Abstract
Objective
Intussusception secondary to pathologic lead points (PLPs) is a challenging condition for pediatric surgeons, and few studies have been published on this subject. The aim of this study was to review and analyze clinical data on the diagnosis and management of intussusception secondary to PLPs in children.
Methods
Between 2002 and 2016, a total of 65 pediatric patients with a diagnosis of intussusception secondary to PLPs were retrospectively reviewed.
Results
The series comprised 47 males and 18 females. The average age of the patients was 4.9 years old. All patients had typical clinical manifestations, and intussusception was proven by ultrasound. Fifty-one patients had recurrent intussusception, of whom 21 had one, 14 had two, 10 had three, and 6 had more than three. There were 20 episodes of recurrence within 24 h (39.2%), 15 episodes were found between 24 and 72 h (29.4%), and the remaining 31.4% (16/51) of recurrences occurred after 72 h. All patients received surgical intussusception reduction. Meanwhile, enterectomy was the procedure of choice in 55 patients, polypectomy in 5 patients, and cystectomy in 3 patients. The types of intussusception secondary to PLPs included small intestinal (n = 25), ileocolic (n = 19), ileocecal (n = 11), ileo–ileocolic (n = 9) and cecalcolic (n = 1). The types of PLPs included Meckel diverticulum (n = 32), intestinal duplication (n = 14), benign polyps (n = 5), malignant lymphoma (n = 4), Peutz–Jeghers syndrome (n = 3), mesenteric cyst (n = 3), intestinal wall hematoma of hemophilia (n = 2), allergic purpura (n = 1), and hamartoma (n = 1). All patients recovered well with no relapse during follow-up, except for one patient who had an intestinal obstruction from adhesions that occurred approximately 3 months after discharge and who was curable after conservative treatment.
Conclusions
Intussusception secondary to PLPs tends to exhibit recurrence. There are various types of intussusception secondary to PLPs. It is necessary to improve auxiliary examinations to identify the etiology and avoid intraoperative omission. Surgical reduction of intussusception secondary to PLPs is the preferred clinical management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intussusception is the most common abdominal emergency and leading cause of intestinal obstruction in young children [1,2,3]. Most cases were found to be idiopathic, and secondary intussusception (SI) caused by PLPs accounts for approximately 6% of cases [4]. Children with SI generally present with different manifestations and various causes [5]. Non-surgical reduction by air or barium enema has become the preferred first-line treatment for most cases of idiopathic intussusception [6]. However, for those SIs, surgical treatment is ultimately required. Identification and treatment of SI at an early stage would spare patient injury caused by repeated unnecessary enemas and improve prognosis. If inappropriately managed, it can result in serious complications, such as bowel perforation and secondary peritonitis, which can be life-threatening in extreme cases. The clinical diagnosis of intussusception is relatively easy, but further diagnosis of SI and clarification of the cause is rather difficult. In this study, we reviewed a series of 65 pediatric intussusceptions secondary to PLPs treated at our institute over the last 15 years, analyzing the clinical data and suggesting a strategy for diagnosis and treatment.
Materials and methods
Patients
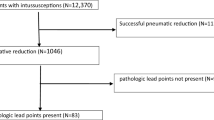
Between January 2002 and December 2016, a total of 11,025 pediatric patients with intestinal intussusception were treated in our hospital. Most of the cases had a successful air enema reduction and 986 cases underwent laparotomy. A total of 65 operated intussusception cases secondary to PLPs were ultimately included in this research.
Methods
The demographic and clinical features of those patients were retrospectively reviewed. The ultimate diagnosis was made post-operation from the tissue sections resected by a pathologist. The study was approved by the Ethics Committees of the Second Affiliated Hospital and Yuying Children’s Hospital of Wenzhou Medical University.
Results
Clinical features of intussusception secondary to PLPs
From 2002 to 2016, 47 male and 18 female pediatric patients were diagnosed with intussusception secondary to PLPs. The clinical features of our patients are shown in Table 1. Patients’ ages ranged from 2 months to 12 years, with a median age of 4.9 years old. The breakdown of cases showed that 21.5% were <2 years of age, 47.7% were between 2 and 5 years of age, and 30.8% were >5 years of age. All patients underwent emergency admissions with obvious signs and symptoms. In 52 patients (80%), the main clinical symptoms were intermittent crying or abdominal pain. Vomiting was also another common symptom, which occurred in 42 patients (64.6%). Fifteen patients (23.1%) also had bloody stool. The duration of symptoms ranged from several hours to 3 days, with or without increasing severity. Nearly half of the patients (52.3%) had typical signs of a palpable mass in the right abdomen.
Ultrasonography (US) was performed in all patients, and intussusception was proven by US. However, PLPs were observed in only four patients on US. Ten patients underwent computed tomography (CT) scans for further diagnosis, and five patients had positive results. Fifteen patients were also examined by Technetium-99 m pertechnetate scans. Among these, six patients had positive results. Routine blood tests were performed in all patients, and an elevated white blood cell count was found in 30 (46.2%) patients.
Features of 51 recurrent intussusceptions secondary to PLPs
All 65 patients were initially reduced by air reduction enema. Recurrent intussusception was defined as that the patient presented typical clinical symptoms again after a successful air reduction enema and intussusception was confirmed by US. Of these, 14 failed to reduce and 51 were reduced successfully in the first reduction. The remnant 51 recurrence patients were treated again with air reduction enema, and 33 ultimately failed to reduce. As shown in Table 2, 51 patients were found to have a recurrence after reduction during the follow-up, including 21 who had one, 14 who had two, 10 who had three, and 6 who had more than three. There were 20 episodes of recurrence within 24 h (39.2%), 15 episodes were found between 24 and 72 h (29.4%), and the remaining 31.4% (16/51) of recurrences occurred after 72 h.
The types of intussusception secondary to PLPs
All patients received laparotomy under general anesthesia, and the surgical procedure was chosen by the surgeon according to intraoperative findings. The basic operation was intussusception reduction. Meanwhile, enterectomy and enteroanastomosis was the procedure of choice in 55 patients, polypectomy in 5 patients, cystectomy in 3 patients, and only intussusception reduction in 2 patients. Based on the anatomic location of the surgical findings, all cases of intussusception were divided into five different types: small intestinal, ileocolic, ileocecal, ileoileocolic and cecalcolic. The type of intussusception was shown in Table 3.
PLPs in patients with intussusception
PLPs were found during the operation (Table 4). The main types of PLPs included Meckel diverticulum (n = 32) and intestinal duplication (n = 14). Other less frequent PLPs included five benign polyps (four ileal polyps and one colic polyp), four malignant lymphoma (two Burkitt’s lymphoma, one diffuse large B cell lymphoma and one T cell large granular lymphocyte leukemia), three Peutz–Jeghers syndrome, three mesenteric cysts, two intestinal wall hematoma of hemophilia, one allergic purpura and one hamartoma.
Patients with malignant lymphoma were treated with conventional chemotherapy receiving surgery in the hematology department. All patients recovered well with no relapse during follow-up, except for one patient who had an intestinal obstruction from adhesions that occurred approximately 3 months after discharge and who was curable after conservative treatment.
Discussion
Intussusception is a gastrointestinal condition that describes the involution of a proximal portion of the bowel into a more distal portion, often leading to bowel obstruction [7]. The vast majority of intussusception cases are primary. A few cases of intussusception are secondary, caused by PLPs, and are relatively difficult to diagnose before surgery. In our study, we found that there were more male patients than female patients, with a male:female ratio of 4:1. This is higher than the global male:female ratio of intussusception cases [8]. We also found that those >2 years old, especially between 2 and 5 years of age, were more likely to have PLPs than those <2 years old. This was different from previous studies. Blakelock et al. reported that 60% of cases of PLPs occurred in children 5–14 years of age [9].
Intussusception secondary to PLPs has a wide spectrum of clinical presentations that lack specificity. Those presentations are similar to primary intussusception. In general, intermittent abdominal pain is the main clinical symptom. The presentation of infants, especially those younger than 2 years old, is mainly intermittent noisy crying in lieu of abdominal pain. Other symptoms were gastrointestinal in nature and included vomiting, bloody stools and abdominal distention. Examining children, the right lower quadrant seemed empty, but a tender mass was felt in most cases. In our study, 52 patients had the main symptoms of intermittent crying or abdominal pain and 34 patients had typical signs of a palpable mass in the right abdomen.
Preoperative auxiliary examination must not be limited to the diagnosis of intussusception, but must aim at searching for a lead point. Because it is easy and inexpensive, US was employed as a routine imaging tool for intussusception. In the study by Daneman [10], ultrasound was shown to be the most basic diagnostic method and was able to diagnose two thirds of PLP cases. According to Zhang Y et al.’s study [11], US can be used as a feasible and effective method to discriminate PI from SI. In our series, all intussusception cases could be detected by US. However, it is difficult to diagnose PLPs. PLPs were observed in only four patients on US. This may be related to the techniques of the ultrasound physicians. Meanwhile, its sensitivity and specificity were not as good as those of CT. In our study, 50% of patients showed PLPs on CT. However, many patients directly underwent emergency surgery because of the failure of reduction enema. The most useful method for the detection of Meckel’s diverticulum is the Technetium-99 m pertechnetate scan. It has a sensitivity of 80–90%, a specificity of 95% and an accuracy of 90% in children [12]. In our study, patients with greater than or equal to three episodes of intussusception underwent a Technetium-99 m pertechnetate scan. 16 (24.6%) patients were diagnosed intussusception secondary to PLPs prospectively. In all, for those older than 2 years with recurrent intussusception, it is necessary to improve auxiliary examinations before the operation. The scan can not only preoperatively identify the etiology of intussusception but also avoid intraoperative omission.
Intussusception secondary to PLPs tends to exhibit recurrence. The overall recurrence rate of all intussusception cases is extremely variable depending on the series, ranging from 2 to 20% [13,14,15,16]. In our study, 78.5% patients with intussusception secondary to PLPs were found to have a recurrence after the first episode, which is higher than those with primary intussusception. Among these patients, 30 (58.8%) patients had greater than or equal to three episodes of intussusception, with a maximum of seven. Meanwhile, we found that the time interval of recurrence ranged from 6 h to 7 months. Some studies showed that intussusception within less than 12 h is due to incomplete reduction [17, 18]. Our results indicated that it may be related to PLPs. We also found that 39.2% of recurrences occurred within 24 h and 68.6% within 72 h, which suggested that close monitoring for 72 h after the initial reduction should also be recommended to the parents.
Non-surgical reduction is the first treatment for intussusception secondary to PLPs, except when there is a contraindication to non-surgical reduction or a definite presence of PLPs. Intussusception secondary to PLPs eventually requires surgery to cure. Surgical methods also vary and include intussusception reduction, polypectomy, cystectomy, enterectomy and enteroanastomosis. Laparoscopic surgery is also a safe and minimally invasive surgical technique for intussusception reduction in experienced hands. In addition, which method the surgeon chooses depends on the intraoperative findings. Different types of intussusception exist, and the most common type of intussusception is ileocolic. However, in our study, small intestinal was the most common type of intussusception secondary to PLPs, followed by ileocolic. In the study by Zhang [11], the common types of SI were ileoileal, ileoileocolic, or colocolic, but not ileocolic. The common causes of SI in children are Meckel’s diverticulum and intestinal duplication. Other rare causes include intestinal polyps, allergic purpura and intestinal tumors. In our study, PLPs were found in all patients and the types of PLPs varied widely. Meckel’s diverticulum was the main type of PLP, which was consistent with previous reports.
Conclusion
Intussusception secondary to PLPs tends to exhibit recurrence. There are various types of intussusception secondary to PLPs. It is necessary to improve auxiliary examinations to identify the etiology and avoid intraoperative omission. Surgical reduction of intussusception secondary to PLPs is the preferred clinical management.
References
Yao XM, Chen ZL, Shen DL et al (2015) Risk factors for pediatric intussusception complicated by loss of intestine viability in China from June 2009 to May 2014: a retrospective study. Pediatr Surg Int 31(2):163–166
Takahashi T, Miyano G, Kayano H et al (2014) A child with colo-colonic intussusception due to a large colonic polyp: case report and literature review. Afr J Paediatr Surg 11(3):261–263
Wong CW, Jin S, Chen J et al (2016) Predictors for bowel resection and the presence of a pathological lead point for operated childhood intussusception: a multi-center study. J Pediatr Surg 51(12):1998–2000
Wang Z, He QM, Zhang H et al (2015) Intussusception patients older than 1 year tend to have early recurrence after pneumatic enema reduction. Pediatr Surg Int 31(9):855–858
van Heurn LW, Pakarinen MP, Wester T (2014) Contemporary management of abdominal surgical emergencies in infants and children. Br J Surg 101(1):e24–e33
Huang HY, Huang XZ, Han YJ et al (2017) Risk factors associated with intestinal necrosis in children with failed non-surgical reduction for intussusception. Pediatr Surg Int 33(5):575–580
Morrison J, Jeanmonod R (2011) Intussusception secondary to a Meckel’s diverticulum in an adolescent. Case Rep Emerg Med. doi:10.1155/2011/623863
Huppertz HI, Soriano-Gabarró M, Grimprel E et al (2006) Intussusception among young children in Europe. Pediatr Infect Dis J 25(1 Suppl):S22–S29
Blakelock RT, Beasley SW (1998) The clinical implications of non-idiopathic intussusception. Pediatr Surg Int 14(3):163–167
Daneman A, Alton DJ, Lobo E et al (1998) Patterns of recurrence of intussusception in children: a 17-year review. Pediatr Radiol 28(12):913–919
Zhang Y, Dong Q, Li SX et al (2016) Clinical and ultrasonographic features of secondary intussusception in children. Eur Radiol 26(12):4329–4338
Kong MS, Chen CY, Tzen KY et al (1993) Technetium-99 m pertechnetate scan for ectopic gastric mucosa in children with gastrointestinal bleeding. J Formos Med Assoc 92:717–720
Ksia A, Mosbahi S, Brahim MB et al (2013) Recurrent intussusception in children and infants. Afr J Paediatr Surg. 10(4):299–301
Hsu WL, Lee HC, Yeung CY et al (2012) Recurrent intussusception: when should surgical intervention be performed? Pediatr Neonatol 53(5):300–303
Esmaeili-Dooki MR, Moslemi L, Hadipoor A et al (2016) Pediatric Intussusception in Northern Iran: comparison of recurrent with non-recurrent cases. Iran J Pediatr 26(2):e3898
Niramis R, Watanatittan S, Kruatrachue A et al (2010) Management of recurrent intussusception: nonoperative or operative reduction? J Pediatr Surg 45(11):2175–2180
Haber JJ, Waseem M (2013) Recurrent intussusception. Pediatr Emerg Care 29(6):753–755
Fecteau A, Flageole H, Nguyen LT et al (1996) Recurrent intussusception: safe use of hydrostatic enema. J Pediatr Surg 31(6):859–861
Acknowledgements
We would like to thank our colleagues from the Department of Pediatric Surgery, for their assistance with data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the ethic committee of The Second Affiliated Hospital and Yuying Children’s Hospital of Wenzhou Medical University and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
We declare that we have no conflict of interest.
Rights and permissions
About this article
Cite this article
Lin, Xk., Xia, Qz., Huang, Xz. et al. Clinical characteristics of intussusception secondary to pathologic lead points in children: a single-center experience with 65 cases. Pediatr Surg Int 33, 793–797 (2017). https://doi.org/10.1007/s00383-017-4101-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-017-4101-8