Abstract
Background and aims
The objective of this work is to evaluate the health care utilization and cost of different types of functional bowel disorder (FBD) in a population of Iranian patients and compare the costs in consulters and non-consulters.
Materials and methods
A consecutive sample of 1,023 patients in an outpatient gastroenterology clinic in central Tehran were interviewed, using two questionnaires based on the Rome II criteria, from December 2004 to May 2005 to detect FBD patients and to determine the frequency of health resource utilization (physician visit, hospitalization, laboratory tests, imaging studies, and drugs) and productivity loss (days off work or with low functionality) due to FBD symptoms in the past 12 months. Societal perspective was used and cost per person per year was estimated in purchasing power parity dollars (PPP$).
Results
The direct costs (for consulters, non-consulters; data presented in this order) were: irritable bowel syndrome (IBS; $92.04, $1.04), unspecified functional bowel disorder (FBD; $100.94, $0.39), functional constipation ($57.23, $1.04), and functional abdominal bloating ($71.35, $0.63). Indirect costs (for consulters, non-consulters) were: IBS ($811.85, $669.09), unspecified FBD ($705.85, $263.47), functional constipation ($587.48, $97.49), and functional abdominal bloating ($147.88, $38.60). Total yearly costs of IBS and functional constipation for urban adult population of Iran were roughly estimated at 2.94 billion PPP$ and 89.2 million PPP$, respectively.
Conclusions
As proven in developed countries, FBD and especially IBS seem to put a heavy burden on the economy of a developing country like Iran. Further population-based studies are needed for more precise estimations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Functional bowel disorders (FBD) are functional gastrointestinal disorders with symptoms attributable to the mid- or lower gastrointestinal tract. They include irritable bowel syndrome (IBS), functional abdominal bloating (FAB), functional constipation (FC), functional diarrhea (FD), and unspecified functional bowel disorder (UFBD). The diagnosis always presumes the absence of a structural or biochemical explanation for the symptoms, and it is based mainly on symptom evaluation and clinical criteria, as well as the ruling out of organic disturbances [1]. FBD are commonly encountered disorders and two different population-based studies in Canada and Israel have reported the prevalence of FBD as 41.6 and 26%, respectively, considering Rome II criteria, which is the latest validated diagnostic criteria for FBD [2, 3]. Most of the studies about FBD have focused on IBS and only a few studies have addressed other types of FBD.
Different prevalences of IBS were reported in different areas. The study of Hoseini-Asl and Amra [4] in Shahrekord, Iran reported the prevalence of IBS (defined by Rome II) about 5.8% among individuals who are over 20 years old. IBS is associated with a broad pattern of increased health care use and cost. Some studies have shown that more than two-thirds of IBS patients (diagnosed by Rome II criteria) consult some type of health care professional since the onset of disease, and 80% of these patients refer to a doctor during a 12-month period [5, 6]. Physicians request several investigations (i.e., lab tests, imaging, etc.) for two-thirds of IBS patients during their disease period to rule out organic disorders [5]. These studies have also shown that more than 70% of IBS patients consume drugs for their disease [5, 6]. On the other hand, over a 12-month period, 8% of the patients are admitted to the hospital for about 6 days in average [5]. In addition to direct costs including cost of physician visit, diagnostic procedures, drugs, and hospitalization, IBS has some indirect costs caused by missed days from work and loss of productivity while at work. A study has demonstrated that over a 1-year period, 11% of employed IBS patients have to take time off [5]. Another study in the US showed that the employees with IBS had a 15% greater loss in work productivity because of gastrointestinal symptoms than those without IBS, and IBS was associated with a 21% reduction in work productivity, equivalent to working less than 4 days in a 5-day workweek [7]. Muller-Lissner et al. performed a study on 200 IBS patients in 2002 to estimate the cost of IBS. This study showed that the total direct cost of one IBS patient per year was about 1548 DEM (791.48 euros), which increased to 1946 DEM (994.97 euros) considering the indirect costs for sick leave [8]. Another study in France reported the average monthly medical costs of IBS to be 71.8 euros [9]. There are several other studies that have compared the health care costs between IBS and non-IBS patients and have shown that IBS increases these costs [10–14]. The symptoms of IBS are significantly bothersome and place a substantial burden on the personal and working lives of patients. A study in France in 2004 reported that two-thirds of the IBS individuals changed their diet; 54 and 29% said IBS affected their social life and professional life, respectively [5]. IBS also reduces patients’ quality of life [6, 15].
The prevalence of functional constipation was reported to be about 14% according to the Rome II criteria in Canada and Spain [16, 17]. However, there is no data about its prevalence based on Rome II in Iran. The study of Pekmezaris et al. [18] in the US showed that the average cost per day for care, specifically for the treatment of constipation, was US $2.11 in 2002.
There is not so much data available about the prevalence, health care use, and cost of other types of FBD. The goal of this study was to evaluate the health care utilizations and costs of different types of FBD (as defined by the Rome II criteria) in a population of Iranian patients and to compare the costs in consulters and non-consulters.
Materials and methods
The study was conducted in an outpatient gastroenterology clinic in central Tehran from December 2004 to May 2005. All of the patients referring to the clinic were first interviewed by a general practitioner before their gastroenterology visit. At the beginning of the interview, all of the patients were given the explanation that participating in the study was not compulsory and the obtained information would be kept confidential. The interviewer first used a preliminary questionnaire asking about patients’ sex, date of birth, and whether they had experienced frequent occurrence (at least 4 days/month) of abdominal pain/discomfort (relieved with defecation), constipation, diarrhea, or bloating during the past 12 months. Patients were then visited by a gastroenterologist, who excluded the patients with colorectal organic disorders such as inflammatory bowel disease, celiac disease, diverticulitis, and colorectal cancer. Then those patients who had at least one of the FBD-related symptoms mentioned in the preliminary questionnaire and did not have any colorectal organic diseases were asked to attend a second interview with the general practitioner and a main questionnaire was filled out for them by the interviewer. This questionnaire asked the patients about FBD-related symptoms and their duration in detail, and the general practitioner strove to confirm the diagnosis of each type of FBD based on Rome II criteria. It also included questions about the utilization of health resources due to FBD-related symptoms within the past 12 months before the study. Health resource utilization was categorized into the following categories: physician visit (GP, specialist), hospitalization, laboratory tests, imaging studies, and drugs. Productivity loss was measured by the number of the days on which FBD symptoms had completely interfered with patient’s daily activities or had caused at least 30% functionality loss in daily activities but not totally disabling the patient. In this regard, the patients were asked how many days during the past 12 months they had been absent from their job and how many days during the same period they had low function (at least 30% loss of function) in their job or daily activities because of FBD symptoms (that had been explained to them in previous questions). Finally, two questions asked the patient to what extent the disease hurt them and how much they were concerned about their disease.
All costs were viewed from the societal perspective disregarding subsidies. The unit cost of different health resources including physician (GP/specialist) visits, laboratory tests, and imaging studies were calculated based on the price lists approved by the joint committee composed of Iranian Parliament members, representatives of Iranian Medical Association, and two government ministers, for year 2005. The electronic Farsi version of the document can be found at IRTEB.COM Web site (http://www.irteb.com/fee.htm).
Regarding laboratory tests, we simply asked about the type of the sample that the patient had given to the laboratory, as we assumed that it could be the best remembered point about a laboratory test to the patient. Therefore, the patient only had to determine if he had a blood, urine, or stool test for a certain number of times asked by a physician for workup of FBD-related symptoms. Then the minimum cost of a blood test was assumed to be equal to the cost of a CBC count, as it is one of the most common and cheapest tests ordered by a physician. Similarly, the minimum costs of a urinalysis and a stool exam were considered for a urine or stool test, respectively.
The prices of chemical drugs were also retrieved form the drug list of Food and Drug Organization of Iran finalized for 2005 and published in Farsi at the IRTEB.COM Web site. When considering the cost of herbal and chemical drugs, if different brands were available, the cheapest brand was taken into account. As most of the patients did not know the exact dose and amount of the drugs they had used, we considered the lowest dose for adults and the minimum accepted duration of medical therapies unless the patient exactly knew how long he or she had taken the drug. In addition, although herbals in this report are meant to include both herbal drugs and herbs having therapeutic effects, we only included the herbal drugs in cost analysis. We define herbal drugs here as those existing as registered herbal drugs in Iranian pharmacopoeia, a list of which was published in Farsi in (http://www.irteb.com/herbal/herbaldrugeindex.htm). The authors could not find the cost of herbal drugs listed in Iranian pharmacopoeia in any hardcopy or electronic publication. Therefore, the authors contacted the corresponding manufacturers to get the price of the herbal drugs.
To estimate the cost of productivity loss, the days of total activity loss were summed up. Three days with low functionality (see definition above) were considered as one day of total activity loss. Then, the average number of days of total activity loss for each patient in a year (by FBD type) was estimated. Iranian GNI (gross national income) per capita (in 2004) in US and purchasing power parity dollars (PPP$) were retrieved from the World Bank Web site (http://www.worldbank.org). The average daily income of each Iranian was assumed to be 1/365 of the GNI per capita. The rate of unemployment (11.2%, reported by the World Bank Organization) was applied. US dollar was assumed to be in an average rate of 9,000 Rials based on reports from the Central Bank of Iran in 2005. Comparing 2004 GNI per capita in US dollars ($2,300) and PPP dollars (7,550 PPP$) from the World Bank database (and the exchange rate of US $1 = 9,000 Rials), we arrived at the estimation of one PPP$ to be 2,727 Rials. This was then used to convert costs from Iranian Rials to PPP dollars. Using PPP dollars is preferred to the US $ based on usual exchange rates and makes cross-country comparison of costs more reliable.
It is worth mentioning that the definition of a consulter in this study was quite different from the definitions in the previous relevant paper published based on data from the same patients [19]. In this cost analysis study, we defined consulters as those who had referred to a physician for their FBD symptoms in the past 12 months, whereas in the previous paper mentioned above, we defined a consulter as the patient presenting in her current gastroenterology visit (i.e., when she was interviewed) for FBD symptoms.
SPSS 10 software (SPSS, IL, USA) was used for statistical analysis. Chi-square test was used for the analysis of nominal data in detecting statistically significant differences between different FBD groups in their frequency of use of different health resources. The Mann–Whitney U test was employed to compare the means of continuous data with nonparametric distribution (the number of days of total activity loss or days with low functionality) and ordinal variables (self-estimated level of suffering from disease or concern about disease) in any two groups (different groups of FBD and consulters vs non-consulters). P values below 0.05 were considered significant.
Results
It is worth mentioning that this study was performed in parallel with another study determining the relative distribution of different types of FBD and their symptom patterns among FBD patients of the same clinic. The results of that study were published in a previous paper by the same authors. The cost analysis results from the same patients are brought here. The reader is referred to Roshandel et al.’s [19] work for more details.
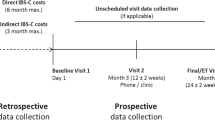
Of 410 FBD patients, 110 were consulters (i.e., they had seen a physician for their FBD symptoms in the past 12 months) [19]. The proportion of consulters to all patients in each FBD patient group is illustrated in Fig. 1. The highest proportion of consulters was found in IBS patients and decreased in functional bloating and functional constipation patients and reached the minimum in the patients with unspecified functional bowel disorder. These differences in consulter proportions in different FBD groups were statistically significant with a Chi-square test (p < 0.001).
Proportion of consulters among patients with different types of FBD. The difference between the consulter proportions in the FBD groups was statistically significant (p < 0.001, Chi-square). IBS Irritable bowel syndrome, FAB functional abdominal bloating, FC functional constipation, UFBD unspecified functional bowel disorder, FBD functional bowel disorder
The self-estimated level of suffering from disease (i.e., how much FBD hurt the patient from patients’ point of view) and the extent of concern about disease in a five-degree scale are shown in Table 1. The highest self-estimated level of suffering from the disease was observed among IBS patients (p < 0.001). Consulters self-assessed their level of suffering from disease higher than non-consulters in functional abdominal bloating, functional constipation, and unspecified functional bowel disorder (Table 1), but not in the IBS group. IBS patients showed higher levels of concern about their disease than patients with other types of FBD did (p = 0.001). In addition, consulters were more concerned about their disease than non-consulters in all FBD groups (Table 1).
The frequency of patients using medical resources in the past 12 months are shown in Table 2 by the FBD group, as well as the resource category including physician visit, drugs, laboratory tests, and imaging studies. None of our patients were hospitalized for FBD-related symptoms within the past 12 months of the study. Patients visited a range of physicians (for their FBD symptoms) including general practitioner, gastroenterologist, surgeon, urologist, gynecologist, psychologist, infectious disease specialist, and homeopath. None of the functional diarrhea patients had consulted a doctor during the 12 months before the study. However, the reason for the current gastroenterology visit in four out of the seven functional diarrhea patients was diarrhea.
Metronidazole, bismuth, and clidinium-C were the most frequently used chemical drugs prescribed for the patients in all groups. IBS patients used chemical drugs more than patients in other FBD groups (p < 0.001). Only two patients with functional diarrhea used chemical drugs during the past 12 months.
C-lax tablet and psyllium powder were the herbal drugs that were used in all groups of FBD patients except for functional diarrhea. Moreover, carmint drop was used by some patients with functional constipation and functional abdominal bloating. Functional constipation patients used herbals more than the other groups (p < 0.05). Only one functional diarrhea patient used herbs to relieve FBD-related symptoms.
Considering the consulter group only, there was no statistically significant difference between the frequencies of patients in different FBD groups having used lab tests, imaging studies, or diagnostic procedures. In other words, no particular category of resources aimed at patients’ diagnosis (lab tests, imaging studies, etc.) was associated with increased use in any group of FBD patients.
The frequency of patients in FBD groups having experienced loss of work days or days spent in low functionality (>30% loss of function) due to FBD (within the past 12 months) is shown in Table 3. There was no statistically significant relationship between the type of FBD and the number of lost workdays using the Mann–Whitney U test. However, IBS patients experienced a higher number of low-functionality days than other FBD patients (p < 0.001). The seven patients with functional diarrhea reported no days off work or days with low function in the 12 months before the study.
The direct medical costs and indirect (productivity loss) costs of disease per person per year for the different types of FBD and by resource utilization category are shown in Table 4.
Discussion
Functional bowel disorders are common entities in many communities and, therefore, are expected to be of remarkable economic burden. Though there have been some cost analyses on IBS and constipation, all FBD types as defined in Rome II have rarely been analyzed economically together in one study. In this study, we mainly aimed to have an estimate of the cost per year per person of each type of FBD from the societal perspective in both consulter and non-consulter FBD patients in a developing country.
Though the study revealed interesting facts about FBD costs in a developing country, the results of this study must be interpreted after the reader considers the following issues in this research work. First, this study was not population-based and, therefore, the selection bias of the study population must be kept in mind. The study was performed in an outpatient gastroenterology clinic located in the center of Tehran, the Iranian capital where patients presented mostly from urban areas of Tehran province and, to a lesser extent, from other provinces of Iran. In addition, the patients’ level of education seemed to be above the average for Iranian population. The reader is referred to the paper by Roshandel et al. [19] for more details about the study population. Second, the validation of the Rome II criteria has not yet been tested in Iranian population. Nevertheless, a multinational study using the subjects from several Asian countries including China, Hong Kong, Indonesia, Korea, Malaysia, Singapore, Taiwan, Thailand, and Vietnam has partially supported use of Rome II among Asian patients with functional gastrointestinal disorders [20]. It is also noteworthy that despite some controversies around Rome II such as its being too restrictive for clinical practice, it is especially considered the most appropriate for clinical and epidemiological research purposes [21]. Finally, measuring the frequency of health resource use by patients was mostly based on patients’ recollection and this could also be a source of bias.
As Table 4 shows, the most costly FBD, considering all direct and indirect (productivity) costs, is IBS closely followed by UFBD, while the least costly one was FAB. It is noteworthy that the main cause for this dominance of costs in IBS and UFBD is their significantly higher indirect costs. The reasons for higher costs associated with IBS and especially UFBD can be difficult to explain. IBS is known to significantly decrease patients’ quality of life, and its degree of nuisance or unsuccessful pharmacological therapies may be a reason for higher costs. In addition, abdominal pain has been reported to be the most important factor associated with health care seeking among IBS patients [22]. This could be one of the causes for higher direct costs in IBS patients. Chronicity and vagueness of symptoms in UFBD patients may cause the physician to more frequently order paraclinical and imaging tests to rule out organic disease or even try some courses of experimental pharmacotherapy. Whether the symptoms in a proportion of UFBD patients were due to extra-intestinal organic or even psychological diagnostically challenging disorders elusive to the physician is a question that could not be answered in our study. These issues merit more attention in future studies.
It is also interesting that all FBD types in our study caused indirect costs over ten times higher than direct costs. Most indirect costs are due to cumulative productivity loss caused by the days with low functionality. It is noteworthy that there were outliers among most FBD groups when considering the number of days of total activity loss or with low function (Table 3), and these influenced the mean of the number of days of productivity loss in each group of FBD patients. However, in a health–economic approach as the one in this report, we are interested in the economic cost of this lost productivity; therefore, this mean will be an appropriate index. The reader is referred to the ranked categorization in Table 3 to get a more realistic view of the values in each FBD group. For instance, though the average number of days of full productivity loss is 10.2 per person per year in UFBD patients (Table 3), the majority (88.9%) of such patients literally experienced no days of full productivity loss.
Comparing consulters and non-consulters showed that the direct costs in non-consulters were primarily due to consumption of drugs, while in consulters imaging studies comprised a significant portion of the costs. It might be explained by considering non-consulters as those patients viewing their disease as less bothersome (see below and Table 1) and so they resort to over-the-counter drugs for symptom relief rather than going to a physician. Among consulters, the relative dominance of the costs of imaging studies (compared to other direct costs) seems to be due to the fact that it is mandatory for the physician to rule out abdominal organic pathologies in order to make a diagnosis of FBD. In addition, the high cost of imaging studies could play a role here. Comparing indirect costs in consulters and non-consulters shows that the indirect costs in consulters were about three to ten times higher than that in non-consulters. An exception was IBS, where consulters and non-consulters showed rather similar indirect costs (Table 4).
Consulters in all FBD groups except IBS were more concerned about their disease and also felt that their disease would hurt them to a further extent compared to non-consulters. This is of course expected for consulters since such factors may force a patient to see a physician. It is interesting that unlike other FBD patients, IBS consulters and non-consulters both showed high levels of concern and self-estimated suffering from disease. Therefore, it could not be postulated that the aforementioned factors could potentially influence our IBS patient to become a consulter. This also raised a question: what would cause some IBS patients to be consulters and some to get along with their disease otherwise? Though we did not investigate this, some reasons could be suggested. First, our non-consulters might have been involved with more bothersome non-bowel diseases that pushed down IBS as a second priority, especially that we were studying on FBD patients in a gastroenterology clinic. In addition, IBS is one of three subtypes and the symptoms in some subtypes might be more bothersome than others. Finally, abdominal pain has been shown in one report to be the most important factor associated with health care seeking among IBS patients [22]. All these factors can also be important in making an IBS patient a consulter, in addition to the degree of concern about the disease.
A point that must be stressed when considering the cost analyses in this study is the fact that the authors took a minimal cost approach. First, the tariffs used for health services are those applied in state sector centers and the costs of services in many private centers can be higher. However, since the societal perspective was used, all subsidies were disregarded and non-subsidized costs were taken into account. Second, the “cheapest brand” prices of drugs were used. Moreover, only the cost of the herbal drugs listed in Iranian pharmacopoeia was included, while some patients used herbs not assumed as herbal drugs (i.e., these costs were not included). Third, if patients had undergone a laboratory test, the cost of the cheapest test was considered. Last but not the least, the non-medical direct costs such as transportation, care giver time, and the like were not included in our direct costs.
Comparing the costs estimated in this study, which took place in a developing country. and those from other studies (e.g., in developed world) can be useful. First, it seems that cost analysis data on FBDs other than IBS is scarce. Second, different cost analyses use different methods such as different economic perspectives; therefore, the results are variable. Our study used societal perspective. A systematic review considering studies from USA, Canada, and UK by Inadomi et al. reported the mean direct costs of irritable bowel syndrome management to be UK £90, Canadian $259, and US $619 per patient annually, and productivity costs ranging from US $335 to 748 [23], Maxion-Bergemann et al. [24], in a review on UK and US studies, showed that the total direct cost estimates per patient per year ranged from US $348 to 8,750 (calculated for year 2002). They also showed that the average number of days off work per year because of IBS was between 8.5 and 21.6 and indirect (productivity) costs ranged from US $355 to 3,344. Our direct medical costs for IBS were lower than even the minimum of these ranges. These lower direct costs may be due to lower cost of drugs, imaging studies, or other health services in a developing country like Iran compared to Western countries. Regarding productivity costs, as stated before, we considered 3 days with low function (i.e., at least 30% function loss) equivalent to 1 day of lost productivity and added them with days off work. Our average figures showing 36 (non-consulter) to 44 (consulter) days of work loss per patient per year seems higher than that found in Western studies (8.5–21.6 days) [24]. However, the productivity costs in PPP$ for the IBS in our study (669.9–811.85 PPP$) is within the range of Western studies [23, 24]. It is interesting that our finding of higher productivity costs for IBS was also proven by Bentkover et al. in a Canadian study (using societal perspective) showing that the productivity costs per patient per year (Canadian $748.16) was three times higher than direct costs (Canadian $258.82) [25].
Considering the cost per person per year estimated for FBD in this study and the evidence from the few population-based studies already performed in Iran on IBS, a rough estimate of yearly costs of IBS in Iran may be estimated. The study of Hoseini-Asl et al. in Shahrekord city of Iran among over-20-year old individuals showed that the prevalence of IBS was about 5.8% [4]. Ghannadi et al. [26] reported the prevalence of IBS to be about 18.4% among 1,200 university students in Khoram Abad city, the center of Lorestan province in the west of Iran. Both of these studies were based on Rome II. Another study by Massarrat et al., which was not based on Rome II, found an IBS prevalence of 3% [27]. Since our study population were primarily urban (see discussion below), we assume that our estimation for FBD cost per person per year only applies to urban adult population of Iran. According to the latest World Bank reports published in 2005, 67% of the Iranian population of 66.9 million live in urban areas and the individuals over 15 years old comprised 71% of the total population. These can give rise to an estimate of 31.82433 million of over-15 urban population in Iran. If we take the prevalences of IBS from the studies based on Rome II, which were newer and performed in other urban areas of Iran, we may assume that IBS prevalence ranges from 5.8% to 18.4% (average: 12.1%) among adult urban population. We do not have the proportion of FBD patients referring to health services (consulter rate) in Iran. The evidence from two western studies showed that two-thirds of IBS patients (diagnosed by Rome II criteria) consult some type of health care professional since the onset of disease and 80% of these patients refer to a doctor during a 12-month period [5, 6]. If we assume that only 40% of IBS patients finally see a physician for their problem (i.e., consulters), then we reach a total cost estimation of 2.94 billion PPP$ per year (1.39 and 1.55 billion PPP$ for consulters and non-consulters, respectively), which comprises direct costs (0.14 billion PPP$) and productivity costs (2.80 billion PPP$). As explained above, this cost is only for adult urban population of Iran. This estimation is rough, and population-based studies estimating consulter rate for IBS in Iran may help these calculations get closer to reality in the future.
Regarding constipation, there are no studies based on Rome II from Iran. Massarrat et al. [27] reported the prevalence of constipation symptom to be 3.1 and 3.6% among male Iranian pastoral nomads and industrial laborers, respectively. Khoshbaten et al. [28] also found a prevalence of 3.6% for constipation symptom in a population-based study in northwest Iran. As these provide evidence on the prevalence of the constipation symptom and it seems a reasonable assumption that only a proportion of those having the constipation symptom meet Rome II criteria for constipation, it may therefore be inferred that the prevalence of individuals with Rome II criteria constipation is below these figures (especially that constipation symptom may be due to organic diseases or exist in other FBDs such as IBS). In addition, we do not have consulter rate for constipation in Iran. A report by Harris [29] in the USA claimed that one-third of patients with constipation symptom seek medical care. If we assume that this is true for those with Rome II criteria constipation and, from figures above, we make an arbitrary assumption of prevalence of Rome II criteria constipation in Iran to be 1% (one-third of prevalence of constipation symptom), we can arrive at a rough estimation of total yearly costs for functional constipation. Using this, total yearly costs of functional constipation for the urban adult population of Iran might be 89.2 million PPP$ per year (68.3 and 20.9 million PPP$ for consulters and non-consulters, respectively), which comprises direct costs (6.29 million PPP$) and productivity costs (82.94 million PPP$). However, these figures are rough, and population-based studies using Rome II are needed to determine the prevalence of functional constipation and the consulter rate for this functional constipation in Iran.
In conclusion, this study suggests that, as proven in developed countries, FBDs especially IBS seem to put a heavy burden on the economy of a developing country like Iran. However, the study limitations as stated before must be considered, and further population-based studies are needed for more accurate estimations.
References
Thompson WG, Longstreth GF, Drossman DA et al (1999) Functional bowel disorders and functional abdominal pain. Gut 45(Supp1 II):II43–II47
Thompson WG, Irvine EJ, Pare P et al (2002) Functional gastrointestinal disorders in Canada: first population-based survey using Rome II criteria with suggestions for improving the questionnaire. Dig Dis Sci 47(1):225–235 (Jan)
Sperber AD, Shvartzman P, Friger M, Fich A (2005) Unexpectedly low prevalence rates of IBS among adult Israeli Jews. Neurogastroenterol Motil 17(2):207–211 (Apr)
Hoseini-Asl MK, Amra B (2003) Prevalence of irritable bowel syndrome in Shahrekord, Iran. Indian J Gastroenterol 22(6):215–216 (Nov–Dec)
Dapoigny M, Bellanger J, Bonaz B et al (2004) Irritable bowel syndrome in France: a common, debilitating and costly disorder. Eur J Gastroenterol Hepatol 16(10):995–1001 (Oct)
Badia X, Mearin F, Balboa A et al (2002) Burden of illness in irritable bowel syndrome comparing Rome I and Rome II criteria. Pharmacoeconomics 20(11):749–758
Dean BB, Aguilar D, Barghout V et al (2005) Impairment in work productivity and health-related quality of life in patients with IBS. Am J Manag Care 11(1 Suppl):S17–S26 (Apr)
Muller-Lissner SA, Pirk O (2002) Irritable bowel syndrome in Germany. A cost of illness study. Eur J Gastroenterol Hepatol 14(12):1325–1329 (Dec)
Le Pen C, Ruszniewski P, Gaudin AF et al (2004) The burden cost of French patients suffering from irritable bowel syndrome. Scand J Gastroenterol 39(4):336–343 (Apr)
Leong SA, Barghout V, Birnbaum HG et al (2003) The economic consequences of irritable bowel syndrome: a US employer perspective. Arch Intern Med 163(8):929–935 (Apr 28)
Longstreth GF, Wilson A, Knight K et al (2003) Irritable bowel syndrome, health care use, and costs: a U.S. managed care perspective. Am J Gastroenterol 98(3):600–607 (Mar)
Akehurst RL, Brazier JE, Mathers N et al (2002) Health-related quality of life and cost impact of irritable bowel syndrome in a UK primary care setting. Pharmacoeconomics 20(7):455–462
Patel RP, Petitta A, Fogel R et al (2002) The economic impact of irritable bowel syndrome in a managed care setting. J Clin Gastroenterol 35(1):14–20 (Jul)
Levy RL, Von Korff M, Whitehead WE et al (2001) Costs of care for irritable bowel syndrome patients in a health maintenance organization. Am J Gastroenterol 96(11):3122–3129 (Nov)
Akehurst RL, Brazier JE, Mathers N et al (2002) Health-related quality of life and cost impact of irritable bowel syndrome in a UK primary care setting. Pharmacoeconomics 20(7):455–462
Pare P, Ferrazzi S, Thompson WG et al (2001) An epidemiological survey of constipation in canada: definitions, rates, demographics, and predictors of health care seeking. Am J Gastroenterol 96(11): 3130–3137 (Nov)
Garrigues V, Galvez C, Ortiz V et al (2004) Prevalence of constipation: agreement among several criteria and evaluation of the diagnostic accuracy of qualifying symptoms and self-reported definition in a population-based survey in Spain. Am J Epidemiol 159(5):520–526 (Mar 1)
Pekmezaris R, Aversa L, Wolf-Klein G et al (2002) The cost of chronic constipation. J Am Med Dir Assoc 3(4):224–228 (Jul–Aug)
Roshandel D, Rezailashkajani M, Shafaee S, Zali MR (2006) Symptom patterns and relative distribution of functional bowel disorders in 1,023 gastroenterology patients in Iran. Int J Colorectal Dis 21(8):814–825
Kwan AC, Bao TN, Chakkaphak S, Chang FY, Ke MY, Law NM, Leelakusolvong S, Luo JY, Manan C, Park HJ, Piyaniran W, Qureshi A, Long T, Xu GM, Xu L, Yuen H (2003) Validation of Rome II criteria for functional gastrointestinal disorders by factor analysis of symptoms in Asian patient sample. J Gastroenterol Hepatol 18(7):796–802 (Jul)
Boyce PM, Koloski NA, Talley NJ (2000) Irritable bowel syndrome according to varying diagnostic criteria: are the new Rome II criteria unnecessarily restrictive for research and practice? Am J Gastroenterol 95(11):3176–3183 (erratum in Am J Gastroenterol 96(4):1319)
Talley NJ, Zinsmeister AR, Melton LJ 3rd (1995) Irritable bowel syndrome in a community: symptom subgroups, risk factors, and health care utilization. Am J Epidemiol 142(1):76–83 (Jul 1)
Inadomi JM, Fennerty MB, Bjorkman D (2003) Systematic review: the economic impact of irritable bowel syndrome. Aliment Pharmacol Ther 18:671–682
Maxion-Bergemann S, Thielecke F, Abel F, Bergemann R (2006) Costs of irritable bowel syndrome in the UK and US. Pharmacoeconomics 24(1):21–37
Bentkover JD, Field C, Greene EM, Plourde V, Casciano JP (1999) The economic burden of irritable bowel syndrome in Canada. Can J Gastroenterol 13(Suppl A):89A–96A
Ghannadi K, Emami R, Bashashati M et al (2005) Irritable bowel syndrome: an epidemiological study from the west of Iran. Indian J Gastroenterol 24(5):225–226 (Sep–Oct)
Massarrat S, Saberi-Firoozi M, Soleimani A et al (1995) Peptic ulcer disease, irritable bowel syndrome and constipation in two populations in Iran. Eur J Gastroenterol Hepatol 7(5):427–433 (May)
Khoshbaten M, Hekmatdoost A, Ghasemi H, Entezariasl M (2004) Prevalence of gastrointestinal symptoms and signs in northwestern Tabriz, Iran. Indian J Gastroenterol 23(5):168–170 (Sep–Oct)
Harris LA (2005) Prevalence and ramifications of chronic constipation. Manag Care Interface 18(8):23–30 (Aug)
Acknowledgement
The authors wish to express their gratitude to the Research Center for Gastroenterology and Liver Diseases, Shaheed Beheshti University of Medical Sciences, Tehran, Iran for kindly funding and supporting this research project.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Roshandel, D., Rezailashkajani, M., Shafaee, S. et al. A cost analysis of functional bowel disorders in Iran. Int J Colorectal Dis 22, 791–799 (2007). https://doi.org/10.1007/s00384-006-0226-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-006-0226-2