CIV-5-FU concurrently with XRT to increase pCR (Table 2). When used with leucovorin (LV) in a prospective nonrandomized trial in 15 patients with LARC, pCR was 13%, SP rates were 26.6%, and the 3-year overall survival rates were 66.7% [15]. In another similar study, pCR was 14%, with 82% of patients having a sphincter-saving operation, and 3-year survival rate was 69 [16] Combination of 5-FU with cisplatin showed similar results with pCR of 23%, SP rate 35%, and 3-year survival of 82% [19]. Mitomycin combination with CIV-5-FU showed 20% pCR and a 5-year survival rate of 64% [18]. All combination regimens appear to be effective with pCR ranging from 13 to 23% with no grade IV toxicity (Table 3).
Capecitabine with radiotherapy
The use of single-agent capecitabine with radiotherapy for neoadjuvant treatment of LARC is still in the early stages of development. There are no randomized controlled trials comparing oral capecitabine to CIV-5-FU in this setting. All available studies are based on phase I or II trials with small sample sizes.
There are two phase I trials done using capecitabine with XRT in LARC to determine the maximum-tolerated dose (MTD). In the trial by Dunst et al. [21], 36 patients received continuous capecitabine (250–1250 mg/m2 twice daily, 7 days/week) plus radiotherapy (50.4 Gy in 1.8-Gy daily fractions) for approximately 6 weeks in the neoadjuvant, adjuvant, or palliative settings. There was no grade III/IV toxicity reported with a capecitabine dose of 825 mg/m2 twice daily in combination with standard radiotherapy. In the neoadjuvant setting, one pathologic complete remission of a T3N1 tumor and nine partial remissions were observed in ten patients. In another phase I trial by Ngan et al. [22], dose escalation of capecitabine was discontinued at the MTD of 1,000 mg/m2 with two of five patients having developed a dose-related toxicity (DLT). Capecitabine 900 mg/m2 (Monday–Friday) twice daily in combination with radiotherapy throughout the course of preoperative pelvic irradiation (50.4 Gy) was associated with no DLTs. Out of 28 patients, five (19%) achieved a pathologic complete response.
Based on these phase I trials, several phase II trials were performed to further evaluate the efficacy and toxicity of concurrent capecitabine with XRT.
In one phase II study [24], 58 patients with LARC were treated with preoperative chemoradiation with capecitabine (825 mg/m2 twice daily). Treatment was well tolerated with no grade IV toxicity, and the primary grade III toxicities were leukopenia (10%), lymphopenia (10%), and diarrhea (4%). Complete response was observed in 30 of 49 evaluable patients, and downstaging occurred in 38 patients.
In another phase II study, Lin et al. [25] treated 54 patients with locally advanced rectal cancer with radiotherapy and concomitant neoadjuvant oral capecitabine 825 mg/m2 twice daily for 35 consecutive days, followed by surgery, followed by adjuvant capecitabine 1,250 mg/m2 twice daily (2 weeks on/1 week off). There was 79% overall response rate, with 16% of the patients achieving pCR. Treatment was generally well tolerated, with no grade IV toxicities. Fifty-two percent of patients exhibited grade III lymphopenia.
Table 4 summarizes the other phase II trials using capecitabine with concurrent radiation in the neoadjuvant setting of LARC. All studies showed similar results with pCR between 9 and 24% [26–30] and was generally well tolerated with no grade IV toxicity (Table 5).
Capecitabine + other agents with XRT
Capecitabine has been used with agents with XRT in LARC to possibly increase the efficacy.
Kim et al. [23] used capecitabine (1,650 mg/m2 per day) with leucoverin (20 mg/m2 per day) concurrently with radiation in the neoadjuvant setting for 45 patients with LARC.
Thirty-eight patients received definitive surgery. Tumor and nodal downstaging occurred in 63 and 90%, with pCR of 31% of patients. No grade III or IV hematological toxicities were observed.
The benefit of combination of capecitabine- and irinotecan/oxaliplatin-containing chemoradiotherapy regimens for locally advanced rectal cancer is under active study.
A phase I trial done by Hofheinz et al. used capecitabine in combination with weekly irinotecan with concurrent pelvic radiotherapy in patients with LARC [32]. Patients received weekly irinotecan at a dose of 50 mg/m2 beginning on day 1 of radiotherapy for 5 consecutive weeks (days 1, 8, 15, 22, and 29) 1 h before irradiation and capecitabine at three different dose levels (DLs): DL I (500 mg/m2 twice daily), DL II (625 mg/m2 twice daily), and DL III (750 mg/m2 twice daily). The study showed that capecitabine at 500 mg/m2 twice daily in combination with weekly irinotecan was safe and effective. Gastrointestinal adverse events at the recommended DL (DL I) comprised grade I or II diarrhea in 75% and nausea or vomiting in approximately 50% of the patients. No grade III gastrointestinal adverse events were seen in patients treated at DL I. pCR was found in four (21%), and microfoci (few tumor cells scattered within fibrotic tissue) were found in another 5 (26%) of 19 patients. Based on phase I trial results, Willeke et al. [33] enrolled 36 patients with LARC to receive weekly neoadjuvant irinotecan 50 mg/m2 (1 h before radiation) and capecitabine (1,000 mg/m2; days 1–38) with a concurrent radiotherapy dose of 50.4 Gy (45 + 5.4 Gy). Pathological complete remission was observed in five patients, and a further nine patients showed microfoci of residual tumor only. The main toxicities were grade III/IV leucopenia (20%), grade III nausea or vomiting (3%), and grade III transaminase increases (3%).
Oxaliplatin also has been used with a CAP and XRT combination in this setting. in a phase I trial, Glynne-Jones et al. [34] treated 18 patients with LARC with continuous capecitabine (500–825 mg/m2 twice daily, 7 days/week), oxaliplatin 2-h intravenous infusion (130 mg/m2, days 1 and 29), and pelvic radiotherapy (Monday–Friday for 5 weeks, total dose 45 Gy in 25 daily 1.8-Gy fractions). The MTD of capecitabine was 825 mg/m2 twice daily: Dose-limited toxicities occurred in two of six patients (grade III diarrhea, rectal pain with local skin reaction), but none in the patients receiving capecitabine at 650 mg/m2 twice daily. Fourteen patients had histologically confirmed R0 resections, and five had a pCR.
In a phase I/II trial done by Rödel et al. [35], patients diagnosed with LARC received concurrent capecitabine and oxaliplatin with XRT. Thirty-two patients received preoperative radiotherapy (total dose, 50.4 Gy) concurrently with CAP at 825 mg/m2 twice daily on days 1 to 14 and 22 to 35, with oxaliplatin starting at 50 mg/m2 on days 1, 8, 22, and 29 with planned escalation steps of 10 mg/m2. Dose-limiting grade III gastrointestinal toxicity was observed in two of six patients treated with 60 mg/m2 of oxaliplatin; therefore, the dose of 50 mg/m2 was the recommended dose for the phase II study. Tumor downstaging was observed in 17 of 31 (55%) of operated patients, and a pCR was identified in 19% of the resected specimens. Treatment was well tolerated with only two patients experiencing grade III diarrhea.
Analysis
There are no large prospective randomized controlled trials comparing oral capecitabine to CIV-5-FU with concurrent radiation in the preoperative treatment of LARC. However, there is one small phase III trial comparing capecitabine to bolus 5-FU [31]. One hundred and twenty-seven patients with LARC received concurrent preoperative chemoradiation with two cycles bolus 5-FU (500 mg/m2 per day) plus LV (20 mg/m2 per day), and 97 patients with LARC received concurrent chemoradiation using two cycles 1,650 mg/m2 per day of oral capecitabine and 20 mg/m2 per day of LV (Group II). A pathologic complete remission was achieved in 11.4 and 22.2% in patients in group I and II, respectively (P = 0.042). Among group I patients, one had grade III and another had grade IV thrombocytopenia and none in group II. No grade IV nonhematological toxicities were noted in either group.
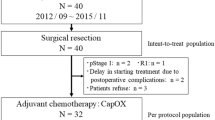
We retrospectively compared the efficacy and toxicity of CIV-5-FU and capecitabine with XRT. We collected data on 542 patients treated on either CIV-5-FU (197) or CAP (345) for LARC in a phase I or II study. All regimens appear active, yielding pCR rates ranging from 10 to 28% in CIV-5-FU/XRT regimens compared to 4 to 31% in CAP/XRT regimens. There were 25 patients in the CIV-5-FU group compared to 85 patients in the CAP group who achieved pCR. Chi-square tests were used to compare the two regimens [36–38]. It showed that pCR was statistically significant favoring the CAP group (23 vs 13%; P = 0.0008, P adj = 0.005). Safety profiles in CAP/XRT and CIV-5-FU/XRT combinations generally appear similar and well tolerated. There were no grade IV toxicities observed in both group. Most common grade III toxicities reported in CIV-5-FU were diarrhea, hematological toxicity, and proctitis. In the CAP group, the most common grade III toxicities were diarrhea, hand–foot syndrome, radiation dermatitis, and leucopenia (see Tables 3 and 5). Overall, capecitabine was generally well tolerated and may be even more efficacious than CIV-5-FU with the combination of XRT in achieving pCR. This comparison has its limitation, as the analysis was based on published information and not based on original case records. Many of these trials, which are reviewed in this article, suffer from similar deficiencies secondary to small numbers and nonstandardized radiation and surgical techniques, which can limit the conclusions that can be drawn.
Conclusions and future directions
Rectal cancer is a common cancer in the USA. In patients with distal tumors, the goal of preoperative radiotherapy alone or combined with chemotherapy is to downstage the tumor and allow for a sphincter-sparing surgical procedure, thereby improving quality of life and possibly overall survival. Although several innovative agents are being investigated in combination with radiotherapy for LARC in the neoadjuvant setting, XRT with 5-FU in continuous infusion remains the standard of care in patients with T3 or T4 rectal cancer until more updates became available. The protracted venous infusion of 5-FU requires specialized pumps and long-term venous access, which is inconvenient to the patient and carry the risk of infections or thrombosis. An oral agent such as capecitabine can be an attractive alternative.
In our pooled analysis with its limitation, we have shown that concomitant radiotherapy plus capecitabine is a very convenient, well-tolerated regimen and produces pathological response rates that are comparable to CIV 5-FU for LARC. Hand–foot syndrome was more common with capecitabine, and the potential risk of patient’s noncompliance, malabsorption, and the likely variable bioavailability of oral capecitabine in individual patients can make usage of capecitabine more challenging.
Although it is too early to assess whether oral capecitabine will be able to replace CIV-5-FU in combination with preoperative radiotherapy, the NSABP R-04 trial will address this question in a large phase III randomized trial. The primary objective of this study is to compare the rate of local–regional relapse in patients receiving preoperative oral capecitabine + radiotherapy to that in patients receiving preoperative CIV-5-FU + radiotherapy. Finally, phase I–II trials evaluating escalating doses of capecitabine with oxaliplatin or irinotecan with radiotherapy are being carried out to assess the MTD and efficacy in the neoadjuvant setting. The results from these trials are not available, and the use of these combinations is not recommended.
References
Jemal A, Siegel R, Ward E, Murray T (2007) Cancer Statistics. CA Cancer J Clin 57:43-66
Sauer R, Becker H, Hohenberger W et al (2004) Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med 351:173
Schüller J, Cassidy J, Dumont ERB, Durston S, Banken L, Utoh M et al (2000) Preferential activation of capecitabine in tumor following oral administration in colorectal cancer patients. Cancer Chemother Pharmacol 45:291–297
Cassidy J, Twelves C, Van Cutsem E, Hoff P, Bajetta E, Boyer M et al (2002) First-line oral capecitabine therapy in metastatic colorectal cancer: a favorable safety profile compared with intravenous 5-fluorouracil/leucovorin. Ann Oncol 13:566–575
Cole S, Carey D, Saif MW (2005) Comparison of efficacy and safety of capecitabine (CAP) compared with intravenous continuous infusion (CIV) of 5-FU administration in advanced colorectal cancer (CRC). Proc Am Soc Clin Oncol 23:268s(Abstract 3591)
Liu G, Franssen E, Fitch MI, Warner E (1997) Patient preferences for oral versus intravenous palliative chemotherapy. J Clin Oncol 15:110–115
Byfield JE, Calabro-Jones P, Klisak I, Kulhanian F (1982) Pharmacologic requirements for obtaining sensitization of human tumor cells in vitro to combined 5-fluorouracil or ftorafur and X rays. Int J Radiat Oncol Biol Phys 8:1923
O’Connell MJ, Martenson JA, Wieand HS et al (1994) Improving adjuvant therapy for rectal cancer by combining protracted-infusion 5-FU with radiation therapy after curative surgery. N Engl J Med 331:502
Janjan NA, Khoo VS, Abbruzzese J et al (1999) Tumor downstaging and sphincter preservation with preoperative chemoradiation in locally advanced rectal cancer: the M. D. Anderson Cancer Center experience. Int J Radiat Oncol Biol Phys 44:1027
Marsh R, Chu N et al (1996) Preoperative treatment of patients with locally advanced unresectable rectal adenocarcinoma utilizing continuous chronobiologically shaped 5-fluorouracil infusion and radiation therapy. Cancer 78:217–225
Myerson RJ, Valentini V, Birnbaum EH et al (2001) A phase I/II trial of three-dimensionally planned concurrent boost radiotherapy and protracted venous infusion of 5-FU chemotherapy for locally advanced rectal carcinoma. Int J Radiat Oncol Biol Phys 50:1299–1308
Videtic GM, Fisher BJ, Perera FE et al (1998) Preoperative radiation with concurrent 5-fluorouracil continuous infusion for locally advanced unresectable rectal cancer. Int J Radiat Oncol Biol Phys 42:319
Chen ET, Mohiuddin M, Brodovsky H et al (1994) Downstaging of advanced rectal cancer following combined preoperative chemotherapy and high dose radiation. Int J Radiat Oncol Biol Phys 30:169
Mohiuddin M, Regine WF, John WJ et al (2000) Preoperative chemoradiation in fixed distal rectal cancer: dose time factors for pathological complete response. Int J Radiat Oncol Biol Phys 46:883
Sun XN, Yang Q et al (2003) Pre-operative radiochemotherapy of locally advanced rectal cancer. World J Gastroenterol 9:717–720
Lam CW, Chen WT, Liu MT et al (2005) Effect of preoperative concurrent chemoradiotherapy in locally advanced low rectal cancer after radical resection surgery. Int Surg 90:53
Klautke G, Feyerherd P, Ludwig K et al (2005) Intensified concurrent chemoradiotherapy with 5-fluorouracil and irinotecan as neoadjuvant treatment in patients with locally advanced rectal cancer. Br J Cancer 92:1215–1220
Burke SJ, Percarpio BA, Knight DC, Kwasnik EM (1998) Combined preoperative radiation and mitomycin/5-fluorouracil treatment for locally advanced rectal adenocarcinoma. J Am Coll Surg 187:164
Weinstein GD, Rich TA, Shumate CR et al (1995) Preoperative infusional chemoradiation and surgery with or without an electron beam intraoperative boost for advanced primary rectal cancer. Int J Radiat Oncol Biol Phys 32:197
Chu E, Eng C, Abbruzzese J et al (2003) Efficacy and safety of capecitabine for colorectal cancer. Am J Oncol Rev 2(Suppl 3):1–28
Dunst J, Reese T, Sutter T et al (2002) Phase I trial evaluating the concurrent combination of radiotherapy and capecitabine in rectal cancer. J Clin Oncol 20:3983–3991
Ngan SY, Michael M, Mackay J et al (2004) A phase I trial of preoperative radiotherapy and capecitabine for locally advanced, potentially resectable rectal cancer. Br J Cancer 91:1019–1024
Kim JS, Kim JS, Cho MJ, Song KS, Yoon WH (2002) Preoperative chemoradiation using oral capecitabine in locally advanced rectal cancer. Int J Radiat Oncol Biol Phys 54:403–408
Dunst J, Reese T, Debus J, Hoelscher T, Budach W, Rudat V et al (2004) Phase-II-study of preoperative chemoradiation with capecitabine in rectal cancer. Proc Am Soc Clin Oncol 23:260
Lin EH, Skibber J, Delcos M, Eng C, Christopher C, Brown T et al (2005) A phase II study of capecitabine and concomitant boost radiotherapy (XRT) in patients (pts) with locally advanced rectal cancer (LARC). Proc Am Soc Clin Oncol 23:26(Abstract 3593)
Kocakova I, Svoboda M, Klocova K et al (2004) Combined therapy of locally advanced rectal adenocarcinoma with capecitabine and concurrent radiotherapy. Proc Am Soc Clin Oncol 23:299(Abstract 3720)
De Paoli A, Chiara S, Luppi G et al (2004) A phase II study of capecitabine (CAP) and pre-operative radiation therapy (RT) in resectable, locally advanced rectal cancer (LARC). Proc Am Soc Clin Oncol 23:255(Abstract 3540)
Veerasarn V, Phromratanapongse P, Lorvidhaya V et al (2004) Preoperative capecitabine (X) chemoradiation is effective and well tolerated in patients (pts) with locally advanced rectal cancer (LARC): findings from a phase I dose escalation study. In: Proc ESTRO (Abstr 610)
Maricela A, Minea L et al (2006) Concomitant capecitabine and radiotherapy for elderly patients with rectal cancer. In: Proc Am Soc Clin Oncol Gastrointestinal Cancers Symposium (Abstract 357)
Marsh RD, Larson B et al (2006) phase II trial of neo-adjuvant capecitabine combined with hyperfractionated accelerated radiation therapy in locally advanced rectal cancer. Proc Am Soc Clin Oncol Gastrointestinal Cancers Symposium (Abstract 355)
Kim JS, Kim JS, Cho MJ, Yoon WH, Song KS (2006) Comparison of the efficacy of oral capecitabine versus bolus 5-FU in preoperative radiotherapy of locally advanced rectal cancer. J Korean Med Sci 21(1):52–57
Hofheinz RD, von Gerstenberg-Helldorf B et al (2005) Phase I trial of capecitabine and weekly irinotecan in combination with radiotherapy for neoadjuvant therapy of rectal cancer. J Clin Oncol 23:1350–1357
Willeke F, Horisberger K, Kraus-Tiefenbacher U et al (2007) A phase II study of capecitabine and irinotecan in combination with concurrent pelvic radiotherapy (CapIri-RT) as neoadjuvant treatment of locally advanced rectal cancer. Br J Cancer 96:912–917
Glynne-Jones R, Sebag-Montefiore D, Maughan TS et al (2006) A phase I dose escalation study of continuous oral capecitabine in combination with oxaliplatin and pelvic radiation (XELOX-RT) in patients with locally advanced rectal cancer. Ann Oncol 17:50–56
Rödel C, Grabenbauer GG, Papadopoulos T et al (2003) Phase I/II trial of capecitabine, oxaliplatin, and radiation for rectal cancer. J Clin Oncol 21:3098–3104
Benjamini Y, Yekutieli D (2001) The control of the false discovery rate in multiple hypothesis testing under dependency. Ann Stat 29(4):1165–1188
Hochberg Y, Benjamini Y (1990) More powerful procedures for multiple significance testing. Stat Med 9:811–818
Cox DR (1965) A remark on multiple comparison methods. Technometrics 7:223–224
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Saif, M.W., Hashmi, S., Zelterman, D. et al. Capecitabine vs continuous infusion 5-FU in neoadjuvant treatment of rectal cancer. A retrospective review. Int J Colorectal Dis 23, 139–145 (2008). https://doi.org/10.1007/s00384-007-0382-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-007-0382-z