Abstract
Background
Dysplasia, carcinoma in situ, and other malignant transformation or premalignant/malignant histopathology (PMMH) seem uncommon in pediatric choledochal cyst (CC). A literature review and the authors’ experience are presented.
Methods
All reports about PMMH in CC patients 15 years old or younger published in English and all cases of PMMH in specimens excised from CC patients 15 years old or younger by the authors were reviewed.
Results
Of 20 published reports, PMMH was adenocarcinoma (n = 4), sarcoma (n = 4), and dysplasia (n = 12). Treatment for malignancies was primary pancreaticoduodenectomy (PD; n = 2) or cyst excision/hepaticojejunostomy (Ex/HJ; n = 6). Outcomes at the time of writing for malignancies: 2 deaths, 4 survivors after follow-up of 2 years, and 2 lost to follow-up. No dysplasia case has undergone malignant transformation. The authors have experienced 7 cases of PMMH; adenocarcinoma in situ (AIS; n = 1) and dysplasia (n = 6).
Conclusions
The present study identified the youngest cases of AIS and dysplasia from specimens excised when they were 3 years old and 4 months old, respectively. Both are published for the first time as evidence that PMMH can complicate CC in young patients. Long-term protocolized postoperative follow-up is mandatory when PMMH is diagnosed in pediatric CC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Irwin and Morison [1] and Ferraris et al. [2] reported an association between choledochal cyst (CC) and malignancy, premalignant/malignant histopathology (PMMH) defined as dysplasia, carcinoma in situ, and other malignant transformation. PMMH has been identified in excised specimens from adult CC patients [3,4,5], but specific data for pediatric CC patients are lacking. In the present study, PMMT cases published in the English language literature and the authors’ experience were reviewed and two cases presented to improve knowledge about PMMT in pediatric CC.
Methods
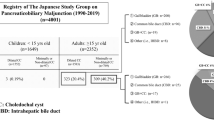
Systematic searches of English-language articles were conducted using the PubMed database developed and maintained by the National Center for Biotechnology Information at the US National Library of Medicine (NLM), located at the national Institutes of Health (NIH). PubMed facilitates searching across several NLM literature resources such as MEDLINE, PubMed Central, and Bookshelf. Keywords used were choledochal cyst, pancreaticobiliary maljunction (PBMJ), malignancy, cholangiocarcinoma, dysplasia, and pediatric. Pediatric was defined as up to and including 15 years old at the time of cyst excision (Ex) and hepaticoenterostomy biliary tract reconstruction, usually hepaticojejunostomy (HJ) at the authors’ institutes. All searches were performed on August 27 and 28 in 2023.
The authors also reviewed all pediatric CC patients who had histopathologic evidence for PMMT in excised CC and gallbladder specimens between 2001 and 2023. For histopathologic examination, hematoxylin–eosin (H&E) staining and in recent cases, S-100protein, maspin, and IMP3 immunohistochemical staining to distinguish between dysplasia and benign epithelium in the biliary tree were employed.
Results
Literature review
Table 1 summarizes published cases. There were 20 reports of PMMH in pediatric CC patients aged up to and including 15 years old; 8 cases of malignancy (4 adenocarcinoma and 4 sarcoma) and 12 cases of dysplasia. All PMMH were identified in CC specimens. For treatment of the 8 published malignancy cases, primary pancreaticoduodenectomy was performed in 2 cases because adenocarcinoma was confirmed on intraoperative histopathologic diagnosis (published case 4) and a metastatic lesion was confirmed preoperatively (published case 5). For the other 6 published malignant cases, Ex and choledochojejunostomy or HJ were performed because a definitive histopathologic diagnosis of malignancy was not made intraoperatively. Six published malignant cases (cases 1 to 6) had adjuvant chemotherapy. Details for cases 7 and 8 are unknown. At the time of writing, 2 of the published malignant cases were dead, 4 were alive but had only been followed up for less than 2 years, cases 7 and 8 were lost to follow-up.
Published cases 9–20 all had dysplasia in excised CC specimens diagnosed after definitive Ex/HE. At the time of writing, no malignant transformation has been reported in any dysplasia case after follow-up ranging from 1 to 3 years.
The authors’ experience
At the time of writing, 7 cases of PMMH have been identified in 169 CC cases (4.1%) treated by the authors at their institutes between 2001 and 2023 (Table 2). One case was adenocarcinoma in situ (AIS) and 6 were dysplasia. Histopathologic diagnosis of PMMH was made after Ex/HJ in all 7 cases. PMMT was identified in excised CC (n = 4), excised gall bladder (GB; n = 2) and both (CC + GB; n = 1). Immunohistochemistry using S-100P, maspin, and IMP3 was performed on tissue from the 4 dysplasia cases; excised CC PMMH lesions were positive for maspin and IMP3 and negative for S-100P (n = 3; author cases 5, 6, and 7). All PMMH cases were diagnosed after Ex/HJ from histopathologic assessment of excised specimens. Despite being diagnosed with PMMH, none have received adjuvant chemotherapy and at the time of writing, all 7 PMMH cases were alive and well. None of the authors’ cases have been published. The AIS case (authors’ case 1) and one dysplasia case (authors’ case 6) are presented.
Authors’ case 1
A 3-year-2-month-old boy was admitted for suspected pancreatitis. At presentation, serum amylase (AMY) (133 IU/L) and lipase (LIP) (529 IU/L) were elevated, but serum direct bilirubin, aspartate aminotransferase (AST), alanine aminotransferase (ALT), and γ-glutamyl transpeptidase (GGTP) were all within reference ranges. Magnetic resonance cholangiopancreatography (MRCP) identified PBMJ and cystic CC without dilated intrahepatic bile ducts. There were no other remarkable findings on MRCP or ultrasonography (US). Laparoscopic Ex with HJ was performed. Histopathology of the excised CC identified an increase in the number of glandular lumens associated with carcinogenesis, as well as back-to-back glands. In this lesion, cells showed anisokaryosis, irregular nuclei, and cloudy mucus within the cytoplasm, typical findings of AIS (Fig. 1). Proximal and distal margins of the excised CC were negative for evidence of malignancy. Although adjuvant chemotherapy was not performed, follow-up has been more intensive because of the diagnosis of AIS. MRCP and US have continued to be unremarkable for almost 13 years; he is currently almost 16 years old and well.
Histopathology: authors’ case 1. A Open arrowheads show an increase in the number of glandular lumens associated with carcinogenesis, as well as back-to-back glands. B Cells show anisokaryosis, irregular nuclei (red arrows), and cloudy mucus within the cytoplasm (open arrowheads). C Cells show no anisokaryosis. D Irregular nuclei and mucus within the cytoplasm are not seen
Authors’ case 6
A 7-day-old girl was admitted for suspected CC on routine abdominal echography. Biochemistry identified elevated serum direct bilirubin (18.2 mg/dL), AST (50 IU/L), and GGTP (272 IU/L). AMY and LIP were within reference ranges. She underwent tube drainage of the CC on day 10 of life, followed by Ex with HJ at 4 months old. Histopathology showed micropapillary architecture, and loss of cellular polarity, anisokaryosis, and hyperchromasia on H&E staining. Immunohistochemical examination revealed diffuse, intermediate to strong cytoplasmic staining for IMP3, and diffuse, strong, and combined nuclear/cytoplasmic staining patterns for maspin (Fig. 2), indicating dysplasia of the mucosa of CC. She has been well postoperatively and is currently 20 months old.
Discussion
Although a few PMMH cases complicating pediatric CC have been reported, the authors have expanded the data base for PMMH in pediatric CC from 21 to 27 by presenting the youngest case of AIS diagnosed in an excised specimen from a 3-year-2-month-old boy followed-up for more than 10 years, and the youngest case of dysplasia diagnosed in an excised specimen from a 4-month-old girl.
CC is known as being one of the high-risk factors for the development of carcinoma of the biliary tract ranging from 2.5% to 30% for all age groups [13,14,15] because of its association with PBMJ. However, reports of pediatric cases are rare. It has been considered that reflux of pancreatic secretions into bile causes inflammation, repeated cycles of damage and healing of the biliary epithelium, and can promote malignant transformation [16]. In fact, disrupted mucosa of excised CC was observed next to the lesion of AIS in the authors’ case 1 (Fig. 3). Patients with CC develop malignancies at a younger age compared with cholangiocarcinoma patients (median: 49.5 years versus 65 years, respectively) [3, 17]. Moreover, Gao R, et al. reported that age, recurrent attacks of biliary pancreatitis, symptom duration, cyst diameter, and history of biliary surgery are individual risk factors for premalignant lesions in younger aged CC patients [12]. However, 2 malignant cases (published case 6 [11] and authors’ case 1) and 5 dysplasia cases (authors’ cases 2, 3, 4, 6, and 7) were all less than 5 years old when specimens were excised. As a result, it would be prudent for an entire excised specimen to be examined thoroughly by skilled pathologists with immunochemistry such as S-100P, maspin, and IMP3 as well as more traditional staining techniques to distinguish between dysplasia and benign epithelium in the biliary tree precisely [18, 19]. The present study should encourage pediatric surgeons to have a high index of suspicion for carcinogenesis in younger CC patients and foster acceptance that CC has an oncologic aspect that has not been a routine focus of management or follow-up to date.
Although Ex and HE are generally accepted as standard surgical intervention for CC, published cases 4 and 5 had pancreaticoduodenectomy and both cases can be considered as unique examples of malignancies complicating CC; in fact, in published case 4, a slightly elevated lesion was present and biopsied. The general consensus can be summarized by Saikura et al. [11] who advocated early radical surgery combined with thorough intraoperative histopathology examination once CC was diagnosed. Minimally invasive surgery using laparoscopy with 4 K imaging [20] as well as intraoperative endoscopy performed routinely by the authors, even during laparoscopic Ex and HE to examine the common channel, CC, and intrahepatic bile duct [21] for debris and calculi have improved surgery for CC. Intraoperative endoscopy is excellent for careful mucosal examination and irrigation during Ex.
This study has clinical impact by providing evidence for the existence PMMH in pediatric CC. To the best of the authors’ knowledge, there is only 1 report specifically about PMMH in pediatric CC, Gao, et al. [13] who reported 12/210 CC cases (5.7%) with dysplasia and no reports investigating the incidence of PMMH in excised specimens from adults with CC. By comparing Gao’s data with the authors’ experience where PMMH was identified in 7/169 CC cases (4.1%), it would appear that the incidence of PMMH in pediatric CC is of the order of 5%, which is not low compared with reported incidences ranging from 2.5% to 30% for all age groups [13,14,15]. This result is noteworthy because it was unexpectedly high and surgeons should be aware of PMMH in young children less than 3 years old with CC. The importance of thorough histopathologic examination and meticulous protocolized follow-up are mandatory for managing pediatric CC patients thoroughly and safely.
Data availability
The datasets generated and/analyzed during current study are available from the corresponding author on reasonable request.
References
Irwin ST, Morison JE (1944) Congenital cyst of the common bile-duct containing stones and undergoing cancerous change. Br J Surg 32:319
Ferraris LV, Navarro A, Malbran JE (1944) Dilatation congenital del hepatocodedoco y adenocarcinoma. Bol Soc Cir Cordaba 5:21
Ten Hove A, de Meijer VE, Hulscher JBF, de Kleine RHL (2018) Meta-analysis of risk of developing malignancy in congenital choledochal malformation. Br J Surg 105:482–490. https://doi.org/10.1002/bjs.10798
Banales JM, Cardinale V, Carpino G, Marzioni M, Andersen JB, Invernizzi P (2016) Expert consensus document: cholangiocarcinoma: current knowledge and future perspectives consensus statement from the European network for the study of cholangiocarcinoma (ENS-CCA). Nat Rev Gastroenterol Hepatol 13:261–280. https://doi.org/10.1038/nrgastro.2016.51
Clements O, Eliahoo J, Kim JU, Taylar-Robinson SD, Khan SA (2020) Risk factors for intrahepatic and extrahepatic cholangiocarcinoma: a systematic review and meta-analysis. J Hepatol 72:95–103. https://doi.org/10.1016/j.jhep.2019.09.007
Tsuchiya R, Harada N, Ito T, Furukawa M, Yoshihiro I, Kusano T, Uchimura M (1976) Malignant tumors in choledochal cysts. Ann Surg 186:22–28
Iwai N, Deguchi E, Yanagihara J, Iwai M, Matsuo H, Todo S, Imashuku S (1990) Cancer arising in a choledochal cyst in a 12-year-old girl. J Pediatr Surg 25:1261–1263
Patil KK, Omojola MF, Khurana P, Iyengar JK (1992) Embryonal rhabdomyosarcoma within a choledochal cyst. Can Assoc Radiol J 43:145–148
Tanaka S, Kubota M, Yagi M, Okuyama A, Ohtaki M, Yamazaki S, Hirayama Y, Kurosaki I, Hatakeyama K (2006) An 11-year-old male patient demonstrating cholangiocarcinoma associated with congenital biliary dilatation. J Pediatr Surg 41:e15-19
Nakamura H, Katayose Y, Rikiyama T, Onogawa T, Yamamoto K, Yoshida H, Hayashi H, Ohtsuka H, Hayashi Y, Egawa S (2008) Advanced bile duct carcinoma in a 15-year-old patient with pancreaticobiliary maljunction and congenital biliary cystic disease. J Hepatobiliary Pancreat Surg 15:554–559
Saikura N, Naito S, Iinuma Y, Ohtani T, Yokoyama N, Nitta K (2009) Invasive cholangiocarcinoma identified in congenital biliary dilatation in a 3-year-old boy. J Pediatr Surg 44:2202–2205
Gao R, Ke M, Shi J, Zhang Y, Zou J, Diao M, Li L (2023) Establishment and validation of a predictive nomogram for the risk of premalignant lesions in children with choledochal cyst. Front Pediatr 11:1108788. https://doi.org/10.3389/fped.2023.1108788
Sastry AV, Abbadessa B, Wayne MG, Steele JG, Cooperman AM (2015) What is the incidence of biliary carcinoma in choledochal cyst, when do they develop, and how should it affect management? World J Surg 39:487–492
Mukai M, Kaji T, Masuya R, Yamada K, Sugita K, Moriguchi T (2018) Long-term outcome of surgery for choledochal a single-institution study focusing on follow-up and late complications. Surg Today 48:835–840
Madadi-Sanjani O, Wirth TC, Kuebler JF, Petersen C, Ure BM (2019) Choledochal cyst and malignancy: a plea for lifelong follow-up. Eur J Pediatr Surg 29:143–149
Shimada K, Yanagisawa J, Nakayama F (1991) Increased lysophosphatidylcholine and pancreatic enzyme content in bile of patients with anomalous pancreaticobiliary ductal junction. Hepatology 13:438–444
Mihalache F, Tantau M, Diaconu B, Acalovchi M (2010) Survival and quality of life of cholangiocarcinoma patients: a prospective study over a 4-year period. J Gastrointesin Liver Dis 19:285–290
Levy M, Lin F, Xu H, Dhall D, Spaulding BO, Wang HL (2010) S100P, von Hippel-Lindau gene product, and IMP3 serve as a useful immunohistochemical panel in the diagnosis of adenocarcinoma on endoscopic bile duct biopsy. Human Pathol 41:1210–1219
Chen L, Haung K, Himmelfarb EA, Zhai J, Lai JP, Lin F, Wang HL (2015) Diagnostic value of maspin in distinguishing adenocarcinoma from benign biliary epithelium on endoscopic bile duct biopsy. Human Pathol 46:1647–1654
Koga H, Ochi T, Seo S, Miyake Y, Lane GJ, Yamataka A (2022) Comparison of 2K and 4K imaging systems for choledochal cyst in children. J Pediatr Surg 57:235–238
Miyano G, Koga H, Shimotakahara A, Takahashi T, Kato Y, Lane GJ, Okazaki T, Yamataka A (2011) Intralaparoscopic endoscopy: its value during laparoscopic repair of choledochal cyst. Pediatr Surg Int 27:462–466
Author information
Authors and Affiliations
Contributions
T.O. and A.Y. wrote the main manuscript text. All authors performed clinical data collection. Y.F. performed histopathologic examination. G.L. made English corrections. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Okazaki, T., Nikai, K., Koga, H. et al. Premalignant/malignant histology in excised choledochal cyst specimens from children. Experience and literature review. Pediatr Surg Int 40, 5 (2024). https://doi.org/10.1007/s00383-023-05582-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s00383-023-05582-z