Abstract
Background/aims
The advent of contrast-enhanced ultrasound (CEUS) has called into question the efficacy of standard ultrasonographic techniques. In this study, we evaluated B-mode and color-duplex imaging and CEUS in the detection of liver metastases, using intraoperative and histological findings as a reference.
Materials and methods
Before laparotomy, 108 patients suspected of having liver metastases were prospectively examined with B-mode and color-duplex imaging, followed by contrast-enhanced ultrasound (2.4 ml SonoVue). Patients with unresectable tumors (n=8) were excluded from the analysis. The sonographic diagnosis in the remaining 100 patients was compared to the intraoperative and histological findings.
Results/findings
CEUS improved the sensitivity for detecting liver lesions from 56.3% (B-mode) to 83.8% (CEUS) (p=0.004). In particular, the contrast agent led to an improvement in ultrasonographic detection in the following cases: nodular metastases smaller than one centimeter; after adjuvant chemotherapy; for tumors near the surface of the liver; and for lesions situated around the ligamentum teres.
Interpretation/conclusions
CEUS provides significant improvement in the detection of liver metastases, and should therefore, be performed routinely in the surveillance of cancer patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Generally, hepatic metastasis is a sign of advanced tumor stage [1–3]. Curative treatment is only possible in a very small number of patients, e.g., only 20% of patients with colorectal metastases. In patients with pancreatic carcinoma, hepatic metastases imply a palliative situation [4–6].
When the objective is cure, liver resection is the most effective therapy [7–9]. For liver surgery, precisely imaging the number and distribution of the metastases is required. According to the literature, in detecting liver metastases, unenhanced ultrasonography achieves a sensitivity between 48 and 92% and a specificity between 76 and 96% [10–14]. Thus, its efficacy is inferior to the imaging modalities using contrast media [computed tomography (CT), magnetic resonance imaging (MRI)].
In Europe, contrast agents have been available for ultrasonography since 1995 [15, 16]. Complementing other new ultrasonographic technology, contrast agents have improved the detection of liver metastases considerably. Some authors have even reported sensitivities and specificities of up to 100% for contrast-enhanced ultrasonography (CEUS) [17–19]. However, in theses studies, the reference methods used in comparison were other imaging modalities, which lessens the impact of such reports, as none of the imaging methods reach the efficacy of today’s gold standard, intraoperative evaluation of the liver [20–22].
The aim of our work was to evaluate the efficacy of unenhanced and enhanced ultrasonography in the detection of liver metastases, as compared to intraoperative findings.
Materials and methods
For this prospective, nonrandomized study, a total of 108 patients underwent diagnostic CEUS for staging or exclusion of liver metastases between January, 2003 and April, 2005. This study was approved by the local ethics committee and performed according to the declaration of Helsinki. All patients gave their informed consent before their inclusion into the study.
There were 59 men and 41 women with a median age of 60 years (24 to 82 years). Sixty-five patients were examined when a suspicious lesion was noted during surveillance of their previously diagnosed cancer. Twenty of the 65 patients had already received adjuvant chemotherapy after primary surgery. Forty-three were referred for exclusion of liver metastases (n=36) or staging (n=7).
All patients first underwent diagnostic hepatic ultrasonography without contrast enhancement (B-mode and color duplex), followed by contrast-enhanced ultrasound with pulse inversion and low MI (0.07–0.14). A bolus of 2.4-ml SonoVue (Bracco-Altana, Milan, Italy), a second-generation ultrasound contrast agent, was used as the contrast medium. The ultrasound device used was a Sonoline Elegra (3.5-MHz transducer, Siemens Medical Solutions, Erlangen, Germany).
The ultrasonographic diagnosis was made by one of three examiners. This group of examiners consisted of an attending physician and two experienced residents. All examiners were blinded to any diagnosis of hepatic metastases obtained before ultrasonography.
Preoperatively, the liver was screened for metastases with and without contrast enhancement. The number and localization of the liver metastases were recorded and each metastasis was marked on a diagram of the liver segments (Couinaud). Correspondingly, during surgery, the intraoperative findings (obtained by inspection, palpation, and intraoperative ultrasonography) were drawn onto a similar diagram. To avoid bias, the data evaluation (comparison of both diagrams) was performed in a blinded fashion by someone not involved in performing the sonographic examinations. Statistical analysis was performed using the two-tailed McNemar test (SPSS V12.01).
A preoperative spiral CT or MRI of the abdomen with intravenous contrast was also available for all patients. As these CT and/or MRI studies originated from different institutions and varied to a great extent in the examination technique, they were not included in the results of this study. A repetition of the exams was avoided as the main focus of the study was the evaluation of unenhanced and enhanced sonography.
To minimize the number of unnecessary laparotomies, only patients with resectable lesions (n=65), as determined by sonography and CT or MRI, or patients scheduled for surgery for their primary cancers were selected for the study. In 29 patients, after intraoperative exclusion of liver metastasis, the primary cancer was resected. Six additional patients received palliative bypass surgery when the intraoperative examination of the liver led to the conclusion that the primary tumor was unresectable (Table 1). Eight patients initially scheduled for surgery who underwent CEUS were later dropped from the study. Two of these patients had large metastases in the right lobe of the liver and additional central metastases. Four patients had multiple metastases (two patients with six metastases, one patient with seven, and one patient with nine). In another two patients, large metastases infiltrated the central portal vein. For this group of eight patients, unenhanced sonography showed 20 metastases in six patients, while enhanced ultrasound accounted for 32 metastases. None of these eight patients underwent surgery and all were excluded from the study. The metastases were biopsied percutaneously under sonographic guidance to acquire a histological diagnosis. In two patients, the three lesions were only visible while using contrast media. In these cases, the biopsy was performed while using the contrast agent, thereby, avoiding a laparotomy.
Results
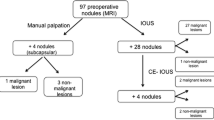
A total of 100 patients underwent laparotomy. Intraoperatively, by inspection, bimanual palpation and in situ ultrasonography of the liver, 134 lesions suspicious for metastases were found in 71 patients. Using B-mode ultrasonography, only 70 of these 134 (52.2%) lesions in 46 patients were detected (Fig. 1), while CEUS was able to detect 122 of 134 (91%) suspicious lesions in 60 patients (Fig. 2). In 52 patients, the histological diagnosis was obtained from the surgical specimen, while in 19 patients, the metastasis was biopsied percutaneously. In five of these patients not undergoing surgery, radio frequency ablation was performed.
Same Patient as Fig. 1. Evidence of two additional lesions in the arterial phase after administration of SonoVue
In the 67 of the 71 patients, surgery and final histology revealed 130 metastases (Fig. 3). The number of metastases varied between 1 and 10. In the remaining four patients, the final histological analysis showed a blood-filled liver cyst in one patient who had suffered from blunt abdominal trauma, a small cholangioma in two other patients (6 and 8 mm), and a 7-mm adenoma in one patient. None of these benign lesions were distinguishable preoperatively from metastases as they were small and demarcated in the late phase of the CEUS (Table 1).
Same Patient as Fig. 1. Operation specimen after right hemihepatectomy
Sonographic imaging compared with intraoperative results
In assessing the number of hepatic metastases by ultrasonography as compared to the intraoperative results, the rate of correct ultrasound findings rose from 67% (n=67) without contrast enhancement to 84% (n=84) with SonoVue. The use of the contrast medium provided additional information, particularly for metastases smaller than 10 mm. By CEUS, 18 small nodular metastases were detected in nine patients, whereas, unenhanced sonography only detected five metastases in four patients. Intraoperatively, 20 metastases smaller than 10 mm were discovered in 11 patients.
Further information was also obtained by CEUS after adjuvant chemotherapy. In these cases, unenhanced sonography detected six lesions in five patients. With the use of SonoVue the detection rate rose, identifying 17 metastases in 11 patients. In total, for 14 patients who had undergone adjuvant chemotherapy, 21 metastases were detected.
Thus, in the assessment of the number of hepatic metastases detected by different techniques, the sensitivity of CEUS was significantly higher than without contrast enhancement (83.8 vs 56.3%; p=0.004). There was no significant difference in the specificity (p=0.43) (Table 2).
CEUS in colorectal metastases
Forty-nine patients suspected of having colorectal metastases underwent laparotomy. Intraoperatively, 55.1% of all unenhanced sonograms were shown to be correct (n=27) while 79.6% of the CEUS examinations were accurate (n=39). During surgery, 14 patients exhibited 24 metastases close to the diaphragm in segments 7 and 8. Unenhanced sonography had only shown 11 of these in six patients. By using the contrast agent, correct detection was increased to 23 metastases in 13 patients. Similarly, metastases located along the ligamentum teres were detected more reliably when using contrast agent. During surgery, 18 metastases along the ligament were detected in 12 patients. By unenhanced sonography, six of these were seen in three patients, while CEUS detected 13 metastases in eight patients.
False negative findings were obtained by CEUS in six patients. In four of these patients, five additional metastases were found at surgery around the ligamentum teres, and one metastasis was found in each of segments 5 and 8.
In six patients, no metastases were found during surgery. Of those in two patients, the preoperative diagnosis of a metastasis-free liver was confirmed and the primary colorectal cancer was resected (true negative finding). In four patients, a local recurrence was suspected during follow-up after partial liver resection. CEUS showed suspicious lesions without contrast enhancement measuring up to 12 mm. However, during surgery, these areas were found to be cicatrices (false positive findings).
Thus, the additional information gained by using SonoVue is reflected in the significantly increased sensitivity (p=0.001) of liver metastasis detection as compared to unenhanced sonography. No difference was found regarding specificity (p=0.52) (Table 2).
CEUS in non-colorectal metastases
Fifty-one patients underwent surgery for non-colorectal metastases to the liver. The findings obtained by unenhanced sonography were verified by intraoperative exploration of the liver (including intraoperative sonography) in 78.4% (n=40) of the patients, while the findings obtained by CEUS were verified in 88.2% (n=45) of the patients. In 25 patients, the liver was found to be free of metastases intraoperatively, as predicted by both unenhanced and contrast-enhanced ultrasound (true negative findings). Of those, 23 had pancreatic cancer, one patient had cancer of the gallbladder, and one had gastric cancer. All of these patients underwent resection of the primary tumor.
The advantage of CEUS over unenhanced sonography in providing additional information was most evident in cases of superficial metastases and lesions along the ligamentum teres. Of nine superficial metastases discovered intraoperatively in seven patients, unenhanced sonography had detected only six in four patients. CEUS, however, predicted eight metastases in six patients. Along the round ligament, where 12 metastases were found in nine patients intraoperatively, unenhanced ultrasound only detected six metastases in four patients. CEUS identified ten metastases in seven patients.
False positive results were obtained in one patient, in which a scar after resection of a liver metastasis of a renal cell carcinoma was misinterpreted as recurrence. False negative results in five patients were observed despite the application of SonoVue. In two patients with pancreatic cancer, miliary metastases had not been detected by any preoperative imaging. In two patients, after thyroid carcinoma and renal cell carcinoma, respectively, one metastasis in each case in segment four close to the ligamentum teres was not detected sonographically. Furthermore, in one patient, a diffuse infiltrating non-Hodgkin lymphoma was not diagnosed by CEUS. In this case, the contrast-enhanced sonogram was interpreted as an irregularity in the distribution of adipose tissue. The lesion was biopsied. As no final diagnosis was determined by biopsy, open surgery was performed.
Thus, the sensitivity in the detection of non-colorectal liver metastases was raised from 60.0% in unenhanced sonography to 80.0% by using the contrast agent. However, there was no statistically significant difference (p=0.21) in the sensitivity between the two methods. The specificity remained unchanged at 96.2% (Table 2).
The origin of the metastases (colorectal vs non-colorectal) had no effect on detection rates by either unenhanced ultrasonography or CEUS (Table 3).
Discussion
Since the introduction of contrast-enhanced ultrasonography, a number of studies have demonstrated its safety. Side effects include dysesthesia at the site of injection, headache, nausea, rash, and symptoms of anaphylaxis [15, 23–25]. However, such side effects are described with a frequency of only about 0.002% in the literature [26]. In our patients, one anaphylactoid reaction with dyspnea required an inhaled beta-2-agonist and intravenous corticosteroid.
Besides known allergies, additional contraindications to SonoVue administration are unstable angina pectoris or an acute coronary syndrome within 7 days before the CEUS exam. Patients with these diagnoses have a markedly elevated risk of cardiac damage during anaphylactoid reactions [25].
The use of a contrast agent can double the time required for an ultrasound exam. However, in our opinion, the additional information obtained by CEUS outweighs this disadvantage. CEUS is very cost-effective, as the amount normally administered (2.4 ml) is available for 30–35 Euro.
Most studies, to date, have evaluated the ability of CEUS to differentiate various types of liver lesions and to detect liver metastases. However, in these studies, the reference methods used, are generally, other imaging procedures such as MRI or CT [27–32].
For our study, we chose intraoperative findings as the benchmark for the quality of the preoperative diagnosis. The intraoperative results were obtained by a combination of surgical examination with inspection and palpation and intraoperative ultrasound of the liver. According to Hölscher and Stadler (1989) [21] , this procedure achieves the highest detection rate for hepatic metastases. In 85 patients having 128 metastases, Hölscher reported the detection of 89 metastases by the combination of preoperative unenhanced ultrasound and CT scan (sensitivity: 48.5%, specificity: 93.3%). By intraoperative inspection palpation of the liver, 110 metastases were detected (sensitivity: 75.4%, specificity: 98.3%). Problems arose in detecting small metastases located deep within the parenchyma. Intraoperative unenhanced ultrasound, alone, revealed 120 metastases (sensitivity: 89.9%, specificity: 98.3%). However, by this method, the detection of superficial metastases became problematic. Thus, only the combination of inspection, palpation, and intraoperative ultrasound reached the highest detection rate with 127 correctly detected metastases (sensitivity: 100.0%, specificity: 98.3%) [21]. However, these results show that even this intraoperative “gold standard” cannot guarantee 100% reliability as, for example, it is unable to detect micrometastases [33].
In comparing unenhanced ultrasound and ultrasound with contrast agent vs intraoperative findings, CEUS showed a significant improvement in sensitivity in the detection of liver metastases from all primary cancers (p=0.001) and from colorectal cancer alone (p=0.004). No significant difference was observed for non-colorectal metastases. This is due to the smaller proportion of patients with such metastases and not the efficacy of CEUS. This is substantiated by the absence of statistically significant differences in sensitivity comparing the results of CEUS in the detection of colorectal vs non-colorectal metastases (Table 3).
Because of their subphrenic location, focal lesions, and in particular, metastases near the surface of segments 7 and 8 are often overlooked. This also applies to the subphrenic areas of segments 2 and 4a; it is well-known that it is difficult to detect focal metastases around the ligamentum teres [10, 33–35]. By using a contrast agent, the detection of metastases in these regions can be markedly improved [36]. This was verified in this study as well. The improved sonographic detection resulted, in most cases, from the identification of the metastases in the portal venous and late phase of the exam. In contrast to a sensitivity of 88.3% published by our group in 1998 [33], the present study shows poorer sensitivity (56.3%) of unenhanced ultrasound in the detection of liver metastases. A reason for this discrepancy is the high percentage of patients included in this study who had already undergone adjuvant chemotherapy at the time of examination. The detection of liver metastases is dependent upon differences between the impedances of the metastases and the surrounding normal liver tissue. Preoperative chemotherapy is known to render unenhanced ultrasound of the liver more difficult, as it decreases the differences in the impedance [33]. In our study, the use of the ultrasound contrast agent in these patients revealed an additional 11 metastases (52.4%) in six out of 14 patients undergoing surgery. Therefore, we are of the opinion that the patients most likely to profit from CEUS are those who have been given chemotherapy.
Both unenhanced and enhanced ultrasonography achieved a very high specificity (96.2%) in the group of patients with non-colorectal metastases. This is mainly due to the high number of correct negative findings which led to surgery for the primary cancer (e.g., a pancreatic carcinoma). In contrast, the specificities for the two ultrasonographic methods in the group of patients with colorectal metastases is comparably low (50 and 66%). The reason for this is a very low number of true negative findings. Small alterations in these numbers impart a large difference in the specificity. Hence, the significance of the calculated specificity for CEUS for colorectal and non-colorectal metastases should not be overestimated.
Liver metastases smaller than 10 mm remain very difficult to detect by preoperative staging methods. We, like other authors, confirm the benefits of contrast-enhanced ultrasonography in the detection of these small nodular metastases. In our study, the detection rate was increased by 65% (13 metastases) with the use of a contrast agent as compared to unenhanced sonography in patients with such lesions. According to literature, CEUS improves the number of detected small nodular metastases by 22–82%. It has been shown that metastases larger than 5 mm are, generally, easily identified when contrast agent is used, and even metastases smaller than 5 mm are frequently detected [16, 20, 38–41]. More studies of CEUS are needed with patients at risk for small miliary metastasis (e.g., pancreatic carcinoma). This group of patients could benefit greatly from CEUS when liver metastases are detected, as unnecessary laparotomies could, thereby, be avoided.
Conclusion
CEUS of the liver with SonoVue provides a significantly higher sensitivity in the detection of liver metastases as compared to unenhanced sonography and identifies up to 40% more of metastases. This is mainly due to improved detection of metastases in the superficial subphrenic areas and around the ligamentum teres. Especially with small nodular metastases and after chemotherapy, patients benefit from the additional information obtained by CEUS. Particularly in these patients, we consider contrast-enhanced ultrasound to be an indispensable part of modern treatment.
References
Tocchi A, Mazzoni G, Brozzetti S, Miccini M, Cassini D, Bettelli E (2004) Hepatic resection in stage IV colorectal cancer: prognostic predictors of outcome. Int J Colorectal Dis 19:580–585
Konopke R, Saeger H-D (2003) Lebermetastasen: Diagnostik und Therapie 74:866–886
Scheele J, Altendorf-Hofmann A, Grube T, Hohenberger W, Stangl R, Schmidt K (2001) Resection of colorectal liver metastases. What prognostic factors determine patient selection? Chirurg 72:547–560
Luque-de Leon E, Tsiotos GG, Balsiger B, Barnwell J, Burgart LJ, Sarr MG (1999) Staging laparoscopy for pancreatic cancer should be used to select the best means of palliation and not only to maximize the resectability rate. J Gastrointest Surg 3:111–117
Sakorafas GH, Tsiotou AG (1999) Surgical palliation of pancreatic cancer. Eur J Surg Oncol 25:556
Adam R (2003) Chemotherapy and surgery. New perspectives on the treatment of unresectable liver metastases. Ann Oncol 14(Suppl 2):ii13–ii16
Nakamura S, Suzuki S, Baba S (1997) Resection of liver metastases of colorectal carcinoma. World J Surg 21:741–747
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH (1999) Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis consecutive cases. Ann Surg 230:309–318
Nordlinger B, Guiguet M, Vaillant JC, Balladur P, Boudjema K, Bachellier P, Jaeck D (1996) Surgical resection of colorectal carcinoma metastases to the liver. A prognostic scoring system to improve case selection, based on 1568 patients. Association Francaise de Chirurgie. Cancer 77:1254–1262
Bernatik T, Strobel D, Hahn EG, Becker D (2001) Detection of liver metastases: comparison of contrast-enhanced wide-band harmonic imaging with conventional ultrasonography. J Ultrasound Med 20:509–515
Eberhardt S, Choi P, Bach A, Funt S, Felderman H, Hann L (2003) Utility of sonography for small hepatic lesions found on computed tomography in patients with Cancer. J Ultrasound Med 22:335–343
Jang HJ, Lim HK, Lee WJ, Kim SH, Kim KA, Kim EY (2000) Ultrasonographic evaluation of focal hepatic lesions: comparison of pulse inversion harmonic, tissue harmonic and conventional imaging techniques. J Ultrasound Med 19:293–299
Fevery J, Baert AL, Marchal GM, Broeckaert L, De Groote J, Vantrappen G (1985) The value of computed tomography, ultrasonography, and peritoneoscopy with biopsy in the detection of liver metastases secondary to gastro-enterological tumors. Acta Gastroenterol Belg 48:105–110
Schreve RH, Terpstra OT, Ausema L, Lameris JS, van Seijen AJ, Jeekel J (1984) Detection of liver metastases. A prospective study comparing liver enzymes, scintigraphy, ultrasonography and computed tomography. Br J Surg 71:947–949
Dietrich Ch, Becker D (2002) Signalverstärkte Farbdopplersonographie des Abdomens. Byk Gulden, Konstanz
Albrecht T (2003) Contrast medium-supported sonography of the liver—a challenge to German radiology. Rofo 175:889–891
Hohmann J, Skrok J, Puls R, Albrecht T (2003) Characterization of fokal liver lesion with contrast-enhanced low MI real time ultrasound and SonoVue. Fortschr Röntgenstr 175:835–843
von Herbay A, Vogt C, Willers R, Haussinger D (2004) Real-time imaging with the sonographic contrast agent SonoVue: differentiation between benign and malignant hepatic lesions. J Ultrasound Med 23:1557–1568
Youk JH, Kim CS, Lee JM (2003) Contrast-enhanced agent detection imaging. Value in the characterisation of focal hepatic lesions. J Ultrasound Med 22:910–987
Solbiati L, Tonolini M, Cova L, Goldberg N (2001) The role of contrast-enhanced ultrasound in the detection of focal liver lesions. Eur Radiol 11(suppl 3):E15–E26
Hölscher AH, Stadler J (1989) Intraoperative Sonographie zum Nachweis occulter Lebermetastasen beim kolorektalen Carzinom. Langenbecks Arch Chir 374:363–369
Vogl TJ, Schwarz W, Blume S et al (2003) Preoperative evaluation of malignant liver tumours: comparison of unenhanced and SPIO (Revovist)-enhanced MR imaging with biphasic CTAP and intraoperative US. Eur Radiol 13:262–272
Bokor D, Chambers JB, Rees PJ, Mant TG, Luzzani F, Spinazzi A (2001) Clinical safety of SonoVue, a new contrast agent for ultrasound imaging, in healthy volunteers and in patients with chronic obstructive pulmonary disease. Invest Radiol 36:104–109
Morel DR, Schwieger I, Hohn L, Terrettaz J, Llull JB, Cornioley YA, Schneider M (2000) Human pharmacokinetics and safety evaluation of SonoVue, a new contrast agent for ultrasound imaging. Invest Radiol 35:80–85
de Groot MC, van Zwieten-Boot BJ, van Grootheest AC (2004) Severe adverse reactions after the use of sulphur hexafluoride (SonoVue) as an ultrasonographic contrast agent. Ned Tijdschr Geneeskd 148:1887–1888
Torzilli G (2005) Adverse effects associated with SonoVue use. Expert Opin Drug Saf 4:399–401
Wilson SR, Burns PN, Muradali D, Wilson JALai X (2000) Harmonic hepatic US with microbubbles contrast agent: initial experience showing improved characterization of hemangioma, hepatocellular carcinoma and metastases. Radiology 215:153–161
Strobel D, Hoefer A, Martus P, Hahn EG, Becker D (2001) Dynamic contrast-enhanced power Doppler sonography improves the differential diagnosis of liver lesions. Int J Colorectal Dis 16:247–256
Basilico R, Blomley MJ, Harvey CJ et al (2002) Which continuous US scanning mode is optimal for the Detection of vascularity in liver lesions when enhanced with the second generation contrast agent. Eur J Radiol 41:184–191
Leen E (2001) The role of contrast-enhanced ultrasound in the characterisation of fokal liver lesions. Eur Radiol 11(suppl. 3):E27–E34
Kim TK, Choi BI, Han JK, Hong HS, Park SH, Moon SG (2000) Hepatic tumors: contrast agent-enhancement patterns with pulse-inversion harmonic US. Radiology 216:411–417
Albrecht T, Blomley MJ, Burns PN et al (2003) Improved detection of hepatic metastases with pulse-inversio US during the liver-specific phase of SHU 508A: multicenter study. Radiology 227:361–370
Bunk A, Stolben E, Konopke R, Nagel M, Saeger H-D (1998) Color Doppler sonography in liver surgery. Status of perioperative monitoring. J Ultrasound Med 19:202–212
Gross M, Zoller WG (1995) Ultrasound criteria versus histology. Bildgebung 62:25–30
Bernatik T, Becker D, Neureiter D et al (2003) Detection of liver metastases—comparison of contrast-enhanced ultrasound using first versus second generation contrast agents. J Ultrasound Med 24:175–179
Konopke R, Kersting S, Saeger H-D, Bunk A (2005) Detection of liver lesions by contrast-enhanced ultrasound—comparison to intraoperative findings. Ultraschall Med 26:107–113
Schuessler G, Ignee A, Hirche T, Dietrich CF (2003) Improved detection and characterisation of liver tumors with echo-enhanced ultrasound. Z Gastroenterol 41:1167–1176
Lencioni R, Cioni D, Crocetti L et al (2002) Ultrasound imaging of focal liver lesions with a second-generation contrast Agent. Acad Radiol 9(suppl 2):371–374
Harvey CJ, Blomley MJ, Eckersley RJ, Heckemann RA, Butler-Barnes J, Cosgrove DO (2000) Pulse-inversion mode imaging of liver specific microbubbles: improved detection of subcentimetre metastases. Lancet 355:807–808
Dalla Palma L, Bertolotto M, Quaia E, Locatelli M (1999) Detection of liver metastases with pulse inversion harmonic imaging: preliminary results. Eur Radiol 9(suppl 3):382–387
Kockerling F, Schug-Pass C, Weskott HP, Tatchen R (2000) Malignant hepatobiliary tumors. Surgical requirement concerning preoperative diagnosis. Zentralbl Chir 125:616–623
Author information
Authors and Affiliations
Corresponding author
Additional information
Dr. Konopke and Dr. Kersting contributed equally to this work.
Rights and permissions
About this article
Cite this article
Konopke, R., Kersting, S., Bergert, H. et al. Contrast-enhanced ultrasonography to detect liver metastases. Int J Colorectal Dis 22, 201–207 (2007). https://doi.org/10.1007/s00384-006-0134-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-006-0134-5